Abstract
Recently, the presence of CEBPA mutation was identified as an important prognostic factor for normal karyotype (NK) acute myeloid leukemia (AML). Because AML with CEBPA mutation is closely associated with CD7, CD15, CD34, and HLA-DR expression, we investigated the prognostic implications of CD7+ CD15+ CD34+ HLA-DR + immunophenotype in NK-AML. We analyzed the immunophenotype of 329 patients with NK-AML from the Japan Adult Leukemia Study Group (JALSG) AML97 population. NK-AML with the CD7+ CD15+ CD34+ HLA-DR + immunophenotype was classified as the CEBPA type, and NK-AML that did not meet this criterion was considered as the non-CEBPA type. The influence of the CEBPA status on event-free survival (EFS) and overall survival (OS) was assessed using log-rank test and a multivariate Cox proportional hazard regression model. Furthermore, the surface antigen expression profile in AML according to the CEBPA mutation status (monoallelic or biallelic) was also investigated. Of the 329 NK-AML patients that were studied, 39 and 243 were classified as having CEBPA and non-CEBPA type NK-AML, respectively. Patients with CEBPA type NK-AML had significantly better EFS and OS than those with non-CEBPA type NK-AML. Multivariate analysis showed that the CEBPA type and white blood cell (WBC) counts of >20 × 109/L were independent prognostic factors for EFS and OS. Moreover, NK-AML with the biallelic CEBPA mutation was more closely associated with CD34 positivity than that with the monoallelic CEBPA mutation. NK-AML with the CD7+ CD15+ CD34+ HLA-DR + immunophenotype is a clinically discrete entity, and this may have a possible role in risk stratification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, immunophenotyping of hematologic neoplasms has become standard practice to establish a diagnosis and define the origin of the malignant cell lineage. Patients with acute myeloid leukemia (AML) often show aberrant cellular antigen expression as well as chromosomal abnormalities. The clinical significance of surface antigen expression has been studied for more than 20 years, but thus far, it has yielded inconsistent results [1]. Nevertheless, if the evaluation of antigen expression is limited to a subtype of AML, we would be more likely to find a significant relationship between surface antigen expression and prognosis. For example, the significance of CD56 expression as an adverse prognostic factor in both acute promyelocytic leukemia (APL) and AML with t(8;21) is widely accepted [2, 3].
Normal karyotype (NK)-AML is the most common subtype of AML, accounting for 40–50 % of cases [4-6]. Patients with this subtype are considered to have an intermediate risk, and upfront hematopoietic stem cell transplantation (HSCT) is commonly recommended [7-9]. However, even though treatment strategies seem promising, the prognosis of NK-AML is variable when molecular evaluation of the FLT3, NPM1, and CEBPA mutations is taken into account [10-14]. Schlenk et al. [10] reported that NK-AML patients with the CEBPA mutation or NPM1 mutation, but without the FLT3 mutation, had a favorable prognosis and that upfront HSCT in these patients did not contribute to the overall survival (OS). Although the detection of subgroups is necessary for decisions on the most appropriate treatment strategy, routine molecular diagnoses are often difficult in clinical practice.
AML with the CEBPA mutation has a homologous surface antigen expression that is closely associated with CD7, CD15, CD34, and HLA-DR positivity [15, 16]. We speculated that immunophenotyping for CD7, CD15, CD34, and HLA-DR in patients with NK-AML could identify a distinct subtype of AML that clinically mimics AML with the CEBPA mutation. In the Japan Adult Leukemia Study Group (JALSG) AML97 study, almost 42 % of the patients with AML were diagnosed with NK-AML. For this study, results of surface antigen expression were obtained at the time of enrollment. Further, we used data from the JALSG AML97 study to investigate the clinical significance of these surface antigens for the prognosis of patients with NK-AML.
Patients and methods
Patients
We conducted a retrospective review of patient data from the multicenter JALSG AML97 study. Detailed information of this study and its results has previously been reported [17, 18]. Briefly, between December 1997 and July 2001, patients aged 15–64 years, with newly diagnosed de novo AML, excluding those with APL, were consecutively enrolled to the JALSG AML97 study. In total, 789 of the 809 AML patients were eligible for the study, and informed consent was obtained from all patients or their guardians before enrollment. The study protocol was approved by the research ethics boards of all participating institutions, and the study was conducted in accordance with the Declaration of Helsinki.
Cytogenetic studies
The results from the cytogenetic studies, which were performed at each of the institutions, were reported to the JALSG Statistical Center. Routinely, 20 metaphases were counted for each patient and analyzed according to the recommendations of the International System for Human Cytogenetic Nomenclature.
Flow cytometry
Immunophenotyping was performed at each institution, primarily on freshly collected bone marrow or peripheral blood samples that were collected at the time of diagnosis. Leukemic cell analysis was performed at local or reference laboratories by standard immunofluorescence methods using monoclonal antibodies directed against the CD2, CD3, CD4, CD5, CD7, CD8, CD11b, CD13, CD15, CD19, CD33, CD34, CD41a, CD56, and HLA-DR surface antigens. Samples were considered positive if at least 20 % of blasts expressed the antigen.
Treatment regimen used in the JALSG AML97 study
Induction therapy consisted of Ara-C at a dose of 100 mg/m2 per day as a continuous infusion on days 1–7 and idarubicin (IDR) at a dose of 12 mg/m2 per day as a 30-min infusion on days 1–3. Patients who did not achieve remission after the first induction cycle were given the same therapy again. Patients who obtained complete remission (CR) within two courses of induction therapy were randomly assigned to a group that received either four courses of standard dose consolidation therapy without maintenance (arm A) or three courses of standard dose consolidation along with six courses of maintenance therapy (arm B). In the JALSG AML97 study, the 5-year overall survival rate and the 5-year disease-free survival (DFS) rate between the arms were not statistical different [17].
Surface antigen expression profile according to the CEBPA mutant pattern
We also investigated the surface antigen expression profiles according to CEBPA mutant pattern in 318 AML patients based on the data records of AML patients enrolled at the Kumamoto and Nagasaki Universities. High molecular weight genomic DNA was extracted from the bone marrow or peripheral blood samples after Ficoll separation of mononuclear cells. Mutations of the CEBPA gene was detected by genomic DNA PCR, and direct sequencing was performed at each institution, as described previously [19, 20].
Statistical analysis
OS for all patients was defined as the period from the date of diagnosis to the date of death. Event-free survival (EFS) was defined as the period from the date of diagnosis to the date of the first recurrence after CR or any cause of death. All patients who underwent HSCT were censored from the EFS analysis on the date of HSCT treatment. The Kaplan-Meier method was used to estimate the EFS and OS. The log-rank test was used to compare the EFS or OS of the two groups. Factors that could potentially affect clinical outcome, including age, sex, WBC count, performance status at diagnosis, and the expression of each surface antigen were analyzed by the multivariate Cox proportional hazard regression model. Fisher’s exact test and Student’s t test were used to compare factor differences between the two groups. Statistical analysis was performed with the JMP software version 8.0.1 (SAS Institute Inc., Cray, NC, USA).
Results
Definition of the CEBPA type
For this study, CEBPA type NK-AML was defined as NK-AML that showed the CD7+ CD15+ CD34+ HLA-DR + immunophenotype because these antigens are commonly expressed in AML with the CEBPA mutation [15, 16]. Non-CEBPA type NK-AML was defined as NK-AML that did not have the CD7+ CD15+ CD34+ HLA-DR + immunophenotype.
In total, 329 patients were diagnosed with NK-AML. The expression of CD7, CD15, CD34, and HLA-DR was examined in 303, 201, 306, and 302 patients, respectively. Of the 329 NK-AML patients, 39 were classified as having the CEBPA type and 243 were classified as having the non-CEBPA type NK-AML. We excluded 47 patients whose of immunophenotype could not be determined.
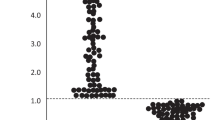
EFS and OS
The 5-year EFS rate for patients with CEBPA type NK-AML was 48.5 %, which was significantly higher than the 30.5 % for patients with non-CEBPA type NK-AML (P = 0.044, Fig. 1a). Furthermore, the 5-year OS rate for patients with CEBPA type NK-AML was also significantly higher than that for patients with non-CEBPA type NK-AML (67.4 vs 35.7 %, P = 0.0038, Fig. 1b).
Kaplan-Meier curves show event-free survival (EFS) and overall survival (OS) according to the CEBPA status. EFS and OS for each group are shown in a and b, respectively. Log-rank test revealed the 5-year EFS to be 48.5 and 30.5 % for patients with CEBPA and non-CEBPA type NK-AML, respectively, which was significantly different (P = 0.044). The 5-year OS of patients with CEBPA and non-CEBPA type NK-AML was also significant (67.4 and 35.7 %, respectively; P = 0.0038)
Univariate analysis showed that the outcome of patients with increased WBC counts at diagnosis was significantly worse (Tables 1 and 2), in agreement with previous reports [1]. Furthermore, CEBPA type was also a significant factor for better EFS and OS (Tables 1 and 2). Multivariate analysis showed CEBPA type and increased WBC counts to be independent prognostic factors (Tables 1 and 2). Other factors such as age, performance status, sex, or the expression of each of the single surface antigens did not affect the EFS and OS rates.
Our study included 12 patients with CEPBA type NK-AML and 77 patients with non-CEBPA type NK-AML who received HSCT. There was no significant difference among patients who received HSCT in these two groups (Table 3). The 2-year OS after HSCT in these groups were 61 and 41 %, respectively, which did not reach significance (P = 0.467).
Clinical profiles in CEBPA type
The CEBPA type was identified as an independent prognostic factor for EFS and OS. Therefore, we analyzed the characteristics of CEBPA type (Table 3). Sex, WBC count, or performance status was not associated with CEBPA or non-CEBPA type NK-AML. In contrast, compared with non-CEBPA type NK-AML, CEBPA type NK-AML was associated with younger age, higher myeloperoxidase (MPO)-positive rates, frequent presentation with Auer rods, and a French-American-British (FAB) classification of M1 or M2.
Surface antigen profiles according to CEBPA mutant pattern
We investigated the expression of surface antigens according to monoallelic or biallelic CEBPA mutation in patients with AML. Of the 318 AML patients, 41 were diagnosed with the CEBPA mutation, which included 29 with biallelic and 12 with monoallelic mutations. The presence of the CEBPA mutation was common in intermediate risk AML, including NK-AML. In contrast, the mutation was uncommon in core-binding factor (CBF)-AML and adverse risk AML.
To investigate the association between surface antigen expression and CEBPA mutant pattern in NK-AML patients, the expressions of CD7, CD34, and HLA-DR were examined (Table 4). There was a significantly higher frequency of CD34 expression in AML patients with biallelic CEBPA mutation than in those with monoallelic mutation.
Discussion
The results of this study show that the CD7+ CD15+ CD34+ HLA-DR + immunophenotype is a significant predictor of OS in patients with NK-AML. We were able to analyze data from a well-designed, uniform, prospective study. In addition, we observed that CEBPA type NK-AML was a discrete clinical entity, which is closely associated with high MPO positivity rates, Auer rod positivity, FAB classification of M1 or M2, and a younger age. These characteristics are very similar to the characteristics of AML with CEBPA mutation as previously reported: AML with the CEBPA mutation also had high MPO rates [19], FAB classification of M1 or M2 [21], and better OS [10, 11]. In addition, the prognosis of CEBPA type NK-AML was almost similar to that in the favorable risk group of AML as indicated by the JALSG scoring system [17] and that in AML patients with the CEBPA mutation [10, 11], as previously reported. Moreover, of 282 patients with NK-AML, 14 % had CEBPA type NK-AML, which is similar to that observed in previous reports (i.e., 10–18 % of patients with NK-AML had the CEBPA mutation) [22].
It is also known that the expressions of CD7, CD34, and HLA-DR are associated with poor clinical outcomes in AML [1]. In contrast to previous reports, our study, which was limited to NK-AML patients, demonstrated that the expression of single surface antigens including CD7, CD15, CD34, and HLA-DR did not have prognostic significance. Moreover, the CEBPA immunophenotype demonstrated a favorable OS even though the population positively expressed CD7, CD34, and HLA-DR, which have previously been considered poor prognostic factors.
It was previously reported that CD7 expression is associated with the FLT3 mutation [23], CEBPA mutation [15, 16], and adverse risk cytogenetics [2, 24]. Furthermore, CD34 positivity is frequently observed in patients with adverse risk cytogenetics and t(8;21) AML [2], and it is negatively associated with NPM1 mutations [25]. Another surface antigen, the B-cell marker CD19, which is observed in t(8;21) AML and that is associated with negativity for KIT mutation, favorably affects CR in AML patients with t(8;21) [2, 26]. Taken together, these results represent the difficulty in analyzing the heterogeneous population of AML as a total group because the impact of chromosomal and/or molecular abnormalities on prognosis makes it difficult to conclusively interpret the significance of surface antigen expression.
On the other hand, the population, which we detected with this combination of surface antigens, is evidently a distinct subtype of NK-AML with a discrete clinical profile (Table 3). Our findings show that specific subtypes of AML such as NK-AML with the CEBPA mutation potentially exist, and it suggests that the population of patients who have a favorable prognosis may well be identified through an analysis of the surface antigens that are expressed. Therefore, if the molecular evaluation is unavailable, an analysis of surface antigens may help in identifying patients with a favorable prognosis.
It is known that biallelic CEBPA mutations, but not monoallelic mutations, have a favorable prognosis [27]. Our study, which included all cases with the CEBPA mutation, showed that 93 % of cases with biallelic mutation were positive for CD34, while only 50 % of cases with monoallelic mutation were positive (Table 4), suggesting that CD34 is an important factor for distinguishing the mutant pattern. Because low activity of CEBPA is thought to be a critical factor for sustaining the immature character of AML cells [28], we hypothesized that a more potent inactivation of CEBPA by biallelic mutation results in the frequent incidence of CD34 positivity.
In this study, immunophenotypic analyses were not performed at a central facility. Another limitation of our study is the possible selection bias; not all the institutes performed cytometric analysis of all AML97 study antigens at the time of patient enrollment. This resulted in a reduction in sample size, because CEBPA status was not detected in 14 % of patients with NK-AML. JALSG has recently investigated whether molecular evaluations, including that of the CEBPA mutation, affect patient prognosis [29]. In the future, we hope to clarify the relationships among surface antigen expression, cytogenetics, molecular evaluation results, and clinical features of AML. In conclusion, we found that the CD7+ CD15+ CD34+ HLA-DR + immunophenotype has a potential role in risk stratification for patients with NK-AML.
References
Mason KD, Juneja SK, Szer J (2006) The immunophenotype of acute myeloid leukemia: is there a relationship with prognosis? Blood Rev 20(2):71–82
Iriyama N, Hatta Y, Takeuchi J, Ogawa Y, Ohtake S, Sakura T, Mitani K, Ishida F, Takahashi M, Maeda T, Izumi T, Sakamaki H, Miyawaki S, Honda S, Miyazaki Y, Taki T, Taniwaki M, Naoe T (2013) CD56 expression is an independent prognostic factor for relapse in acute myeloid leukemia with t(8;21). Leuk Res 37(9):1021–1026
Montesinos P, Rayón C, Vellenga E, Brunet S, González J, González M, Holowiecka A, Esteve J, Bergua J, González JD, Rivas C, Tormo M, Rubio V, Bueno J, Manso F, Milone G, de la Serna J, Pérez I, Pérez-Encinas M, Krsnik I, Ribera JM, Escoda L, Lowenberg B, Sanz MA, PETHEMA, HOVON Groups (2011) Clinical significance of CD56 expression in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and anthracycline-based regimens. Blood 117(6):1799–1805
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, Rees J, Hann I, Stevens R, Burnett A, Goldstone A (1998) The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children’s Leukaemia Working Parties. Blood 92(7):2322–2333
Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A, Paietta E, Willman CL, Head DR, Rowe JM, Forman SJ, Appelbaum FR (2000) Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood 96(13):4075–4083
Byrd JC, Mrózek K, Dodge RK, Carroll AJ, Edwards CG, Arthur DC, Pettenati MJ, Patil SR, Rao KW, Watson MS, Koduru PR, Moore JO, Stone RM, Mayer RJ, Feldman EJ, Davey FR, Schiffer CA, Larson RA, Bloomfield CD, Cancer and Leukemia Group B (CALGB 8461) (2002) Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood 100(13):4325–4336
Cornelissen JJ, van Putten WL, Verdonck LF, Theobald M, Jacky E, Daenen SM, van Marwijk KM, Wijermans P, Schouten H, Huijgens PC, van der Lelie H, Fey M, Ferrant A, Maertens J, Gratwohl A, Lowenberg B (2007) Results of a HOVON/SAKK donor versus no-donor analysis of myeloablative HLA-identical sibling stem cell transplantation in first remission acute myeloid leukemia in young and middle-aged adults: benefits for whom? Blood 109(9):3658–3666
Yanada M, Matsuo K, Emi N, Naoe T (2005) Efficacy of allogeneic hematopoietic stem cell transplantation depends on cytogenetic risk for acute myeloid leukemia in first disease remission: a metaanalysis. Cancer 103(8):1652–1658
Koreth J, Schlenk R, Kopecky KJ, Honda S, Sierra J, Djulbegovic BJ, Wadleigh M, DeAngelo DJ, Stone RM, Sakamaki H, Appelbaum FR, Döhner H, Antin JH, Soiffer RJ, Cutler C (2009) Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: systematic review and meta-analysis of prospective clinical trials. JAMA 301(22):2349–2361
Schlenk RF, Döhner K, Krauter J, Fröhling S, Corbacioglu A, Bullinger L, Habdank M, Späth D, Morgan M, Benner A, Schlegelberger B, Heil G, Ganser A, Döhner H, German-Austrian Acute Myeloid Leukemia Study Group (2008) Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med 358(18):1909–1918
Fröhling S, Schlenk RF, Stolze I, Bihlmayr J, Benner A, Kreitmeier S, Tobis K, Döhner H, Döhner K (2004) CEBPA mutations in younger adults with acute myeloid leukemia and normal cytogenetics: prognostic relevance and analysis of cooperating mutations. J Clin Oncol 22(4):624–633
Döhner K, Schlenk RF, Habdank M, Scholl C, Rücker FG, Corbacioglu A, Bullinger L, Fröhling S, Döhner H (2005) Mutant nucleophosmin (NPM1) predicts favorable prognosis in younger adults with acute myeloid leukemia and normal cytogenetics: interaction with other gene mutations. Blood 106(12):3740–3746
Schnittger S, Schoch C, Kern W, Mecucci C, Tschulik C, Martelli MF, Haferlach T, Hiddemann W, Falini B (2005) Nucleophosmin gene mutations are predictors of favorable prognosis in acute myelogenous leukemia with a normal karyotype. Blood 106(12):3733–3739
Bacher U, Haferlach C, Kern W, Haferlach T, Schnittger S (2008) Prognostic relevance of FLT3-TKD mutations in AML: the combination matters—an analysis of 3082 patients. Blood 111(5):2527–2537
Lin LI, Chen CY, Lin DT, Tsay W, Tang JL, Yeh YC, Shen HL, Su FH, Yao M, Huang SY, Tien HF (2005) Characterization of CEBPA mutations in acute myeloid leukemia: most patients with CEBPA mutations have biallelic mutations and show a distinct immunophenotype of the leukemic cells. Clin Cancer Res 11(4):1372–1379
Röhrs S, Scherr M, Romani J, Zaborski M, Drexler HG, Quentmeier H (2010) CD7 in acute myeloid leukemia: correlation with loss of wild-type CEBPA, consequence of epigenetic regulation. J Hematol Oncol 3:15
Miyawaki S, Sakamaki H, Ohtake S, Emi N, Yagasaki F, Mitani K, Matsuda S, Kishimoto Y, Miyazaki Y, Asou N, Matsushima T, Takahashi M, Ogawa Y, Honda S, Ohno R, Japan Adult Leukemia Study Group AML 97 Study (2005) A randomized, postremission comparison of four courses of standard-dose consolidation therapy without maintenance therapy versus three courses of standard-dose consolidation with maintenance therapy in adults with acute myeloid leukemia: the Japan Adult Leukemia Study Group AML 97 Study. Cancer 104(12):2726–2734
Sakamaki H, Miyawaki S, Ohtake S, Emi N, Yagasaki F, Mitani K, Matsuda S, Kishimoto Y, Miyazaki Y, Asou N, Takahashi M, Ogawa Y, Honda S, Ohno R (2010) Allogeneic stem cell transplantation versus chemotherapy as post-remission therapy for intermediate or poor risk adult acute myeloid leukemia: results of the JALSG AML97 study. Int J Hematol 91(2):284–292
Tominaga-Sato S, Tsushima H, Ando K, Itonaga H, Imaizumi Y, Imanishi D, Iwanaga M, Taguchi J, Fukushima T, Yoshida S, Hata T, Moriuchi Y, Kuriyama K, Mano H, Tomonaga M, Miyazaki Y (2011) Expression of myeloperoxidase and gene mutations in AML patients with normal karyotype: double CEBPA mutations are associated with high percentage of MPO positivity in leukemic blasts. Int J Hematol 94(1):81–89
Nanri T, Uike N, Kawakita T, Iwanaga E, Mitsuya H, Asou N (2010) A family harboring a germ-line N-terminal C/EBPalpha mutation and development of acute myeloid leukemia with an additional somatic C-terminal C/EBPalpha mutation. Genes Chromosome Cancer 49(3):237–241
Ho PA, Alonzo TA, Gerbing RB, Pollard J, Stirewalt DL, Hurwitz C, Heerema NA, Hirsch B, Raimondi SC, Lange B, Franklin JL, Radich JP, Meshinchi S (2009) Prevalence and prognostic implications of CEBPA mutations in pediatric acute myeloid leukemia (AML): a report from the Children’s Oncology Group. Blood 113(26):6558–6566
Döhner K, Döhner H (2008) Molecular characterization of acute myeloid leukemia. Haematologica 93(7):976–982
Rausei-Mills V, Chang KL, Gaal KK, Weiss LM, Huang Q (2008) Aberrant expression of CD7 in myeloblasts is highly associated with de novo acute myeloid leukemias with FLT3/ITD mutation. Am J Clin Pathol 129(4):624–629
Li X, Li J, Du W, Zhang J, Liu W, Chen X, Li H, Huang S, Li X (2011) Relevance of immunophenotypes to prognostic subgroups of age, WBC, platelet count, and cytogenetics in de novo acute myeloid leukemia. APMIS 119(1):76–84
Ferrari A, Bussaglia E, Úbeda J, Facchini L, Aventin A, Sierra J, Nomdedéu JF (2012) Immunophenotype distinction between acute promyelocytic leukaemia and CD15–CD34− HLA-DR− acute myeloid leukaemia with nucleophosmin mutations. Hematol Oncol 30(3):109–114
De J, Zanjani R, Hibbard M, Davis BH (2007) Immunophenotypic profile predictive of KIT activating mutations in AML1-ETO leukemia. Am J Clin Pathol 128(4):550–557
Wouters BJ, Löwenberg B, Erpelinck-Verschueren CA, van Putten WL, Valk PJ, Delwel R (2009) Double CEBPA mutations, but not single CEBPA mutations, define a subgroup of acute myeloid leukemia with a distinctive gene expression profile that is uniquely associated with a favorable outcome. Blood 113(13):3088–3091
Cammenga J, Mulloy JC, Berguido FJ, MacGrogan D, Viale A, Nimer SD (2003) Induction of C/EBPalpha activity alters gene expression and differentiation of human CD34+ cells. Blood 101(6):2206–2214
Miyawaki S (2012) Clinical studies of acute myeloid leukemia in the Japan Adult Leukemia Study Group. Int J Hematol 96(2):171–177
Acknowledgments
We thank the clinicians and the leaders of the 103 institutions who entered their patients into the JALSG AML97 study and provided the data necessary to make this study possible. The study was supported by Grants-in-Aid from the Ministry of Health, Labor and Welfare for Cancer Research (Clinical Cancer Research H23-004) and the National Cancer Center Research and Development Fund (23-A-23).
Conflict of interest
There are no relevant conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iriyama, N., Asou, N., Miyazaki, Y. et al. Normal karyotype acute myeloid leukemia with the CD7+ CD15+ CD34+ HLA-DR + immunophenotype is a clinically distinct entity with a favorable outcome. Ann Hematol 93, 957–963 (2014). https://doi.org/10.1007/s00277-014-2013-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-014-2013-4