Abstract
Type 2 interleukin-1 receptor (IL1R2) is a member of the IL1 family. It has been reported that IL1R2 is expressed and plays important roles in several cancers. However, its potential role in human osteosarcoma has not been reported. In the present study, a recombinant lentivirus harboring short hairpin RNA against IL1R2 was constructed and then transfected human osteosarcoma U-2 OS cells. The proliferation of infected cells was measured by 3-(4, 5- dimethyl-2-thiazolyl)-2, 5-diphenyl-2H-tetrazolium bromide (MTT) assay and plate colony formation assay. Results showed that efficiency of lentivirus infection was more than 80 %. The knockdown efficiency of IL1R2 mRNA level was up to 95 % compared with control group. After treatment with lentiviruses containing shIL1R2 (Lv-shIL1R2), the proliferation and colony formation of U-2 OS cells were obviously reduced (P < 0.001). Cell cycle assay was used to investigate the mechanism of the inhibition of proliferation of U-2 OS cells. We found that after Lv-shIL1R2 treatment, the percentage of cells at G0/G1 phase decreased significantly, whereas cells at S and G2/M phases increased markedly (P < 0.05). In conclusion, shIL1R2 indeed inhibited the proliferation of U-2 OS cells which might be associated with the blockage of S and G2/M phases. The results suggested that IL1R2 could have oncogenic potential and shIL1R2 might represent a new and effective therapeutic treatment for osteosarcoma patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteosarcoma is the most common primary malignant bone tumor and represents over 56 % of all bone tumors [1, 2]. The estimated incidence worldwide is approximately one to four cases per million people per year [2, 3]. It has a bimodal age distribution, with a primary peak during adolescence and a smaller, secondary peak in the elderly [1–4]. Among patients under 21 years of age, osteosarcoma accounts for approximately 60 % of bone tumors [5], while patients older than 60 years constitute about 10 % of the patient population [1]. Osteosarcoma occurs in the long bones of the limbs, near the metaphyseal region. Common sites include the femur, the tibia and the humerus, and less commonly the skull, the jaw or the pelvis [1, 3]. The mainstay treatments include surgery and chemotherapy [2, 3, 6, 7]. With the combination of neoadjuvant chemotherapy and radical tumor resection [8], the 5-year overall survival rate is >70 % and the 5-year event-free survival rate is up to 70 % for patients with localized disease [1–3, 6–11]. However, survival for patients with metastatic or relapsed osteosarcoma has remained virtually unchanged over the past 30 years, with an overall 5-year survival rate of about 20 % [3, 9]. To further improve prognosis for osteosarcoma patients, new treatments are urgently needed
Interleukin-1 receptor type 2 (IL1R2) is a member of the IL1 family, which was first characterized by McMahon et al. [12–14] in 1991. In humans, IL1R2 is located on the long arm of chromosome 2 at band 2q12. IL1R2 is natively found on neutrophils, B-cells, monocytes and macrophages. As a decoy receptor, IL1R2 is natural inhibitor of IL1 and plays important roles in inflammation and immune regulation. Notably, several studies have shown IL1R2 expression in various cancers such as prostate cancer [15–17], ovarian cancer [18–20], breast cancer [21, 22], Hodgkin lymphoma [23], lung cancer [24], hepatocellular carcinoma [25], pancreatic cancer [26], colon carcinoma [27] and adrenocortical cancer [28, 29]. These studies suggested that IL1R2 might be involved in tumorigenesis and progression of the above cancers. As far as we know, there has been no study concerning the possible roles of IL1R2 in human osteosarcoma. Therefore, the objective of this study was to investigate the possible function of IL1R2 in human osteosarcoma U-2 OS cells.
Materials and methods
Cell culture
Human embryonic kidney 293T (HEK293T) cell line and the osteosarcoma cell line (U-2 OS) were purchased from Cell Bank of Chinese Academy of Science (Shanghai, China). Cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM; Hyclone, Shanghai Bioleaf Biotech Co., Ltd, China) supplemented with 10 % fetal bovine serum (Bioind, Shanghai XP Biomed Ltd., China), 100 U/ml penicillin and 100 mg/ml streptomycin (Hyclone, Shanghai Bioleaf Biotech Co., Ltd, China) under standard cell culture conditions at 37 °C in a 5 % CO2-humidified atmosphere.
Construction of recombinant lentivirus and IL1R2 silencing
The small interfering RNA (siRNA) sequence for IL1R2 (5′-GACCATTCCTGTGATCATTTCCTCGAGGAAATGATCACAGGAATGGTC-3′) was selected after screening to validate potential siRNAs. Non-silencing siRNA (5′-GCGGAGGGTTTGAAAGAATATCTCGAGATATTCTTTCAAACCCTCCGCTTTTTT-3′) was used as control. ShRNAs for IL1R2 and control RNA, corresponding to the above siRNA sequences, were then generated, respectively. They were synthesized and inserted downstream of the U6 promoter in the lentiviral vector pFH-L (Hollybio Co., Ltd., Shanghai, China). Lentiviruses were generated by triple transfection of 80 % confluent HEK293T cells with modified pFH-L plasmid (shRNA vector), pVSVG-I and pCMV△R8.92 pHelper plasmids (Hollybio Co., Ltd., Shanghai, China) using Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA). Lentiviruses were harvested in serum-free medium after 3 days, filtered and concentrated in primed Centricon Plus-20 filter devices (Millipore, Billerica, MA, USA).
Lentivirus infection
To assess the effect of IL1R2 on human osteosarcoma U-2 OS cells, lentiviruses containing shIL1R2 (Lv-shIL1R2) were added at multiplicity of infection (MOI) of 20 to 6-well plates whose initial cell inoculation density was 3 × 104 cells/well, and then, they were blended gently and incubated for 8 h. Subsequently, fresh medium was added to cell plates. After further 72-h incubation, cell images were recorded under a fluorescence microscope (Olympus Co., Ltd., Shanghai, China) to count the lentivirus infection.
RNA extraction and quantitative real-time PCR (qRT-PCR)
Total RNA was extracted from infected U-2 OS cells at the 5th day of culture using Trizol reagent (Invitrogen, Carlsbad, CA) according to the manufacturer’s instructions. The concentration and purity of RNA were measured spectrophotometrically at 260 and 280 nm on a microplate reader [Bio-Rad Laboratories (Shanghai) Co., Ltd., China], whereas RNA integrity was assessed by agarose gel electrophoresis. Only the samples with the OD A260/A280 ratio close to value of 2.0, which indicates that the RNA is pure, were subsequently analyzed [30].
Two μg of total RNA was used to synthesize cDNA using M-MLV reverse transcriptase (Promega, USA). Quantitative real-time PCR was performed on a Bio-Rad Connect Real-Time PCR platform [Bio-Rad Laboratories (Shanghai) Co., Ltd., China] with iQSYBR Green Supermix [Bio-Rad Laboratories (Shanghai) Co., Ltd., China]. β-actin was used as the input reference. The following primers were used: IL1R2: 5′-CCAGGAGAAGAAGAGACACGGATG-3′ as forward and 5′-GTATGAGATGAACGGCAGGAAAGC-3′ as reverse; β-actin: 5′-GTGGACATCCGCAAAGAC-3′ as forward and 5′-AAAGGGTGTAACGCAACTA-3′ as reverse. The amplification steps were as follows: initial denaturation at 95 °C for 1 min, followed by 40 cycles consisting of denaturation at 95 °C for 5 s and annealing extension at 60 °C for 20 s. Absorbance value was read at the extension stage. The expression levels of IL1R2 were calculated utilizing the 2−ΔΔCt method [31].
Cell viability analysis and colony formation assay
The effect of shIL1R2 on U-2 OS cells was assessed by using MTT assay as described by Mosmann [32]. U-2 OS cells from different groups were seeded at an initial density of 1 × 104 cells/ml per well into 96-well plates. After 24-h incubation, MTT solution was added into each well at a final concentration of 5 mg/ml. After further 4-h incubation, the medium was removed, and dimethylsulfoxide (DMSO) was then added to dissolve the formazan crystals. Each sample was measured with a microplate reader [Bio-Rad Laboratories (Shanghai) Co., Ltd., China] at a wavelength of 595 nm. Viability of cells was expressed relative to theoretical absorbance (A).
To assay colony formation, infected cells were planted at an initial density of 500 cells/well in 6-well plates. Clone growth was observed every day under a microscope (Olympus Co., Ltd., Shanghai, China). The interval of medium change was 2 days. After 9-day incubation, cells were fixed with methanol and stained with Giemsa. The number and size of colonies in each group were recorded and counted.
Cell cycle analysis by flow cytometry
The mechanism of shIL1R2 on U-2 OS cells was investigated by using cell cycle analysis. U-2 OS cells from different groups were seeded at an initial density of 8 × 104 cells/dish into Petri dishes (6 cm in diameter). After about 40-h incubation, the medium was removed, cells were washed by phosphate-buffered saline (PBS) to prepare single cell suspension, and then the single cell suspension was fixed with 75 % pre-cooling ethanol at 4 °C for 24 h. Subsequently, the cells were centrifuged and resuspended with PBS. After centrifugation again, supernate was removed and fresh solution of Prodium Iodide (PI solution, containing PI and RNase A) was added to residual sediments to suspend cells. After 1-h incubation at 37 °C, the above prepared samples were transferred to ice or stored at 4 °C in the dark. Finally, the samples were tested on a flow cytometer according to the manufacturer’s guidelines, and the percentage of cells at G0/G1, S and G2/M phases of the cell cycle were determined using Modfit LT 3.0 analytical software (Becton–Dickinson, San Jose, CA, USA).
Statistical analysis
Data were expressed mean ± standard deviations (SD). All statistical analyses were performed using SPSS 13.0 (SPSS, Inc., Chicago, IL, USA) statistic software. The differences between groups were compared using Student’s t test. P < 0.05 was considered to indicate a significantly statistical difference.
Results
Lentivirus infection and knockdown efficiency of IL1R2 mRNA level
In this study, we successfully constructed Lv-shIL1R2. To assess IL1R2 function in osteosarcoma cells, shRNA targeting IL1R2 was designed and inserted into recombinant lentivirus plasmid. Efficiency of lentivirus infection was approximately 80 % as evidenced by GFP expression 3 days after infection (Fig. 1a). IL1R2 mRNA expression was then measured with qRT-PCR. The knockdown efficiency of IL1R2 mRNA level was up to 95 %. There was significantly statistical difference in the express of IL1R2 mRNA level between control group (cells infected Lv-Control-shRNA) and Lv-shIL1R2 group (cells infected Lv-shIL1R2) (P < 0.001, Fig. 1b).
Lentivirus infection and knockdown efficiency of IL1R2 mRNA level. a Images of U-2 OS cells infected with indicated lentivirus at MOI of 20 are shown under a fluorescence microscope. Scale bar 10 μm. b Knowdown efficiency of IL1R2 mRNA levels analyzed by qRT-PCR. The data are shown means with SD (error bars); ***P < 0.001, significant versus control group; shCon: cells infected with Lv-Control-shRNA, shIL1R2: cells infected with Lv-shIL1R2
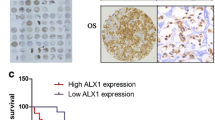
IL1R2 knockdown inhibited osteosarcoma cells proliferation in vitro
To elucidate the function of IL1R2 in osteosarcoma proliferation, human osteosarcoma U-2 OS cells were infected with Lv-Control-shRNA and Lv-shIL1R2, respectively. The proliferation of infected cells was first examined by MTT assay. The growth curves for cells infected with Lv-shIL1R2 were markedly lower than those for control cells (cells infected with Lv-Control-shRNA) at the 4th day of culture (P < 0.001, Fig. 2a). Furthermore, colony formation assay in monolayer culture showed that the number and size of surviving colonies of cells after treatment with Lv-shIL1R2 were obviously reduced compared with the control group, suggesting that Lv-shIL1R2 could result in inhibition of colony formation of U-2 OS cells (P < 0.001, Fig. 2b, c).
Effects of IL1R2 siRNA on the proliferation and colony formation of U-2 OS cells. a Downregulation of IL1R2 gene inhibits proliferation of U-2 OS cells. b Images show the number and size of colonies in each group. Scale bar 25 μm. c Statistical analysis of the number of colonies in each group. The data are shown means with SD (error bars); ***P < 0.001, significant versus control group; shCon: cells infected with Lv-Control-shRNA, shIL1R2: cells infected with Lv-shIL1R2
The suppression of proliferation in U-2 OS cells resulted from blocked cell cycle progression
To determine how IL1R2 knockdown inhibited osteosarcoma cells proliferation, we used cell cycle analysis to examine the change of cell cycle distribution of U-2 OS cells after Lv-shIL1R2 treatment. Cell cycle distributions of control group and Lv-shIL1R2 group are shown in Fig. 3a. As summarized in Fig. 3b, the percentage of G0/G1 phase cells was 43 % in control group, while that was 35 % in Lv-shIL1R2 group. The percentage of cells at S and G2/M phases was 42 and 15 %, respectively, in control group, while that in Lv-shIL1R2 group was 46 and 19 %, respectively. Therefore, after treatment with Lv-shIL1R2, the percentage of cells at G0/G1 phase decreased significantly (P < 0.001), while that of cells at S and G2/M phases increased markedly (P < 0.05, P < 0.01, respectively). These results suggested that the inhibition of osteosarcoma cells proliferation by Lv-shIL1R2 might be associated with the above change of cell cycle distribution.
Effects of IL1R2 siRNA on the cell cycle of U-2 OS cells. a Cell cycle distribution of each group by flow cytometer. b Statistical analysis of cell cycle distribution of each group. The data are shown means with SD (error bars); *P < 0.05, **P < 0.01, ***P < 0.001, significant vs. control group; shCon: cells infected with Lv-Control-shRNA, shIL1R2: cells infected with Lv-shIL1R2
Discussion
Several studies have found that IL1R2 was expressed in various cancers and might be involved in tumorigenesis and tumor development [12–29]. Ricote et al. [15] found that only the periphery of epithelial cells expressed IL1R2 in prostate carcinoma (PC) samples. The percentage of IL1R2- positive samples was similar in PC samples with low and high Gleason grades. They deduced that IL1R2 expression in PC might be related to the ability of this receptor as a natural inhibitor of IL1 function, and this expression might be an effort to counteract IL1 function. Ma et al. [23] reported that IL1R2 protein level was significantly elevated in Hodgkin lymphoma (HL) and concluded that IL1R2 secreted by Hodgkin and Reed-Sternberg (HRS) cells was capable of capturing IL1α or IL1β expressed on HRS cells and reactive cells, thus preventing their interaction with the functional receptor IL1R1 and blocking effective IL1 signaling on HRS cells and/or reactive cells. Significant overexpression of IL1R2 was found in adrenocortical cancer (ACC) in one microarray study [28], while the expression of IL1R2 was downregulated in ACC after treatment with 9-cis retinoic acid which had the potential antitumoral effects [29]. IL1R2 might be involved in ACC development through immune response [29].
Pantschenko et al. [21] showed IL1R2 expression in human breast cancer and concluded that activation of the IL1/IL1R cytokine family via autocrine and/or paracrine mechanisms leaded to a cascade of secondary protumorigenic cytokines. These secondary signals induced the expression of numerous protumorigenic activities and subsequently contributed to angiogenesis, tumor proliferation and tumor invasion. Jung et al. [22] found that IL1R2 was upregulated in mice breast cancer tissues, but downregulated in lymph nodes during tumor growth and suggested that different regulation of the expression of cytokines and cytokine-related genes resulted in a beneficial effect for tumor progression. Rückert et al. [26] validated for the first time an upregulation of IL1R2 in pancreatic cancer by means of qRT-PCR and deduced that IL1R2 might protect pancreatic cancers from apoptosis induced by the immune response. Laios et al. [19] believed that IL1R2 upregulation might play an important role in tumor angiogenesis in the recurrence of ovarian carcinomas and targeting IL1R2 may be an appropriate therapeutic strategy for inhibiting tumor angiogenesis. Su et al. [33] found that IL1R2 was constitutively overexpressed in an immortalized human uroepithelial cell line (HUC-1) which was chronically exposed to low doses of inorganic arsenite and its trivalent methylated metabolites in culture. Their research group [34] subsequently found that IL1R2 overexpression resulted in changes in cell morphology, actin rearrangement and promoted cell migration and suggested that IL1R2 overexpression was likely through activation of the pIL-1α pathway to enhance cell migration. These results showed the oncogenic potential of IL1R2 which was further corroborated by Leshem et al. [16] in a xenograft mouse model of human prostate cancer.
Considering to the above studies, we can summarize that IL1R2, as a decoy receptor of IL1, may be involved in tumorigenesis and tumor development through inflammation and/or immune regulation. But even more important, IL1R2 may have the oncogenic potential and be useful in tumor proliferation, angiogenesis and tumor invasion.
In this study, we constructed Lv-shIL1R2 and used these special lentiviruses to infect human osteosarcoma U-2 OS cells. We found that shIL1R2 could obviously inhibit the proliferation and colony formation of U-2 OS cells. And after treatment with Lv-shIL1R2, cells at G0/G1 phase decreased significantly, whereas cells at S and G2/M phases increased markedly. The similar change of cell cycle distribution was also reported in the previous published literature. Seo et al. [35] found S-G2/M phase cell cycle accumulation in canine osteosarcoma cell lines with fluoroquinolone antibiotics and suggested that fluoroquinolone-mediated inhibition of canine osteosarcoma cell lines might be related to S-G2/M cell cycle arrest. Tsui et al. [36] reported that A549 cells (a non-small cell lung carcinoma cell line) at G0/G1 phase was reduced with concomitant increases in both S and G2/M phases following flavonoid treatment and suggested that the inhibition of A549 cells growth with flavonoids could be attributed to the cell cycle arrest at S and G2/M phases. Therefore, we believed that the inhibition of proliferation and colony formation of U-2 OS cells with Lv-shIL1R2 treatment should be associated with the change of cell cycle distribution in the present study.
In conclusion, this study demonstrates for the first time that IL1R2 silencing inhibits the proliferation and colony formation of human osteosarcoma U-2 OS cells, and these should be associated with the blockage of S and G2/M phases. These results suggest that IL1R2 maybe have oncogenic potential and provide a new perspective for the treatment of osteosarcoma. Further studies are needed to investigate the possible molecular mechanisms of IL1R2 in osteosarcoma and illustrate whether shIL1R2 may be used as a potential therapeutic treatment for osteosarcoma patients.
References
Mirabello L, Troisi RJ, Savage SA. Osteosarcoma incidence and survival rates from 1973 to 2004: data from the surveillance, epidemiology, and end results program. Cancer. 2009;115:1531–43.
He JP, Hao Y, Wang XL, et al. Review of the molecular pathogenesis of osteosarcoma. Asian Pac J Cancer Prev. 2014;15:5967–76.
Kansara M, Teng MW, Smyth MJ, et al. Translational biology of osteosarcoma. Nat Rev Cancer. 2014;14:722–35.
Mirabello L, Pfeiffer R, Murphy G, et al. Height at diagnosis and birth-weight as risk factors for osteosarcoma. Cancer Causes Control. 2011;22:899–908.
Longhi A, Pasini A, Cicognani A, et al. Height as a risk factor for osteosarcoma. J Pediatr Hematol Oncol. 2005;27:314–8.
Ferrari S, Smeland S, Mercuri M, et al. Neoadjuvant chemotherapy with high-dose Ifosfamide, high-dose methotrexate, cisplatin, and doxorubicin for patients with localized osteosarcoma of the extremity: a joint study by the Italian and Scandinavian Sarcoma Groups. J Clin Oncol. 2005;23:8845–52.
Hegyi M, Semsei AF, Jakab Z, et al. Good prognosis of localized osteosarcoma in young patients treated with limb-salvage surgery and chemotherapy. Pediatr Blood Cancer. 2011;57:415–22.
Aponte-Tinao L, Ayerza MA, Muscolo DL, et al. Survival, recurrence, and function after epiphyseal preservation and allograft reconstruction in osteosarcoma of the knee. Clin Orthop Relat Res. 2014. http://springerlink.bibliotecabuap.elogim.com/article/10.1007%2Fs11999-014-4028-5.
Mialou V, Philip T, Kalifa C, et al. Metastatic osteosarcoma at diagnosis: prognostic factors and long- term outcome—the French pediatric experience. Cancer. 2005;104:1100–9.
Meyers PA, Healey JH, Chou AJ, et al. Addition of pamidronate to chemotherapy for the treatment of osteosarcoma. Cancer. 2011;117:1736–44.
Briccoli A, Rocca M, Salone M, et al. Resection of recurrent pulmonary metastases in patients with osteosarcoma. Cancer. 2005;104:1721–5.
Boraschi D, Tagliabue A. The interleukin-1 receptor family. Semin Immunol. 2013;25:394–407.
Peters VA, Joesting JJ, Freund GG. IL-1 receptor 2 (IL-1R2) and its role in immune regulation. Brain Behav Immun. 2013;32:1–8.
McMahan CJ, Slack JL, Mosley B, et al. A novel IL-1 receptor, cloned from B cells by mammalian expression, is expressed in many cell types. EMBO J. 1991;10:2821–32.
Ricote M, García-Tuñón I, Bethencourt FR, et al. Interleukin-1 (IL-1 alpha and IL-1beta) and its receptors (IL-1RI, IL-1RII, and IL-1Ra) in prostate carcinoma. Cancer. 2004;100:1388–96.
Leshem O, Madar S, Kogan-Sakin I, et al. TMPRSS2/ERG promotes epithelial to mesenchymal transition through the ZEB1/ZEB2 axis in a prostate cancer model. PLoS One. 2011;6:e21650.
Jones DZ, Ragin C, Kidd NC, et al. The impact of genetic variants in inflammatory-related genes on prostate cancer risk among men of African Descent: a case control study. Hered Cancer Clin Pract. 2013;11:19.
Kondera-Anasz Z, Mielczarek-Palacz A, Switała J. Significantly increased interleukin-1A and interleukin-1 soluble type II receptor levels in women with ovarian cancer. Ginekol Pol. 2003;74:761–6.
Laios A, O’Toole SA, Flavin R, et al. An integrative model for recurrence in ovarian cancer. Mol Cancer. 2008;7:8.
Keita M, AinMelk Y, Pelmus M, et al. Endometrioid ovarian cancer and endometriotic cells exhibit the same alteration in the expression of interleukin-1 receptor II: to a link between endometriosis and endometrioid ovarian cancer. J Obstet Gynaecol Res. 2011;37:99–107.
Pantschenko AG, Pushkar I, Anderson KH, et al. The interleukin-1 family of cytokines and receptors in human breast cancer: implications for tumor progression. Int J Oncol. 2003;23:269–84.
Jung MY, Kim SH, Cho D, et al. Analysis of the expression profiles of cytokines and cytokine- related genes during the progression of breast cancer growth in mice. Oncol Rep. 2009;22:1141–7.
Ma Y, Visser L, Roelofsen H, et al. Proteomics analysis of Hodgkin lymphoma: identification of new players involved in the cross-talk between HRS cells and infiltrating lymphocytes. Blood. 2008;111:2339–46.
Fennell DA, Myrand SP, Nguyen TS, et al. Association between gene expression profiles and clinical outcome of pemetrexed-based treatment in patients with advanced non-squamous non-small cell lung cancer: exploratory results from a phase II study. PLoS One. 2014;9:e107455.
Sun H, Chua MS, Yang D, et al. Antibody arrays identify potential diagnostic markers of hepatocellular carcinoma. Biomark Insights. 2008;3:1–18.
Rückert F, Dawelbait G, Winter C, et al. Examination of apoptosis signaling in pancreatic cancer by computational signal transduction analysis. PLoS One. 2010;5:e12243.
Stadnyk AW, Yeung MM, Yan SR. Human colon carcinomas constitutively express and shed type II IL-1 receptor, an IL-1 antagonist. Dig Dis Sci. 2003;48:1737–44.
Tömböl Z, Szabó PM, Molnár V, et al. Integrative molecular bioinformatics study of human adrenocortical tumors: microRNA, tissue-specific targetprediction, and pathway analysis. Endocr Relat Cancer. 2009;16:895–906.
Szabó DR, Baghy K, Szabó PM, et al. Antitumoral effects of 9-cis retinoic acid in adrenocortical cancer. Cell Mol Life Sci. 2014;71:917–32.
Chen P, Xi Q, Wang Q, et al. Downregulation of microRNA-100 correlates with tumor progression and poor prognosis in colorectal cancer. Med Oncol. 2014;31:235.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–8.
Mosmann T. Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods. 1983;65:55–63.
Su PF, Hu YJ, Ho IC, et al. Distinct gene expression profiles in immortalized human urothelial cells exposed to inorganic arsenite and itsmethylated trivalent metabolites. Environ Health Perspect. 2006;114:394–403.
Chang SY, Su PF, Lee TC. Ectopic expression of interleukin-1 receptor type II enhances cell migration through activation of the pre-interleukin 1 alpha pathway. Cytokine. 2009;45:32–8.
Seo KW, Holt R, Jung YS, et al. Fluoroquinolone-mediated inhibition of cell growth, S-G2/M cell cycle arrest, and apoptosis in canine osteosarcoma cell lines. PLoS One. 2012;7:e42960.
Tsui KC, Chiang TH, Wang JS, et al. Flavonoids from Gynostemma pentaphyllum Exhibit Differential Induction of Cell Cycle Arrest in H460 and A549 Cancer Cells. Molecules. 2014;19:17663–81.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
An expression of concern to this article can be found online at http://dx.doi.org/10.1007/s12032-018-1177-5.
Rights and permissions
About this article
Cite this article
Liu, X., Min, L., Duan, H. et al. Short hairpin RNA (shRNA) of type 2 interleukin-1 receptor (IL1R2) inhibits the proliferation of human osteosarcoma U-2 OS cells. Med Oncol 32, 364 (2015). https://doi.org/10.1007/s12032-014-0364-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0364-2