Abstract
Central nervous system (CNS) relapse continues to be a frequent and usually fatal complication in patients with diffuse large B cell lymphoma (DLBCL). Multiple factors identify the possibility of relapse and justify neurological prophylaxis; however, most of these have not been confirmed. Thus, the use of prophylaxis has not been defined. From 1988 to 2008, 3,258 patients with DLBCL with higher clinical risks and multiple extranodal involvement that have been treated with standard anthracycline-based chemotherapy: CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone) or CHOP-R (CHOP plus rituximab) and that achieve complete response were retrospectively analyzed to assess the efficacy of CNS prophylaxis. One thousand five patients received different schedules for CNS prophylaxis, and 2,253 patients did not receive CNS prophylaxis. CNS relapse was similar in patients who receive prophylaxis (6 %) compared to patients who did not receive prophylaxis (5.9 %). Overall survival of patients who either receive or did not receive prophylaxis was not statistically significant: 49 % versus 53 % (p = 0.802). Thus, it seems that CNS prophylaxis did not improve outcome in this special setting of patients, and no prognostic factors to predict the presence of CNS relapse were identified. It is evident that multicentric studies are necessary to define the role of prophylaxis in order to prevent CNS relapse and that the therapeutic procedure will be carefully revised.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Central nervous system (CNS) relapse in patients with diffuse large B cell lymphoma (DLBCL) has been reported to be between 1.1 and 10.4 %. Although relatively uncommon, it is a serious and mostly fatal complication [1–7]. Multiple attempts have been performed to identify the patients who are considered at risk and who should receive prophylaxis [8–16]. However, no uniform criteria have been developed, and the efficacy of different forms of CNS prophylaxis has never been formally demonstrated. Recently, the use of systemic therapy with higher doses of methotrexate (MTX) or cytosine arabinoside, or with the addition of rituximab to standard chemotherapy, has been advocated as useful to prevent CNS relapse, but contradictory results have been reported [17–20]. Controlled clinical trials are clinically and ethically difficult to prevent, and for this reason, retrospective analysis has been performed to answer this problem. Although multiple therapeutic attempts have been employed to prevent CNS relapse, most reports included only one type of prophylaxis [3, 18, 21, 22], and comparison between the different types is not available. During the last 25 years, we employed different approaches of prophylactic measures. Thus, we revised our experience in this field to evaluate the risk factors in a homogenous group of patients with DLBCL treated with cyclophosphamide, doxorubicin, vincristine and prednisone (CHOP) or CHOP adding rituximab (R-CHOP), with a large follow-up to define whether the CNS relapse can influence overall survival (OS) in patients with DLBCL and poor prognostic factors.
Patients and methods
Patients with proven diagnosis of DLBCL according to WHO classification, without evidence of CNS involvement at diagnosis, who were treated in our institution from 1988 to 2010, were included in the present analysis. Burkitt’s lymphoma, lymphoblastic lymphoma, human immunodeficiency virus (HIV)-associated lymphoma and lymphoma as second neoplasm were excluded.
For all patients, initial staging work-up including clinical examination, complete blood counts, serum chemistry, serum determination of lactic dehydrogenase (LDH) and beta 2 microglobulin (B2 M), HIV, hepatitis B and C tests was performed.
Computed tomography of the thorax, abdomen and pelvis, as well as aspirate and biopsy tests of the bone marrow, was also conducted. A lumbar puncture (LP) was performed in all cases with breast, testicle, kidney and bone marrow involvement [23, 24]. Although other extranodal presentations were previously mentioned at risk of CNS relapse as lymphoma manifestation in the head, neck, nasal and bone, in our experience, it is very rare, and LP was not routinely performed in these patients. Patients with positive LP for malignant cells were excluded for analysis. If the patients showed clinical manifestations of CNS involvement, tomography and/or magnetic resonance imaging was performed. A positive result excludes them from the study. All patients were treated with six cycles at standard doses of CHOP or R-CHOP. Patients with nodal bulky disease (tumor mass >10 cm) received adjuvant radiotherapy [25]. Only patients that achieved complete response after chemotherapy were considered candidates for CNS prophylaxis, which began 6–8 weeks after chemotherapy.
Administration of CNS prophylaxis was upon the discretion of the treating physician, who presents the case in an internal round-table, and the total group decides whether the patient received prophylaxis; in all cases LP was performed prior to prophylaxis.
During this time different prophylaxis therapies were administered
Cranial radiotherapy was given along with whole-brain radiation therapy and was administered at a dose of 2.5 Gy in 25 treatment sessions of 0.1 Gy each.
Intrathecal methotrexate (IT MTX) is another therapy administered. Fifteen milligram of MTX plus 100 mg of hydrocortisone was given every 5 days for six doses followed by maintenance therapy, and of the same single dose every 3 months for 1 year (total doses: 10).
A standard dose of 40 mg combined IT MTX and cytosine arabinoside and 100 mg of hydrocortisone were administered at the same schedule mentioned earlier.
On the other hand, 4 g/m2 of high-dose MTX was given every 14 days, for four doses (total dose: 16 g/m2), followed by folinic acid rescue.
To diagnose CNS relapse, patients with symptoms and/or sings of neurological involvement were studied using LP, cranial tomography and magnetic resonance imaging. The diagnosis was based on the detection of lymphoma cells in the spinal fluid and radiological findings. No brain biopsy was performed.
When CNS relapse was documented, the patients were treated with different schedules:
-
Patients with brain relapse and who received radiotherapy for prophylaxis were treated with high-dose MTX: 4 g/m2 with folinic acid rescue on Days 1 and 28, and cytosine arabinoside 2 g/m2 every 12 h for eight doses (total dose: 12 g/m2) on Days 15 and 45.
-
Patients with meningeal relapse were treated with three drugs: MTX, cytosine arabinoside and hydrocortisone with the aforementioned doses every 4 days until clearance of the spinal fluid. Maintenance was continued every 28 days until progression, death or toxicity.
Statistical analysis
The primary endpoint was time to CNS relapse, which is defined as the time of CNS involvement and the end of chemotherapy in patients who achieved CR. The second endpoint was overall survival after CNS relapse until death from any cause. CNS relapse and overall survival were estimated according to the method of Kaplan and Meier. A 5-year CNS relapse rate together with 95 % confidence interval (CI) was reported. Univariate analysis was carried out by means of Cox regression, and log-rank test was performed to evaluate the risk of CNS relapse in terms of these factors. All factors with p values less than 0.10 were included in the multivariate analysis in order to identify prognostic factors for CNS relapse using the Cox regression model.
Relapse-free survival (RFS) was defined as time from diagnosis to relapse, including both CNS and non-CNS relapse. OS was defined as the time from diagnosis to the date of death or date of last follow-up (December 2011).
Results
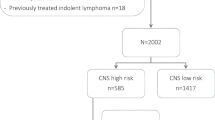
The study was performed in a single center, the Oncology Hospital, National Medical Center of the National Institute of Social Security, which is an tertiary reference center and has a coverage of 36.000.000 people. Patients diagnosed with DLBCL between 1988 and 2008 were included in the study. The median time of follow-up was 13.6 years (range 5–19.3 years). During this time, 7,685 patients were diagnosed with malignant lymphoma. In order to avoid the presence of bias by including different histological types, we considered only patients with DLBCL histology (3,285 cases).
Table 1 shows the clinical and laboratory characteristics. For various reasons, we received patients with advanced disease; patients in the early stages are rare, and most patients have adverse prognostic factors and have bulky disease, higher clinical risks, poor performance status, higher levels of LDH and beta 2-microglobulin and multiple extranodal infiltration.
One hundred and eighty-eight patients had CNS relapse. The median time for CNS relapse was 3.0–32.4 months (median 11.6 months). Thirty-five patients had parenchymal relapse, 50 had a meningeal relapse, and 102 showed relapse in both sites. Table 2 shows the CNS relapse pattern according to the type of CNS prophylaxis. No statistical differences were observed upon comparing the different types of prophylaxis and the nonuse of CNS prophylaxis.
By univariate analysis, no increased risk for CNS relapse was associated with different risk factors that were analyzed (Table 3). Thus, multivariate analysis did not show any statistical differences (data not shown). Sixty-five patients achieved a complete response (35 %), but 30 patients (45 %) showed disseminated relapse 6–21 months after CNS relapse and died, secondary to tumor progression. One hundred twenty-two patients did not respond to treatment and died, secondary to neurological infiltration. At 5 years, OS of patients with CNS relapse was 19 %.
In an intent to analyze the impact of CNS relapse on the outcome of RFS and OS, we reviewed the patients who did not receive prophylaxis and compared them with patients who received prophylaxis to CNS. Actuarial curves at 5 years showed that OS was 53 % in patients who did not receive compared to 49 % in patients who received prophylaxis, which is not statistically significant (p = 0.802).
The study was approved by the Ethical and Scientific Committee of our institution, and all patients gave informed consent to receive or not to receive CNS prophylaxis (Table 4).
Discussion
Although the problem of CNS recurrence in patients with aggressive lymphoma is well recognized, it is still unclear which patients are at risk of the event, and for this reason, a better prophylaxis to avoid the presence of CNS relapse remains undefined. The incidence of CNS relapse has been reported to be from 0.9 to 35 %, depending on histology subtypes presented in the study population. In DLBCL it has been reported to be ±5 % in patients who did not receive prophylaxis, but until now there is no information about the risk of patients who received prophylaxis.
Multiple studies have been performed to identify the prognostic factors to predict the risk of CNS relapse which include higher clinical risks, advanced stage, higher levels of serum LDH, extranodal involvement with some specific organs, such as testicle, breast, sinuses, kidney, bone marrow involvement, and the presence of bulky disease [8–16], but none of these risk factors have been confirmed. Attempts have been performed to develop risk models and to increase the possibility of identifying the risk of CNS relapse, but again, independent studies have not been able to confirm the initial results [8–11, 19].
In the present study, we present a larger series of patients with uniform criteria: diagnosis of DLBCL, patients who treated with standard anthracycline-based chemotherapy and in the last years introduced monoclonal antibodies, uniform clinical risks, advanced stages, presence of bulky disease and multiple extranodal involvement, including bone marrow infiltration; however, in our results, neither of the mentioned prognostic factors influenced the presence of CNS relapse, and the most important is it did not influence OS when comparing patients who received CNS prophylaxis and those who did not.
On the other hand, different types of prophylaxis have been recommended based on the experience observed in the reports. No consensus exists about the better prophylactic measures. In our experience we employed different prophylaxis, and no clear differences were observed between the different schedules. The addition of rituximab to anthracycline-based chemotherapy has been suggested to reduce the number of CNS relapse [14, 19, 20], but other studies did not confirm these findings [21, 22]. In our study, the addition of rituximab did not influence the presence of CNS relapse.
Extranodal involvement, especially in some organs, has been associated with a higher risk of developing CNS relapse; however, in our study the primary extranodal presentation of breast, testicle or presence of bulky disease did not confirm these findings [23–25].
The most important finding is that the number of CNS relapse was similar in patients who received any prophylactic measure compared with patients who did not receive CNS prophylaxis. The main problem is to define the origin of tumor cells that are the cause of CNS infiltration. Taking into consideration, the short time to CNS relapse is probably that the malignant cells are present in CNS upon diagnosis and are not detected using conventional methods and did not produce clinical symptoms because the tumor mass is small. However, some malignant cells can be resistant to chemotherapy, including rituximab, and can migrate to the CNS system to produce neurological relapse. Thus, the use of higher doses of MTX and cytosine arabinoside should be the preferred prophylaxis.
The aim is to detect the tumor cells when the tumor mass is small, in order to have a better chance to eradicate these tumor cells. Hedge et al. [26] found that flow cytometry can detect occult malignant cells in CNS, however, in these study they found that in 22 % of patients with DLBCL a with negative search using conventional methods to detect tumor cells in the spinal fluid, flow cytometry positively detected malignant cell. Although these patients received CNS prophylaxis, neurological relapse was observed in five patients (45 %). Thus, it has been suggested that differences in results will be secondary to different criteria and different panels, and recently, it has been suggested that flow cytometry will not be considered the standard diagnostic test; controlled clinical trials are necessary to define the role of this laboratory test [27].
The presence of CNS relapse remains to be a worst clinical feature because remission is rare and <10 % of patients are alive at 1 year [28–30]. However, the presence of CNS relapse did not influence the OS of the entire group when compared to patients who did not receive prophylaxis. It appears that some patients have the propensity to relapse in extranodal sites; thus, although CNS relapse can be avoided, relapse in another extranodal site is present, and as is common in this type of relapse, second response is rare and most patients die, secondary to tumor progression. Thus, it is evident that there is urgency to define the patients who are present with a trend to develop a relapse in any extranodal site in order to prevent the relapse and modify the current treatment in this type of patients. Thus, if CNS relapse can be diminished with the use of prophylaxis, other extranodal relapses cannot be avoided and the patients, ultimately, relapse, with a low opportunity to achieve response, leading to death due to tumor progression.
We conclude that in our experience with a larger number of patients and with a longer follow-up period, the use of CNS prophylaxis, as employed actually, did not prevent CNS relapse and that the use of prophylaxis did not affect OS in patients with high clinical risks and poor prognostic factors.
References
Siegal T, Goldschmid T. CNS prophylaxis in diffuse large B-cell lymphoma. If, when, how and for whom. Blood Rev. 2011;26:97–106.
McMillan A. Central nervous system direct preventive therapy in adults with lymphoma. Br J Haematol. 2005;131:13–21.
Franklin JC, Firlay J. Leukemia and lymphomas: treatment and prophylaxis of the central nervous system. Curr Treat Options Neurol. 2006;8:335–44.
Kridel R, Dietrich PY. Prevention of CNS relapse in diffuse large B-cell lymphoma. Lancet Oncol. 2011;12:1258–66.
Hill QA, Owen RG. CNS prophylaxis in lymphoma: who to target and therapy to use. Blood Rev. 2006;20:319–32.
Cheung CW, Burton C, Smith P, Lich DC, Hoskin PJ, Ardeshna KM. Central nervous system chemoprophylaxis in non-Hodgkin’s lymphoma. Br J Haematol. 2005;131:193–200.
Bernstein SH, Unger JM, LeBlanc M, Friedberg J, Miller TP, Fisher RI. Natural history of CNS relapse in patients with aggressive non-Hodgkin’s lymphoma. J Clin Oncol. 2008;27:114–9.
Haioun C, Besson C, Lepage C, Thieblemont C, Simon D, Rose C, et al. Incidence and risk factors of central nervous system relapse in histologically aggressive non-Hodgkin’s lymphoma uniformly treated and receiving intrathecal central nervous system prophylaxis. Ann Oncol. 2000;11:685–90.
Shimazu Y, Notohara K, Veda Y. Diffuse large B-cell lymphoma with central nervous system relapse. Prognosis and risk factors according to retrospective analysis from an single-center experience. Int J Hematol. 2009;89:577–83.
Chihara D, Oki Y, Matsuo K, Onoda H, Taji H, Yamamoto K, et al. Incidence and risk-factors for central nervous system relapse in patients with diffuse large B-cell lymphoma. Leuk Lymphoma. 2011;52:2270–5.
Boehme V, Zeynalova S, Kloess M, Loefler M, Kaiser U, Pfreudschuh M, et al. Incidence and risk factors of central nervous system recurrence in aggressive lymphoma. A survey of 1,693 patients treated in protocols of the German High-grade non-Hodgkin’s Lymphoma Study Group. Ann Oncol. 2007;18:149–57.
Kim SJ, Oh SY, Kim JS, Kim H, Lee GW, Won JH, et al. Secondary central nervous system involvement in patients with diffuse large B-cell lymphoma. Ann Hematol. 2011;90:539–46.
Bollem ELEM, Brouwer RE, Hamers S, Hermans J, Kluis M, Sankatsing RVA. Central nervous system non-Hodgkin’s lymphoma. Arch Neurol. 1997;54:854–9.
Boehme V, Schimtz N, Zeynalova S, Loeffler M, Pfreudschuh M. CNS events in elderly patients with aggressive lymphoma treated with modern chemotherapy (CHOP-14) with or without rituximab. Blood. 2009;113:3896–902.
Hollender A, Kualoy S, Nome E, Skovlunde-Lote K, Holte H. Central nervous system involving following diagnosis of non-Hodgkin’s lymphoma. Ann Oncol. 2002;13:1099–107.
Tilly H, Lepage E, Coiffier B, et al. Intensive conventional chemotherapy (ACVBP) regimen compared with standard CHOP for poor prognosis aggressive non-Hodgkin’s lymphoma. Blood. 2003;102:4283–9.
Recher C, Coiffier B, Haioun C, et al. Intensified chemotherapy with ACVBP plus rituximab versus standard CHOP plus rituximab for the treatment of diffuse large B-cell lymphoma. Lancet. 2011;378:1858–67.
Abramson JS, Hellman M, Barnes JA, Hammerman P, Toomey C, Takuvian T, et al. Intravenous methotrexate as central nervous system (CNS) prophylaxis is associated with a low-risk of CNS recurrence in high-risk patients with diffuse large B-cell lymphoma. Cancer. 2010;116:4283–90.
Mitrovic Z, Bast M, Bierman PI, Bociek RG, Vose JM, Chan WC et al. The addition of rituximab reduces the incidence of secondary central nervous system involvement in patients with diffuse large B-cell lymphoma. Br j Haematol. 2012.
Feugier P, Virion JM, Tilly H, Haioun C, Marit G, Macro M, et al. Incidence and risk for central nervous system recurrence in elderly patients with diffuse large B-cell lymphoma. Influence of rituximab. Ann Oncol. 2004;15:129–33.
Tai WM, Chune J, Tang PL, Koo YY, Hou X, Tay KW, et al. Central nervous system relapse in diffuse large B-cell lymphoma (DLBCL) Pre and post-rituximab. Ann Hematol. 2011;90:809–18.
Arkenau HT, Chont G, Cunningham D, Watkins D, Agarwai R, Sirohi B, et al. The role of intrathecal chemotherapy prophylaxis in patients with diffuse large B-cell lymphoma. Ann Oncol. 2007;18:541–8.
Avilés A, Castañeda C, Neri N, Cleto S, Nambo MJ. Rituximab and dose-dense therapy in primary breast lymphoma. Haematologica. 2007;92:1147–8.
Avilés A, Neri N, Huerta-Guzmán J, et al. Testicular lymphoma. Organ-specific treatment did not improve outcome. Oncology. 2004;67:211–4.
Avilés A, Fernández R, Pérez F, et al. Adjuvant radiotherapy in stage IV diffuse large B-cell lymphoma improve outcome. Leuk Lymphoma. 2004;45:385–9.
Hedge UL, Filie A, Little RF, Janik JE, Grant JN, Steinbergs M, et al. High-incidence of occult leptomeningeal disease detected by flow cytometry in newly diagnosed aggressive B-cell lymphomas at risk for central nervous system involvement. Blood. 2005;105:496–502.
Ahluwalid MS, Wallace PB, Peereboom DM. Flow-cytometry as a diagnostic tool in lymphomatous or leukemia meningitis. Cancer. 2012;118:1747–53.
Tanimoto T, Kusumi E, Hosuda K, et al. CNC prophylaxis in diffuse large B-cell lymphoma. Lancet. 2012;379:1485–6. (Letter).
Jabbour E, O’Brien S, Garcia-Manero G, Fernadoli A, Ravandi F, Cabanillas M, et al. Neurologic complications associated with intrathecal liposomal cytarabine given prophylactically in combination with high-dose methotrexate and cytarabine to patients with acute leucemia. Blood. 2007;109:3214–8.
Perez-Larray JG, Palma JA, Carmona-Iragus M, Fernández-Torron R, Irimiz P, Rodríguez-Otero P, et al. Neurologic complications of intrathecal liposomal cytarabine administered prophylactically to patients with non-Hodgkin’s lymphoma. J Neurooncol. 2011;103:603–9.
Acknowledgments
The study was performed with the owner resources of the Mexican Institute of Social Security and did not receive any financial support.
Conflict of interest
The authors disclose no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Avilés, A., Jesús Nambo, M. & Neri, N. Central nervous system prophylaxis in patients with aggressive diffuse large B cell lymphoma: An analysis of 3,258 patients in a single center. Med Oncol 30, 520 (2013). https://doi.org/10.1007/s12032-013-0520-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-013-0520-0