Abstract
Central nervous system (CNS)-directed prophylactic intrathecal (IT) therapy is indicated in patients with Burkitt and acute lymphoblastic lymphoma. Its role in diffuse large B cell lymphoma (DLBCL), a heterogeneous subtype, is less well defined. While addition of rituximab to standard cyclophosphamide–hydroxydaunorubicin–oncovin–prednisone (CHOP) chemotherapy (R-CHOP) has improved the outcomes of DLBCL patients, its role in reducing CNS relapse is unclear. We aim to (1) evaluate the clinical risk factors predictive of CNS relapse, (2) the role of rituximab in influencing CNS relapse, and (3) role of intrathecal prophylaxis. Four hundred ninety-nine patients with DLBCL from 2000 to 2008 were included (CHOP 179 vs. R-CHOP 320). IT prophylaxis was administered to 82 patients based on our institution’s guidelines. Baseline characteristics between CHOP- and R-CHOP-treated patients were similar. Although R-CHOP significantly increased the complete remission rate from 71% to 81% (P < 0.01), CNS relapse rates remained unchanged (R-CHOP 6% vs. CHOP 5.1%). On multivariate analysis, poor performance status (Eastern Cooperative Oncology Group >1; hazard ratio (HR) = 2.01, 95% confidence interval (CI) 1.29–3.14), failure to attain remission (non-complete response (CR) vs. CR: HR = 2.39, 95% CI = 1.03 to 5.51), testicular (HR = 6.67, 95% CI = 1.62 to 27.53), kidney (HR = 20.14, 95% CI = 5.23 to 77.46), and breast involvement (HR = 6.14, 95% CI = 1.61 to 23.37) were each independently predictive of CNS relapse. Use of IT prophylaxis did not appear to decrease CNS relapse. Median survival after CNS relapse was 3.2 months. CNS relapse, a fatal event, remains a challenge in R-CHOP-treated patients. IT prophylaxis may not be sufficient to reduce CNS relapse, and strategies including systemic agents with high CNS penetration should be evaluated in high-risk patients identified in this study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of isolated central nervous system (CNS) relapse in patients with diffuse large B cell lymphoma (DLBCL) has been reported to be between 1.1% and 10.4% [1–8]. While relatively uncommon, it is almost always fatal. Patients at risk of CNS recurrence include those with advanced stage of disease, elevated lactate dehydrogenase (LDH), and involvement of extranodal sites such as bone marrow and testes [1–6]. To reduce the risk of CNS recurrences in these patients, most authorities, such as the British Columbia Cancer Agency and the National Cancer Comprehensive Network, advocate routine intrathecal (IT) prophylaxis. Nonetheless, the benefit of intrathecal prophylaxis in preventing CNS disease has been questioned in recent years [3]. While the addition of rituximab, a chimeric anti-CD 20 monoclonal antibody to cyclophosphamide–hydroxydaunorubicin–oncovin–prednisone (CHOP) chemotherapy (R-CHOP), has certainly improved the survival of patients with DLBCL [9–13], its efficacy in preventing CNS relapse though remains controversial.
This study aimed to evaluate the incidence of CNS relapse, its natural history, and risk factors in a homogenous group of patients with DLBCL treated with either CHOP or R-CHOP chemotherapy. We also aim to evaluate the efficacy of rituximab and intrathecal prophylaxis in reducing CNS recurrences.
Methods
Patients
Patients with DLBCL without CNS disease at diagnosis treated in our institution from 2000 to 2008 were included in this retrospective study. Four hundred ninety-nine consecutive patients with DLBCL in our electronic clinical database who received at least one cycle of CHOP/R-CHOP chemotherapy with curative intent were included. Patients with DLBCL who received non-curative treatment or who died soon after diagnosis were excluded. The Ann Arbor staging system was used to stage all patients prior to the commencement of treatment. This included history; physical examination; standard laboratory tests; computed tomography scans of the chest, abdomen, pelvis, and other relevant sites; and bone marrow biopsy. Both the staging investigations and histology were centrally reviewed. Following completion of CHOP or R-CHOP chemotherapy, patients were reviewed every three to four monthly in the first 3 years. In the fourth and fifth year, they were reviewed six monthly. Thereafter, patients were seen yearly till the tenth follow-up year. Out of 364 surviving patients, 40 were lost to follow-up.
Detection of CNS disease
CNS disease at diagnosis or CNS relapse is based on either radiologic evidence, cytologic proof, or clinical presentation of CNS involvement. At the discretion of the treating physician, cerebrospinal fluid (CSF) analysis was also performed in patients who were deemed at high risk of CNS relapse, defined in our institution as those with >1 extranodal sites of involvement and specific sites of involvement (orbit, sinus/posterior nasal space, breast, testicular, bone, and bone marrow). Of the 203 patients deemed at risk of CNS relapse as defined, CSF analysis was eventually performed in 82 patients.
Intrathecal prophylaxis
At the discretion of the treating physician and patient preference, prophylactic intrathecal prophylaxis was administered to those who were deemed at high risk of CNS relapse, as previously defined. Thus, among the 203 patients deemed at high risk of CNS relapse (i.e., >1 extranodal sites of involvement, or involvement of orbit, sinus/posterior nasal space, breast, testicular, or bone marrow), 82 had CSF analysis and subsequent IT prophylaxis. Eighty-two patients received a median of four intrathecal methotrexate 12 mg given on the same day as intravenous chemotherapy.
Statistical analysis
Clinical characteristics were compared between patients who received CHOP and those with R-CHOP chemotherapy using Fisher’s exact test in terms of age, gender, Eastern Cooperative Oncology Group (ECOG), LDH, number of extranodal sites involved, testicular, status of bone marrow involvement, kidney, sinus, post-nasal space, liver, breast, IT prophylaxis, B symptoms, stage, international prognostic index (IPI), and response to treatment.
Time to CNS relapse was defined as time from diagnosis to CNS relapse, if no CNS relapse, to the date of death or date of last follow-up. Only the CNS relapse was considered as events, and the rest were censored when calculating cumulative CNS relapse rate using Kaplan–Meier survival curve. Two-year CNS relapse rate together with 95% confidence interval (CI) were reported. Univariate analyses were carried out by means of Cox regression, and log-rank test was performed to evaluate the effects of different risk factors on CNS relapse in terms of these factors. All factors with P values less than 0.10 were included in the multivariate analysis to identify prognostic factors for CNS relapse using Cox regression model. The strength of prognostic factors was estimated by determining hazard ratios (HR) and the corresponding 95% CIs.
CNS relapse-free survival was calculated from date of chemotherapy to date of documented CNS relapse or death; patients alive without progressive/relapsed disease were censored on the date of last follow-up visit. Time to relapse (TTS) was defined as time from diagnosis to relapse including both CNS and non-CNS relapse. Overall survival (OS) was defined as time from diagnosis to the date of death or date of last follow-up. Kaplan–Meier survival curves were also performed to estimate TTS and OS of patients with CNS relapse and those with non-CNS relapse. The equality of TTS or OS between these two groups of patients was assessed using log-rank test. Similar tests were done to compare the OS between patients developing CNS relapse after diagnosis and another 18 patients with CNS disease at diagnosis. All analyses were carried out using STATA version 9.0 (STATA Corporation, College Station, TX, USA).
Results
Patient characteristics
A total of 499 patients without CNS disease at diagnosis were included in the analysis; 179 (36%) received CHOP chemotherapy and 320 (64%) received R-CHOP chemotherapy. Clinical characteristics of patients who received CHOP or R-CHOP chemotherapy were listed in Table 1. The clinical characteristics were not significantly different between the two treatment arms except for a B symptoms (CHOP 34% vs. R-CHOP 23%; P = 0.012) and complete response (CR) rates (CHOP 71% vs. R-CHOP 81%; P < 0.001). Clinical characteristics of patients who received IT prophylaxis were listed separately in Table 2. As shown in the table, patients who received prophylactic IT generally had more advanced stages of disease and more extranodal involvement.
CNS relapse and risk factors
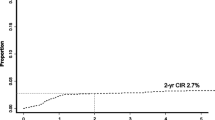
The median duration of follow-up for the patients who received CHOP and R-CHOP were 5.45 and 2.70 years, respectively. The 2-year cumulative incidences of CNS relapse were 5.1% (95% CI = 2.6% to 9.9%) for patients with CHOP and 6.0% (95% CI = 3.8% to 9.4%) for patients with R-CHOP. The median time from diagnosis to CNS relapse was not achieved for both patients with CHOP or R-CHOP (Fig. 1). Time to CNS relapse was not significantly different the two treatment groups (P = 0.818).
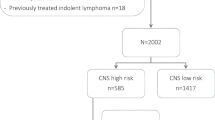
The incidence of CNS relapse among patients treated with intrathecal prophylaxis was 11% (9 out of 82), compared to 5% (21 out of 417) among those who did not receive any IT prophylaxis. Patients with more than one extranodal site of involvement and site-specific involvement comprising of orbit, sinus/posterior nasal space, breast, testicular, bone, and bone marrow were deemed at an increased risk of CNS relapse. We identified 203 patients with one or more mentioned features. Eighty-two patients received intrathecal prophylaxis together with systemic chemotherapy while 121 patients received only systemic chemotherapy. The baseline characteristics are shown in Table 3. The Kaplan–Meier estimate of CNS relapse-free survival between these two groups of patients is shown in Fig. 2. Addition of intrathecal prophylaxis did not confer an additional benefit (P = 0.981)
For the entire cohort of patients, the factors that increased the risk of CNS relapse included ECOG performance status >1, elevated LDH, >1 extranodal sites of involvement, testicular involvement, bone marrow involvement, kidney involvement, breast involvement, presence of B symptoms, stage IV at diagnosis, and failure to attain complete remission (Table 4).
On Cox regression, ECOG performance >1 (HR = 2.01, 95% CI 1.29–3.14), failure to attain remission (non-CR vs. CR: HR = 2.39, 95% CI = 1.03 to 5.51), testicular (HR = 6.67, 95% CI = 1.62 to 27.53), kidney (HR = 20.14, 95% CI = 5.23 to 77.46), and breast involvement (HR = 6.14, 95% CI = 1.61 to 23.37) were each independently predictive of CNS relapse (Table 5).
We also attempted to evaluate the risk factors for CNS relapse among patients treated with R-CHOP alone. On univariate analysis, LDH > 2ULN, ECOG performance status >1, >1 extranodal sites of involvement, bone marrow involvement, kidney involvement, liver involvement, B symptoms, stage IV disease at presentation, IPI score ≥3, and failure to attain CR were each associated with increased risk of CNS relapse (Table 4). Kidney involvement, ECOG performance status >1, and failure to attain complete remission were each independently predictive of CNS relapse on multivariate analysis (Table 5).
The median time to CNS relapse among 30 patients with CNS relapse was 0.56 year (range, 0.16 to 3.77 years). Among the 76 patients with non-CNS relapse, the median time to relapse was 0.93 year (range, 0.13 to 6.44 years). This difference is statistically significant on log-rank test (P = 0.009).
Overall survival of patients with CNS relapse
The median overall survival for the 30 patients with CNS relapse was 1.08 years, compared to 1.38 years for the 76 patients with non-CNS relapse (P = 0.3590). The median survival and estimated 2-year survival rate for these 30 patients following a diagnosis of CNS recurrence were 0.27 year and 20%, respectively. Compared to these 30 patients with CNS recurrence, the median OS of the 18 patients with CNS disease at diagnosis was 2.29 years (P = 0.0570; Fig. 3).
Discussion
While rituximab undoubtedly improves the outcome of patients with DLBCL [9, 10, 13], its impact in reducing CNS relapse in this group of patients remains uncertain. The RICOVER-60 trial represents the largest prospective study available evaluating this question. This trial primarily investigated the benefits of adding rituximab to CHOP-14 chemotherapy and the optimal number treatment cycles (six or eight) in 1,217 elderly patients. In the trial, the authors reported a modest though statistical significant reduction in the estimated 2-year incidence of CNS events from 6.9% in patients treated with CHOP to 4.1% in patients treated with R-CHOP-14 (P = 0.043). Nonetheless, since almost 20% of the patients in the study population did not have DLBCL, the true effect of rituximab in this group of patients remains unknown [3].
Several retrospective series have also attempted to clarify this matter. For instance, in a recent study, Shimazu et al. [4] reported a protective effect of rituximab against CNS relapse in 403 patients with DLBCL (more than half had stage ¾ disease and more than 30% had >1 extranodal site of involvement; HR 0.48, P = 0.027). In another study involving 435 patients with DLBCL from the British Columbia, Villa et al. reported a trend toward reduced likelihood of CNS relapse in R-CHOP-treated patients (3-year risk 9.7% vs. 6.4, P = 0.085). However, the GELA group [10] found similar rates of CNS recurrence in 399 elderly patients treated with or without rituximab. Likewise, Yamamoto and colleagues in a study involving 375 consecutive patients with DLBCL also found that the use of rituximab did not have an impact on CNS recurrence [14]. In our study of 499 patients with DLBCL, we also did not find any significant difference in the CNS recurrence rates between patients who received CHOP chemotherapy and R-CHOP chemotherapy. Taken together, these data suggest that the impact of rituximab in reducing CNS events is modest, at best. Clearly better strategies to prevent CNS recurrences are needed.
Most centers routinely administer prophylactic intrathecal chemotherapy to patients with high-risk features such as bone marrow, testicular, and sinus involvement. However, there is no randomized study to show that this approach is effective in reducing CNS relapses. On the contrary, there is emerging evidence to suggest that IT prophylaxis might not confer a protective effect on the incidence of CNS recurrence [1–3, 7]. In our study, 203 patients were deemed at high risk of CNS relapse, defined as those with >1 extranodal sites of involvement and specific sites of involvement (orbit, sinus/posterior nasal space, breast, testicular, bone, and bone marrow). Among them, prophylactic intrathecal prophylaxis was administered at the discretion of the treating physician and accordance to patient’s preference. Among the 203 patients, 82 patients eventually had CSF analysis and subsequent IT prophylaxis. This provided us an opportunity to compare the rates of CSF rates between those who did not have IT prophylaxis (n = 121) with those who did (n = 82). The corresponding rates of CNS relapse were 8.3% (10 out of 121) vs. 11% (9 out of 82), respectively (P = 0.52). Thus, addition of intrathecal therapy certainly did not seem to improve the CNS recurrence rate among patients thought to potentially benefit from this treatment (Fig. 2). Considering the uncertain efficacy of intrathecal prophylaxis and the physical discomfort as well as inconvenience associated with its administration, a randomized trial to address this question is timely.
Consistent with the Southwest Oncology Group study [7], ours findings show that CNS recurrence typically occur either during chemotherapy or shortly after its completion. The median time from diagnosis to CNS relapse was 8.4 months and 77% of the recurrences occur within the first year. The early relapse observed likely reflects the presence of sub-clinical CNS involvement at diagnosis and inadequate CNS-directed treatment. The need to improve on the pickup rate is further exemplified by the observation that patients with CNS involvement at diagnosis in actual fact had a better median OS of 2.29 years compared to 1.08 years among those with CNS relapse (Fig. 2; P = 0.057). It is conceivable that more intensive upfront CNS-directed therapy resulted in improved survival in patients with CNS involvement at diagnosis. There were 18 patients with CNS disease at diagnosis, whom 17 received either intensive intrathecal therapy or high-dose intravenous methotrexate.
Of relevance, Hegde and colleagues from the National Cancer Institute found CSF analysis by flow cytometry to be significantly more sensitive than routine cytology in identifying lymphomatous CNS involvement [15]. Among 51 newly diagnosed lymphoma patients at risk of CNS relapse, flow cytometry detected 11 (22%) cases of occult CSF involvement compared to only one by cytology (P = 0.002). Of these 11 patients, nine received aggressive intrathecal therapy. Even so, five (45%) patients relapsed in the CNS and died, suggesting that intrathecal therapy alone might not be sufficient in the treatment of CNS involvement. Interestingly, in another study from France evaluating the effectiveness of an intensive conventional chemotherapy (doxorubicin–cyclophosphamide–vindesine–bleomycin–prednisone (ACVBP) regimen) compared to standard CHOP in patients with poor-prognosis aggressive non-Hodgkin lymphoma, significantly fewer CNS progressions or relapsed occurred in the ACVBP group (9 out of 323) compared to the CHOP group (26 out of 312). Of note, in the ACVBP regimen, CNS prophylaxis consisted of four intrathecal injections of methotrexate during induction followed by two consolidative courses of high-dose intravenous methotrexate [16]. Taken together, these data suggest that early detection of occult CNS disease via a more sensitive test is needed and perhaps systemic administration of chemotherapy such as high-dose methotrexate might be more efficacious than intraventricular/intrathecal administration in preventing relapse. Both strategies should be explored further.
There is some suggestion that prophylactic cranial irradiation seems to result in a lower incidence of CNS relapse when incorporated into the treatment regimen of adult lymphoblastic lymphoma. Gokbuget and Hoelzer found that combination of cranial irradiation, systemic high-dose chemotherapy, and intrathecal therapy produced a CNS relapse rate of only 5% with a higher rate of relapse detected when cranial irradiation was omitted [17, 18]. Its role, however, in DLBCL remains doubtful. A combined analysis evaluating the efficacy of either intrathecal therapy or cranial irradiation resulted in similar CNS relapse rates between patients who received prophylaxis (2.8%) vs. patients who did not (3.6%; P = 0.74) [7].
The predictive risk factors for CNS relapse in this study were consistent with previous reports [1–6]. Our study showed ECOG performance status >1, >1 extranodal sites of involvement, bone marrow involvement, kidney involvement, liver involvement, B symptoms, and stage IV disease remained predictive of CNS relapse in patients treated R-CHOP at presentation. Consistent with Villa et al. [1], presence of renal involvement seemed to confer an especially high risk of CNS recurrence. It remains unknown whether the incidence of CNS relapse itself is increased in different genetic subtypes of DLBCL. Moving forward, incorporation of gene expression/microarray analysis in addition to clinical parameters could potentially aid in identifying patients at risk of CNS relapse.
Our study has several limitations and weaknesses. It is a retrospective study with its inherent confounders and biases. We attempted to evaluate the difference in CNS relapse between patients who received CHOP chemotherapy and R-CHOP chemotherapy in this study. The main difference between the two groups of patients was the period during which they were treated. The obvious difference in follow-up time between the two groups (5.4 vs. 2.7 years) needs to be emphasized as it is subjected to further bias. However, the median time to CNS relapse was found to be 0.56 year, perhaps attenuating this difference.
In conclusion, CNS relapse in DLBCL while uncommon portends a poor prognosis. Despite the additional survival benefit from rituximab in DLBCL across all risk groups, its efficacy in preventing CNS relapse appears to be limited. Efforts should be concentrated in better identification of occult CNS involvement, and better prophylactic strategies should be evaluated.
References
Villa D, Connors JM, Shenkier TN, Gascoyne RD, Sehn LH, Savage KJ (2010) Incidence and risk factors for central nervous system relapse in patients with diffuse large B-cell lymphoma: the impact of the addition of rituximab to CHOP chemotherapy. Ann Oncol 21:1046–1052
Boehme V, Zeynalova S, Kloess M, Loeffler M, Kaiser U, Pfreundschuh M, Schmitz N (2007) Incidence and risk factors of central nervous system recurrence in aggressive lymphoma—a survey of 1693 patients treated in protocol of German High-Grade Non-Hodgkin’s Lymphoma Study Group (DSHNHL). Ann Oncol 18:149–157
Boehme V, Schmitz N, Zeynalova S, Loeffler M, Pfreundschuh M (2009) CNS events in elderly patients with aggressive lymphoma treated with modern chemotherapy (CHOP-14) with or without rituximab: an analysis of patients treated in the RICOVER-60 trial of the German High-Grade Non-Hodgkin Lymphoma Study Group (DSHNHL). Blood 113:3896–3901
Shimazu T, Notohara K, Ueda Y (2009) Diffuse large B-cell lymphoma with central nervous system relapse: prognosis and risk factors according to retrospective analysis from a single centre experience. Int J Hematol 89:577–583
Doolittle ND, Abrey LE, Zucca E, Shenkier TN, Tali S, Bromberg JE, Neuwelt EA, Soussain C, Johnke K, Johnston P, Illerhaus G, Schiff D, Batchelor T, Montoto S, Df K, Zucca E (2008) Brain parenchyma involvement as isolated central nervous system relapse of systemic non-Hodgkin lymphoma: an International Primary CNS Lymphoma Collaborative Group report. Blood 111:1085–1093
Van Besien K, Ha CS, Murphy S, McLaughlin P, Rodriguez A, Amin K, Forman A, Romaguera J, Hagemeister F, Younes A, Bachier C, Sarris A, Sobocinski KS, Cox JD, Cabanillas F (1998) Risk factors, treatment, and outcome of central nervous system recurrence in adults with intermediate-grade and immunoblastic lymphoma. Blood 1998:1178–1184
Bernstein SH, Unger JM, Leblanc M, Friedberg J, Miller TP, Fisher RI (2009) Natural history of CNS relapse in patients with aggressive non-Hodgkin lymphoma: a 20-year follow up analysis of SWOG 8516—The Southwest Oncology Group. J Clin Oncol 27:114–119
Arkenau HT, Chong G, Cunningham D, Watkins D, Agarwal R, Sirohi B, Trumper M, Norman A, Wotherspoon A, Horwich A (2007) The role of intrathecal chemotherapy prophylaxis in patients with diffuse large B-cell lymphoma. Ann Oncol 18:541–545
Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, Morel P, Van Den Neste E, Salles G, Gaulard P, Reyes F, Lederlin P, Gisselbrecht C (2002) CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large B cell lymphoma. N Engl J Med 346:235–242
Feugier P, Van Hoof A, Sebban C et al (2005) Long term results of the R-CHOP study in the treatment of elderly patients with diffuse large B-cell lymphoma: a study by the Groupe d’Etude des Lymphomes de I’Adulte. J Clin Oncol 23:4117–4126
Pfreundshcuh M, Trumper L, Osterborg A et al (2006) CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good prognosis diffuse large B-cell lymphoma: a randomized controlled trial by the MabThera International Trial (MInT) Group. Lancet Oncol 7:379–391
Haberman TM, Weller EA, Morrison VA et al (2006) Rituximab-CHOP versus CHOP alone or with maintenance rituximab in older patients with diffuse large B-cell lymphoma. J Clin Oncol 24:3121–3127
Pfreundshcuh M, Schubert Z, Ziepert M et al (2008) Six versus eight cycles of bi-weekly CHOP-14 with or without rituximab in elderly patients with aggressive CD20+ B-cell lymphomas: a randomized controlled trial (RICOVER-60). Lancet Oncol 9:105–116
Yamamoto W, Ishigatsubo Y et al (2010) Central nervous system involvement in diffuse large B-cell lymphoma. Eur J Hematol 85:6–10
Hegde U, Filie A, Little RF, Janik JE, Grant N, Steinberg SM, Dunleavy K, Jaffe Es, Abati A, Stetler-Stevenson M, Wilson WH (2005) High incidence of occult leptomeningeal disease detected by flow cytometry in newly diagnosed aggressive B-cell lymphomas at risk for CNS involvement: the role of flow cytometry versus cytology. Blood 105:496–502
Tilly H, Lepage E, Coiffier B, Blanc M, Herbrecht R, Bosly A, Attal M, Fillet G, Guettier C, Molina TJ, Gisselbrecht C, Reyes F (2003) Intensive conventional chemotherapy (ACVBP regimen) compared with standard CHOP for poor-prognosis aggressive non Hodgkin lymphoma. Blood 102:4284–4289
Gokbuget N, Hoelzer D (2002) Recent approaches in acute lymphoblastic leukemia in adults. Rev Clin Exp Hematol 6:114–140
Gokbuget N, Hoelzer D (1998) Meningeosis leukaemia in adult acute lymphoblastic leukaemia. J Neuro Oncol 38:167–180
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Tai, W.M., Chung, J., Tang, P.L. et al. Central nervous system (CNS) relapse in diffuse large B cell lymphoma (DLBCL): pre- and post-rituximab. Ann Hematol 90, 809–818 (2011). https://doi.org/10.1007/s00277-010-1150-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-010-1150-7