Abstract
Cancerous inhibitor of protein phosphatase 2A (CIP2A) is a recently identified human oncoprotein that stabilizes the c-MYC protein. Herein, we aimed to investigate its expression pattern, clinical significance, and biological function in urothelial cell carcinoma (UCC) of the bladder. CIP2A expression was examined in 20 fresh bladder UCC tissues and paired adjacent normal bladder tissues by RT-PCR and Western blot. Immunohistochemistry for CIP2A was performed on additional 117 bladder UCC tissues. The clinical significance of CIP2A expression was analyzed. CIP2A downregulation was performed in bladder UCC cell line T24 with high abundance of CIP2A, and the effects of CIP2A silencing on cell proliferation, migration, invasion in vitro, and tumor growth in vivo were evaluated. We found that CIP2A expression was upregulated in bladder UCC tissues relative to adjacent normal bladder tissues. Clinicopathological analysis showed that CIP2A expression was significantly associated with tumor stage (P = 0.004), histological grade (P = 0.007), and lymph node status (P = 0.001). The Kaplan–Meier survival curves revealed that CIP2A expression was associated with poor prognosis in bladder UCC patients (log-rank value = 14.704, P < 0.001). CIP2A expression was an independent prognostic marker of overall patient survival in a multivariate analysis (P = 0.015). Knockdown of the CIP2A expression reduced cell proliferation, anchorage-independent growth, migration, invasion, and tumor growth in xenograft model mice. Our findings suggest that CIP2A is an independent predictor of poor prognosis of bladder UCC patients, and inhibition of its expression might be of therapeutic significance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bladder cancer is the fourth most commonly diagnosed malignancy in men in the United States. In 2012, an estimated 73,510 new cases will be diagnosed, which could result in an estimated 14,880 deaths [1]. Urothelial cell carcinoma (UCC), previously designated as transitional cell carcinoma (TCC), accounts for approximately 90 % of all bladder cancers [2]. At presentation, 70–80 % of patients have non-muscle-invasive UCC (stage Ta, T1, and Tis) and 20–30 % have invasive disease (≥stage T2). Radical cystectomy with urinary diversion is currently the standard treatment for those patients with refractory non-muscle-invasive and muscle-invasive bladder UCC [3]. Unfortunately, however, disease recurrence is observed in 30–56 % of patients undergoing surgery, most often the result of occult metastatic disease [4]. The prognosis for patients with disease recurrence following cystectomy is poor. Therefore, better understanding of the pathogenesis and biological features of bladder UCC, looking for useful biomarkers, and exploring novel therapeutic targets for treatment are urgently demanding tasks.
Cancerous inhibitor of protein phosphatase 2A (CIP2A), also known as KIAA1524 and p90, is a recently characterized human oncoprotein that stabilizes c-MYC protein level by inhibiting protein phosphatase 2A (PP2A) dephosphorylation activity toward c-MYC serine 62 (S62), thereby restraining c-MYC degradation mediated by PP2A in cancer cells [5, 6]. Moreover, transformation of immortalized human cells is observed when CIP2A is overexpressed [5]. In loss of function studies, CIP2A depletion has been shown to reduce the overall xenograft tumor volume in nude mice [5, 7, 8], impair clonogenicity and anchorage-independent growth [5, 7–14], and to attenuate the migration and invasion of tumor cells [15].
CIP2A is expressed in only very few normal tissues but it is overexpressed in a wide variety of cancers such as head and neck squamous cell carcinoma [5], breast cancer [7], non-small cell lung cancer [8, 9], gastric cancer [10, 11], esophageal squamous cell carcinoma [14], renal cell carcinoma [15], oral squamous cell carcinoma [16], colorectal cancer [12, 17], tongue cancer [18], ovarian cancer [19], prostate cancer [20], cervical cancer [13, 21], and acute myeloid leukemia [22]. More importantly, the increased expression of CIP2A has been correlated with clinically aggressive behavior and/or poor patient survival in several cancer types [7, 9, 11, 12, 15, 17–19].
However, the expression pattern, clinical relevance, and biological function of CIP2A in bladder cancer have so far not been investigated. In the present study, we examined both mRNA and protein expression patterns in bladder UCC tissues. We also investigated the correlations between CIP2A protein expression and clinicopathologic parameters, and its prognostic value for survival of patients with bladder UCC. Then, we employed the small interfering RNA (siRNA) technique to evaluate the effects of knockdown of CIP2A on proliferation, anchorage-independent growth, migration, and invasion of bladder UCC cell line T24 in vitro. In addition, using an in vivo xenograft model, we provide evidence that CIP2A depletion inhibits T24 xenograft growth in nude mice. Collectively, our findings indicate that CIP2A plays a role in human bladder UCC progression.
Materials and methods
Patients and surgical specimens
The protocol of this study was approved by the Ethics Committee of Gannan Medical University (Ganzhou, China), and written informed consent was obtained from each patient. Tumor samples from resection specimens were collected from two cohorts of patients with primary bladder UCC, who underwent a transurethral resection or a total cystectomy for the disease at the Department of Urology, First Affiliated Hospital of Gannan Medical University (Ganzhou, China) between January 2010 and July 2010 for cohort A and between January 2003 and June 2006 for cohort B. The patients of both cohorts were selected based on (a) distinctive histopathologic diagnosis of UCC, (b) availability of sufficient resection tissue, and (c) availability of detailed clinicopathologic data. Patients with any anticancer treatment prior to surgery or with evidence of other malignancies were excluded from the study. Cohort A consisted of 20 patients (16 males and 4 females; median age 51 years; range 32–78 years), from whom fresh tumor samples coupled with adjacent histologically normal bladder tissues were obtained for analysis of CIP2A gene expression. After removal at surgery, all the fresh tissues were immediately frozen in liquid nitrogen and stored at −80 °C until RNA or protein extraction. Cohort B comprised 117 patients (98 males and 19 females; median age 57 years; range 31–82 years), whose paraffin-embedded specimens were available at the surgical pathology archive of First Affiliated Hospital of Gannan Medical University, allowing for immunohistochemical analysis. Of these, 51 patients underwent transurethral resection of bladder tumor and 66 patients underwent radical cystectomy. Tumors were staged according to the 6th edition of the pTNM classification of the International Union Against Cancer (UICC, 2002). A total of 62 patients were of stage Ta or T1, and 55 of stage T2–T4. Histologic grading of tumors was defined according to the criteria of the WHO (G1, n = 23; G2, n = 53; G3, n = 41). The clinicopathologic characteristics are summarized in Table 1. Thirty cases of normal bladder mucosa from adjacent non-neoplastic bladder tissue of the same UCC patients, in paraffin blocks, were also obtained. The median follow-up time was 57.1 months (range 5–90 months). By the end of follow-up, 61 patients died.
Semiquantitative RT-PCR assay
Total RNA was isolated from tissues or cells using Trizol reagent (Invitrogen) according to the manufacturer’s protocol. cDNA was synthesized with use of the RevertAid™ First Strand cDNA Synthesis kit (Fermentas, Ontario, Canada) following the manufacturer’s protocol. The following primers were used for amplification: CIP2A, forward primer (5′-GGGAATTCCC TGATTCCTCTTCA-3′) and reverse primer (5′-CCCTCGAGCTAGAAGCTTACTTCCAT -3′), and β-actin, forward primer (5′-GTGGGGCGCCCCCAGGCACCA-3′) and reverse primer (5′-CTCCTTAATGTCACGCACGAT-3′). The PCR reactions were performed in a PTC-100 thermal cycler (MJ Research Inc., Waltham, MA, USA) for 30 cycles. Each cycle consisted of 30 s of denaturation at 94 °C, 30 s of annealing at 55 °C, and 30 s of extension at 72 °C. The reaction mixtures of PCR were run at 1 % agarose gel and photographed. The amplification of β-actin was used as an internal control.
Western blot assay
Tissues or cells were lysed in lysis buffer containing protease inhibitor cocktail. Protein concentration was determined using a Bio-Rad protein assay system (Bio-Rad, Hercules, CA, USA). Equivalent amounts of proteins were separated by SDS-PAGE, and then transferred to polyvinylidene difluoride membranes (Bio-Rad). After being blocked in Tris-buffered saline (TBS) containing 5 % non-fat milk, the membranes were incubated with primary antibodies against CIP2A (1:500; Novus Biologicals, Littleton, CO, USA), c-MYC (1:1000; Abcam, Cambridge, MA, USA), and β-actin (1:500; Santa Cruz Biotechnology, Santa Cruz, CA, USA) at 4 °C for 12 h, and then with anti-rabbit or anti-mouse IgG secondary antibody conjugated to horseradish peroxidase (Assay Design, MI, USA) at room temperature for 2 h. Proteins were visualized using ECL (Pierce, Rockford, IL, USA) and detected using BioImaging Systems (UVP Inc., Upland, CA, USA). The relative protein levels were calculated based on β-actin protein as a loading control.
Immunohistochemistry staining
Paraffin sections (4 μm thick) were deparaffinized in xylene and rehydrated in grade alcohol, followed by boiling in 10 mmol/L of citrate buffer (pH 6.0) for antigen retrieval. After inhibition of endogenous peroxidase activities for 30 min with methanol containing 0.3 % H2O2, the sections were blocked with 2 % bovine serum albumin for 30 min and incubated overnight at 4 °C with primary polyclonal rabbit anti-human CIP2A antibody (1:250; Novus Biologicals, Littleton, CO, USA). After washing thrice with PBS, the slides were incubated with horseradish peroxidase-conjugated goat anti-rabbit IgG for 30 min, followed by reaction with diaminobenzidine and counterstaining with Mayer’s hematoxylin. Negative control was done by omission of the primary antibody and substituting it with non-specific rabbit IgG.
Evaluation of immunohistochemical staining
Three pathologists (H.Y., S.P., and X.H.) evaluated the immunostaining in a blinded fashion without any knowledge of the clinical outcome or other clinicopathological data. If there was a discrepancy in individual evaluations, then all the three pathologists reevaluated the slides together to reach a consensus. Immunohistochemical staining of CIP2A was evaluated using a semiquantitative scoring system for both staining intensity and the percentage of positive cells. Staining intensity was graded as 0, no staining; 1, weak staining; 2, moderate staining; and 3, strong staining. Percentage scores were assigned as 1, 1–25 %; 2, 26–50 %; 3, 51–75 %; and 4, 76–100 %. The staining results were finally recorded as 0, negative (−); ≤4, low expression (+); 5–8, moderate expression (++); and ≥9, high expression (+++). Tumor samples scored (+) to (+++) were considered positive.
Cell lines
Bladder cancer cell lines T24, 5637, BIU-87, J82, and an immortalized normal human urothelial cell line SV–HUC–1 were purchased from the Cell Bank of Type Culture Collection of Chinese Academy of Sciences (Shanghai, China). These cells were cultured in DMEM supplemented with 10 % fetal bovine serum, 100 μg/mL penicillin, and 100 μg/mL streptomycin at 37 °C in a humidified atmosphere containing 5 % CO2.
Gene silencing using siRNA
The siRNA targeting CIP2A and control siRNA were purchased from Invitrogen. The siRNA sequence for CIP2A was 5′-GACAACUGUCAAGUGUACCACUCUU-3′. Cells were transfected with either CIP2A or control siRNA using Oligofectamine reagent (Invitrogen) according to the manufacturer’s instructions. Following transfection, the mRNA and protein levels were assessed 48 h later.
MTT assay
T24 cells were plated in 96-well culture plates at about 5 × 103 cells per well 24 h after transfection. Then, 20 μL of 5 mg/mL MTT (thiazolyl blue) solution was added to each well and incubated for 4 h at 37 °C, the media was removed from each well, and the resultant MTT formazan was solubilized in 150 μL of DMSO. The absorbance values at 490 nm were measured using a microplate reader (Bio-Rad). The experiment was repeated three times, and each experiment had six replicate wells.
Anchorage-independent soft agar growth assay
T24 cells were transfected with control or CIP2A siRNA for 48 h. Cells were then plated on a 0.6 % agarose base in six-well plates (1.0 × 103 cells per well) in 1 mL of DMEM medium containing 10 % fetal bovine serum and 0.3 % agarose. The plates were incubated at 37 °C in 5 % CO2 for 16 days; colonies were fixed and stained with 0.1 % crystal violet. The colonies containing at least 50 cells were counted.
Scratch migration assay
T24 cells were seeded to 12-well plates and transfected with control or CIP2A siRNA. At 24 h after transfection, cells were scratched using the tip of a sterile 200-μL pipette (width: ~1 mm) in each well. The plates were washed twice with PBS in order to remove the detached cells and incubated at 37 °C in 5 % CO2. Wound closure was monitored at various time points by observation under a microscope, and the degree of cell migration was quantified by the ratio of gap distance at 24 h to that at 0 h. The experiment was done in triplicate.
Matrigel invasion assay
Cell invasion assay was performed using a 24-well Transwell chamber with a pore size of 8 μm (Costar, New York, NY, USA). The inserts were coated with 50 μl Matrigel (dilution at 1: 2; BD Bioscience, Franklin Lakes, NJ, USA). T24 cells were trypsinized after transfection with control or CIP2A siRNA for 48 h and transferred to the upper Matrigel chamber in 100 μl of serum-free medium containing 1 × 105 cells and incubated for 24 h. The lower chamber was filled with medium that contained 10 % fetal bovine serum as chemoattractants. After incubation, the non-invaded cells on the upper membrane surface were removed with a cotton tip, and the cells that passed through the filter were fixed and stained using 0.1 % crystal violet. The numbers of invaded cells were counted in five randomly selected high-power fields under a microscope. This experiment was performed in triplicate.
Cancer xenograft model and tumorigenicity assay
Four-week-old male BALB/c nude mice (Institute of Zoology, Chinese Academy of Sciences) were housed in a specific pathogen-free environment at the Animal Laboratory Unit, Gannan Medical University, China. T24 cells (1.0 × 107) were suspended in 100 μL PBS and injected subcutaneously in the right flank region of nude mice. After 2 weeks, the injected nude mice with tumor burden were randomly divided into two groups (n = 6 for each group): (1) control siRNA group, intratumoral injection of control siRNA complex every 5 days; (2) CIP2A siRNA group, intratumoral injection of CIP2A siRNA complex every 5 days. Each complex contained 10 μg of siRNA and 7.5 μL Oligofectamine (Invitrogen) in PBS, which was mixed according to manufacturer’s instruction of Oligofectamine. The tumor diameters were measured two times a week with a caliper. The tumor volumes (mm3) were calculated according to the following formula: length × width2/2. All mice were sacrificed humanely after 5 times of treatment, and the resected tumors were weighed. All experimental manipulations were undertaken in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals, with the approval of the Scientific Investigation Board of the Gannan Medical University, Ganzhou, China.
Statistical analysis
The statistical analyses were performed using the Statistical Package for the Social Sciences, version 16.0 (SPSS Inc., Chicago, IL, USA). A paired-samples t test was used to compare CIP2A mRNA and protein expression in the UCC tissues with that of their paired adjacent normal tissue samples. The relationship between CIP2A protein expression and the clinicopathological features was analyzed using χ2 tests. Overall survival curves were calculated with the Kaplan–Meier method and were analyzed with the log-rank test. A Cox proportional hazards analysis was used in univariate and multivariate analyses to explore the effects of CIP2A expression and UCC clinicopathological variables on survival. Unpaired 2-tailed Student’s t tests were used to analyze comparisons between the two groups. A P value of <0.05 was regarded as statistically significant.
Results
Expression of CIP2A mRNA and protein in UCC tissues
We first examined CIP2A mRNA expression in 20 bladder UCC tissues and paired adjacent normal bladder tissues by semiquantitative RT-PCR. β-actin was used as an internal control, and the ratio of CIP2A/β-actin was used to reflect the relative mRNA expression level of CIP2A. As shown in Fig. 1a, the relative level of CIP2A mRNA in UCC tissues was significantly higher than that in adjacent normal bladder tissues (P < 0.01). To investigate whether CIP2A was also elevated at the protein level, Western blot was performed on those tissues. We found that the relative level of CIP2A protein in UCC tissues was significantly higher than that in adjacent normal bladder tissues (P < 0.01, Fig. 1b), consistent with the results of RT-PCR.
Analysis of CIP2A mRNA and protein expression in 20 cases of bladder UCC tissues and adjacent normal bladder tissues. a Semiquantitative RT-PCR detection of CIP2A mRNA expression. b Western blot detection of CIP2A protein expression. β-actin was used as an internal control. N, adjacent normal bladder tissues; T, bladder UCC tissues. Each assay was performed at least three times
Immunohistochemical analysis of CIP2A expression in bladder UCC samples and its relationship to clinicopathological parameters
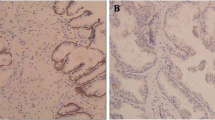
We further analyzed CIP2A protein level in 117 UCC tissues and 30 normal bladder tissues using an immunohistochemical approach. As shown in Fig. 2a, normal bladder epithelia showed negative CIP2A staining. Conversely, the immunoreactive patterns of CIP2A were predominantly positively identified in the cancer tissues. The CIP2A protein appeared to be expressed in both cytoplasmic and nuclear components of tumor cells with stronger signal seen in the former one (Fig. 2 b–d). Of these tumor tissues, 85 (72.6 %) cases showed CIP2A-positive expression. The relationship between CIP2A protein expression and various clinicopathological parameters is described in Table 1. CIP2A protein expression significantly correlated with tumor stage (P = 0.004), histological grade (P = 0.007), and lymph node status (P = 0.001). However, CIP2A protein expression was not associated with other clinicopathological features such as age, gender, and tumor number.
CIP2A protein expression and patient survival. a Immunohistochemical analysis of CIP2A protein expression in 117 cases of bladder UCC tissues: (a) Normal bladder urothelium with negative CIP2A expression (–); (b) tumors with low CIP2A expression (+); (c) tumors with moderate CIP2A expression (++); and (d) tumors with high CIP2A expression (+++). Magnification, all ×200. b Overall survival analysis using the Kaplan–Meier method revealed that patients with positive CIP2A expression had obviously lower overall survival rates than did those with negative CIP2A expression
CIP2A expression and patient survival
The prognostic value of CIP2A for overall survival in bladder UCC patients was evaluated by comparing the patients with positive and negative CIP2A expression. According to the Kaplan–Meier survival analysis, bladder UCC patients with positive CIP2A expression had obviously lower overall survival rates than did those with negative CIP2A expression (Fig. 2b, log-rank value = 14.704, P < 0.001). Upon univariate analysis with the Cox proportional hazards model, tumor stage (P < 0.001), histologic grade (P = 0.001), lymph node status (P < 0.001), and CIP2A expression (P < 0.001) were all positively correlated with a poor prognosis. Multivariate analyses revealed that tumor stage (P < 0.001), lymph node status (P = 0.013), and CIP2A expression (P = 0.015) were independent prognostic factors (Table 2). Thus, CIP2A expression may be useful for predicting the overall survival of bladder UCC patients.
CIP2A expression in bladder cancer cell lines
We also used RT-PCR and Western blot to detect the expression of CIP2A mRNA and protein in four bladder cancer cell lines as well as in an immortalized normal urothelial cell line. As shown in Fig. 3a, the T24, 5637, BIU-87, and J82 showed higher level of CIP2A mRNA relative to the normal urothelial cell line SV–HUC–1. Likewise, CIP2A protein expression was elevated in those bladder cancer cell lines compared to the SV–HUC–1 cell line (Fig. 3b).
Expression of CIP2A mRNA and protein in bladder cancer cell lines and CIP2A knockdown by CIP2A siRNA. a and b CIP2A mRNA and protein expression detected in several human bladder cell lines (T24, 5637, BIU-87, and J82) as well as in an immortalized normal urothelial cell line SV–HUC–1 by RT-PCR and Western blot analysis, respectively. c RT-PCR analysis of CIP2A mRNA expression in T24 cells transfected with the specific siRNA targeting CIP2A for 48 h. d Western blot analysis of CIP2A and c-MYC protein expression in T24 cells transfected with the CIP2A siRNA for 72 h
Effects of CIP2A depletion on c-MYC expression and cell growth in vitro
To explore the biological significance of CIP2A in bladder UCC, we specifically knocked down its expression in T24 cells using RNA interference (RNAi). This UCC cell line was chosen because of its high abundance of CIP2A. The efficacy of CIP2A siRNA for knockdown of CIP2A mRNA and protein was confirmed by RT-PCR and Western blot analysis, respectively. We observed that CIP2A mRNA and protein levels were significantly reduced in cells transfected with specific siRNA for CIP2A compared with those transfected with control siRNA (Fig. 3c, d). Thus, the CIP2A siRNA could effectively knock down CIP2A expression at both transcriptional and translational levels. Furthermore, knockdown of CIP2A by siRNA resulted in inhibition of c-MYC protein expression (Fig. 3d). We next studied the impact of CIP2A silencing on cell proliferation. The results of the MTT assay showed that CIP2A siRNA significantly reduced the proliferation rate of T24 cells compared with the control siRNA-transfected cells (P < 0.01; Fig. 4a). Soft agar colony formation assay further showed that downregulation of CIP2A in T24 cells with transfection of CIP2A siRNA resulted in a clear reduction of the anchorage-independent colony formation capacity compared with the control siRNA-transfected cells (P < 0.01; Fig. 4b). These findings collectively highlight an important role for CIP2A in regulation of UCC cell growth and survival.
Effects of CIP2A depletion on cell growth in vitro. a Inhibition of T24 cell proliferation by CIP2A siRNA tested by MTT assay. b Inhibition of T24 cell anchorage-independent colony formation capacity by CIP2A siRNA. Experiments were repeated at least three times, and representative data are presented; bars, SD.*, P < 0.01, relative to control
Effect of CIP2A deletion on migration and invasion in vitro
In scratch migration assay, downregulation of CIP2A suppressed the migration of T24 cells (Fig. 5a). The migrating distance was 0.838 ± 0.047 mm in the control siRNA group and 0.492 ± 0.038 mm in the CIP2A siRNA group (P < 0.05). Matrigel invasion assay showed that downregulation of CIP2A suppressed the invasiveness of T24 cells (Fig. 5b). The average cell counts crossing Matrigel-coated membrane in one high-power field were 44.1 ± 8.7 for the control siRNA group and 19.6 ± 5.5 for the CIP2A siRNA group (P < 0.05).
CIP2A depletion attenuated the migration and invasion capability of T24 cells in vitro. a Scratch migration assay showed that CIP2A decreased tumor cell migration. b Matrigel invasion assay showed that CIP2A siRNA-transfected cells resulted in low penetration through the Matrigel-coated membrane, compared with control cells. The experiments were repeated thrice. *, P < 0.05, relative to control
Depletion of CIP2A inhibits tumor growth in vivo
To investigate whether CIP2A siRNA had the effect of inhibition on tumor growth in vivo, a nude mice xenograft model of bladder UCC was established, and intratumoral injection with CIP2A siRNA or control siRNA complex in the nude mice with tumor burden was performed and repeated every 5 days for a total of 5 times. As shown in Fig. 6a, the tumor volume of CIP2A siRNA group from days 22 to the end was significantly smaller than control siRNA groups (P < 0.01). Furthermore, CIP2A siRNA resulted in a significant decrease in the tumor volume and weight as measured at the end of the experiment at day 42 when compared with control siRNA (P < 0.01; Fig. 6b). In addition, the relative protein expression of CIP2A in CIP2A siRNA group was decreased (Fig. 6c).
Knockdown of CIP2A by siRNA inhibits the growth of T24-derived xenografts in nude mice. a Left, macrographic image showed that the tumor size of CIP2A group was markedly smaller on the 42nd day after tumor cells inoculation than that of control group. Right, growth curves of the tumor xenografts; bars, SD.*, P < 0.01, relative to control. b The final tumor volume (left) and weight (right) of CIP2A group were decreased than that of control group, P < 0.01. c CIP2A siRNA inhibited the protein expression of CIP2A in vivo as determined by Western blot
Discussion
Recent data from several groups have highlighted that CIP2A is upregulated in a wide variety of malignant tumors [7–22]. CIP2A overexpression has also been reported to be associated with worse prognosis and to serve as a prognostic marker in numerous human cancers [9, 11, 12, 15–17]. These findings imply an oncogenic role for CIP2A; however, little is known about its expression pattern and biological significance in bladder UCC, one of the most common malignancies worldwide. In this study, we showed that CIP2A expression determined by RT-PCR and Western blot is upregulated in bladder UCCs relative to adjacent normal bladder tissues. Immunohistochemical analysis performed in a relatively large cohort of bladder UCC specimens revealed that CIP2A expression is significantly correlated with tumor stage, histologic grade, and lymph node status. Most importantly, CIP2A expression predicts poor prognosis of bladder UCC patients, as an independent prognostic factor. To extend our clinical studies and investigate its biological function, we employed siRNA to knock down CIP2A expression in bladder UCC cell line T24. Depletion of endogenous CIP2A attenuated proliferation of T24 cells in vitro and reduced the growth of T24-derived xenografts in nude mice. Furthermore, depletion of CIP2A could inhibit cell migration and invasion in vitro. Collectively, these data strongly suggest that CIP2A served as both a prognostic biomarker and a potential therapeutic target in bladder UCC.
It has been shown that CIP2A inhibits PP2A activity toward the oncogenic transcription factor c-MYC Ser62 and thereby stabilizes the c-MYC protein by preventing its proteolytic degradation [5, 6]. As a proto-oncoprotein, c-MYC has many important biological functions, including cell proliferation, differentiation, senescence, apoptosis, and transformation [23–28]. Overexpression of c-MYC has been found in bladder cancers [29–32]. Consistently, our data showed that the depletion of CIP2A expression in human bladder UCC cell line T24 resulted in reduced c-MYC protein levels. Loss of CIP2A also inhibited T24 cell proliferation, anchorage-independent growth, and tumor growth in xenograft model mice.
In our study, we also demonstrated that knockdown of CIP2A reduces migration and invasion capability of T24 cells, which is in good agreement with a recent observation by Ren and colleagues in cultured renal cell carcinoma cells [15]. The molecular mechanism for CIP2A in promoting cancer cell migration, invasion, and metastasis has been largely unknown. Based on the role of CIP2A in stabilizing and upregulating the MYC oncoprotein, one possible explanation was that MYC is involved in CIP2A-stimulated invasiveness of tumor cells. Deregulation of the MYC oncoprotein confers a selective advantage on cancer cells in differing contexts by promoting proliferation, cell survival, differentiation blockade, and genetic instability [33–36], all of which can contribute to metastasis. In fact, a recent study suggested that MYC functions as a regulator of invasion and metastasis in a mouse model of non-small cell lung cancer by modulating growth, differentiation, and angiogenesis [37]. RNAi-mediated MYC knockdown in highly metastatic MDA-MB-231 breast cancer cells disrupts cellular invasion, migration, and metastasis in vivo [38]. Furthermore, MYC has been found to regulate the epithelial-to-mesenchymal transition that is necessary for cellular invasion and migration in some contexts. MYC does this by promoting TGF-β-mediated activation of the SNAIL transcription factor though a microRNA network involving a LIN28B/let-7/HMGA2 cascade [39–42]. All these effects of MYC may contribute to tumor cell invasion and metastasis driven by CIP2A; however, further study is necessary to elucidate the role of MYC in CIP2A-mediated bladder UCC invasion and metastasis.
Our data strengthen the case for the use of CIP2A as an anticancer target. CIP2A is expressed at undetectable or low levels in normal tissues, thereby creating a potential therapeutic window for CIP2A targeting agents. Tseng et al. [43] demonstrated that bortezomib downregulated CIP2A in HCC-1937 xenograft tumors and inhibited their tumor growth. Moreover, it has been shown that the traditional chemotherapeutic agent doxorubicin downregulates CIP2A expression and that increased CIP2A expression confers doxorubicin resistance in breast cancer cells [44]. More recently, Ma et al. [8] demonstrated that rabdocoetsin B, a novel natural compound extracted from a Chinese medicinal herbal Rabdosia coetsa, inhibits CIP2A at mRNA level, resulting in downregulation of both CIP2A and pAKT proteins. They propose that the inhibition of the CIP2A-AKT pathway by rabdocoetsin B in lung cancer cells leads to reduced proliferation and induced apoptosis. It will therefore be interesting to see whether future studies may uncover similar effects in mouse models for bladder UCC and in clinical studies.
Taken together, we identified a frequent overexpression of CIP2A in bladder UCC patients. This overexpression positively correlates with the aggressive phenotype and predicts poor survival outcome in bladder UCC patients as an independent predicting factor. This finding suggests that CIP2A would serve as a potential biological marker to identify a subgroup of patients of poor prognosis. We have also presented experimental evidence that depletion of CIP2A in human bladder UCC cell line T24 using siRNA inhibited cell proliferation, anchorage-independent growth, migration, invasion, and tumor growth in xenograft model mice. Based on these findings, we conclude that CIP2A is functionally important in the development and progression of bladder UCC and may serve as a new target for future cancer therapeutics.
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
Kaufman DS, Shipley WU, Feldman AS. Bladder cancer. Lancet. 2009;374:239–49.
Stenzl A, Cowan NC, De Santis M, et al. The updated EAU guidelines on muscle-invasive and metastatic bladder cancer. Eur Urol. 2009;55:815–25.
Shariat SF, Karakiewicz PI, Palapattu GS, et al. Outcomes of radical cystectomy for transitional cell carcinoma of the bladder: a contemporary series from the bladder cancer research consortium. J Urol. 2006;176:2414–22.
Junttila MR, Puustinen P, Niemela M, et al. CIP2A inhibits PP2A in human malignancies. Cell. 2007;130:51–62.
Junttila MR, Westermarck J. Mechanisms of MYC stabilization in human malignancies. Cell Cycle. 2008;7:592–6.
Côme C, Laine A, Chanrion M, et al. CIP2A is associated with human breast cancer aggressivity. Clin Cancer Res. 2009;15:5092–100.
Ma L, Wen ZS, Liu Z, et al. Overexpression and small molecule-triggered downregulation of CIP2A in lung cancer. PLoS ONE. 2011;6:e20159.
Dong QZ, Wang Y, Dong XJ, et al. CIP2A is overexpressed in non-small cell lung cancer and correlates with poor prognosis. Ann Surg Oncol. 2011 ;18:857–65.
Li W, Ge Z, Liu C, et al. CIP2A is overexpressed in gastric cancer and its depletion leads to impaired clonogenicity, senescence, or differentiation of tumor cells. Clin Cancer Res. 2008;14:3722–8.
Khanna A, Bockelman C, Hemmes A, et al. MYC-dependent regulation and prognostic role of CIP2A in gastric cancer. J Natl Cancer Inst. 2009;101:793–805.
Teng HW, Yang SH, Lin JK, et al. CIP2A is a predictor of poor prognosis in colon cancer. J Gastrointest Surg. 2012;16:1037–47.
Liu J, Wang X, Zhou G, et al. Cancerous inhibitor of protein phosphatase 2A is overexpressed in cervical cancer and upregulated by human papillomavirus 16 E7 oncoprotein. Gynecol Oncol. 2011;122:430–6.
Qu W, Li W, Wei L, et al. CIP2A is overexpressed in esophageal squamous cell carcinoma. Med Oncol. 2012;29:113–8.
Ren J, Li W, Yan L, et al. Expression of CIP2A in renal cell carcinomas correlates with tumour invasion, metastasis and patients’ survival. Br J Cancer. 2011;105:1905–11.
Basile JR, Czerninski R. The role of CIP2A in oral squamous cell carcinoma. Cancer Biol Ther. 2010;10:700–2.
Böckelman C, Koskensalo S, Hagström J, et al. CIP2A overexpression is associated with c-Myc expression in colorectal cancer. Cancer Biol Ther. 2012;13:289–95.
Böckelman C, Hagström J, Mäkinen LK, et al. High CIP2A immunoreactivity is an independent prognostic indicator in early-stage tongue cancer. Br J Cancer. 2011;104:1890–5.
Böckelman C, Lassus H, Hemmes A, et al. Prognostic role of CIP2A expression in serous ovarian cancer. Br J Cancer. 2011;105:989–95.
Vaarala MH, Väisänen MR, Ristimäki A. CIP2A expression is increased in prostate cancer. J Exp Clin Cancer Res. 2010;29:136.
Huang LP, Adelson ME, Mordechai E, et al. CIP2A expression is elevated in cervical cancer. Cancer Biomark. 2010–2011; 8:309–17.
Wang J, Li W, Li L, et al. CIP2A is over-expressed in acute myeloid leukaemia and associated with HL60 cells proliferation and differentiation. Int J Lab Hematol. 2011;33:290–8.
Koskinen PJ, Alitalo K. Role of myc amplification and overexpression in cell growth, differentiation and death. Semin Cancer Biol. 1993;4:3–12.
Hurlin PJ, Dezfouli S. Functions of myc:max in the control of cell proliferation and tumorigenesis. Int Rev Cytol. 2004;238:183–226.
Xu D, Popov N, Hou M, et al. Switch from Myc/Max to Mad1/Max binding and decrease in histone acetylation at the telomerase reverse transcriptase promoter during differentiation of HL60 cells. Proc Natl Acad Sci USA. 2001;98:3826–31.
Facchini LM, Penn LZ. The molecular role of Myc in growth and transformation: recent discoveries lead to new insights. FASEB J. 1998;12:633–51.
Donzelli M, Bernardi R, Negri C, et al. Apoptosis-prone phenotype of human colon carcinoma cells with a high level amplification of the c-myc gene. Oncogene. 1999;18:439–48.
Albihn A, Johnsen JI, Henriksson MA. MYC in oncogenesis and as a target for cancer therapies. Adv Cancer Res. 2010;107:163–224.
Shiina H, Igawa M, Shigeno K, et al. Beta-catenin mutations correlate with over expression of C-myc and cyclin D1 Genes in bladder cancer. J Urol. 2002;168:2220–6.
Christoph F, Schmidt B, Schmitz-Dräger BJ, et al. Over-expression and amplification of the c-myc gene in human urothelial carcinoma. Int J Cancer. 1999;84:169–73.
Lipponen PK. Expression of c-myc protein is related to cell proliferation and expression of growth factor receptors in transitional cell bladder cancer. J Pathol. 1995;175:203–10.
Masters JR, Vesey SG, Munn CF, et al. c-myc oncoprotein levels in bladder cancer. Urol Res. 1988;16:341–4.
Grandori C, Cowley SM, James LP, et al. The Myc/Max/Mad network and the transcriptional control of cell behavior. Annu Rev Cell Dev Biol. 2000;16:653–99.
Podsypanina K, Du YC, Jechlinger M, et al. Seeding and propagation of untransformed mouse mammary cells in the lung. Science. 2008;321:1841–4.
Soucek L, Whitfield J, Martins CP, et al. Modeling Myc inhibition as a cancer therapy. Nature. 2008;455:679–83.
Ma L, Young J, Prabhala H, et al. miR-9, a MYC/MYCN-activated microRNA, regulates E-cadherin and cancer metastasis. Nat Cell Biol. 2010;12:247–56.
Rapp UR, Korn C, Ceteci F, et al. MYC is a metastasis gene for non-small-cell lung cancer. PLoS ONE. 2009;4:e6029.
Wolfer A, Wittner BS, Irimia D, et al. MYC regulation of a “poor-prognosis” metastatic cancer cell state. Proc Natl Acad Sci USA. 2010;107:3698–703.
Chang TC, Yu D, Lee YS, et al. Widespread microRNA repression by Myc contributes to tumorigenesis. Nat Genet. 2008;40:43–50.
Chang TC, Zeitels LR, Hwang HW, et al. Lin-28B transactivation is necessary for Myc-mediated let-7 repression and proliferation. Proc Natl Acad Sci USA. 2009;106:3384–9.
Smith AP, Verrecchia A, Faga G, et al. A positive role for Myc in TGFbeta-induced Snail transcription and epithelial-to-mesenchymal transition. Oncogene. 2009;28:422–30.
Thuault S, Tan EJ, Peinado H, et al. HMGA2 and Smads co-regulate SNAIL1 expression during induction of epithelial-to-mesenchymal transition. J Biol Chem. 2008;283:33437–46.
Tseng LM, Liu CY, Chang KC, et al. CIP2A is a target of bortezomib in human triple negative breast cancer cells. Breast Cancer Res. 2012;14:R68.
Choi YA, Park JS, Park MY, et al. Increase in CIP2A expression is associated with doxorubicin resistance. FEBS Lett. 2011;585:755–60.
Acknowledgments
We are very grateful for the sincere help and excellent technical support by the Laboratory of Cell Biology in Gannan Medical University.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yijun Xue, Gengqing Wu, and Xiaoning Wang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Xue, Y., Wu, G., Wang, X. et al. CIP2A is a predictor of survival and a novel therapeutic target in bladder urothelial cell carcinoma. Med Oncol 30, 406 (2013). https://doi.org/10.1007/s12032-012-0406-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-012-0406-6