Abstract
The 2022 WHO classification reflects increases in the knowledge of the underlying pathogenesis of parathyroid disease. In addition to the classic characteristic features of parathyroid neoplasms, subtleties in histologic features which may indicate an underlying genetic abnormality reflect increased understanding of the clinical manifestations, histologic, and genetic correlation in parathyroid disease. The importance of underlying genetic aberrancies is emphasized due to their significance to the care of the patient. Traditionally, the term “parathyroid hyperplasia” has been applied to multiglandular parathyroid disease; however, the concept of hyperplasia is generally no longer supported in the context of primary hyperparathyroidism since affected glands are usually composed of multiple “clonal” neoplastic proliferations. In light of these findings and management implications for patient care, the 2022 WHO classification endorses primary hyperparathyroidism-related multiglandular parathyroid disease (multiglandular multiple parathyroid adenomas) as a germline susceptibility-driven multiglandular parathyroid neoplasia. From such a perspective, pathologists can provide additional value to genetic triaging by recognizing morphological and immunohistochemical harbingers of MEN1, CDKN1B, MAX, and CDC73-related manifestations. In the current WHO classification, the term “parathyroid hyperplasia” is now used primarily in the setting of secondary hyperplasia which is most often caused by chronic renal failure. In addition to expansion in the histological features, including those that may be suggestive of an underlying genetic abnormality, there are additional nomenclature changes in the 2022 WHO classification reflecting increased understanding of the underlying pathogenesis of parathyroid disease. The new classification no longer endorses the use of “atypical parathyroid adenoma”. This entity is now being replaced with the term of “atypical parathyroid tumor” to reflect a parathyroid neoplasm of uncertain malignant potential. The differential diagnoses of atypical parathyroid tumor are discussed along with the details of worrisome clinical and laboratory findings, and also features that define atypical histological and immunohistochemical findings to qualify for this diagnosis. The histological definition of parathyroid carcinoma still requires one of the following findings: (i) angioinvasion (vascular invasion) characterized by tumor invading through a vessel wall and associated thrombus, or intravascular tumor cells admixed with thrombus, (ii) lymphatic invasion, (iii) perineural (intraneural) invasion, (iv) local malignant invasion into adjacent anatomic structures, or (v) histologically/cytologically documented metastatic disease. In parathyroid carcinomas, the documentation of mitotic activity (e.g., mitoses per 10mm2) and Ki67 labeling index is recommended. Furthermore, the importance of complete submission of parathyroidectomy specimens for microscopic examination, and the crucial role of multiple levels along with ancillary biomarkers have expanded the diagnostic workup of atypical parathyroid tumors and parathyroid carcinoma to ensure accurate characterization of parathyroid neoplasms. The concept of parafibromin deficiency has been expanded upon and term “parafibromin deficient parathyroid neoplasm” is applied to a parathyroid neoplasm showing complete absence of nuclear parafibromin immunoreactivity. Nucleolar loss is considered as abnormal finding that requires further molecular testing to confirm its biological significance. The 2022 WHO classification emphasizes the role of molecular immunohistochemistry in parathyroid disease. By adopting a question–answer framework, this review highlights advances in knowledge of histological features, ancillary studies, and associated genetic findings that increase the understanding of the underlying pathogenesis of parathyroid disease that are now reflected in the updated classification and new entities in the 2022 WHO classification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Advances in the understanding of parathyroid disorders have significantly improved the understanding of parathyroid neoplasia and are reflected in a spectrum of clinicopathological entities, including specific genetic and pathological changes that manifest with multiglandular parathyroid disease. Ancillary biomarkers have also improved the clinical practice and helped to better characterize parathyroid proliferations. This practical review adopted a question–answer framework to provide an overview of the new WHO classification of parathyroid disorders in respect to relevant clinical, pathologic, and molecular features. This review serves as a primer for multidisciplinary team members dealing with parathyroid disorders.
Question 1. Are There Any Nomenclature Changes or New Entities in the 2022 WHO Classification of Parathyroid Tumors?
In addition to expansion in the histological features, including those that may be suggestive of an underlying genetic abnormality, ancillary studies, in more extensive genetic correlates of disease, there are important nomenclature changes in the 2022 WHO classification reflecting increased understanding of the underlying pathogenesis of parathyroid disease.
Primary hyperparathyroidism involving multiple parathyroid glands historically has been traditionally referred to as “parathyroid hyperplasia”. However, it is now known that the multiglandular parathyroid involvement in cases of primary hyperparathyroidism appears to be due to multiple clonal proliferations [1,2,3]. Thus, terms such as multiglandular parathyroid disease and multiple multiglandular parathyroid adenomas have now replaced the historical term “parathyroid hyperplasia”. A characteristics example of this is the involvement of multiple parathyroid glands in the setting of multiple endocrine neoplasia (MEN) type 1 (MEN1) [4,5,6], MEN4 [7], and MEN5 [8] syndromes. Involvement of the parathyroid glands in MEN syndromes may be asymmetrical and can occur in an asynchronous manner [4, 5]. Histologically, the hypercellular parathyroid glands can show nodular proliferations of chief cells as well as other cell types and often lack of rim of normal or atrophic appearing nonlesional parathyroid tissue. As hyperparathyroidism-related multiglandular parathyroid disease appears to be a germline susceptibility-driven multiglandular parathyroid neoplasia, underlying genetic testing may be helpful in identifying underlying possible genetic abnormalities that may affect patient care.
The concept of parafibromin deficiency has been expanded upon, and the term “parafibromin deficient parathyroid neoplasm” is new to the 2022 WHO classification. This term is applied to a parathyroid neoplasm (e.g., parathyroid adenoma, atypical parathyroid tumor, parathyroid carcinoma) showing complete absence of nuclear parafibromin immunoreactivity. Nucleolar loss is considered as abnormal finding that requires further molecular testing to confirm its biological significance. As CDC73 encodes parafibromin, complete loss of nuclear parafibromin immunoreactivity indicates biallelic CDC73 inactivation, often arising in the setting of germline mutation/deletion [9,10,11,12]. The presence of parafibromin expression does not, however, completely exclude the possibility of underlying CDC73 inactivation as point mutations of CDC73 can result in preserved parafibromin expression [13, 14]. A “parafibromin deficient” parathyroid neoplasm is significant as it suggests an underlying germline or somatic CDC73 mutation, and the identification of a “parafibromin deficient” parathyroid neoplasm is also an indication for germline CDC73 mutation testing [9, 11, 12]. Parathyroid adenomas usually retain parafibromin nuclear immunoreactivity unless they are in the setting of underlying germline pathogenic CDC73 variants leading to either hyperparathyroidism jaw tumor (HPT-JT) or familial isolated hyperparathyroidism syndromes. Still, long-term follow-up is recommended as metachronous disease can occur in other glands [13]. In addition to indicating the possibility of underlying germline CDC73 disorder such as HPT-JT syndrome, parafibromin may be helpful in predicting outcome in atypical parathyroid tumors [15, 16]. In addition to the high life risk of parathyroid carcinoma in the setting of HPT-JT syndrome, somatic only CDC73 mutations are also associated with sporadic parathyroid carcinoma [10, 13, 17, 18]. Although parathyroid adenomas account for most parathyroid disease in HPT-JT, the lifetime risk of parathyroid carcinoma is thought to be up to 15% [19, 20]. Parathyroid carcinoma is rare overall but occurs in up to 15% of individuals with HPT-JT. Thus, germline CDC73 mutation testing is recommended for all individuals diagnosed with parathyroid carcinoma. Up to 30% of apparently sporadic parathyroid carcinomas are associated with underlying germline CDC73 inactivation (Fig. 1) [9, 11,12,13, 21,22,23].
Proposed scheme for triaging parathyroid tumors using histology, immunohistochemistry, and molecular genetics. Parathyroid tumor classification is based on histopathology, in which several factors are weighed before a diagnosis is made. Tumors lacking (or exhibiting only few) atypical features are diagnosed as parathyroid adenoma, while atypical parathyroid tumors are lesions with several worrisome histological and/or immunohistochemical features in which a differential diagnosis of parathyroid carcinoma is considered, yet definite criteria of malignancy are lacking. Parathyroid carcinoma is a diagnosis reserved for cases displaying one or several definite criteria of malignancy. Parafibromin (PFIB) immunohistochemistry is recommended for atypical parathyroid tumors and parathyroid carcinoma in order to appreciate the risk of tumor recurrence and to indicate the possibility of an underlying CDC73 gene mutation. PFIB triaging of parathyroid adenoma is not recommended in clinical routine, but could be considered in specific instances (young patients with multiple tumors) in order to increase the likelihood of identifying an unknown germline CDC73 gene mutation. *Other immunohistochemical aberrancies that are also a recurrent feature of parathyroid carcinoma, apart from PFIB. Created with BioRender.com
Atypical parathyroid tumor is new to the 2022 WHO classification. Atypical parathyroid tumor defined as a parathyroid neoplasm that demonstrates atypical cytological and architectural features that are worrisome for parathyroid carcinoma, but lacks unequivocal capsular, vascular, or perineural invasion or invasion into adjacent structures or metastases. These tumors can have histologic features often seen in parathyroid carcinoma including adherence to adjacent structures, monotonous sheet-like or trabecular growth, cytologic atypia, fibrosis, including band-like fibrosis, and cells extending into but not through the capsule, but they do not show unequivocal invasion as would be required for diagnosis of parathyroid carcinoma (Figs. 2 and 3). Conventional parathyroid adenomas can show areas of fibrosis particularly if they are large or if there has been prior fine needle aspiration or trauma (including ethanol injection). A focal area of fibrosis or an occasional mitotic figure is insufficient for designation of parathyroid adenoma as an atypical parathyroid tumor. Therefore, the term atypical parathyroid tumor is reserved for a parathyroid neoplasm with atypical features unrelated to a previous manipulation for which differential diagnosis is parathyroid carcinoma (Fig. 1). Atypical parathyroid tumors are considered as a neoplasm of uncertain malignant potential and usually warrant long-term follow-up.
Histological features of atypical parathyroid tumors. A Trabecular, nested and solid areas of chief cells are commonly noted in atypical parathyroid tumors. B Irregular fibrous bands can be visualized, creating a nodular appearance of tumor cells. C Fibrosis highlighted by a van Gieson stain. Note the difficulties in interpreting the tumor cell relationship to the true tumor capsule in tumors with extensive, intercalating fibrosis. D Nuclear pleomorphism and an increased mitotic count are features coupled to atypical parathyroid tumors
Diagnostic predicaments in atypical parathyroid tumors. A Parathyroid tumors often exhibit peliosis (erythrocyte-filled cavitations without an endothelial layer mimicking a true blood vessel), and tumor cells may falsely appear to invade a vascular space. CD34 (endothelial marker) and CD61 (thrombus identification) would both be negative in this case. B Same tumor exhibiting fibrous bands, mimicking capsular invasion. C Atypical parathyroid tumors often display an increased Ki-67 labeling index similarly to parathyroid carcinoma. D Atypical parathyroid tumor displaying absent parafibromin immunoreactivity. Note the retained expression in the normal rim (marked with asterisk). This tumor was found to carry a germline CDC73 gene mutation, and the risk of recurrence is not neglectable
Question 2. What Are the Clinicopathological Correlates of Hyperparathyroidism in the 2022 WHO Classification? What Clinical Information Is Critical for Pathologist to be Provided in the Evaluation of Parathyroidectomy Specimens?
The hallmark of hyperparathyroidism is the presence of autonomous PTH secretion. With the advent of screening programs, patients are more frequently diagnosed in the absence of classical signs (e.g., nephrolithiasis, osteitis fibrosis cystica, ileus, constipation, polyuria, polydipsia) of hyperparathyroidism and also with normocalcemic manifestations [1, 24, 25].
Based on clinical and laboratory findings, autonomous PTH secretion is subtyped into three distinct clinicopathological forms including (i) primary hyperparathyroidism due to clonal (neoplastic) proliferation(s), (ii) secondary hyperparathyroidism due to underlying chronic disorder (e.g., chronic renal failure) or chronic stimulation (e.g., lithium administration) that interferes with PTH secretion, and (iii) tertiary hyperparathyroidism due to clonal expansion in refractory secondary hyperparathyroidism [1]. The distinction between clinicopathological subtypes is of significance since secondary and tertiary hyperparathyroidism almost always manifest with multiglandular parathyroid disease, whereas primary hyperparathyroidism often manifests with a uniglandular parathyroid disease [1].
Autonomous PTH secretion is reflected in enlarged and heavy parathyroid gland(s). A normal parathyroid gland measures up to 6–8 mm and does not exceed a weight of weigh 40–60 mg [1]; therefore, any figure beyond the upper limit of normal ranges should be considered pathological. A cellular parenchyma alone is not always a sign of pathological disease in the absence of increased glandular weight. For instance, it is not uncommon to identify vitamin D deficiency-related slightly cellular and slightly enlarged parathyroid glands. Moreover, in the case of parathyroid lipoadenoma, the cellularity may be sparse in a parathyroid gland that is enlarged and increased in glandular weight [26, 27]. Therefore, it is crucial to accurately document the weight of a parathyroid gland [1]. Nevertheless, most abnormal parathyroids are enlarged and cellular, and they are typically reflected in either parathyroid hyperplasia or parathyroid neoplasia.
Traditionally, the term “parathyroid hyperplasia” has been applied to multiglandular parathyroid disease; however, the concept of hyperplasia is generally no longer supported in the context of primary hyperparathyroidism since affected glands are usually composed of multiple “clonal” neoplastic proliferations [1,2,3]. In light of these findings and management implications for patient care, the 2022 WHO classification endorses primary hyperparathyroidism-related multiglandular parathyroid disease as a germline susceptibility-driven multiglandular parathyroid neoplasia. Therefore, germline screening of affected individuals is recommended, taking into consideration the overall morphological and molecular immunohistochemistry findings as well as clinical and laboratory findings. While there are some morphological and immunohistochemical harbingers of inherited hyperparathyroidism, pathologists must be given the appropriate clinical information on whether the patient clinically has a primary or secondary/tertiary hyperparathyroidism.
In the 2022 WHO classification, the spectrum of parathyroid neoplasms encompasses parathyroid adenoma (benign parathyroid tumor), atypical parathyroid tumor (parathyroid tumor of uncertain malignant potential), and parathyroid carcinoma. This morphological spectrum is mainly reflected in all patients with primary hyperparathyroidism. Epidemiology data from several countries show an increase in the frequency of parathyroid carcinoma diagnoses [28,29,30,31,32]; however, parathyroid adenomas are still the most common neoplastic correlates of autonomous PTH secretion. Patients with tertiary hyperparathyroidism may, although extremely rare, develop parathyroid carcinoma [33, 34].
The 2022 WHO bluebook reviews many aspects of parathyroid disorders. Pathologists must be provided relevant clinical and laboratory findings when assessing parathyroidectomy specimens. In addition to precise weight and measurements of a parathyroid gland, the clinical type of hyperparathyroidism (primary vs secondary vs tertiary), the number of involved parathyroid glands, the family history of hyperparathyroidism or genetic susceptibility in the family, the history of a former manipulation to parathyroid glands (e.g., fine-needle aspiration biopsy, PTH washout, ethanol injection), the preoperative imaging results, the preoperative serum calcium, PTH and vitamin D levels, and the results of intraoperative PTH assays along with postoperative calcium and PTH levels are all critical parameters in the accurate pathological characterization of hyperparathyroidism [1, 35]. The identification of significant drop of intraoperative PTH (usually defined as greater than 50%) indicates the removal of the source of hyperparathyroidism and often correlates with a uniglandular parathyroid disease [1]. This information provides a guidance to surgeons on the extent of parathyroid exploration especially when dealing with a Sestamibi and CT-scan non-localizing parathyroid disease.
There are also clinical and laboratory findings that should alert the diagnosticians to the possibility of a parathyroid carcinoma. These include (i) palpable neck mass, (ii) parathyroid gland measuring > 3 cm, (iii) severe hypercalcemia characterized one of the following: > 3 mmol/L, > 12 mg/dL, 3–4 mg over the upper limit of normal, (iv) significantly elevated PTH levels (> 3 times the upper limit of normal, usually 10 times the upper limit of normal), (iv) 3rd to 2nd generation PTH ratio > 1, and (v) intraoperative observation of adhesion to adjacent structures [35,36,37,38,39,40,41,42,43,44].
In the absence of metastatic tumor spread, these worrisome clinical and laboratory findings alone do not warrant a definitive diagnosis of parathyroid carcinoma. The final diagnosis of malignancy should be based on histopathological examination of an entirely submitted parathyroidectomy specimen. The new WHO classification outlines diagnostic criteria applied to atypical parathyroid tumors and parathyroid carcinomas, and provides information on the role of ancillary techniques. The details of various clinicopathological manifestations are discussed in other questions of this review article.
Question 3. What Are the Clinicopathological Correlates of Parathyroid Adenomas in the 2022 WHO Classification? What Does Multiglandular Parathyroid Adenomas Mean?
Clinically, parathyroid adenoma has evolved from a rare disease presenting with renal stones, bone pain due to bone loss, and osteitis fibrosa cystica [45] to a frequently diagnosed often asymptomatic disease identified on elevated serum calcium levels. The extent of screening of serum calcium levels in the general population correlates with the rate of asymptomatic hyperparathyroidism [46]. Moreover, increasing measurements of PTH in normocalcemic patients leads to an increased detection rate of “normocalcemic primary hyperparathyroidism”, with a prevalence of up to 3.4% in postmenopausal women as reported in a Swedish study [47]. These individuals may benefit from surgery for preservation of bone density and reduction of renal stones, but an individual approach is still suggested until further data are available [48]. The size of the parathyroid adenoma correlates with calcium/PTH level. For instance, smaller adenomas (40–100 mg) are associated with lower to normal serum levels of calcium and mild to asymptomatic hyperparathyroidism [49], whereas parathyroid adenomas > 1 cm are more frequently associated with higher levels of serum calcium and PTH and increased possibility of bone disease or hypercalcemic crisis [50]. Although rare, “giant parathyroid adenomas” can occur and measure several centimeters [51].
Histologically, parathyroid adenoma is a well-delineated neoplasm composed of chief, transitional, oncocytic, and water clear cells (Fig. 4). A rim of normal appearing parathyroid tissue is often observed in over half the cases (Fig. 5) [52]. A rim is identified more often when the gland is transected horizontal to the vascular pole. Stromal fat is usually markedly decreased or absent in adenomas. Chief cells show small regular nuclei without nucleoli and scant cytoplasm, and nuclear pleomorphism is usually mild, when present. There is a delicate network of capillaries, and chief cells often show a palisading along these capillaries at the border of the nests. Follicular structures are frequently formed, and if follicular structures are prominent can be mistake in for thyroid tissue (Fig. 6). While immunopositivity for PTH can confirm tissue as parathyroid, this distinction may be difficult during intraoperative consultation. However, the following features may assist pathologists in the distinction of parathyroid origin: distinct cell membranes, the lack of bi-refringent calcium-oxalate crystals in the material within follicular structures, and/or the presence of intracellular lipid. In addition, parathyroid cells are also generally more vacuolated and smaller than thyrocytes, often have empty follicles, and may have rounder nuclei with denser chromatin than thyrocytes.
Focal oncocytic change can occur in the background of a chief-cell predominant adenoma. However, the term “oncocytic parathyroid adenoma” is applied when the tumor consists of > 75% of oncocytic cells (Fig. 7). These adenomas are larger [53, 54], with possibly higher preoperative serum calcium levels (10.8 vs 10.4 mg/dL) [53] and are more frequently localized with Sestamibi scan [55].
Water clear cell parathyroid adenomas are composed entirely of “water clear” cells and represent 1.5 of 1000 parathyroid adenomas (Fig. 8) [56]. The cytoplasm is distended and vacuolated, with hyperchromatic nuclei often allocated to the basal aspect of the cell. The cell membranes are clearly visible. The granular vacuolization is most likely attributed to an accumulation of glycogen, as positive periodic acid-Schiff (PAS) and negative diastase-PAS reactions usually are reported in water clear cell adenoma [57, 58]. Ultrastructurally, the glycogen-rich vacuoles observed in parathyroid water clear cell lesions appear to be derived from dilated cisterns of the granular endoplasmic reticulum, alternatively from secretory Golgi-derived granules [59]. As in chief cell adenomas, the stromal fat content is reduced or absent, and the cells stain positive for chromogranin A, PTH (Fig. 9) and GATA3 [60]. These lesions are often larger than chief cell adenomas, but may be difficult to locate by scintigraphy. The molecular pathogenesis of these tumors is largely unknown; however, their peculiar features warrant further investigations.
Degenerative changes, including cyst formation and hemorrhage, may occur in larger adenomas [56]. If these cystic changes comprise > 50% of the tumor, the terminology cystic parathyroid adenoma may be used. These tumors can be misinterpreted as thyroid cysts in scintigraphy due to lack of MIBI accumulation. These cystic changes can be associated with areas of fibrosis and focal calcifications [61], not to be misinterpreted as signs of malignancy.
Parathyroid lipoadenomas are tumors with an increase in both parathyroid parenchymal and adipose tissue, with more than 50% of the glandular volume consisting of adipose tissue (Fig. 10) [26, 27, 62]. As a result, these tumors may not be localized on Sestamibi scan [27]. The abnormal weight of the gland (> 40–60 mg) is an important finding that should alert the diagnostician to the possibility of a parathyroid lipoadenoma in the appropriate morphological context and clinical setting [26, 27]. A significant drop of intraoperative PTH and evidence of postoperative biochemical cure also supports the diagnosis [26, 27]. Middle-aged female patients are slightly overrepresented among individuals with lipoma adenomas. The molecular etiology is unknown.
Up to 15% of individual with primary hyperparathyroidism (PHPT) show multiglandular disease with two or more parathyroid adenomas. This affects more frequently the superior parathyroid glands than the inferior glands [63]. Multiglandular disease, as well as male sex, age of occurrence under 45 years, and malignancy are factors associated with inherited hyperparathyroidism and should prompt consideration of genetic testing in light of morphological and molecular immunohistochemistry findings [64]. Multiglandular parathyroid disease was formerly regarded as a type of “hyperplasia”, but this nomenclature is a misnomer as multiglandular disease in the primary hyperparathyroidism is now generally thought to be composed of several synchronous or metachronous monoclonal proliferations.
From an immunohistochemical standpoint, parathyroid adenomas show diffuse immunopositivity for PTH and GATA3, as well as chromogranin-A and may show staining for synaptophysin [10]. Thyroid follicular cell markers TTF1, thyroglobulin, and monoclonal PAX8 are negative. The use of some polyclonal PAX8 antibodies may show weak to moderate reactivity in parathyroid proliferations as well as in other neuroendocrine neoplasms. Therefore, pathologists should be aware of the clone of PAX8 antibodies used in their laboratory. Nuclear parafibromin staining is almost always present (Fig. 11), except for rare adenomas arising in individuals with pathogenic germline CDC73 variants [13, 65].
Ancillary immunohistochemical markers in parathyroid tumors. Whereas parathyroid adenomas (left) recurrently display positivity for parafibromin (PFIB) and APC, they often stain negative for galectin-3 (GAL-3) and PGP9.5. The Ki-67 index is often below 1%. Atypical parathyroid tumors (center) may exhibit a variable immunohistochemical phenotype, in which cases with risk of recurrences often are parafibromin-deficient and display immunophenotypes mimicking that of parathyroid carcinomas (right)
Question 4. What Are the Clinicopathological Correlates of Parathyroid Carcinoma in the 2022 WHO Classification?
Histological criteria for the pathological diagnosis of parathyroid carcinoma have not changed under the 2022 WHO classification. However, the definition of what constitutes an invasive growth was clearly discussed in this classification. Therefore, the histological diagnosis of parathyroid carcinoma is restricted to a parathyroid neoplasm that shows one of the followings: (i) angioinvasion (vascular invasion), (ii) lymphatic invasion, (iii) perineural (or intraneural) invasion, (iv) local malignant invasion into adjacent anatomic structures, or (v) histologically/cytologically documented metastatic disease (Fig. 12).
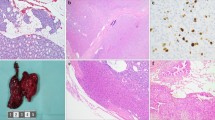
Parathyroid carcinoma. A This is an example of a parathyroid carcinoma that is angioinvasive. Although parathyroid adenomas and atypical parathyroid tumors can have some atypical features such as mitotic activity in fibrosis, they do not show on equivocal capsular, vascular, or perineural invasion. B Angioinvasion with tumor within a vessel associated with thrombus. C CD61 immunohistochemistry highlighting the platelet fibrin thrombus complex. D GATA3 immunostain highlighting the intravascular tumor cells
The complete submission of a parathyroid neoplasm is essential to assess the status of invasive growth. Moreover, multiple levels can also assist the assessment of invasive growth. Angioinvasion is defined as tumor invading through a vessel wall and associated thrombus, or intravascular tumor cells admixed with thrombus (Fig. 12) [35, 38, 66]. Given the fenestrated endothelium of endocrine tissues, angioinvasion is assessed at the intersection of the tumor and non-tumorous parenchyma, but not within the tumor substance. When a fibrin/thrombus complex is subtle, intravascular tumor cells (positive for GATA3 and PTH) admixed with platelet–fibrin thrombus complex can be highlighted using the Martius-Scarlet blue histochemistry or CD61 immunohistochemistry (Fig. 12). Lymphatic invasion can be confirmed using D2-40 immunohistochemistry. Perineural invasion requires at least the involvement of the epineurium.
Some parathyroid neoplasms may be associated with complete or incomplete encapsulation, the invasion into the lesion capsule does not qualify for a diagnosis of carcinoma since invasion requires local invasion into adjacent structures. An intrathyroidal parathyroid neoplasm or superior glands that are often embedded in the thyroid pseudocapsule, these features should be revisited when assessing invasive growth in such manifestations.
The differential diagnoses of parathyroid carcinoma include atypical parathyroid tumor, parathyromatosis (microscopic foci of parathyroid tissue that usually grows at the site of a former surgery or biopsy due to an implantation of lesional parathyroid tissue), a benign parathyroid proliferation (adenoma or hyperplasia) with worrisome histologic alterations following fine needle aspiration or ethanol injection, and contour irregularities seen in parathyroids from patients with longstanding secondary/tertiary hyperparathyroidism [67,68,69,70,71,72,73,74]. The clinical information and biomarker studies can narrow down the differential diagnoses.
Longstanding secondary or tertiary hyperparathyroidism may be associated with enlarged parathyroid glands with some atypical features including contour irregularity that can mimic invasive growth. Thus, caution is urged before the diagnosis of parathyroid carcinoma is made in the setting of advanced chronic renal failure. A malignant diagnosis should only be offered when there is unequivocal angioinvasion, spread outside the neck, or very marked invasive growth — for example unequivocal invasion into esophagus, or skeletal muscle rather than just microscopic extension into the immediate adipose tissue.
Another important aspect of the new WHO classification is related to an increased emphasis on parathyroid carcinoma as a potentially hereditary disease associated with HPT-JT or isolated familial hyperparathyroidism syndrome due to pathogenic germline CDC73 variants which encodes parafibromin [9, 14, 19, 20, 75,76,77]. Thus, the possibility of germline susceptibility should be considered in all patients with parafibromin-deficient parathyroid carcinoma even in the absence of a suggestive personal history [19, 21, 78]. Sporadic and what was clinically thought to be apparently sporadic-looking parathyroid carcinomas are often associated with biallelic CDC73 mutation/inactivation [21, 22, 79,80,81,82]. The CDC73 mutations are frequently germline, indicative of de novo mutations or undetected germline alterations [21, 22, 83]. Given the role of parafibromin in malignancy, it has been proposed that a lower threshold for invasive growth may be needed to support the diagnosis of parathyroid carcinoma in parafibromin deficient parathyroid tumors [9].
The new classification has also brought an emphasis on the judicious use of immunohistochemical biomarkers to support a diagnosis of malignancy in the differential diagnosis with parathyroid carcinoma. Among these, loss of expression of parafibromin, APC, RB, E-cadherin, p27, Bcl-2a, mdm-2, and 5-hmC and positivity for PGP9.5, galectin-3, hTERT, and p53 overexpression along with increased Ki67 labeling index (often > 5%) [10, 11, 13, 15, 17, 35, 38, 66, 84,85,86,87,88,89,90,91] are considered biomarker correlates of parathyroid carcinoma. Although no individual marker is definitive, combinations of these markers are particularly useful in difficult to classify cases [10, 17, 85,86,87, 89, 92, 93]. The details of these biomarkers are discussed in the question that deals with ancillary tools.
Question 5. How Are Atypical Parathyroid Tumors Defined in the 2022 WHO Classification?
Atypical parathyroid tumor is defined as a parathyroid neoplasm that demonstrates atypical cytological and architectural features (Figs. 1 and 13), but lacks unequivocal capsular, vascular, or perineural invasion or invasion into adjacent structures or metastases. Atypical parathyroid tumors usually occur sporadically but can occur in the setting of inherited hyperparathyroidism [94]. The serum calcium levels are often intermediate between that of a parathyroid adenoma and a parathyroid carcinoma.
Atypical parathyroid tumors show some worrisome histologic features often seen in parathyroid carcinoma including adherence to adjacent structures, monotonous sheet-like or trabecular growth, cytologic atypia, fibrosis (which can be band-like, tumor cells extending into but not through the tumor capsule), and mitotic activity (> 5 per 50 high-power fields/ ~ 10mm2), but they do not show unequivocal invasion as would be required for diagnosis of parathyroid carcinoma (Figs. 2 and 3). Atypical parathyroid tumors do not show full-thickness capsular invasion, vascular invasion, perineural invasion, or invasion into adjacent structures as would be diagnostic for parathyroid carcinoma.
Atypical parathyroid tumors are composed predominantly of chief cells with variable amounts of oxyphil and transitional cells and may show monotonous, solid growth of sheets of cells in closely packed nests similar to parathyroid carcinoma (Fig. 2). Mitotic activity can be seen in benign and malignant parathyroid disease, but a mitotic activity that exceeds 5 mitoses per 50 high-power fields/ ~ 10mm2 in association with coagulative tumor necrosis, macronucleoli, atypical mitoses, or Ki67 proliferation index > 5% are highly worrisome features for malignancy (Figs. 1 and 3) [94, 95]. Parathyroid carcinoma is often have a Ki-67 labeling index of greater than 5%, parathyroid adenomas typically have a much lower labeling index whilst the proliferative index of atypical parathyroid tumors may be intermediate (Fig. 14). However, a definitive diagnosis of parathyroid carcinoma requires invasive growth or metastasis as discussed in the former question (Fig. 1).
Conventional parathyroid adenomas can show areas of fibrosis particularly if they are large. Fibrosis can also be seen with prior manipulation such as fine-needle aspiration biopsy or cystic parathyroid neoplasm in which there may be hemosiderin deposition or irregularity in the contour to suggest prior trauma [67, 72]. Fibrosis may also be seen in the setting of secondary or tertiary hyperparathyroidism. Conventional parathyroid adenomas can also have occasional mitotic figures. The presence of focal fibrosis or occasional mitotic figures (< 5 per 50 high-power fields/ ~ 10mm2) is insufficient to qualify a parathyroid neoplasm as an atypical parathyroid tumor. The term atypical parathyroid tumor is reserved for a parathyroid neoplasm with atypical features for which the differential diagnosis is parathyroid carcinoma. These features have been reflected in the algorithm provided (Fig. 1).
Immunohistochemically, atypical parathyroid tumors show positivity for PTH, chromogranin-A, and GATA3. Many biomarkers, including Ki67, PGP9.5, cyclin D1, p27, P53, galectin 3, RB, Bcl-2a, mdm2, and E-cadherin, have been studied in parathyroid neoplasms (Fig. 11) [10, 17, 54, 84, 85, 93, 96,97,98]. However, these are not able to consistently differentiate parathyroid carcinomas from adenomas, but may provide help in the diagnostic workup of parathyroid tumors showing atypical features.
Parafibromin is encoded for by CDC73, and complete absence of nuclear parafibromin immunoreactivity and parathyroid neoplasm is regarded as “parafibromin deficiency” indicating an underlying biallelic somatic or germline CDC73 inactivation [10,11,12, 91]. However, point mutations of CDC73 may result in preserved parafibromin expression, thus the presence of parafibromin does not rule out the possibility of an underlying germline pathogenic variants [13, 14]. Parathyroid adenomas generally retain nuclear immunoreactivity for parafibromin, however those in the setting of underlying CDC73 mutations (such as hyperparathyroidism jaw tumor syndrome) will also show loss of parafibromin [13]. Somatic CDC73 mutations are also associated with sporadic parathyroid carcinoma [10, 13, 17, 18]. Evidence suggests that parafibromin may be helpful in predicting outcome in atypical parathyroid tumors [15, 16]. For instance, parafibromin deficient atypical parathyroid tumors have been shown to develop metachronous disease in other glands, and also as true recurrence [11, 15, 16, 91]. Thus, long-term follow-up is indicated for parafibromin deficient parathyroid neoplasms [11, 15, 16, 91]. The new classification also encourages a routine germline CDC73 mutation testing in the setting of a parafibromin deficient parathyroid neoplasm, as well as in all parathyroid carcinomas (Fig. 1) [11, 12, 91].
In summary, the 2022 WHO classification categorizes atypical parathyroid tumor as a neoplasm of uncertain malignant potential. Most atypical parathyroid tumors behave similarly to parathyroid adenomas and do not recur after excision, however recurrent disease, often metachronous, and metastasis have been reported especially in the context of parafibromin deficiency [9, 11, 15, 16]. Therefore, a clinical and biochemical follow-up only is recommended for the management of this tumor type.
Question 6. Which Ancillary Tools Should Pathologists Consider Utilizing in the Accurate Assessment of Parathyroid Tumors?
While the diagnosis of an atypical parathyroid tumor or parathyroid carcinoma is strictly based on histopathological criteria, there are several ancillary markers that the pathologist could use in the diagnostic work-up and/or to identify underlying genetic aberrations of value in the clinical approach to of the individual patient. Although the vast majority of parathyroid tumors are benign and often straight-forward to diagnose with routine morphology alone, there are several instances in which immunohistochemistry may be of direct value to the pathologist.
Parathyroid cells show neuroendocrine differentiation, and therefore, parathyroid tumors exhibit immunoreactivity with chromogranin A and occasionally also to synaptophysin, whereas expression of second-generation neuroendocrine markers such INSM1 seem to be absent [99,100,101]. Moreover, normal parathyroid cells and tumors almost always stain positive for PTH and GATA3 and are consistently negative for TTF1 — thereby setting them apart from thyroid tissue. While monoclonal PAX8 antibodies are negative in parathyroid tissues, other polyclonal PAX8 antibodies may shows staining in parathyroid tumors and should therefore not be used to distinguish between parathyroid and thyroid [102].
After correctly identifying a parathyroid tumor, the pathologist must assess the risk of malignancy. While the gold standard of this procedure is based upon histologic assessment of malignant features discussed elsewhere in this review, there are several immunohistochemical markers available to aid in the evaluation of potentially troublesome parathyroid tumors. Most of this research has been focused on identifying markers that distinguish parathyroid carcinoma from adenoma, and studies have found significant differences in expression for many proteins — of which some of the most important are listed in Fig. 11. Most notably, parathyroid adenomas often retain their immunoreactivity for parafibromin, APC, E-cadherin, p27, RB, Bcl-2a, mdm2, and 5-hmC, while one or several of these markers usually exhibit negative staining in parathyroid carcinoma (Fig. 15) [10, 11, 17, 84, 90, 91, 103]. On the contrary, while parathyroid carcinomas often show PGP9.5, Galectin-3, and p53 expression, these markers are not typically expressed in parathyroid adenomas (Figs. 11, 15, and 16) [13, 66, 86, 87, 89, 104]. The increased proliferative indices of parathyroid carcinoma can be identified through a Ki-67 labeling index, which is usually above 5%, while parathyroid adenomas typically display much lower proliferative indices (Fig. 11) [84, 105, 106]. Even so, the overlap between parathyroid adenomas, hyperplasias, and carcinomas in terms of the proliferation labeling index is considerable, limiting the utility of this marker particularly if it not used in combination with others [107]. There is no formal grading system in parathyroid carcinomas, but the 2022 WHO classification encourages the use of Ki-67 immunohistochemistry in parathyroid carcinomas (Fig. 17).
Immunohistochemical features of parathyroid adenoma. A Retained nuclear parafibromin expression is noted in virtually all parathyroid adenomas without CDC73 gene aberrancies. B PGP9.5 expression is generally absent. C Cytoplasmic APC immunoreactivity is observed in the majority of parathyroid adenomas, while lost in subsets of parathyroid carcinoma. D Galectin-3 expression may occasionally be seen in atypical parathyroid tumors and parathyroid carcinoma but is usually absent in adenoma. E CyclinD1 overexpression is recurrently seen in parathyroid adenoma. F RB expression may be heterogenous in parathyroid adenoma, but there is no global loss
Histological and immunohistochemical features of parafibromin-deficient parathyroid tumors. A Parathyroid carcinoma displaying sheet-like growth, eosinophilic cytoplasm, nuclear enlargement and perinuclear cytoplasmic clearing. B This tumor stained diffusely negative for parafibromin, while internal controls (fibroblasts, endothelial cells) are weakly positive. C The same cases showed absence of APC immunoreactivity, which has also been coupled to parathyroid malignancy. D PGP9.5 expression was diffusely positive, also supporting the diagnosis
Other biomarkers such as the bona fide parathyroid oncogene CyclinD1 is up-regulated in parathyroid adenoma and carcinoma alike, and thus displays reduced specificity towards malignant disease (Fig. 15) [65, 108, 109]. Similarly, loss of Rb protein expression was initially suggested to be highly specific for loss of heterozygosity of the RB1 gene locus, a feature seen in some parathyroid carcinomas [110], but ensuing studies found this genetic aberrancy also to be present in subsets of parathyroid adenomas [106, 111]. Also, the Rb stain may be heterogenous even in cases with retained RB1 alleles, making the interpretation of this marker difficult (Fig. 15). Nevertheless, the global loss of Rb expression is considered as a concerning finding.
Given the association between parafibromin (protein encoded by CDC73) expression and CDC73-mutations that are enriched in parathyroid carcinomas, the 2022 WHO classification puts emphasis on the use of parafibromin immunohistochemistry as a clinically useful marker. Complete loss of nuclear parafibromin immunoreactivity in all tumor cells identifies a parathyroid tumor as “parafibromin-deficient”, a phenomenon highly correlated to underlying CDC73 gene mutations, irrespective of whether the variant is found in somatic or germline tissues [9]. Mutations are often deleterious and accompanied with deletions of the wild-type allele in somatic tissues [21, 22, 79]. Alternate modes of parafibromin dysregulation apart from CDC73 gene mutations, such as aberrant CDC73 promoter methylation, are not recurrent themes in parathyroid tumors [112, 113]. While some authors report diffuse loss of nuclear expression in the presence of internal positive controls (fibroblasts, endothelial cells) in CDC73 gene–mutated cases (Fig. 16), other groups have observed a reduction of the proportion of parafibromin positive cell nuclei rather than a complete absence — possibly due to methodological differences in the staining protocol or technical issues or difficulties (Fig. 18) [9, 11, 13, 82, 114]. Thus, additional genetic testing may be suggested in both situations. However, in the 2022 WHO classification, complete nuclear loss of expression of parafibromin is considered as parafibromin-deficiency. Subsets of cases may show loss of nucleolar parafibromin expression and concurrent retained nuclear staining, possibly signifying underlying CDC73 gene mutations in the nucleolar localization signal (NoS) sequence (Fig. 18) [11, 115, 116]. As the disruption of nucleolar parafibromin also may drive parathyroid tumorigenesis, this finding may be considered as indicating the possibility of underlying pathogenic mutation [117]. Therefore, the loss of nucleolar reactivity requires molecular testing to confirm its biological significance. A genotype–phenotype correlation has been suggested, in which the authors noted that parafibromin-deficient tumors have distinct features as discussed in the last question of this review.
Aberrant parafibromin immunostaining in parathyroid carcinoma. A Parathyroid carcinoma exhibiting partial loss of nuclear parafibromin immunoreactivity. This pattern has been reported in CDC73 mutated parathyroid tumors and has been interpreted as parafibromin-deficient by some institutions. Increased Ki-67 labeling index in the same case. B Nucleolar loss of parafibromin immunoreactivity may be coupled to CDC73 missense mutations perturbing the nucleolar localization signals of this protein
A parafibromin-deficient phenotype can occasionally be seen in parathyroid adenomas (particularly in the setting of underlying pathogenic germline CDC73 variants), but parafibromin deficiency may be more frequently observed in atypical parathyroid tumors and is highly prevalent among parathyroid carcinomas. The possibility of a seemingly sporadic looking parathyroid adenoma that arises in the background of germline pathogenic CDC73 variants is not an uncommon event in the absence of family history or other manifestations of HPT-JT syndrome [19, 22, 65]. In the absence of germline CDC73 variants, a parafibromin-deficient parathyroid adenoma diagnosis may be due to a somatic CDC73 gene mutation leading to sporadic parathyroid adenomas often with cystic features. Therefore, individuals with parafibromin-deficient parathyroid neoplasms should undergo CDC73 gene sequencing to avoid missing a potential germline alteration (that can present as a de novo event in the proband), but with the notion that the genetic aberrancy may be somatic if germline (constitutional) CDC73 screening is negative [16]. In some series, the proportion of parafibromin-deficient atypical parathyroid tumors is equal to that of parathyroid carcinoma, a finding that further supports a shared molecular phenotype between these groups [118]. Parafibromin deficiency in an atypical parathyroid tumor is a particularly worrisome for the possibility of aggressive behavior as discussed in the former question.
Apart from immunohistochemistry alone, various combinations of immunohistochemical and in situ hybridization approaches have also been evaluated, but these observations need confirmatory studies before being recommended in the clinical setting [100].
Question 7. What Are the Molecular Correlates of Parathyroid Tumors? Are There any Diagnostic Molecular Studies in the Workup of Parathyroid Tumors?
Deleterious germline mutations of the MEN1 gene on chromosome 11q13 underlie the MEN1 syndrome in which multiglandular primary hyperparathyroidism is the cardinal disease, and it is therefore not surprising to find somatic MEN1 mutations and deletions as the main genetic abnormality in sporadic parathyroid adenomas as well [119,120,121,122]. The MEN1 mutations are often accompanied by loss of heterozygosity (LOH) of the wild-type allele, thereby fulfilling the two-hit hypothesis for a bona fide tumor suppressor gene. MEN1 encodes menin, a ubiquitously expressed protein with a variety of cellular functions, affecting specific transcription factors as well as epigenetic programs through various histone modifications [18]. Specifically, menin inhibits the JunD transcription factor, which in turn is known to activate gene programs coupled to proliferation [123]. Moreover, menin mediates increased tri-methylation of H3K4, allowing an opening of the chromatin which in turn facilitate gene transcription (Fig. 19) [124]. Beyond MEN1 aberrancies, somatic mutations in other genes propelling the formation of parathyroid adenomas are rarely described [125,126,127]. Interestingly, the CDC73 gene encoding parafibromin is recurrently mutated in parathyroid tumors with unknown or established malignant potential (atypical parathyroid tumors and parathyroid carcinoma, respectively). But it should be noted that small subsets of cystic parathyroid adenomas also may harbor somatic mutations in this gene [65]. Other recurrent mechanisms of interest in parathyroid adenoma include overexpression of the proto-oncogene cyclin D1 (encoded by the CCND1 gene) is found in large subsets of parathyroid adenomas [108, 109]. In rare instances, this phenomenon is due to a chromosome 11 inversion, bringing the CCND1 gene under regulation from the PTH gene promoter [128], but aberrant promoter methylation of so-called cyclin dependent kinase inhibitors (CDKIs) may also cause cyclin D1 up-regulation [129]. Cyclin D1 associates with the CDK4 complex and promotes passage through the G1 phase of the cell cycle by inhibiting the retinoblastoma protein (Rb), so up-regulation of cyclin D1 will promote proliferation (Fig. 19) [130]. Other genes with altered expression levels in parathyroid adenoma compared to normal tissues include the observed down-regulation of CASR and VDR mRNA, two main parathyroid “brake pedal function” genes that normally inhibit the proliferative activity of the parathyroid glands when binding to their ligands calcium and vitamin D, respectively (Fig. 19) [131].
Parathyroid idle state vs adenoma. Schematic overview of normal parathyroid cell regulation (left) compared to somatic molecular alterations underlying the development of parathyroid adenoma (right). Under normal physiological conditions, the normal parathyroid cell is idle. Extracellular calcium binds to the G-protein coupled transmembrane calcium sensing receptor (CaSR), causing a reduction of PTH secretion. Likewise, activated vitamin D (D3) will bind the nuclear vitamin D receptor (VDR), also inhibiting parathyroid cell proliferation. The proliferative state is also regulated by the retinoblastoma protein (pRb), a nuclear tumor suppressor protein that promotes cell cycle arrest. Menin (encoded by the MEN1 tumor suppressor gene) is abundantly expressed in the nuclear compartment, which in turn represses the JunD transcription factor from activating gene programs leading to proliferation, while simultaneously promoting methylation of various histones which enables transcription of specific gene sequences, including various cell cycle regulators essential for growth control. In parathyroid adenomas, CaSR and VDR mRNA levels are often downregulated, causing an increase in PTH release and proliferative activity. Moreover, MEN1 is recurrently mutated and/or deleted, causing activation of JunD transcriptional programs as well as a reduction in histone methylation. Also, cyclin D1 levels are frequently increased in parathyroid adenoma, leading to the nuclear accumulation of the CDK4-cyclin D1 complex, in turn inhibiting pRb, leading to cell cycle progression
The association between inactivating CDC73 gene mutations and parathyroid carcinoma is best exemplified by the HPT-JT syndrome, in which parathyroid malignant tumors are markedly overrepresented compared to the incidence in the general population [19, 21, 78]. Similarly, between 40 and 80% of sporadic parathyroid carcinomas display inactivating CDC73 gene mutations, often in combination with loss of the remaining allele [21, 22, 79, 81]. Strikingly, these mutations are often found to be present also on the germline level, suggesting a high rate of previously undetected syndromic cases, or representing de novo alterations [21, 22, 83]. The CDC73 mutations are often deleterious, causing disruption of the nuclear localization signals, leading to aborted nuclear translocation [13, 132, 133].
CDC73 encodes parafibromin, a predominantly nuclear protein with multiple tumor suppressive functions. Parafibromin has been established as a member of the human RNA polymerase II-associated factor (hPAF) complex involved in facilitating DNA transcription [134, 135], and has also been shown to regulate the expression of the proto-oncogenes CCND1 (encoding cyclin D1) and c-Myc, as well as interacting with the Wnt pathway effector beta-catenin [136,137,138]. Inactivating CDC73 gene mutations most often lead to the reduction of parafibromin nuclear levels, thus leading to up-regulation of CCND1/cyclin D1 and c-Myc mRNA, leading to cell cycle progression and inhibition of apoptosis (Fig. 20).
Parafibromin functions. Comparison of cellular mechanisms and effects in CDC73/parafibromin (PFIB) wild-type (left) vs. mutated parathyroid tumors (right). In CDC73 wild-type parathyroid tumors, nuclear parafibromin is down-regulating the expression of proto-oncogenes CCND1 (encoding cyclin D1) and c-Myc, while retinoblastoma protein (pRb) levels inhibit cell cycle progression. Moreover, parafibromin may also stimulate apoptosis. In the event of a CDC73 mutation, repression of CCND1/cyclin D1 and c-Myc is lifted, leading to cell cycle progression and reduced/inhibited apoptosis. The bottom panel depicts genomic differences in CDC73 wild-type vs. CDC73 mutated carcinomas. CDC73 gene wild-type cases usually exhibit low tumor mutational burden (TMB) and a stable genome, while CDC73-mutated tumors display increased TMB and copy number alterations. Moreover, the risk of disease recurrence (as exemplified here by a regional lymph node metastasis) is higher in CDC73-mutated/PFIB deficient carcinomas
In addition to CDC73 mutations, somatic mutations in parathyroid carcinoma seem to amass in PI3K- and TP53-related pathways [139]. Moreover, mutations in the other cancer-related gene elements have been reported for small subsets of cases, including the TERT promoter and the DICER1 tumor suppressor gene [139].
Moreover, epigenetic dysregulation is commonly observed in parathyroid carcinomas, with aberrant promoter methylation levels reported for the adenomatous polyposis coli (APC) tumor suppressor gene, the cell cycle regulators cyclin-dependent kinase inhibitor 2A and 2B (CDKN2A and CDKN2B) [140, 141]. On a global level, reduction of 5-hydroxymethylcytosine (5hmC) expression was recently reported, indicative of decreased de-methylation events across the genome [142]. Via methylation array analyses, parathyroid adenoma and carcinoma seem to exhibit distinct epigenetic profiles with 263 genes found significantly different in methylation patterns between these two groups [140]. Interestingly, hypermethylation of the Wnt pathway associated genes SFRP1, SFRP2, and SFRP4 was noted in parathyroid tumors as compared to normal parathyroid tissues, further establishing the role of a dysregulated Wnt pathway in parathyroid tumorigenesis [140].
Molecular data suggest that parathyroid adenoma and carcinoma to a large extent harbor different genetic aberrancies. For example, while parathyroid adenomas recurrently display deleterious and somatic MEN1 gene mutations, this gene is rarely mutated in atypical parathyroid tumors and parathyroid carcinomas. Similarly, while somatic CDC73 gene mutations are found in large proportions of atypical parathyroid tumors and parathyroid carcinomas, these events are very seldomly identified in sporadic adenomas. Indeed, atypical parathyroid tumors in general display a genetic profile that more closely resembles parathyroid carcinoma than adenoma, suggesting a genetic relationship between these entities [143]. However, the exact mechanisms driving the possible transformation into full-blown malignancy are not fully understood.
On the expression level, parathyroid lesions fall into three main clusters, a hyperplasia cluster (mostly hyperplastic parathyroid lesions), a CDC73 driven cluster (including both sporadic and hereditary parathyroid adenoma and carcinoma with CDC73 gene mutations) and a MEN1-related cluster (including mostly adenomas) [144]. This clustering proposes that parathyroid tumors with CDC73 gene mutations follow pathways separate from MEN1-mutated parathyroid tumors, and suggests additional molecular alterations may influence the malignant behavior of parathyroid tumors apart from CDC73, given the similar expressional profiles of CDC73 mutated parathyroid adenoma and carcinoma. Studies have indicated that CDC73-mutated adenomas may harbor a distinct cytogenetic prolife compared to carcinomas with the same mutation, making it likely that additional factors are at play [145].
In terms of molecular work-up in the clinical setting, there are no clear-cut recommendations in the new 2022 WHO classification. However, parafibromin deficient tumors and parathyroid carcinomas are indications for genetic testing. We know that CDC73-mutated parathyroid carcinomas display increased tumor mutational burden, an overall genomic instability and poorer patient outcomes compared to CDC73 wild-type parathyroid carcinomas (Fig. 16) [146]. Although most pathology laboratories do not perform CDC73 gene sequencing on the somatic level as part of their routine diagnostic work-up, parafibromin immunohistochemistry is of value in this context, as a negative stain may identify cases in which an underlying CDC73 gene event is probable. Moreover, parathyroid carcinomas often display mutations in actionable genes suitable for targeted treatment, such as neurofibromatosis type 1 (NF1), phosphatase and tensin homolog (PTEN), and phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA), to name a few [139, 147]. Thus, comprehensive sequencing of selected cases may be of potential clinical value if conventional therapy is deemed unsuccessful. These findings also expand the molecular correlates of CDC73 wild-type disease and may help us better understand the heterogeneous spectrum of sporadic parathyroid carcinomas.
Question 8. What Are Correlates of Genetic Predisposition in Parathyroid Tumors? What Are Morphologic and Immunohistochemical Harbingers of Germline Susceptibility in Parathyroid Tumors?
The distinction of inherited hyperparathyroidism form sporadic manifestations is an evolved clinical responsibility of endocrine pathologists. The recently defined MEN5 syndrome (due to germline pathogenic MAX variants) [8] has expanded the well-established inherited hyperparathyroidism syndromes which include HPT-JT, MEN1, MEN2, MEN4, and familial-isolated hyperparathyroidism syndromes [7]. In addition, there are rare germline pathogenic variants including but not limited to GCM2 that can cause inherited familial hyperparathyroidism.
As a general practice rule, any of the following conditions require exclusion of underlying germline susceptibility: (a) young age (< 45 years old), (b) primary hyperparathyroidism with multiglandular parathyroid disease, (c) family history for primary hyperparathyroidism or components of well-defined inherited hyperparathyroidism syndromes, (d) personal history of tumors that can be a component of inherited hyperparathyroidism syndromes, (e) histological findings suggestive of CDC73-related disease, (f) parafibromin deficiency, (g) global loss of p27, menin, or MAX in the setting of multiple nodular proliferations in a single gland or in the background of multiglandular parathyroid disease, and (h) recurrence of primary hyperparathyroidism due to asynchronous parathyroid involvement.
The ideal approach would be to perform either a whole exome or whole-genome sequencing in any patients with a suspected inherited hyperparathyroidism based on the former criteria. However, problems related to access and cost are major limitations. Therefore, a select panel or targeted gene testing is typically performed in most practices. Pathologists may help multidisciplinary team by performing biomarkers and recognizing characteristic features of a subset of germline manifestations.
Genotype-morphological phenotype correlations have thought us that CDC73-related parathyroid neoplasms are often reflected in sheet like (rather than acinar) growth pattern, nuclear enlargement but with relatively preserved N:C ratios, eosinophilic cytoplasm but with perinuclear cytoplasmic clearing and scattered binuclear or multinucleate cells (Fig. 21). Such manifestations should be further assessed with parafibromin immunohistochemistry. However, it is emphasized that parafibromin may be a difficult stain to perform and interpret and that not all tumors associated with biallelic mutation/inactivation of CDC73 will show loss of immunohistochemical expression of parafibromin [9, 11, 13, 23, 87]. Thus, molecular testing and genetic counseling may still be appropriate in suggestive clinical or morphological expression even if parafibromin demonstrates apparently preserved expression.
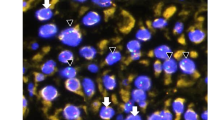
Parafibromin deficient parathyroid tumor in HPT-JT syndrome. A parafibromin deficient parathyroid tumor arising in the setting of HPT-JT syndrome. In this case, there are several morphological clues, including eosinophilic cytoplasm with perinuclear cytoplasmic clearing imparting an almost “koilocytic like” appearance, occasional binucleate cells and a sheet-like growth pattern
MEN1-related manifestations have a distinct multinodular growth reflecting multiple small adenomas arising in the background of multiglandular parathyroid disease (Fig. 22). MEN4 and the recently defined MEN5 syndrome also show MEN1-like findings. Therefore, the demonstration of the global loss of menin, p27, and MAX expression in multinodular proliferations may facilitate the screening for MEN1-, MEN4-, and MEN5-related pathogenesis. While the overall performance of MAX immunohistochemistry has been questioned by some experts, molecular immunohistochemistry findings alone only serve as an ancillary screening tool. Therefore, germline testing is required to distinguish somatic/epigenetic inactivation from an underlying genetic susceptibility.
References
Duan K, Gomez Hernandez K,Mete O (2015) Clinicopathological correlates of hyperparathyroidism. J Clin Pathol 68: 771-787.
Mete O,Asa SL (2013) Precursor lesions of endocrine system neoplasms. Pathology 45: 316-330.
Friedman E, Sakaguchi K, Bale AE, Falchetti A, Streeten E, Zimering MB, Weinstein LS, McBride WO, Nakamura Y, Brandi ML,et al. (1989) Clonality of parathyroid tumors in familial multiple endocrine neoplasia type 1. N Engl J Med 321: 213-218.
Thakker RV (2014) Multiple endocrine neoplasia type 1 (men1) and type 4 (men4). Mol Cell Endocrinol 386: 2-15.
Schernthaner-Reiter MH, Trivellin G,Stratakis CA (2016) Men1, men4, and carney complex: pathology and molecular genetics. Neuroendocrinology 103: 18-31.
Doherty GM, Lairmore TC,DeBenedetti MK (2004) Multiple endocrine neoplasia type 1 parathyroid adenoma development over time. World J Surg 28: 1139-1142.
Duan K, Mete O (2016) Familial hyperparathyroidism syndromes. Diagnostic histopathology 22: 92-100.
Seabrook AJ, Harris JE, Velosa SB, Kim E, McInerney-Leo AM, Dwight T, Hockings JI, Hockings NG, Kirk J, Leo PJ, Love AJ, Luxford C, Marshall M, Mete O, Pennisi DJ, Brown MA, Gill AJ, Hockings GI, Clifton-Bligh RJ,Duncan EL (2021) Multiple endocrine tumors associated with germline max mutations: multiple endocrine neoplasia type 5? J Clin Endocrinol Metab 106: 1163-1182.
Gill AJ, Lim G, Cheung VKY, Andrici J, Perry-Keene JL, Paik J, Sioson L, Clarkson A, Sheen A, Luxford C, Elston MS, Meyer-Rochow GY, Nano MT, Kruijff S, Engelsman AF, Sywak M, Sidhu SB, Delbridge LW, Robinson BG, Marsh DJ, Toon CW, Chou A,Clifton-Bligh RJ (2019) Parafibromin-deficient (hpt-jt type, cdc73 mutated) parathyroid tumors demonstrate distinctive morphologic features. Am J Surg Pathol 43: 35-46.
Erickson LA,Mete O (2018) Immunohistochemistry in diagnostic parathyroid pathology. Endocr Pathol 29: 113-129.
Juhlin CC, Nilsson IL, Lagerstedt-Robinson K, Stenman A, Branstrom R, Tham E,Hoog A (2019) Parafibromin immunostainings of parathyroid tumors in clinical routine: a near-decade experience from a tertiary center. Mod Pathol 32: 1082-1094.
Williams MD, DeLellis RA, Erickson LA, Gupta R, Johnson SJ, Kameyama K, Natu S, Ng T, Perren A, Perrier ND, Seethala RR,Gill AJ (2021) Pathology data set for reporting parathyroid carcinoma and atypical parathyroid neoplasm: recommendations from the international collaboration on cancer reporting. Hum Pathol 110: 73-82.
Gill AJ, Clarkson A, Gimm O, Keil J, Dralle H, Howell VM,Marsh DJ (2006) Loss of nuclear expression of parafibromin distinguishes parathyroid carcinomas and hyperparathyroidism-jaw tumor (hpt-jt) syndrome-related adenomas from sporadic parathyroid adenomas and hyperplasias. Am J Surg Pathol 30: 1140-1149.
Mehta A, Patel D, Rosenberg A, Boufraqech M, Ellis RJ, Nilubol N, Quezado MM, Marx SJ, Simonds WF,Kebebew E (2014) Hyperparathyroidism-jaw tumor syndrome: results of operative management. Surgery 156: 1315–1324; discussion 1324–1315.
Juhlin CC, Nilsson IL, Johansson K, Haglund F, Villablanca A, Hoog A,Larsson C (2010) Parafibromin and apc as screening markers for malignant potential in atypical parathyroid adenomas. Endocr Pathol 21: 166-177.
Kruijff S, Sidhu SB, Sywak MS, Gill AJ,Delbridge LW (2014) Negative parafibromin staining predicts malignant behavior in atypical parathyroid adenomas. Ann Surg Oncol 21: 426-433.
Hosny Mohammed K, Siddiqui MT, Willis BC, Zaharieva Tsvetkova D, Mohamed A, Patel S, Sharma J, Weber C,Cohen C (2017) Parafibromin, apc, and mib-1 are useful markers for distinguishing parathyroid carcinomas from adenomas. Appl Immunohistochem Mol Morphol 25: 731-735.
Juhlin CC,Erickson LA (2021) Genomics and epigenomics in parathyroid neoplasia: from bench to surgical pathology practice. Endocr Pathol 32: 17-34.
Carpten JD, Robbins CM, Villablanca A, Forsberg L, Presciuttini S, Bailey-Wilson J, Simonds WF, Gillanders EM, Kennedy AM, Chen JD, Agarwal SK, Sood R, Jones MP, Moses TY, Haven C, Petillo D, Leotlela PD, Harding B, Cameron D, Pannett AA, Hoog A, Heath H, 3rd, James-Newton LA, Robinson B, Zarbo RJ, Cavaco BM, Wassif W, Perrier ND, Rosen IB, Kristoffersson U, Turnpenny PD, Farnebo LO, Besser GM, Jackson CE, Morreau H, Trent JM, Thakker RV, Marx SJ, Teh BT, Larsson C,Hobbs MR (2002) Hrpt2, encoding parafibromin, is mutated in hyperparathyroidism-jaw tumor syndrome. Nat Genet 32: 676-680.
Bricaire L, Odou MF, Cardot-Bauters C, Delemer B, North MO, Salenave S, Vezzosi D, Kuhn JM, Murat A, Caron P, Sadoul JL, Silve C, Chanson P, Barlier A, Clauser E, Porchet N, Groussin L,Group GTE (2013) Frequent large germline hrpt2 deletions in a french national cohort of patients with primary hyperparathyroidism. J Clin Endocrinol Metab 98: E403-408.
Shattuck TM, Valimaki S, Obara T, Gaz RD, Clark OH, Shoback D, Wierman ME, Tojo K, Robbins CM, Carpten JD, Farnebo LO, Larsson C,Arnold A (2003) Somatic and germ-line mutations of the hrpt2 gene in sporadic parathyroid carcinoma. N Engl J Med 349: 1722-1729.
Cetani F, Pardi E, Borsari S, Viacava P, Dipollina G, Cianferotti L, Ambrogini E, Gazzerro E, Colussi G, Berti P, Miccoli P, Pinchera A,Marcocci C (2004) Genetic analyses of the hrpt2 gene in primary hyperparathyroidism: germline and somatic mutations in familial and sporadic parathyroid tumors. J Clin Endocrinol Metab 89: 5583-5591.
Gill AJ (2014) Understanding the genetic basis of parathyroid carcinoma. Endocr Pathol 25: 30-34.
Bollerslev J, Rejnmark L, Zahn A, Heck A, Appelman-Dijkstra NM, Cardoso L, Hannan FM, Cetani F, Sikjaer T, Formenti AM, Bjornsdottir S, Schalin-Jantti C, Belaya Z, Gibb FW, Lapauw B, Amrein K, Wicke C, Grasemann C, Krebs M, Ryhanen EM, Makay O, Minisola S, Gaujoux S, Bertocchio JP, Hassan-Smith ZK, Linglart A, Winter EM, Kollmann M, Zmierczak HG, Tsourdi E, Pilz S, Siggelkow H, Gittoes NJ, Marcocci C, Kamenicky P (2021) European expert consensus on practical management of specific aspects of parathyroid disorders in adults and in pregnancy: Recommendations of the ese educational program of parathyroid disorders. Eur J Endocrinol
Aojula N, Khan S, Gittoes N,Hassan-Smith Z (2021) Normocalcaemic primary hyperparathyroidism: What is the role of parathyroid surgery? Ther Adv Endocrinol Metab 12: 2042018821995370.
Chow LS, Erickson LA, Abu-Lebdeh HS,Wermers RA (2006) Parathyroid lipoadenomas: a rare cause of primary hyperparathyroidism. Endocr Pract 12: 131-136.
Hyrcza MD, Sargin P,Mete O (2016) Parathyroid lipoadenoma: a clinicopathological diagnosis and possible trap for the unaware pathologist. Endocr Pathol 27: 34-41.
Kong SH, Kim JH, Park MY, Kim SW,Shin CS (2021) Epidemiology and prognosis of parathyroid carcinoma: Real-world data using nationwide cohort. J Cancer Res Clin Oncol 147: 3091-3097.
Wang P, Xue S, Wang S, Lv Z, Meng X, Wang G, Meng W, Liu J,Chen G (2017) Clinical characteristics and treatment outcomes of parathyroid carcinoma: a retrospective review of 234 cases. Oncol Lett 14: 7276-7282.
Ryhanen EM, Leijon H, Metso S, Eloranta E, Korsoff P, Ahtiainen P, Kekalainen P, Tamminen M, Ristamaki R, Knutar O, Loyttyniemi E, Niskanen L, Vaisanen M, Heiskanen I, Valimaki MJ, Laakso M, Haglund C, Arola J,Schalin-Jantti C (2017) A nationwide study on parathyroid carcinoma. Acta Oncol 56: 991-1003.
Brown S, O'Neill C, Suliburk J, Sidhu S, Sywak M, Gill A, Robinson B,Delbridge L (2011) Parathyroid carcinoma: increasing incidence and changing presentation. ANZ J Surg 81: 528-532.
Lee PK, Jarosek SL, Virnig BA, Evasovich M,Tuttle TM (2007) Trends in the incidence and treatment of parathyroid cancer in the united states. Cancer 109: 1736-1741.
Cappellacci F, Medas F, Canu GL, Lai ML, Conzo G, Erdas E,Calo PG (2020) Parathyroid carcinoma in the setting of tertiary hyperparathyroidism: case report and review of the literature. Case Rep Endocrinol 2020: 5710468.
Nasrallah MP, Fraker DL,LiVolsi VA (2014) Parathyroid carcinoma in the setting of tertiaryhyperparathyroidism after renal transplant. Endocr Pathol 25: 433-435.
Duan K,Mete O (2015) Parathyroid carcinoma: diagnosis and clinical implications. Turk Patoloji Derg 31 Suppl 1: 80-97.
Asare EA, Silva-Figueroa A, Hess KR, Busaidy N, Graham PH, Grubbs EG, Lee JE, Williams MD,Perrier ND (2019) Risk of distant metastasis in parathyroid carcinoma and its effect on survival: a retrospective review from a high-volume center. Ann Surg Oncol 26: 3593-3599.
Cavalier E, Betea D, Schleck ML, Gadisseur R, Vroonen L, Delanaye P, Daly AF,Beckers A (2014) The third/second generation pth assay ratio as a marker for parathyroid carcinoma: evaluation using an automated platform. J Clin Endocrinol Metab 99: E453-457.
Erovic BM, Goldstein DP, Kim D, Mete O, Brierley J, Tsang R, Freeman JL, Asa SL, Rotstein L,Irish JC (2013) Parathyroid cancer: outcome analysis of 16 patients treated at the princess margaret hospital. Head Neck 35: 35-39.
Harari A, Waring A, Fernandez-Ranvier G, Hwang J, Suh I, Mitmaker E, Shen W, Gosnell J, Duh QY,Clark O (2011) Parathyroid carcinoma: a 43-year outcome and survival analysis. J Clin Endocrinol Metab 96: 3679-3686.
Schaapveld M, Jorna FH, Aben KK, Haak HR, Plukker JT,Links TP (2011) Incidence and prognosis of parathyroid gland carcinoma: a population-based study in the netherlands estimating the preoperative diagnosis. Am J Surg 202: 590-597.
Cavalier E, Daly AF, Betea D, Pruteanu-Apetrii PN, Delanaye P, Stubbs P, Bradwell AR, Chapelle JP,Beckers A (2010) The ratio of parathyroid hormone as measured by third- and second-generation assays as a marker for parathyroid carcinoma. J Clin Endocrinol Metab 95: 3745-3749.
Caron P, Maiza JC, Renaud C, Cormier C, Barres BH,Souberbielle JC (2009) High third generation/second generation pth ratio in a patient with parathyroid carcinoma: clinical utility of third generation/second generation pth ratio in patients with primary hyperparathyroidism. Clin Endocrinol (Oxf) 70: 533-538.
Busaidy NL, Jimenez C, Habra MA, Schultz PN, El-Naggar AK, Clayman GL, Asper JA, Diaz EM, Jr., Evans DB, Gagel RF, Garden A, Hoff AO, Lee JE, Morrison WH, Rosenthal DI, Sherman SI, Sturgis EM, Waguespack SG, Weber RS, Wirfel K,Vassilopoulou-Sellin R (2004) Parathyroid carcinoma: a 22-year experience. Head Neck 26: 716-726.
Wynne AG, van Heerden J, Carney JA,Fitzpatrick LA (1992) Parathyroid carcinoma: clinical and pathologic features in 43 patients. Medicine (Baltimore) 71: 197-205.
Fraser WD (2009) Hyperparathyroidism. Lancet 374: 145-158.
Lin X, Fan Y, Zhang Z,Yue H (2021) Clinical characteristics of primary hyperparathyroidism: 15-year experience of 457 patients in a single center in China. Front Endocrinol (Lausanne) 12: 602221.
Lundgren E, Hagstrom EG, Lundin J, Winnerback K, Roos J, Ljunghall S,Rastad J (2002) Primary hyperparathyroidism revisited in menopausal women with serum calcium in the upper normal range at population-based screening 8 years ago. World J Surg 26: 931-936.
Dawood NB, Yan KL, Shieh A, Livhits MJ, Yeh MW,Leung AM (2020) Normocalcaemic primary hyperparathyroidism: an update on diagnostic and management challenges. Clin Endocrinol (Oxf) 93: 519-527.
Goasguen N, Chirica M, Roger N, Munoz-Bongrand N, Zohar S, Noullet S, de Roquancourt A, Cattan P,Sarfati E (2010) Primary hyperparathyroidism from parathyroid microadenoma: specific features and implications for a surgical strategy in the era of minimally invasive parathyroidectomy. J Am Coll Surg 210: 456-462.
Sala TD, Muresan S, Roman R, Lazar A, Ion R,Pascanu I (2019) Hypercalcaemic crisis due to primary hyperparathyroidism: report of two cases. J Crit Care Med (Targu Mures) 5: 34-39.
Mantzoros I, Kyriakidou D, Galanos-Demiris K, Chatzakis C, Parpoudi S, Sapidis N, Loutzidou L, Ioannidis O, Angelopoulos S,Tsalis KG (2018) A rare case of primary hyperparathyroidism caused by a giant solitary parathyroid adenoma. Am J Case Rep 19: 1334-1337.
Akerstrom G, Malmaeus J,Bergstrom R (1984) Surgical anatomy of human parathyroid glands. Surgery 95: 14-21.
Howson P, Kruijff S, Aniss A, Pennington T, Gill AJ, Dodds T, Delbridge LW, Sidhu SB,Sywak MS (2015) Oxyphil cell parathyroid adenomas causing primary hyperparathyroidism: a clinico-pathological correlation. Endocr Pathol 26: 250-254.
Erickson LA, Jin L, Papotti M,Lloyd RV (2002) Oxyphil parathyroid carcinomas: a clinicopathologic and immunohistochemical study of 10 cases. Am J Surg Pathol 26: 344-349.
Durmus ET, Atmaca A, Kefeli M, Mete O, Canbaz Tosun F, Baycelebi D, Polat C,Colak R (2021) Clinicopathological variables that correlate with sestamibi positivity in uniglandular parathyroid disease: a retrospective analysis of 378 parathyroid adenomas. Ann Nucl Med
Hu Y, Cui M, Xia Y, Su Z, Zhang X, Liao Q, Jiang Y,Zhao Y (2018) The clinical features of cystic parathyroid adenoma in chinese population: a single-center experience. Int J Endocrinol 2018: 3745239.
El Hussein S,Poppiti R (2017) Water clear cell adenoma of the parathyroid gland: a forgotten cause of primary hyperparathyroidism. Int J Surg Pathol 25: 384-388.
Pirela D, Treitl D, El Hussein S, Poppiti R, Mesko T,Manzano A (2016) Intrathyroidal clear cell tumor of parathyroid origin with review of literature. Case Rep Pathol 2016: 7169564.
Roth SI (1970) The ultrastructure of primary water-clear cell hyperplasia of the parathyroid glands. Am J Pathol 61: 233-248.
Juhlin CC, Nilsson IL, Falhammar H,Zedenius J (2021) Institutional characterisation of water clear cell parathyroid adenoma: a rare entity often unrecognised by tc-99m-sestamibi scintigraphy. Pathology 53: 852-859.
Chandramohan A, Sathyakumar K, John RA, Manipadam MT, Abraham D, Paul TV, Thomas N,Paul MJ (2014) Atypical ultrasound features of parathyroid tumours may bear a relationship to their clinical and biochemical presentation. Insights Imaging 5: 103-111.
Krawitz R, Glover A, Koneru S, Jiang J, Di Marco A, Gill AJ, Aniss A, Sywak M, Delbridge L,Sidhu S (2020) The significance of histologically “large normal” parathyroid glands in primary hyperparathyroidism. World J Surg 44: 1149-1155.
Milas M, Wagner K, Easley KA, Siperstein A,Weber CJ (2003) Double adenomas revisited: nonuniform distribution favors enlarged superior parathyroids (fourth pouch disease). Surgery 134: 995–1003; discussion 1003–1004.
El Lakis M, Nockel P, Gaitanidis A, Guan B, Agarwal S, Welch J, Simonds WF, Weinstein L, Marx S, Nilubol N, Patel D, Merkel R, Tirosh A,Kebebew E (2018) Probability of positive genetic testing results in patients with family history of primary hyperparathyroidism. J Am Coll Surg 226: 933-938.
Juhlin C, Larsson C, Yakoleva T, Leibiger I, Leibiger B, Alimov A, Weber G, Hoog A,Villablanca A (2006) Loss of parafibromin expression in a subset of parathyroid adenomas. Endocr Relat Cancer 13: 509-523.
Erovic BM, Harris L, Jamali M, Goldstein DP, Irish JC, Asa SL,Mete O (2012) Biomarkers of parathyroid carcinoma. Endocr Pathol 23: 221-231.
Hirokawa M, Suzuki A, Higuchi M, Hayashi T, Kuma S, Miya A,Miyauchi A (2021) Histological alterations following fine-needle aspiration for parathyroid adenoma: incidence and diagnostic problems. Pathol Int 71: 400-405.
Schulte JJ, Pease G, Taxy JB, Hall C,Cipriani NA (2021) Distinguishing parathyromatosis, atypical parathyroid adenomas, and parathyroid carcinomas utilizing histologic and clinical features. Head Neck Pathol 15: 727-736.
Kim J, Horowitz G, Hong M, Orsini M, Asa SL,Higgins K (2017) The dangers of parathyroid biopsy. J Otolaryngol Head Neck Surg 46: 4.
Norman J, Politz D,Browarsky I (2007) Diagnostic aspiration of parathyroid adenomas causes severe fibrosis complicating surgery and final histologic diagnosis. Thyroid 17: 1251-1255.
Fernandez-Ranvier GG, Khanafshar E, Jensen K, Zarnegar R, Lee J, Kebebew E, Duh QY,Clark OH (2007) Parathyroid carcinoma, atypical parathyroid adenoma, or parathyromatosis? Cancer 110: 255-264.
Alwaheeb S, Rambaldini G, Boerner S, Coire C, Fiser J,Asa SL (2006) Worrisome histologic alterations following fine-needle aspiration of the parathyroid. J Clin Pathol 59: 1094-1096.
Fraker DL, Travis WD, Merendino JJ, Jr., Zimering MB, Streeten EA, Weinstein LS, Marx SJ, Spiegel AM, Aurbach GD, Doppman JL,et al. (1991) Locally recurrent parathyroid neoplasms as a cause for recurrent and persistent primary hyperparathyroidism. Ann Surg 213: 58-65.
Fitko R, Roth SI, Hines JR, Roxe DM,Cahill E (1990) Parathyromatosis in hyperparathyroidism. Hum Pathol 21: 234-237.
Sarquis MS, Silveira LG, Pimenta FJ, Dias EP, Teh BT, Friedman E, Gomez RS, Tavares GC, Eng C,De Marco L (2008) Familial hyperparathyroidism: surgical outcome after 30 years of follow-up in three families with germline hrpt2 mutations. Surgery 143: 630-640.
Iacobone M, Masi G, Barzon L, Porzionato A, Macchi V, Ciarleglio FA, Palu G, De Caro R, Viel G,Favia G (2009) Hyperparathyroidism-jaw tumor syndrome: a report of three large kindred. Langenbecks Arch Surg 394: 817-825.
Korpi-Hyovalti E, Cranston T, Ryhanen E, Arola J, Aittomaki K, Sane T, Thakker RV,Schalin-Jantti C (2014) Cdc73 intragenic deletion in familial primary hyperparathyroidism associated with parathyroid carcinoma. J Clin Endocrinol Metab 99: 3044-3048.
Simonds WF, Robbins CM, Agarwal SK, Hendy GN, Carpten JD,Marx SJ (2004) Familial isolated hyperparathyroidism is rarely caused by germline mutation in hrpt2, the gene for the hyperparathyroidism-jaw tumor syndrome. J Clin Endocrinol Metab 89: 96-102.
Howell VM, Haven CJ, Kahnoski K, Khoo SK, Petillo D, Chen J, Fleuren GJ, Robinson BG, Delbridge LW, Philips J, Nelson AE, Krause U, Hammje K, Dralle H, Hoang-Vu C, Gimm O, Marsh DJ, Morreau H,Teh BT (2003) Hrpt2 mutations are associated with malignancy in sporadic parathyroid tumours. J Med Genet 40: 657-663.
Haven CJ, van Puijenbroek M, Karperien M, Fleuren GJ,Morreau H (2004) Differential expression of the calcium sensing receptor and combined loss of chromosomes 1q and 11q in parathyroid carcinoma. J Pathol 202: 86-94.
Hunt JL, Carty SE, Yim JH, Murphy J,Barnes L (2005) Allelic loss in parathyroid neoplasia can help characterize malignancy. Am J Surg Pathol 29: 1049-1055.
Cetani F, Ambrogini E, Viacava P, Pardi E, Fanelli G, Naccarato AG, Borsari S, Lemmi M, Berti P, Miccoli P, Pinchera A,Marcocci C (2007) Should parafibromin staining replace hrtp2 gene analysis as an additional tool for histologic diagnosis of parathyroid carcinoma? Eur J Endocrinol 156: 547-554.
Cavaco BM, Santos R, Felix A, Carvalho D, Lopes JM, Domingues R, Sirgado M, Rei N, Fonseca F, Santos JR, Sobrinho L,Leite V (2011) Identification of de novo germline mutations in the hrpt2 gene in two apparently sporadic cases with challenging parathyroid tumor diagnoses. Endocr Pathol 22: 44-52.
Erickson LA, Jin L, Wollan P, Thompson GB, van Heerden JA,Lloyd RV (1999) Parathyroid hyperplasia, adenomas, and carcinomas: differential expression of p27kip1 protein. Am J Surg Pathol 23: 288-295.
Stojadinovic A, Hoos A, Nissan A, Dudas ME, Cordon-Cardo C, Shaha AR, Brennan MF, Singh B,Ghossein RA (2003) Parathyroid neoplasms: clinical, histopathological, and tissue microarray-based molecular analysis. Hum Pathol 34: 54-64.
Bergero N, De Pompa R, Sacerdote C, Gasparri G, Volante M, Bussolati G,Papotti M (2005) Galectin-3 expression in parathyroid carcinoma: immunohistochemical study of 26 cases. Hum Pathol 36: 908-914.
Howell VM, Gill A, Clarkson A, Nelson AE, Dunne R, Delbridge LW, Robinson BG, Teh BT, Gimm O,Marsh DJ (2009) Accuracy of combined protein gene product 9.5 and parafibromin markers for immunohistochemical diagnosis of parathyroid carcinoma. J Clin Endocrinol Metab 94: 434-441.
Osawa N, Onoda N, Kawajiri H, Tezuka K, Takashima T, Ishikawa T, Miyauchi A, Hirokawa M, Wakasa K,Hirakawa K (2009) Diagnosis of parathyroid carcinoma using immunohistochemical staining against htert. Int J Mol Med 24: 733-741.
Truran PP, Johnson SJ, Bliss RD, Lennard TW,Aspinall SR (2014) Parafibromin, galectin-3, pgp9.5, ki67, and cyclin d1: using an immunohistochemical panel to aid in the diagnosis of parathyroid cancer. World J Surg 38: 2845-2854.
Barazeghi E, Gill AJ, Sidhu S, Norlen O, Dina R, Palazzo FF, Hellman P, Stalberg P,Westin G (2017) A role for tet2 in parathyroid carcinoma. Endocr Relat Cancer 24: 329-338.
Akirov A, Asa SL, Larouche V, Mete O, Sawka AM, Jang R,Ezzat S (2019) The clinicopathological spectrum of parathyroid carcinoma. Front Endocrinol (Lausanne) 10: 731.
Davies MP, John Evans TW, Tahir F,Balasubramanian SP (2021) Parathyroid cancer: a systematic review of diagnostic biomarkers. Surgeon 19: e536-e548.
Silva-Figueroa AM, Bassett R, Jr., Christakis I, Moreno P, Clarke CN, Busaidy NL, Grubbs EG, Lee JE, Perrier ND,Williams MD (2019) Using a novel diagnostic nomogram to differentiate malignant from benign parathyroid neoplasms. Endocr Pathol 30: 285-296.
Cetani F, Marcocci C, Torregrossa L,Pardi E (2019) Atypical parathyroid adenomas: challenging lesions in the differential diagnosis of endocrine tumors. Endocr Relat Cancer 26: R441-R464.
Bondeson L, Sandelin K,Grimelius L (1993) Histopathological variables and DNA cytometry in parathyroid carcinoma. Am J Surg Pathol 17: 820-829.
Schneider R, Bartsch-Herzog S, Ramaswamy A, Bartsch DK,Karakas E (2015) Immunohistochemical expression of e-cadherin in atypical parathyroid adenoma. World J Surg 39: 2477-2483.
Fernandez-Ranvier GG, Khanafshar E, Tacha D, Wong M, Kebebew E, Duh QY,Clark OH (2009) Defining a molecular phenotype for benign and malignant parathyroid tumors. Cancer 115: 334-344.
Arribas B, Cristobal E, Alcazar JA, Tardio J, Matinez-Montero JC, Polo JR, Carrion R, Gil L, Azanedo M, Rojas JM,Menarguez J (2000) P53/mdm2 pathway aberrations in parathyroid tumors: P21(waf-1) and mdm2 are frequently overexpressed in parathyroid adenomas. Endocr Pathol 11: 251-257.
Juhlin CC, Zedenius J,Hoog A (2020) Clinical routine application of the second-generation neuroendocrine markers isl1, insm1, and secretagogin in neuroendocrine neoplasia: staining outcomes and potential clues for determining tumor origin. Endocr Pathol 31: 401-410.
Yu Q, Hardin H, Chu YH, Rehrauer W,Lloyd RV (2019) Parathyroid neoplasms: immunohistochemical characterization and long noncoding rna (lncrna) expression. Endocr Pathol 30: 96-105.
O'Connor DT,Deftos LJ (1986) Secretion of chromogranin a by peptide-producing endocrine neoplasms. N Engl J Med 314: 1145-1151.
Altinay S, Erozgur B, Dural AC, Volante M,Papotti MG (2021) Monoclonal/polyclonal pax-8, pth and gata3 immunohistochemistry in parathyroid lesions. J Endocrinol Invest 44: 1997-2008.
Juhlin CC, Haglund F, Villablanca A, Forsberg L, Sandelin K, Branstrom R, Larsson C,Hoog A (2009) Loss of expression for the wnt pathway components adenomatous polyposis coli and glycogen synthase kinase 3-beta in parathyroid carcinomas. Int J Oncol 34: 481-492.
Cryns VL, Rubio MP, Thor AD, Louis DN,Arnold A (1994) P53 abnormalities in human parathyroid carcinoma. J Clin Endocrinol Metab 78: 1320-1324.
Abbona GC, Papotti M, Gasparri G,Bussolati G (1995) Proliferative activity in parathyroid tumors as detected by ki-67 immunostaining. Hum Pathol 26: 135-138.
Lloyd RV, Carney JA, Ferreiro JA, Jin L, Thompson GB, Van Heerden JA, Grant CS,Wollan PC (1995) Immunohistochemical analysis of the cell cycle-associated antigens ki-67 and retinoblastoma protein in parathyroid carcinomas and adenomas. Endocr Pathol 6: 279-287.
Farnebo F, Auer G, Farnebo LO, Teh BT, Twigg S, Aspenblad U, Thompson NW, Grimelius L, Larsson C,Sandelin K (1999) Evaluation of retinoblastoma and ki-67 immunostaining as diagnostic markers of benign and malignant parathyroid disease. World J Surg 23: 68-74.
Vasef MA, Brynes RK, Sturm M, Bromley C,Robinson RA (1999) Expression of cyclin d1 in parathyroid carcinomas, adenomas, and hyperplasias: a paraffin immunohistochemical study. Mod Pathol 12: 412-416.
Hsi ED, Zukerberg LR, Yang WI,Arnold A (1996) Cyclin d1/prad1 expression in parathyroid adenomas: an immunohistochemical study. J Clin Endocrinol Metab 81: 1736-1739.
Cryns VL, Thor A, Xu HJ, Hu SX, Wierman ME, Vickery AL, Jr., Benedict WF,Arnold A (1994) Loss of the retinoblastoma tumor-suppressor gene in parathyroid carcinoma. N Engl J Med 330: 757-761.
Vargas MP, Vargas HI, Kleiner DE,Merino MJ (1997) The role of prognostic markers (mib-1, rb, and bcl-2) in the diagnosis of parathyroid tumors. Mod Pathol 10: 12-17.
Sulaiman L, Juhlin CC, Nilsson IL, Fotouhi O, Larsson C,Hashemi J (2013) Global and gene-specific promoter methylation analysis in primary hyperparathyroidism. Epigenetics 8: 646-655.
Hahn MA, Howell VM, Gill AJ, Clarkson A, Weaire-Buchanan G, Robinson BG, Delbridge L, Gimm O, Schmitt WD, Teh BT,Marsh DJ (2010) Cdc73/hrpt2 cpg island hypermethylation and mutation of 5'-untranslated sequence are uncommon mechanisms of silencing parafibromin in parathyroid tumors. Endocr Relat Cancer 17: 273-282.
Tan MH, Morrison C, Wang P, Yang X, Haven CJ, Zhang C, Zhao P, Tretiakova MS, Korpi-Hyovalti E, Burgess JR, Soo KC, Cheah WK, Cao B, Resau J, Morreau H,Teh BT (2004) Loss of parafibromin immunoreactivity is a distinguishing feature of parathyroid carcinoma. Clin Cancer Res 10: 6629-6637.
Hodgson A, Pakbaz S, Tayyari F, Young JEM,Mete O (2019) Diagnostic pitfall: parathyroid carcinoma expands the spectrum of calcitonin and calcitonin gene-related peptide expressing neuroendocrine neoplasms. Endocr Pathol 30: 168-172.
Juhlin CC, Haglund F, Obara T, Arnold A, Larsson C,Hoog A (2011) Absence of nucleolar parafibromin immunoreactivity in subsets of parathyroid malignant tumours. Virchows Arch 459: 47-53.
Panicker LM, Zhang JH, Dagur PK, Gastinger MJ,Simonds WF (2010) Defective nucleolar localization and dominant interfering properties of a parafibromin l95p missense mutant causing the hyperparathyroidism-jaw tumor syndrome. Endocr Relat Cancer 17: 513-524.
Quinn CE, Healy J, Lebastchi AH, Brown TC, Stein JE, Prasad ML, Callender GG, Carling T,Udelsman R (2015) Modern experience with aggressive parathyroid tumors in a high-volume new england referral center. J Am Coll Surg 220: 1054-1062.
Heppner C, Kester MB, Agarwal SK, Debelenko LV, Emmert-Buck MR, Guru SC, Manickam P, Olufemi SE, Skarulis MC, Doppman JL, Alexander RH, Kim YS, Saggar SK, Lubensky IA, Zhuang Z, Liotta LA, Chandrasekharappa SC, Collins FS, Spiegel AM, Burns AL,Marx SJ (1997) Somatic mutation of the men1 gene in parathyroid tumours. Nat Genet 16: 375-378.
Thakker RV, Bouloux P, Wooding C, Chotai K, Broad PM, Spurr NK, Besser GM,O'Riordan JL (1989) Association of parathyroid tumors in multiple endocrine neoplasia type 1 with loss of alleles on chromosome 11. N Engl J Med 321: 218-224.
Nakamura Y, Larsson C, Julier C, Bystrom C, Skogseid B, Wells S, Oberg K, Carlson M, Taggart T, O'Connell P,et al. (1989) Localization of the genetic defect in multiple endocrine neoplasia type 1 within a small region of chromosome 11. Am J Hum Genet 44: 751-755.
Larsson C, Skogseid B, Oberg K, Nakamura Y,Nordenskjold M (1988) Multiple endocrine neoplasia type 1 gene maps to chromosome 11 and is lost in insulinoma. Nature 332: 85-87.
Agarwal SK, Guru SC, Heppner C, Erdos MR, Collins RM, Park SY, Saggar S, Chandrasekharappa SC, Collins FS, Spiegel AM, Marx SJ,Burns AL (1999) Menin interacts with the ap1 transcription factor jund and represses jund-activated transcription. Cell 96: 143-152.
Hughes CM, Rozenblatt-Rosen O, Milne TA, Copeland TD, Levine SS, Lee JC, Hayes DN, Shanmugam KS, Bhattacharjee A, Biondi CA, Kay GF, Hayward NK, Hess JL,Meyerson M (2004) Menin associates with a trithorax family histone methyltransferase complex and with the hoxc8 locus. Mol Cell 13: 587-597.
Hong YA, Park KC, Kim BK, Lee J, Sun WY, Sul HJ, Hwang KA, Choi WJ, Chang YK, Kim SY, Shin S,Park J (2021) Analyzing genetic differences between sporadic primary and secondary/tertiary hyperparathyroidism by targeted next-generation panel sequencing. Endocr Pathol 32: 501-512.
Cromer MK, Starker LF, Choi M, Udelsman R, Nelson-Williams C, Lifton RP,Carling T (2012) Identification of somatic mutations in parathyroid tumors using whole-exome sequencing. J Clin Endocrinol Metab 97: E1774-1781.
Costa-Guda J, Marinoni I, Molatore S, Pellegata NS,Arnold A (2011) Somatic mutation and germline sequence abnormalities in cdkn1b, encoding p27kip1, in sporadic parathyroid adenomas. J Clin Endocrinol Metab 96: E701-706.
Arnold A, Kim HG, Gaz RD, Eddy RL, Fukushima Y, Byers MG, Shows TB,Kronenberg HM (1989) Molecular cloning and chromosomal mapping of DNA rearranged with the parathyroid hormone gene in a parathyroid adenoma. J Clin Invest 83: 2034-2040.
Arya AK, Bhadada SK, Singh P, Sachdeva N, Saikia UN, Dahiya D, Behera A, Bhansali A,Rao SD (2017) Promoter hypermethylation inactivates cdkn2a, cdkn2b and rassf1a genes in sporadic parathyroid adenomas. Sci Rep 7: 3123.
Kato J, Matsushime H, Hiebert SW, Ewen ME,Sherr CJ (1993) Direct binding of cyclin d to the retinoblastoma gene product (prb) and prb phosphorylation by the cyclin d-dependent kinase cdk4. Genes Dev 7: 331-342.
Brewer K, Costa-Guda J,Arnold A (2019) Molecular genetic insights into sporadic primary hyperparathyroidism. Endocr Relat Cancer 26: R53-R72.
Bradley KJ, Bowl MR, Williams SE, Ahmad BN, Partridge CJ, Patmanidi AL, Kennedy AM, Loh NY,Thakker RV (2007) Parafibromin is a nuclear protein with a functional monopartite nuclear localization signal. Oncogene 26: 1213-1221.
Hahn MA,Marsh DJ (2005) Identification of a functional bipartite nuclear localization signal in the tumor suppressor parafibromin. Oncogene 24: 6241-6248.
Yart A, Gstaiger M, Wirbelauer C, Pecnik M, Anastasiou D, Hess D,Krek W (2005) The hrpt2 tumor suppressor gene product parafibromin associates with human paf1 and rna polymerase ii. Mol Cell Biol 25: 5052-5060.
Rozenblatt-Rosen O, Hughes CM, Nannepaga SJ, Shanmugam KS, Copeland TD, Guszczynski T, Resau JH,Meyerson M (2005) The parafibromin tumor suppressor protein is part of a human paf1 complex. Mol Cell Biol 25: 612-620.
Yang YJ, Han JW, Youn HD,Cho EJ (2010) The tumor suppressor, parafibromin, mediates histone h3 k9 methylation for cyclin d1 repression. Nucleic Acids Res 38: 382-390.
Lin L, Zhang JH, Panicker LM,Simonds WF (2008) The parafibromin tumor suppressor protein inhibits cell proliferation by repression of the c-myc proto-oncogene. Proc Natl Acad Sci U S A 105: 17420-17425.
Mosimann C, Hausmann G,Basler K (2006) Parafibromin/hyrax activates wnt/wg target gene transcription by direct association with beta-catenin/armadillo. Cell 125: 327-341.
Kutahyalioglu M, Nguyen HT, Kwatampora L, Clarke C, Silva A, Ibrahim E, Waguespack SG, Cabanillas ME, Jimenez C, Hu MI, Sherman SI, Kopetz S, Broaddus R, Dadu R, Wanland K, Williams M, Zafereo M, Perrier N,Busaidy NL (2019) Genetic profiling as a clinical tool in advanced parathyroid carcinoma. J Cancer Res Clin Oncol 145: 1977-1986.
Starker LF, Svedlund J, Udelsman R, Dralle H, Akerstrom G, Westin G, Lifton RP, Bjorklund P,Carling T (2011) The DNA methylome of benign and malignant parathyroid tumors. Genes Chromosomes Cancer 50: 735-745.
Svedlund J, Auren M, Sundstrom M, Dralle H, Akerstrom G, Bjorklund P,Westin G (2010) Aberrant wnt/beta-catenin signaling in parathyroid carcinoma. Mol Cancer 9: 294.
Barazeghi E, Gill AJ, Sidhu S, Norlen O, Dina R, Palazzo FF, Hellman P, Stalberg P,Westin G (2016) 5-hydroxymethylcytosine discriminates between parathyroid adenoma and carcinoma. Clin Epigenetics 8: 31.
Mao X, Wu Y, Yu S,Chen J (2021) Genetic alteration profiles and clinicopathological associations in atypical parathyroid adenoma. Int J Genomics 2021: 6666257.
Haven CJ, Howell VM, Eilers PH, Dunne R, Takahashi M, van Puijenbroek M, Furge K, Kievit J, Tan MH, Fleuren GJ, Robinson BG, Delbridge LW, Philips J, Nelson AE, Krause U, Dralle H, Hoang-Vu C, Gimm O, Morreau H, Marsh DJ,Teh BT (2004) Gene expression of parathyroid tumors: Molecular subclassification and identification of the potential malignant phenotype. Cancer Res 64: 7405-7411.
Sulaiman L, Haglund F, Hashemi J, Obara T, Nordenstrom J, Larsson C,Juhlin CC (2012) Genome-wide and locus specific alterations in cdc73/hrpt2-mutated parathyroid tumors. PLoS One 7: e46325.
Hu Y, Zhang X, Wang O, Bi Y, Xing X, Cui M, Wang M, Tao W, Liao Q,Zhao Y (2020) The genomic profile of parathyroid carcinoma based on whole-genome sequencing. Int J Cancer 147: 2446-2457.
Kang H, Pettinga D, Schubert AD, Ladenson PW, Ball DW, Chung JH, Schrock AB, Madison R, Frampton GM, Stephens PJ, Ross JS, Miller VA,Ali SM (2019) Genomic profiling of parathyroid carcinoma reveals genomic alterations suggesting benefit from therapy. Oncologist 24: 791-797.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
This review article was handled by an independent editor and peer-reviewed as per the journal standards.
Ethics Approval
Not applicable.
Consent for Publication
All authors consent to publication.
Competing Interests
Dr. Ozgur Mete is the Editor-in-Chief of Endocrine Pathology. Dr. Lori Erickson is the Senior Associate Editor of Endocrine Pathology. The remaining authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Drs Erickson and Mete are co-first authors in this manuscript.
Rights and permissions
About this article
Cite this article
Erickson, L.A., Mete, O., Juhlin, C.C. et al. Overview of the 2022 WHO Classification of Parathyroid Tumors. Endocr Pathol 33, 64–89 (2022). https://doi.org/10.1007/s12022-022-09709-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12022-022-09709-1