Abstract
Purpose
Anaplastic thyroid carcinoma (ATC) is the most lethal form of thyroid cancer with most patients dying of their disease within a few months. Only a very small percentage of long-term survivors (LTS) are alive for 2 years or longer. In this retrospective case-control study, we provided a comprehensive comparison between 46 ATC LTSs and 75 ATC control patients who suffered disease-specific mortality within 2 years, aiming to identify factors that may be associated with prolonged survival in ATC.
Methods
A comprehensive clinicopathologic and molecular comparison was performed between 46 ATC LTSs and 75 ATC control patients. Peripheral neutrophil count and neutrophil-to-lymphocyte ratio (NLR) were recorded. The composition of the tumor microenvironment was compared using immunohistochemistry.
Results
Compared with ATC control patients, ATC LTSs were characterized by 1) higher frequency of (primary) resection as well as clinicopathologic parameters attributed to resectability; 2) lower rate of concurrent RAS/BRAF and TERT promoter mutations; 3) lower peripheral neutrophil count and NLR; and 4) lower number of tumor-infiltrating neutrophils/myeloid-derived suppressor cells (MDSC). The survival benefits of low peripheral neutrophil counts and low NLR persisted even when controlling for distant metastasis status at presentation.
Conclusions
In addition to traditional beneficial prognostic factors, e.g., surgical resection, factors attributed to resectability, and absence of co-existing RAS/BRAF and TERT promoter mutations, we herein show that tumor-infiltrating and circulating neutrophils/MDSC are adverse prognostic factors in ATC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anaplastic thyroid carcinoma (ATC) is a rare but lethal form of thyroid cancers with a median survival of 3–4 months based on the Surveillance, Epidemiology, and End Results data [1, 2], and 9 months in retrospective studies from large tertiary centers [3,4,5]. Only a very small subset of patients follows a less aggressive clinical course and survives for longer than 2 years after diagnosis. Such patients may be regarded as long-term survivors (LTS) in an otherwise rapidly fatal cancer type.
Distant metastasis is an independent adverse prognostic factor and the primary cause of mortality in ATC [4, 6,7,8]. Emerging evidence suggests that elevated tumor-infiltrating and circulating neutrophils and myeloid-derived suppressor cells (MDSC, a heterogeneous population of immature myeloid cells with an innate immune-suppressive activity) are an essential component of the pre-metastatic niche, a preconditioned microenvironment that receives the cancer cells at distant sites [9,10,11,12,13]. High tumor-associated neutrophils/MDSC, high peripheral neutrophil count, and high neutrophil-to-lymphocyte ratio (NLR) in the peripheral blood have been associated with adverse outcome, in particular increased risk for distant metastasis, in multiple human cancers [9,10,11,12, 14, 15]. Some recent studies have reported that peripheral neutrophilia is a common phenomenon in ATC [16] and a high NLR has been associated with decreased overall survival [17, 18] and progression-free survival [18]. To date, there is no study which has reported the potential prognostic roles of tumor-infiltrating neutrophils/MDSC in ATC.
In this retrospective case control study, we gathered a unique study cohort of 46 ATC LTSs who survived for at least 2 years after the diagnosis of ATC from three tertiary centers. An ATC control group of 75 patients who suffered disease-specific death within 2 years of diagnosis was also included. Their comprehensive clinicopathologic features, molecular alterations, and characteristics of tumor immune microenvironment (in particular peripheral and tumor-infiltrating neutrophils/MDSC) were compared, aiming to identify any factor that may be associated with a more favorable outcome in this deadly disease.
Material and methods
Patient population
The study was approved by the institutional review board of all participating sites. The study group was composed of 46 patients from three tertiary centers (Memorial Sloan Kettering Cancer Center, New York, NY, US n = 43, Mount Sinai Hospital, Toronto, Ontario, Canada: n = 2, Cedar Sinai Medical Center, Los Angeles, CA, US: n = 1) with a diagnosis of ATC who were alive 2 years after the initial ATC diagnosis. Among them, 9 patients were alive 10 years or more after the diagnosis.
The control group was selected from the MSKCC database to include all patients with ATC who suffered disease-specific death within 2 years, and whose tumors underwent next-generation sequencing using MSK-IMPACT platform (n = 75).
Clinicopathologic features
The histology slides and patients’ chart were reviewed by an endocrine pathologist (BX) to gather the following clinicopathologic features: age, sex, type of pathologic specimen collected, presence of different cytologic features of ATC, mitotic index, atypical mitosis, necrosis, neutrophilic inflammatory infiltrate within the tumor, the presence and type of pre-existing/co-existing differentiated thyroid carcinoma, therapy received, and clinical outcomes (including distant metastasis).
A subset of primary thyroid ATC underwent surgical resection, including 37 from the LTS group and 32 from the control group. For these tumors, additional parameters, such as size of primary tumor, size and percentage of ATC within the primary tumor, encapsulation, capsular invasion, vascular invasion, extrathyroidal extension (pathologic or gross), margin status, gross residual disease, and nodal metastasis, were documented.
Complete blood count at the time of ATC diagnosis was reviewed to collect the absolute neutrophil and lymphocyte count. A NLR was calculated for each patient.
Immunohistochemistry for immune microenvironment
Immunohistochemistry was performed in a subset of patients, including 14 ATC LTSs and 12 ATC control patients. The following primary antibodies were used: PD-L1 (clone E1L3N, dilution 1:400, Cell Signaling Technologies, Danvers, MA, USA), PRAME (EPR203301, 1:1000, Abcam, Cambridge, UK), MHC-I (clone A4, ready to use RTU, Ebioscience, Hatfield, UK), PD-1 (clone NAT 105, RTU, Cell Marque, Rocklin, CA, US), CD4 (clone SP35, 1:25, Cell Marque, Rocklin, CA, US), CD8 (clone 4B11, RTU, Leica, Wetzlar, Germany), CD15 (clone MMA, RTU, Ventana), CD68 (clone KP1, RTU, Ventana, Oro Valley, AZ, US), CD163 (clone MRQ26, RTU, Cell Marque, Rocklin, CA, USA), and FOXP3 (clone 236A/E7, 1:500, Abcam, Cambridge, UK).
For PD-L1, a combined positive score (CPS) was calculated as the sum of positive tumor cells and positive immune cells divided by the total tumor cells multiplied by 100. A CPS of ≥1 was considered to be positive for PD-L1. For preferentially expressed antigen in melanoma (PRAME), any nuclear positivity in the tumor cells was interpreted as positive. The percentage of tumor cells showing membranous immunopositivity of MHC-I was recorded and divided into three categories: positive (≥75%), heterogeneous (25–74% of TCs), and negative (<25% of TCs).
Finally, to measure the extent of inflammatory/immune cells, the number of positive cells labeled with CD68, CD163, CD15, CD4, CD8, FOXP3, and PD1 was counted at the hotspot within a high-power field (400X, field diameter: 0.55 mm). The hotspot was defined as the high-power field with the highest number of positive cells within viable ATC. Areas of tumor necrosis and differentiated thyroid carcinoma were excluded from the analysis.
MSK-IMPACT targeted next-generation sequencing
Twenty ATC LTSs with material available and 75 control cases underwent targeted next-generation sequencing using MSK-IMPACT platform. MSK-IMPACT is a Food and Drug Administration-approved deep-coverage targeted next-generation sequencing platform detecting single nucleotide variants (SNVs), small insertions/deletion (indels), copy number variants, and fusion/structural variants in 368 to 468 oncogenes, using custom DNA probes designed for targeted sequencing of all exons and selected introns, including canonical and selected non-canonical transcripts [19].
Statistics
All statistical analyses were performed using the SPSS software 24.0 (IBM Corporation, Armonk, NY, U.S.). Comparisons of clinicopathologic features, immune microenvironment and molecular alterations between ATC LTS and ATC control group were performed using Chi-square test or Fisher’s exact test for categorical variables and two-tailed Student’s t test for continuous variables. Median overall survival and distant metastasis-free survival and their 95% confidence interval (CI) were calculated using log rank test. Correlation between primary tumor size and peripheral neutrophil counts/NLR in the resected thyroid ATC was performed using Pearson correlation test. P values less than 0.05 were considered statistically significant.
Results
Clinicopathologic features
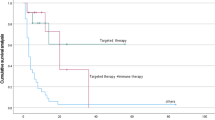
The clinicopathologic characteristics of ATC LTS and ATC control group are summarized in Table 1. The median overall survival (OS) of the ATC LTS was 120 months (95% CI: 86–153 months), and the median OS of ATC control group was 6 months (95% CI: 5–7 months). The median distant metastasis-free survival was 41 months for ATC LTSs (95% CI: 22–59 months) and 1 months for ATC control group (95% CI: 0–2 months).
Compared with ATC control group, ATC LTSs were characterized by significantly higher frequency of resection (89% vs. 55%, p = 0.043), higher rate of resection for primary thyroid ATC (80% vs. 43%, p < 0.001), absence of distant metastasis at presentation (98% vs. 44%, p < 0.001), and lower frequency of tumor necrosis (63% vs. 81%, p = 0.034). Other clinical and pathologic features, including age, sex, cytologic features of ATC, mitotic index, atypical mitosis, presence of neutrophilic infiltrate within the tumor, and pre-existing/co-existing differentiated thyroid carcinoma did not differ between the two groups.
Sixty-nine patients underwent primary resection for thyroid ATC, including 37 (80%) ATC LTSs and 32 (43%) ATC control patients (p < 0.001). Among them, ATC LTS had significant smaller size of primary tumors (median: 4.3 cm vs. 6.0 cm) and ATC component (median 2.2 cm vs. 5.4 cm), lower percentage (median: 60% vs. 100%) of ATC component, as well as lower rate of pathologic evidence of extrathyroidal extension (74% vs. 100%), positive margin (53% vs. 94%), nodal metastasis (31% vs. 63%), gross extrathyroidal extension (13% vs. 52%), and gross residual disease (13% vs. 52%, p < 0.05, Table 1). Eight ATCs were encapsulated, all of which were from the ATC LTS group.
Nine patients were alive 10 years or more after the initial diagnosis of ATC, all of whom underwent resection for primary thyroid ATC (n = 7) or locoregional recurrence (n = 2). None had distant metastasis at presentation. Five (55%) patients developed distant metastases 5 months to 162 months after the initial resection of thyroid ATC. Three patients eventually died of their disease 120 months, 120 months, and 224 months after the initial diagnosis of ATC.
Peripheral neutrophil count and neutrophil-to-lymphocyte ratio
Compared with ATC control patients who often exhibited peripheral neutrophilia with a mean absolute neutrophil count of 8.3 K/mcL and a mean NLR of 6.9, ATC LTS group had significantly lower neutrophil count (mean = 4.2 K/mcL, p < 0.001) and lower NLR ratio (mean = 2.9, p < 0.001, Table 1 and Fig. 1).
ATC long-term survivor is characterized with low CD15-positive tumor-infiltrating myeloid-derived suppressor cells (MDSC)/neutrophils, low peripheral neutrophil count, and low neutrophil-to-lymphocyte ratio (NLR). A The histograms showing the average CD15-MDSC per high power field (HPF), peripheral neutrophil count (K/mcL), and NLR differ significantly between ATC LTS and ATC control patients. Error bars represent standard errors of means. CD15 immunohistochemistry in an ATC LTS (B) and an ATC control patient (C)
In the subgroup of patients without DM at presentation, the peripheral neutrophil count and NLR remained significantly higher in the ATC control group compared with ATC LTS (mean neutrophil count: 4.3 K/mcL in ATC LTS, 8.0 K/mcL in ATC control group, p < 0.001; mean NLR: 2.9 in ATC LTS, 5.5 in ATC control group, p = 0.006).
In patients who underwent primary resection of the thyroid gland for ATC, there was no correlation between primary tumor size and NLR or between primary tumor size and peripheral neutrophil count (Pearson correlation coefficient r ranges from −0.161 to 0.223, p > 0.05, Supplementary Fig. 1).
Among all ATC patients studied, those with distant metastasis at presentation were associated with significantly higher neutrophil count (mean ± standard error of mean SEM: ATC without DM at presentation 6.0 ± 0.5; ATC with DM at presentation 8.5 ± 1.3, p = 0.027) and higher NLR (mean ± SEM: ATC without DM at presentation 4.1 ± 0.5; ATC with DM at presentation 7.8 ± 1.2, p < 0.001).
Tumor microenvironment
Measurements of the immune microenvironment of ATC LTSs and ATC control group are shown in Table 1. Compared with the ATC control group, ATC LTSs were characterized by significantly lower number of CD15-positive tumor infiltrating-MDSC/neutrophils (mean ± SEM: ATC LTS 55 ± 15 per high power field; ATC control group 155 ± 34 per high power field; p = 0.012, Table 1 and Fig. 1). In patients without distant metastases at presentation, there was a nonsignificant trend toward a lower number of CD15-positive tumor infiltrating-MDSC/neutrophils in the ATC LTS group compared to the ATC controls (mean ± SEM: ATC LTS 57 ± 16 per high power field; ATC control group 150 ± 34 per high power field; p = 0.056).
All other measurements, including the rate of PD-L1 positivity, PD-L1 CPS score, rate of PRAME positivity, MHC-1 expression in tumor cells, number of macrophages (CD68-positive or CD163-positive), PD-1-positive immune cells, CD8-positive cytotoxic T cells, CD4-positive helper T cells, and FOXP3-positive regulatory T cells did not differ between the two groups (p > 0.05).
Molecular profile
The molecular profile of the two groups (ATC LTS: n = 20; ATC control group: N = 75) is shown in Fig. 2.
Molecular signature of anaplastic thyroid carcinoma (ATC) according to survival time. ATC long term survivors (ATC LTS) have significantly higher frequency of RB1, KMT2C, BCOR, and RMB10 alterations compared with ATC control group (*p < 0.05). Other molecular alterations do not differ according to survival time. # indicates two patients who survived for at least 10 years
Compared with ATC control group, there was a non-significant trend for ATC LTS to have fewer TERT promoter mutations (ATC LTS: 12/20, 60%; ATC control group: 60/75, 80%, p = 0.080). Co-existence of a BRAF or RAS mutation with a TERT promoter mutation was seen in a significantly higher percentage in the ATC control group (50/75, 67%) compared with ATC LTS (7/20, 35%, p = 0.019). Additionally, ATC LTS group was associated with a significantly higher frequency of RB1, KMT2C, BCOR, and RBM10 alterations (p = 0.032, 0.017, 0.017, and 0.028 respectively).
Other molecular alterations, including those affecting BRAF, RAS, and TP53 did not differ between the two groups. The median mutation count was 6 for ATC LTSs (range 2–21) and 5 for ATC control group (range: 0–30, p = 0.487).
Fusion events observed in the ATC LTS included KMT2C-HILPDA fusion, TP53 intragenic deletion, and NEGR1 intragenic deletion (one case each). CCDC6-RET, EZH2-CUL1, and NOTCH1-NALT1 fusions were detected in the ATC control groups (one case each).
Among the 20 ATC LTSs who were subjected to MSK-IMPACT, two patients had survived for at least 10 years. One tumor harbored BRAF V600E, FAT Q3902*, and TP53 R175H mutations. The other had mutations of TP53, NF1, NF2, RB1, FLCN, EP300, MED12, TEK, and PIK3CD mutations.
Discussion
The key findings of the current study are that ATC LTS is associated with clinicopathologic parameters related to resectability, low frequency of concurrent RAS/BRAF mutations and TERT promoter mutation, a tumor microenvironment characterized by low tumor-infiltrating MDSC/neutrophils, and absence of peripheral neutrophilia characterized by a low peripheral neutrophil count and a low NLR.
Recently, MDSCs/neutrophils have been identified as a major contributor for cancer progression and metastatic spread [9,10,11,12,13]. The bone marrow-derived MDSC/neutrophil is generated and mobilized through multiple tumor-secreting factors, including vascular endothelial growth factor, granulocyte-macrophage colony-stimulating factor, interleukin (IL)-6, IL-10, and transforming growth factor-beta, resulting in peripheral neutrophilia [9,10,11,12,13]. Indeed, high peripheral neutrophil counts and NLR have been reported in multiple cancers to be associated with poorer overall survival and progression-free survival [15]. Several previous studies have also shown that peripheral neutrophilia is a common phenomenon in ATC and a high NLR is associated with decreased survival in ATC [16,17,18]. The current study provides further confirmatory evidence between peripheral neutrophilia and prognosis of ATC, in which a prolonged survival in ATC patients is associated with low peripheral neutrophil count and low NLR. In our study, we have been able to show that this survival difference persists after controlling for stage parameters, such as distant metastasis at presentation.
The mechanisms by which neutrophils/MDSC promote distant metastasis are complex and involve preparation of the pre-metastatic niche, promoting survival of tumor cells, and suppression of T cell functions [9,10,11,12,13]. The pre-metastatic niche is a permissive microenvironment consisting of bone marrow-derived cells (including MDSC/neutrophils), soluble factors, and extracellular matrix, which provide congenial “soil” for disseminated tumor cells to arrest, survive, and colonize [9,10,11,12,13]. In this study, we have shown that higher circulating neutrophils/MDSC measured using peripheral neutrophil count and peripheral NLR is common in ATC with distant metastasis at presentation, providing supportive data of an association between neutrophils/MDSC and metastatic spread.
Tumor-infiltrating neutrophils have also been reported to be an adverse prognostic factor for various types of solid tumors [14, 20]. However, the prognostic role of tumor-infiltrating MDSC/neutrophil in ATC has yet to be determined. ATC is known to be heavily infiltrated by myeloid cells, in particular M2 macrophages and neutrophils [4, 21, 22]. Indeed, we have demonstrated using immunohistochemistry studies that ATC as a whole shows an immune/inflammatory-hot phenotype with abundant macrophages, neutrophils/MDSC, and multiple subsets of T lymphocytes. Additionally, our study provides the first evidence that tumor-infiltrating CD15-positive MDSC/neutrophils identified by immunohistochemistry within the ATC are prognostically relevant for ATC patients and that ATC LTS is associated with a significantly lower number of tumor-infiltrating MDSC/neutrophils. In patients without distant metastasis at presentation, there was a trend toward higher tumor-infiltrating CD15-positive MDSC/neutrophils in short-term survival ATC compared to ATC LTS. This finding together with a significantly higher neutrophilic blood count in short-term ATC survivors who are M0 suggest a role for MDSC/neutrophils in preparing the pre-metastatic niche before the distant disease becomes clinically manifest.
PD-L1 immunopositivity has been reported in a large proportion of ATC. The frequency of PD-L1 positivity ranges from 22% to 94% depending on the detection methods and the cutoff values used [23,24,25,26]. Similarly, the PD-L1 immunopositivity in this study is 76% using a cutoff of CPS ≥ 1. It remains controversial whether PD-L1 immunopositivity is prognostically relevant. A recent meta-analysis failed to demonstrate a significant association between PD-L1 immunoexpression and survival in ATC [25]. In the present study, no significant difference of PD-L1 has been detected between ATC LTS and ATC control patients, indicating that PD-L1 does not impact outcome in ATC.
PRAME is a cancer neoantigen that may serve as a target for cancer vaccination and adoptive T cell therapies [27]. PRAME expression has been detected in various human cancers and is shown to be a prognostic biomarker associated with higher tumor stage, nodal metastasis, and poor disease-free survival in a recent meta-analysis [28]. MHC-I transports and displays cancer neoantigen to the surface of tumor cells, allowing CD8-positive T cells to recognize, bind, and eliminate tumor cells [29]. Down-regulation of MHC-I is a common strategy of immune evasion of many cancers, impairing natural immune response and host response to cancer vaccination [29]. In this study, we have shown that PRAME immunopositivity and MHC-I down-regulation are present in 20% and 36% of ATC, respectively. However, there is no significant difference between ATC LTS and ATC control cases.
The lack of significant prognostic difference of tumor microenvironment, PD-L1, PRAME, and MHCI should be interpreted with caution given the small number of cases tested in each group. Future large-scale studies on tumor microenvironment in ATC are needed.
Previous studies have shown that surgical resectability, negative margin, smaller tumor size, and lack of regional and distant metastasis are independent prognostics factor associated with improved survival in ATC [1, 2, 4, 6, 8, 30]. Not surprisingly, the ATC LTS group in our study was enriched with ATC which was surgically resectable. These primary thyroid ATCs had smaller overall size of primary tumor, smaller size of ATC, lower percentage of ATC within tumors that also harbored a differentiated thyroid carcinoma component, negative margin, as well as absence of gross extrathyroidal extension, gross residual disease, nodal and distant metastasis. Our data provide further evidence that surgical resections and pathologic factors pertinent to resectability are prognostically relevant in ATC.
Several previous studies have identified potential adverse prognostic molecular factors in ATC, including TERT promoter mutation, particularly when it co-exists with BRAF/RAS mutation [4, 22]. In our study, we also reported that the ATC LTS cohort had a significantly lower percentage of cases with both TERT promoter mutations and BRAF/RAS mutation. The frequency of key oncogenic driver events (e.g., BRAF V600E and RAS mutations) and TP53 mutation does not differ between the two groups.
In conclusion, in this comprehensive comparison between ATC long term survivors and ATC control patients, we have identified multiple factors that are associated with prolonged survival including (1) a neutrophil-poor homeostasis and tumor microenvironment characterized by low peripheral blood neutrophil counts, low peripheral blood neutrophil-to-lymphocyte ratios, and low tumor-infiltrating myeloid-derived suppressor cells/neutrophils within the tumor, (2) surgical resection and multiple clinicopathological factors associated with resectability, and (3) a low frequency of concurrent RAS/BRAF mutations with TERT promoter mutation.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
B. Lin, H. Ma, M. Ma, Z. Zhang, Z. Sun et al. The incidence and survival analysis for anaplastic thyroid cancer: a SEER database analysis. Am J. Transl. Res. 11, 5888–5896 (2019)
T.A. Janz, D.M. Neskey, S.A. Nguyen, E.J. Lentsch, Is the incidence of anaplastic thyroid cancer increasing: a population based epidemiology study. World J. Otorhinolaryngol. Head. Neck Surg. 5, 34–40 (2019)
N. Prasongsook, A. Kumar, A.V. Chintakuntlawar, R.L. Foote, J. Kasperbauer et al. Survival in response to multimodal therapy in anaplastic thyroid cancer. J. Clin. Endocrinol. Metab. 102, 4506–4514 (2017)
B. Xu, T. Fuchs, S. Dogan, I. Landa, N. Katabi et al. Dissecting anaplastic thyroid carcinoma: a comprehensive clinical, histologic, immunophenotypic, and molecular study of 360 cases. Thyroid 30, 1505–1517 (2020)
A. Mohebati, M. Dilorenzo, F. Palmer, S.G. Patel, D. Pfister et al. Anaplastic thyroid carcinoma: a 25-year single-institution experience. Ann. Surg. Oncol. 21, 1665–1670 (2014)
G.B. Hvilsom, S.C. Londero, C.H. Hahn, S. Schytte, H.B. Pedersen et al. Anaplastic thyroid carcinoma in Denmark 1996-2012: a national prospective study of 219 patients. Cancer Epidemiol. 53, 65–71 (2018)
J. Wendler, M. Kroiss, K. Gast, M.C. Kreissl, S. Allelein et al. Clinical presentation, treatment and outcome of anaplastic thyroid carcinoma: results of a multicenter study in Germany. Eur. J. Endocrinol./Eur. Federation Endocr. Soc. 175, 521–529 (2016)
I. Sugitani, A. Miyauchi, K. Sugino, T. Okamoto, A. Yoshida et al. Prognostic factors and treatment outcomes for anaplastic thyroid carcinoma: ATC Research Consortium of Japan cohort study of 677 patients. World J. Surg. 36, 1247–1254 (2012)
K. Kos, K.E. de Visser, Neutrophils create a fertile soil for metastasis. Cancer Cell 39, 301–303 (2021)
K. Cole, K. Pravoverov, J.E. Talmadge, Role of myeloid-derived suppressor cells in metastasis. Cancer Metastasis Rev. 40, 391–411 (2021)
M. Wu, M. Ma, Z. Tan, H. Zheng, X. Liu, Neutrophil: a new player in metastatic cancers. Front. Immunol. 11, 565165 (2020)
R. Trovato, S. Cane, V. Petrova, S. Sartoris, S. Ugel et al. The engagement between MDSCs and metastases: partners in crime. Front. Oncol. 10, 165 (2020)
A.M.K. Law, F. Valdes-Mora, D. Gallego-Ortega, Myeloid-derived suppressor cells as a therapeutic target for cancer. Cells 9, 561 (2020).
M. Shen, P. Hu, F. Donskov, G. Wang, Q. Liu et al. Tumor-associated neutrophils as a new prognostic factor in cancer: a systematic review and meta-analysis. PloS One 9, e98259 (2014)
C. Valero, M. Lee, D. Hoen, K. Weiss, D.W. Kelly et al. Pretreatment neutrophil-to-lymphocyte ratio and mutational burden as biomarkers of tumor response to immune checkpoint inhibitors. Nat. Commun. 12, 729 (2021)
T. Sato, M. Omura, J. Saito, A. Hirasawa, Y. Kakuta et al. Neutrophilia associated with anaplastic carcinoma of the thyroid: production of macrophage colony-stimulating factor (M-CSF) and interleukin-6. Thyroid 10, 1113–1118 (2000)
J. Park, J. Park, J.H. Shin, Y.L. Oh, H.A. Jung, et al. Prognostic value of the neutrophil-to-lymphocyte ratio before and after radiotherapy for anaplastic thyroid carcinoma. Cancers 13 13, 1913 (2021).
N. Fukuda, K. Toda, Y.U. Fujiwara, X. Wang, A. Ohmoto et al. Neutrophil-to-lymphocyte ratio as a prognostic marker for anaplastic thyroid cancer treated with lenvatinib. In vivo 34, 2859–2864 (2020)
D.T. Cheng, T.N. Mitchell, A. Zehir, R.H. Shah, R. Benayed et al. Memorial Sloan Kettering-Integrated Mutation Profiling of Actionable Cancer Targets (MSK-IMPACT): a hybridization capture-based next-generation sequencing clinical assay for solid tumor molecular oncology. J. Mol. Diagn. 17, 251–264 (2015)
A.J. Gentles, A.M. Newman, C.L. Liu, S.V. Bratman, W. Feng et al. The prognostic landscape of genes and infiltrating immune cells across human cancers. Nat. Med. 21, 938–945 (2015)
M. Ryder, R.A. Ghossein, J.C. Ricarte-Filho, J.A. Knauf, J.A. Fagin, Increased density of tumor-associated macrophages is associated with decreased survival in advanced thyroid cancer. Endocr.-Relat. Cancer 15, 1069–1074 (2008)
I. Landa, T. Ibrahimpasic, L. Boucai, R. Sinha, J.A. Knauf et al. Genomic and transcriptomic hallmarks of poorly differentiated and anaplastic thyroid cancers. J. Clin. Investig. 126, 1052–1066 (2016)
G.Q. Zhang, W.J. Wei, H.J. Song, Z.K. Sun, C.T. Shen et al. Programmed cell death-ligand 1 overexpression in thyroid cancer. Endocr. Pract. 25, 279–286 (2019)
S. Cameselle-Garcia, S. Abdulkader-Sande, M. Sanchez-Ares, G. Rodriguez-Carnero, J. Garcia-Gomez et al. PD-L1 expression and immune cells in anaplastic carcinoma and poorly differentiated carcinoma of the human thyroid gland: a retrospective study. Oncol. Lett. 22, 553 (2021)
I. Girolami, L. Pantanowitz, O. Mete, M. Brunelli, S. Marletta et al. Programmed death-ligand 1 (PD-L1) is a potential biomarker of disease-free survival in papillary thyroid carcinoma: a systematic review and meta-analysis of PD-L1 immunoexpression in follicular epithelial derived thyroid carcinoma. Endocr. Pathol. 31, 291–300 (2020)
J. Capdevila, L.J. Wirth, T. Ernst, S. Ponce Aix, C.C. Lin et al. PD-1 blockade in anaplastic thyroid carcinoma. J. Clin. Oncol. 38, 2620–2627 (2020)
G. Al-Khadairi, J. Decock, Cancer testis antigens and immunotherapy: where do we stand in the targeting of PRAME? Cancers 11, 984 (2019).
J. Li, J. Yin, J. Zhong, Z. Yang, A. Tang et al. Clinicopathological and prognostic significance of PRAME overexpression in human cancer: a meta-analysis. BioMed. Res. Int. 2020, 8828579 (2020)
K. Dhatchinamoorthy, J.D. Colbert, K.L. Rock, Cancer immune evasion through loss of MHC class I antigen presentation. Front. Immunol. 12, 636568 (2021)
S.M. Glaser, S.F. Mandish, B.S. Gill, G.K. Balasubramani, D.A. Clump et al. Anaplastic thyroid cancer: prognostic factors, patterns of care, and overall survival. Head Neck 38(Suppl 1), E2083–E2090 (2016)
Funding
Research reported in this publication was supported in part by the Cancer Center Support Grant of the National Institutes of Health/National Cancer Institute under award number P30CA008748 and a departmental RFA funded by PaigeAI (SK202-1328).
Author information
Authors and Affiliations
Contributions
Study design: B.X., R.G. Pathology and clinical reviews: B.X., L.X., R.S., I.G., B.B. Molecular analysis: B.X., A.M., I.L., J.A.F. Immunohistochemistry: B.X., V.T. Manuscript drafting: B.X., R.G. Manuscript editing: All authors.
Corresponding author
Ethics declarations
Conflict of interest
No competing financial interests exist for all contributory authors. All of the research meets the ethics guidelines, including adherence to the legal requirements of the country where the study was performed.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Xu, B., Zhang, L., Setoodeh, R. et al. Prolonged survival of anaplastic thyroid carcinoma is associated with resectability, low tumor-infiltrating neutrophils/myeloid-derived suppressor cells, and low peripheral neutrophil-to-lymphocyte ratio. Endocrine 76, 612–619 (2022). https://doi.org/10.1007/s12020-022-03008-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-022-03008-9