Abstract
Background
Anaplastic thyroid carcinoma (ATC) accounts for only 1 to 2% of all thyroid carcinomas, but it is one of the most lethal neoplasms in humans. To date, most findings about ATC have been derived from single-institution studies with limited numbers of cohorts. To obtain further insights into this “orphan disease,” we have established a multicenter registry, the ATC Research Consortium of Japan (ATCCJ). We analyzed prognostic factors and treatment outcomes using the large cohort database of the ATCCJ.
Methods
Most of the Japanese centers involved in the treatment of thyroid cancer were invited to join the ATCCJ and have provided information on ATC patients treated between 1995 and 2008. The database includes 677 cases from 38 registered institutions. Survival curves were determined using Kaplan-Meier methods and were compared using the log-rank test. Cox’s proportional hazards model was used for multivariate analysis.
Results
Clinical varieties of ATC were classified into four types: common type (n = 547); incidental type (n = 29); anaplastic transformation at the neck (n = 95); anaplastic transformation at a distant site (n = 6). The incidental type followed by anaplastic transformation at the neck showed better outcomes than the other types. Anaplastic transformation at a distant site showed the worst outcomes. The 6-month and 1-year cause-specific survival (CSS) rates for common-type ATC were 36 and 18%, respectively. In all, 84 (15%) achieved long-term (>1 year) survival. Multivariate analysis identified age ≥70 years, presence of acute symptoms, leukocytosis (white blood cell count ≥10,000/mm3), large tumor >5 cm, T4b tumor, and distant metastasis as significant risk factors for lower survival. CSS rates also differed significantly depending on UICC stages, with 6-month CSSs of 60% for stage IVA, 45% for IVB, and 19% for IVC. For 36 of 69 (52%) stage IVA patients who underwent radical surgery, adjuvant therapies, including radiation therapy (RTX) and chemotherapy (CTX) did not show additional benefit statistically. Conversely, among 242 stage IVB patients, 80 (33%) underwent radical surgery. For those patients, therapies combining RTX with CTX significantly improved CSS.
Conclusions
Long-term survival is possible for selected patients with ATC. To determine the treatment strategy, UICC stage (disease extent) and other prognostic factors (e.g., biologic malignancy grade) should be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anaplastic thyroid carcinoma (ATC) is one of the most lethal neoplasms in humans, with a disease-specific mortality approaching 100% [1]. Although some patients survive for a fairly long time after aggressive multimodal treatment combined with radical surgical resection, sufficient doses of external-beam radiation therapy (RTX), and chemotherapy (CTX), no definitely effective therapy exists for ATC. Given the poor outcomes with current standard therapy, several clinical trials have been introduced [2]. However, clear evidence of efficacy for any particular regimen is still lacking.
Anaplastic thyroid carcinoma is uncommon, representing only 1 to 2% of all thyroid carcinomas. It accounts, however, for 14 to 39% of thyroid cancer deaths [3, 4]. Because of the aggressive nature and rarity of this disease, it is difficult to improve the quality of evidence with regard to ATC. To date, most existing knowledge about ATC is derived from single-institution studies with limited numbers of cohorts and short-term follow-up. To obtain further insights into this “orphan disease,” we established the ATC Research Consortium of Japan (ATCCJ) in January 2009 as a multicenter registry that accumulates, analyzes, and reviews all the information for ATC that available in Japan. This represents the first report using the ATCCJ database. We analyzed data from a large cohort of 677 ATC patients to determine prognostic factors and treatment outcomes for ATC.
Materials and methods
Most of the Japanese centers involved in the treatment of thyroid carcinoma were invited to complete a form containing the following information for any patient with ATC treated during the 14-year period between 1995 and 2008: It was made anonymous by labeling each case with a connectable identification number; age and sex of the patient; dates of diagnosis, start of treatment, and last follow-up; methods of ATC diagnosis; acute symptoms (duration of severe complaints such as dysphonia, dysphagia, dyspnea, and rapid growth of the tumor <1 month); leukocytosis [white blood cell (WBC) count ≥ 10,000/mm3]; hypercalcemia; tumor size; distant metastasis; T status (T4a: tumor limited to the thyroid, T4b: tumor extends beyond the thyroid capsule) and stage (IVA: T4a anyN M0; IVB: T4b anyN M0; IVC: anyT anyN M1) according to the 7th edition of the Union for International Cancer Control (UICC) classification; previous or concomitant differentiated thyroid carcinoma (DTC); methods of treatment; outcome and cause of death. When data were considered imprecise, an additional query was sent to the physician in charge of the patient. A database recording the collected information was organized at the Cancer Institute Hospital. The institutional review board of the Cancer Institute Hospital approved all study protocols.
As of July 28, 2011, the ATCCJ database included 721 patients with ATC from 38 institutions. One patient treated in 1978 was excluded. Ten data entries, considered to represent multiple inclusions of the same patient treated at multiple institutions, were unified. Another 33 patients for whom diagnosis was not achieved by pathology or cytology examination (i.e., only by clinical presentation) were excluded from the study. Eventually, the study population comprised 677 patients with ATC.
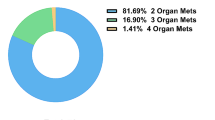
Clinical varieties of ATC were classified into four types: common type (n = 547); incidental type (n = 29); anaplastic transformation at the neck lymph node(s) (n = 95); anaplastic transformation at a distant site (n = 6). Incidental ATC was largely DTC accompanied by a minute (1–2 cm) region of ATC. Anaplastic transformation type was ATC at a site other than the thyroid gland, which was associated with previous or concomitant DTC at the thyroid. Duration of survival was calculated from whichever occurred earlier—date of diagnosis or start of treatment for ATC—until the date of death or last follow-up.
Data analysis was performed using Statistical Analysis System software (SAS Institute, Cary, NC, USA). Survival curves were determined using the Kaplan-Meier method, and the statistical significance of differences was evaluated using the log-rank test. For multivariate survival analysis, the Cox proportional hazards model was used. Values of p < 0.05 were considered statistically significant.
Results
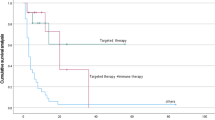
Survival curves for each clinical variety of ATC are shown in Fig. 1. For the incidental type, the median survival time (MST) was 395 days, and the 1-year cause-specific survival (CSS) rate was 57%. These values were significantly better than those for the other ATC types (p < 0.0001). Survival for anaplastic transformation at the neck lymph node(s) (MST 175 days; 1-year CSS 30%) was also better than that for the common type (p = 0.0082). Anaplastic change at a distant site had the worst prognosis (MST 48 days; 1-year CSS 0%; p < 0.0001, compared to the common type). Subsequent analysis focused on the 547 patients with common-type ATC.
Clinical characteristics for common-type ATC are shown in Table 1. Age at diagnosis ranged from 28 to 100 years (mean 68.7 ± 11.0 years). MST was 113 days. The 6-month, 1-year, 3-year, and 5-year CSS rates were 36, 18, 7, and 6%, respectively. Among the 463 patients who died of the disease, causes of death were attributable to local disease including upper airway obstruction (suffocation) and bleeding in 113 patients (24%), distant metastasis or general debility (cachexia) in 293 patients (63%), problems related to treatment in 9 patients (2%), other reasons or unknown in 48 patients.
A total of 84 patients (15%) achieved long-term survival exceeding 1 year after diagnosis of or start of treatment for ATC. Those patients comprised 31 men and 53 women. Mean age was 66.4 ± 10.4 years (range 40–87 years). Among them, 52 (62%) underwent radical surgery, 64 (76%) had ≥40 Gy RTX, and 58 (69%) received some kind of CTX. In all, 29 (35%) patients underwent all three procedures.
Univariate and multivariate analyses of clinical risk factors for survival in the 547 patients with common-type ATC are shown in Table 2. Age ≥70 years, presence of acute symptoms, leukocytosis, large tumor (>5 cm), T4b tumor, and distant metastasis were significant risk factors in both univariate and multivariate analyses. Presence of lymph node metastasis was significant in the univariate analysis but not in the multivariate analysis.
The CSS curves for each UICC stage are shown in Figure 2. The MST and 6-month CSS rate were 236 days and 60%, respectively, for stage IVA; 147 days and 45% for stage IVB; and 81 days and 19% for stage IVC (p < 0.0001).
We also looked at the relations between treatment methods and outcomes in patients with common-type ATC. We found that radical surgery compared to no or palliative surgery, ≥40 Gy of RTX compared to no or <40 Gy RTX, and any CTX compared with no CTX were associated with significantly better outcomes (Table 2).
To investigate the effects of each treatment on individual patients, the relations between treatment methods and outcomes were evaluated separately for each stage of common-type ATC (Table 3). For stage IVA patients, radical surgery and ≥40 Gy of RTX showed a significant association with better outcomes. In contrast, among patients with stage IVA common-type ATC who underwent radical surgery, there was no significant benefit from adjuvant therapies including RTX and CTX according to the Cox proportional hazards model.
As for stage IVB patients, all three treatments (radical surgery, ≥40 Gy RTX, CTX) were significantly associated with favorable outcomes. In stage IVB patients who underwent radical surgery, adjuvant multimodal therapy with both RTX and CTX significantly improved the CSS compared to radical surgery only or surgery with RTX. Altogether, 80 of the 242 patients (33%) with stage IVB disease underwent radical surgery (i.e., macroscopically complete resection). Among these patients, 20 also were subjected to extended resection of the surrounding major organs including the trachea, larynx, and/or esophagus. Survival rates for these patients (MST 131 days; 6-month CSS 37%) were no better than for those who underwent gross curative surgery by resection only of the strap muscles, recurrent laryngeal nerve, or internal jugular vein in addition to the thyroid gland and neck lymph nodes (MST 318 days, 6-month CSS 70%; p = 0.67). In all, 14 of 20 (70%) patients who underwent extended radical resection required a permanent tracheostomy, whereas 59 (27%) of the other patients underwent the procedure (p = 0.00015). The frequency of death due to local disease (suffocation or bleeding) was not different between patients who underwent extended surgery and the others (20 vs. 23%, p = 0.98).
The three treatment methods were also associated with significant effects even in patients with stage IVC disease. However, only 27 patients (12%) could undergo radical surgery. All differences in MST between the presence and absence of treatment were within only 2 months.
Discussion
Several prognostic factors have been reported for patients with ATC [5]. In 2005, Kebebew et al. conducted a study using the U.S. National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) database [6]. The cohort consisted of 516 patients with ATC reported to 12 population-based cancer registries between 1973 and 2000. They analyzed prognostic factors in the greatest number of patients ever reported and concluded that age <60 years, intrathyroidal tumor, and combined use of surgery and RTX were independent predictors of lower cause-specific mortality. Kim et al. also retrospectively reviewed the medical records of 121 patients with ATC from 1995 to 2004 at five major referral centers in Korea [7]. Their multivariate analysis showed that age <60 years, tumor size <7 cm, and lesser extent of disease were independent predictors of lower disease-specific mortality. Besic et al. conducted a multivariate survival analysis of 188 patients with ATC in Slovenia, an iodine-deficient region [8]. They demonstrated that the survival time of patients with ATC was influenced by factors related to the patient (performance status and age), the tumor (rapidity of tumor growth), and the extent of disease (local tumor extension and distant metastasis).
The present study used the ATCCJ database, which included information for 677 patients with ATC treated between 1995 and 2008 at 38 institutions in Japan. As previously described by Sugino et al. [9], patients with incidental-type ATC showed relatively favorable outcomes. In the case of the 547 patients with common-type ATC, age ≥70 years, acute symptoms, leukocytosis, tumor size >5 cm, T4b tumor, and distant metastasis were independent risk factors for cause-specific death on multivariate analysis. In 2001, Sugitani et al. devised a “prognostic index” (PI) based on the number of four unfavorable prognostic factors present in patients with ATC [10]. PI was a useful tool for predicting the prognosis and deciding on the proper therapeutic strategy in individual patients [11]. All four factors for the PI (acute symptoms, leukocytosis, tumor size >5 cm, distant metastasis) were also significant risk factors in the present series.
In terms of treatment methods for ATC, complete resection is considered the cornerstone for longer survival [12–14], and adjuvant RTX and CTX are effective for attaining favorable outcomes [15–17]. Meanwhile, adequate combinations and sequences of therapy for prolonged survival have not yet been sufficiently clarified. Chen et al. noted that the addition of RTX to surgery improved survival for patients with disease extending into adjacent tissue, whereas patients with disease confined to the capsule or who showed further extension or distant metastatic disease did not benefit from RTX after surgery [18]. Our study also showed that adjuvant therapies including RTX and CTX did not provide significant benefits for patients with stage IVA ATC who underwent radical surgery. However, patients who underwent RTX after radical surgery tended to show better outcomes (without statistical significance) than those who underwent radical surgery alone. Further prospective analysis is necessary to evaluate the effectiveness of RTX after radical surgery in stage IVA patients.
On the other hand, for patients with stage IVB ATC with extracapsular disease involving adjacent tissue but no distant metastases, adjuvant multimodal therapy with both RTX and CTX significantly improved the CSS compared to radical surgery alone or surgery with RTX. However, as Passler et al. [12] mentioned, excision of locally advanced tumor causes substantial morbidity on patients. Most of the stage IVB patients who underwent extended radical surgery required tracheostomy and lost their voice, and prolongation of life was limited. The surgical strategy for ATC should be determined by the local tumor extent and the general condition of the patient.
Regarding the selection of CTX for patients with common-type ATC in this study, 98 received etoposide and cisplatin (EP) or etoposide, doxorubicin, and cisplatin (EAP) [19]; 24 underwent chemoradiotherapy using low-dose daily cisplatin, 5-fluorouracil, and doxorubicin [20]; and 14 received induction CTX with weekly paclitaxel [21]. No significant difference in CSS was seen between the three groups. Docetaxel has been introduced more recently as an effective drug for treating ATC [22, 23]. Further prospective comparative studies are necessary to determine the best regimen for CTX.
Although our attempt to collect a large cohort for ATC has been realized in this study with 677 patients, including 547 patients with common-type ATC, we acknowledge that there are some limitations regarding the reliability of data, as this study used a multicenter, retrospective database. Several deficits in data were seen and a pathologic diagnosis was not confirmed in some cases. Detailed evaluation of the extent of thyroidectomy and lymph node dissection [24] and RTX techniques such as hyperfractionation [25, 26] could not be performed in this study. Moreover, the methods applied to assess the extent of disease and indications for therapy were not unified among institutions. Owing to this wide degree of diversity, potential bias remains regarding promising patients with less-advanced disease receiving more-aggressive treatment. When determining the appropriate treatment strategy for patients with ATC, consideration should be given to both UICC stage as an indication of disease extent and other prognostic factors representing the grade of biologic malignancy [11]. For patients who have few risk factors and can expect longer survival, intensive treatment combined radical surgery with RTX and/or CTX is recommended to achieve the best survival results. In such cases, avoiding morbidity is of crucial importance. On the other hand, for patients who cannot anticipate good survival results based on the analysis of prognostic factors, aggressive therapy is likely to worsen the quality of life and occasionally even shorten survival. Best supportive care and local disease control to maintain quality of life and to prevent death from suffocation, dysphagia, and/or bleeding is justifiable for such patients despite the lack of survival benefit (Table 4).
References
Untch BR, Olson JA Jr (2006) Anaplastic thyroid carcinoma, thyroid lymphoma, and metastasis to thyroid. Surg Oncol Clin N Am 15:661–679 x
Kojic SL, Strugnell SS, Wiseman SM (2011) Anaplastic thyroid cancer: a comprehensive review of novel therapy. Expert Rev Anticancer Ther 11:387–402
Hundahl SA, Fleming ID, Fremgen AM et al (1998) A National Cancer Database report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985–1995. Cancer 83:2638–2648
Kitamura Y, Shimizu K, Nagahama M et al (1999) Immediate causes of death in thyroid carcinoma: clinicopathological analysis of 161 fatal cases. J Clin Endocrinol Metab 84:4043–4049
Are C, Shaha AR (2006) Anaplastic thyroid carcinoma: biology, pathogenesis, prognostic factors, and treatment approaches. Ann Surg Oncol 13:453–464
Kebebew E, Greenspan FS, Clark CH et al (2005) Anaplastic thyroid carcinoma: treatment outcome and prognostic factors. Cancer 103:1330–1335
Kim TY, Kim KW, Jung TS et al (2007) Prognostic factors for Korean patients with anaplastic thyroid carcinoma. Head Neck 29:765–772
Besic N, Hocevar M, Zgajnar J et al (2005) Prognostic factors in anaplastic carcinoma of the thyroid: a multivariate survival analysis of 188 patients. Langenbecks Arch Surg 390:203–208
Sugino K, Ito K, Mimura T et al (2002) The important role of operation in the management of anaplastic thyroid carcinoma. Surgery 131:245–248
Sugitani I, Kasai N, Fujimoto Y et al (2001) Prognostic factors and therapeutic strategy for anaplastic carcinoma of the thyroid. World J Surg 25:617–622
Orita Y, Sugitani I, Amemiya T et al (2011) Prospective application of our prognostic index in the treatment of anaplastic thyroid carcinoma. Surgery 150:1212–1219
Passler C, Scheuba C, Prager G et al (1999) Anaplastic (undifferentiated) thyroid carcinoma (ATC): a retrospective analysis. Langenbecks Arch Surg 384:284–293
Pierie JP, Muzikansky A, Gaz RD et al (2002) The effect of surgery and radiotherapy on outcome of anaplastic thyroid carcinoma. Ann Surg Oncol 9:57–64
Ito Y, Higashiyama T, Hirokawa M et al (2009) Investigation of the validity of UICC stage grouping of anaplastic carcinoma of the thyroid. Asian J Surg 32:47–50
Haigh PI, Ituarte PH, Wu HS et al (2001) Completely resected anaplastic thyroid carcinoma combined with adjuvant chemotherapy and irradiation is associated with prolonged survival. Cancer 91:2335–2342
Swaak-Kragten AT, de Wilt JH, Schmitz PI et al (2009) Multimodality treatment for anaplastic thyroid carcinoma: treatment outcome in 75 patients. Radiother Oncol 92:100–104
Ito K, Hanamura T, Murayama K et al (2012) Multimodality therapeutic outcomes in anaplastic thyroid carcinoma: improved survival in subgroups of patients with localized primary tumors. Head Neck 34:230–237
Chen J, Tward JD, Shrieve DC et al (2008) Surgery and radiotherapy improves survival in patients with anaplastic thyroid carcinoma: analysis of the surveillance, epidemiology, and end results 1983–2002. Am J Clin Oncol 31:460–464
Tsutsui K (1995) Treatment for anaplastic carcinoma of the thyroid. Jpn J Cancer Clin 41:137–144 (in Japanese)
Tanaka K, Sugitani I, Fujimoto Y (2011) A novel chemo-radiotherapy with low-dose daily cisplatin, 5-fluorouracil and doxorubicin for anaplastic thyroid carcinoma: a preliminary report. Jpn J Clin Oncol 41:1074–1078
Higashiyama T, Ito Y, Hirokawa M et al (2010) Induction chemotherapy with weekly paclitaxel administration for anaplastic thyroid carcinoma. Thyroid 20:7–14
Troch M, Koperek O, Scheuba C et al (2010) High efficacy of concomitant treatment of undifferentiated (anaplastic) thyroid cancer with radiation and docetaxel. J Clin Endocrinol Metab 95:E54–E57
Kawada K, Kitagawa K, Kamei S et al (2010) The feasibility study of docetaxel in patients with anaplastic thyroid cancer. Jpn J Clin Oncol 40:596–599
Higashiyama T, Ito Y, Hirokawa M et al (2010) Optimal surgical procedure for locally curative surgery in patients with anaplastic thyroid carcinoma: importance of preoperative ultrasonography. Endocr J 57:763–769
Heron DE, Karimpour S, Grigsby PW (2002) Anaplastic thyroid carcinoma: comparison of conventional radiotherapy and hyperfractionation chemoradiotherapy in two groups. Am J Clin Oncol 25:442–446
Tennvall J, Lundell G, Wahlberg P et al (2002) Anaplastic thyroid carcinoma: three protocols combining doxorubicin, hyperfractionated radiotherapy and surgery. Br J Cancer 86:1848–1853
Acknowledgment
This work was supported in part by a grant-in-aid from the Public Trust Fund for Clinical Cancer Research. On behalf of the ATCCJ, we acknowledge and thank the following doctors and participating centers for their involvement in this nationwide study: Dr. Keisei Fujimori, Department of Breast and Endocrine Surgery, Tohoku University Hospital; Dr. Yuichiro Sato, Division of Head and Neck Surgery, Niigata Cancer Center Hospital; Dr. Ken-ichi Ito, Division of Breast and Endocrine Surgery, Shinshu University School of Medicine; Dr. Yuki Tomisawa, Department of Surgery, Iwate Medical University School of Medicine; Dr. Masayuki Tori, Department of Surgery, Osaka Police Hospital; Dr. Katsuhiro Tanaka, Department of Breast and Thyroid Surgery, Kawasaki Medical School; Dr. Nobuyuki Wada, Department of Surgery, Yokohama City University; Dr. Naoyoshi Onoda, Department of Surgical Oncology, Osaka City University Graduate School of Medicine; Dr. Tsuneo Imai, Department of Breast and Endocrine Surgery, Nagoya University; Dr. Makoto Kammori, Department of Surgery, Kanaji Thyroid Hospital; Dr. Yasuhisa Hasegawa, Department of Head and Neck Surgery, Aichi Cancer Center; Dr. Keizo Sugino, Department of Surgery, Akane Foundation Tsuchiya General Hospital; Dr. Hiroyuki Yamada, Department of Otolaryngology, Yamada Red-Cross Hospital; Dr. Tsuyoshi Yoshida, Department of Otolaryngology, Takeda General Hospital; Dr. Hiroshi Hosoi, Department of Otorhinolaryngology–Head and Neck Surgery, Nara Medical University; Dr. Masakazu Miyazaki, Department of Head and Neck Surgery, National Cancer Center East; Dr. Katsumi Iwase, Department of Endocrine Surgery, Fujita Health University; Dr. Masashi Sugasawa, Saitama Medical University International Medical Center; Dr. Yorihisa Orita, Department of Otolaryngology, Okayama Saiseikai General Hospital; Dr. Seiichi Yoshimoto, Department of Head and Neck Oncology, National Cancer Center Hospital; Dr. Tatsuya Uga, Department of Surgery, Nagasaki University; Dr. Atsushi Fukuuchi, Department of Breast and Endocrine Surgery, Mitsui Memorial Hospital; Dr. Hideo Kurihara, Department of Surgery, Kurihara Clinic; Dr. Kazuo Shimizu, Department of Endocrine Surgery, Nippon Medical School; Dr. Hisato Hara, Department of Breast and Endocrine Surgery, University of Tsukuba; Dr. Toshihisa Ogawa, Department of Breast and Endocrine Surgery, University of Tokyo; Dr. Hiroya Kitano, Division of Otolaryngology–Head and Neck Surgery, Department of Medicine of Sensory and Motor Organs, School of Medicine, Faculty of Medicine Tottori University; Dr. Kiyoaki Tsukahara, Tokyo Medical University Hachioji Medical Center, Dr. Minoru Fujimori, Department of Breast Surgery, Tokyo Medical University, Ibaraki Medical Center; Dr. Koki Miura, Head and Neck Oncology Center, International University of Health and Welfare, Mita Hospital; Dr. Yoshiyuki Kadokura, Department of Otolaryngology, Showa University Northern Yokohama Hospital; and Dr. Hirohumi Ami, Department of Surgery, Ohara General Hospital.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sugitani, I., Miyauchi, A., Sugino, K. et al. Prognostic Factors and Treatment Outcomes for Anaplastic Thyroid Carcinoma: ATC Research Consortium of Japan Cohort Study of 677 Patients. World J Surg 36, 1247–1254 (2012). https://doi.org/10.1007/s00268-012-1437-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1437-z