Abstract
Purpose
The evaluation of skeletal fragility in Cushing’s syndrome (CS) is a clinical challenge, since dual-energy X-ray absorptiometry (DXA) does not capture abnormalities in bone microstructure induced by glucocorticoid excess. Hypercortisolism was shown to increase bone marrow adiposity, but it is still unknown whether high bone marrow fat (BMF) as measured by vertebral magnetic resonance spectroscopy may predict fracture risk in this clinical setting. In this cross-sectional study, we evaluated the association between BMF and vertebral fractures (VFs) in patients with CS.
Methods
Twenty patients (5 M, age 44 ± 13 years) with active CS were evaluated for morphometric VFs, lumbar spine BMF, and bone mineral density (BMD). Fifteen healthy volunteers (4 M, age 43 ± 12 years) acted as control group for BMF evaluation.
Results
BMF was significantly higher in CS patients vs. controls (52.0% vs. 27.0%, p < 0.01), and was directly correlated with patients’ age (p = 0.03), 24-hours urine-free cortisol (p = 0.03), midnight serum cortisol (p = 0.02), and serum CTX (p = 0.01). Patients with VFs (13 cases) showed significantly higher BMF vs. patients without VFs (65.0% vs. 24.0%, p = 0.03). Fractured patients with either normal BMD or osteopenia showed comparable BMF to fractured patients with either osteoporosis or low BMD for age (p = 0.71). When the analysis was restricted to patients with normal BMD or osteopenia, VFs were still significantly associated with higher BMF (p = 0.05).
Conclusions
This study provides a first evidence that vertebral adiposity may be a marker of hypercortisolism-induced skeletal fragility and measurement of spine BMF could have a role in the diagnostic work-up for the assessment of fracture risk in CS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic hypercortisolism has multiple severe deleterious systemic effects [1,2,3]. Cushing’s syndrome (CS) frequently causes skeletal fragility as consequence of multiple direct and indirect effects of glucocorticoid excess on bone remodeling and calcium metabolism [4]. Patients with CS characteristically have a low-bone turnover osteoporosis with severe suppression of bone formation and an increased risk of fragility fractures, mainly involving vertebrae and ribs [5, 6]. Noteworthy, vertebral fractures (VFs) may be diagnosed in up to 75% of patients with CS, half of them being clinically symptomatic associated with pain, functional limitation, and height shortening by 3–10 cm of final stature [7].
In the general population, measurement of bone mineral density (BMD) by DXA is used as the primary surrogate of bone strength for clinical diagnosis of osteoporosis [8]. However, in patients with secondary osteoporosis the prediction of fracture risk may be a clinical challenge, since bidimensional DXA measurement of BMD is not able to capture the deterioration of bone quality primarily affected in this clinical setting [9]. As a matter of fact, a remarkable number of patients with CS may fracture in presence of low-normal or even normal BMD values [7, 10,11,12].
Despite the effects of glucocorticoid excess on bone quality being well known and characterized [13,14,15], data on bone microstructure in endogenous hypercortisolism are scant and controversial [12, 16,17,18]. Bone marrow adiposity has been proposed as a reliable biomarker of bone quality and quantity reflecting, the process of mesenchymal stem cell allocation in bone microenvironment and osteoblast differentiation in the basic multicellular units [19, 20]. Using either proton magnetic resonance spectroscopy (MRS) or bone biopsy, some studies reported an association between high bone marrow fat (BMF), low BMD, and high prevalence of VFs in patients with osteoporosis or aging [21,22,23,24]. Noteworthy, high BMF was reported in patients exposed to glucocorticoid excess [25, 26] but is it still unknown whether high bone marrow adiposity may predict fracture risk in this clinical setting [27].
The aim of this cross-section study was to evaluate the association between BMF, as assessed by MRS, and morphometric VFs in patients with active endogenous CS.
Materials and methods
Twenty patients (5 M and 15 F, age 44 ± 13 yrs) with active endogenous CS referring to the Endocrine Unit of the University Hospital “AOU Policlinico G. Martino” of Messina were consecutively enrolled from January 2015 to December 2018. Sixteen patients had ACTH-dependent CS whereas the remaining four patients had ACTH-independent. Diagnosis of CS was performed according to the current guidelines [28]. Thirteen patients had newly diagnosed CS, whereas seven were uncontrolled despite multiple treatments.
Fifteen healthy volunteers (4 M and11 F, age 43 ± 12 yrs), matched for sex and age with the patients, acted as control group for the BMF evaluation.
The exclusion criteria for both patients and controls were: (1) age below 18 years; (2) pregnancy or breastfeeding; (3) BMI above 30 Kg/m2 or below 21 Kg/m2; (4) chronic therapies with drugs potentially causing osteoporosis [29]; (5) treatment with bone active-drugs in the 12 months prior study, except for calcium and vitamin D (2 females and 1 man received supplementation); (6) chronic diseases potentially causing osteoporosis except for CS.
As primary end-point of the study, we evaluated the association between BMF and VFs in patients with active CS. We also explored the following secondary end-points: (1) the association between BMF and VFs in relationship to different BMD categories in patients with CS; (2) determinants of BMF in patients with CS; (3) the difference in BMF between CS and control subjects.
All the patients and volunteers gave their written informed consent, and the study protocol was approved by the Ethic Committee of Messina (Italy).
Evaluation of BMD and VFs
BMD of the lumbar spine was measured by DXA (Hologic Discovery WI). Fractured vertebrae were excluded from the BMD analysis. DXA results were expressed in BMD (g/cm2). In patients aged ≥50 years, BMD was also expressed as T-score, comparing the results with those obtained in a sex-matched Caucasian population at peak of bone mass [8]. A T-score less than or equal to −2.5 SD at the hip or spine was defined as osteoporosis, whereas osteopenia was defined as a T-score between −1 and −2.5 SD. In subjects aged <50 years, the results were expressed as Z-score, comparing the results with those obtained in an age and sex-matched Caucasian population [8]. A Z-score ≤−2.0 SD was used to define a BMD “below the expected range for age”.
VFs were assessed by a quantitative morphometric approach [30]. Using a translucent digitiser and a cursor, six points were marked on each vertebral body to describe vertebral shape. Anterior (Ha), middle (Hm), and posterior (Hp) vertebral heights were measured and height ratios (Ha/Hp, Hm/Hp, Hp/Hp of the above vertebrae, Hp/Hp of the below vertebrae) were calculated for each vertebra from T4 to L4; the fractures were defined mild, moderate and severe based on a height ratio decrease of 20–25%, 26–40%, and more than 40%, respectively [30]. The morphometric analysis was performed by a single operator (G.M.). The intra-observer coefficient of variation, evaluated on a series of 10 measurements, was between 4 and 8%.
Measurement of BMF
All participants underwent MRI acquisition with a 1,5-Tesla unit (Ingenia, Philips Healthcare, Best, Netherlands), in a head-first supine position. Before the MRS analysis, sagittal and coronal T2-weighted images of the lumbar spine were acquired to identify the spectroscopic volume of interest.
Single-voxel MR spectroscopy (SV-H-MRS) was acquired from vertebral body of L3 using point-resolved single-voxel proton spectroscopy (PRESS) acquisition to establish the content of lipids and water. PRESS box (voxel size 4.5 mm3) was positioned in the middle of the vertebral body.
SV-H-MRS was performed using the following parameters: echo time = 37 ms, repetition time = 3000 ms. Spectral data, after baseline, phase and frequency shift rectifications, were elaborated using SIVIC, an extensible, open-source, freely available, and cross-platform software suite designed to support all aspects of MRS data analysis and visualization [31]. Four peaks were well resolved using the present technique: olefinic, double bond -CH=CH- protons at 5.31 ppm, water protons at 4.65 ppm, the CH2methylene protons α- to a double bond (-CH=CHCH2-), at 2.03 ppm, and the bulk CH2methylene protons at 1.3 ppm. The BMF was expressed in percentage and calculated as previously described [32]: Fat content = Imethylene/(Imethylene + Iwater) × 100%, where Imethylene and Iwater were the signal amplitudes of the bulk methylene peak (1.3 ppm) and the water peak (4.65 ppm), respectively.
Biochemical assays
Peripheral blood samples were collected after overnight fasting. All samples were processed in the laboratory of the University Hospital of Messina. Calcium and phosphorus were measured by standard analytical methods. ACTH (Medical Systems SPA, Genova, Italy), cortisol (Beckman Coulter, USA), 24-hours urinary-free cortisol (Beckman Coulter, USA), DHEAS (Beckman Coulter, USA) were measured by commercial chemiluminescence immunoassays, while PTH and osteocalcin (Cisbio Bioassays, France) by radioimmunoassays. CTX and 25(OH)D3 were measured by HPLC (Bio-Rad Laboratories S.r.l., Milano, Italy).
Statistical analysis
All data were expressed as the median and range. Un-paired data were compared using Mann–Whitney test. Multiple comparisons were performed by Kruskal–Wallis test. Frequencies were compared using χ2 test with Fisher correction, when appropriate. Spearman correlation test was applied in order to assess the existence of significant association between L3 BMF and several variables evaluated in the study. The receiver operating characteristic (ROC) curve analysis was performed to assess the best cut-off of BMF associated with VFs. Statistical significance was assumed when p-values were ≤0.05.
Results
In CS patients aged ≥50 years (11 cases), osteoporosis was found in three patients (27.3%), whereas osteopenia and normal BMD were found in five (45.5%) and three (27.7%) patients, respectively. In CS patients aged <50 years (9 cases), the prevalence of lumbar spine BMD “below the expected range for age” was 33.3%.
VFs were found in 13 CS patients (65.0%); five patients had a single fracture, whereas in eight patients two or more vertebral fractures were found. The fractures were mild in six patients, while the remaining seven patients had moderate or severe fractures. Patients with VFs were significantly older as compared to patients who did not fracture, without significant differences in other demographical and clinical features (Table 1). Moreover, fractured patients had significantly lower lumbar spine BMD as compared to those without fractures (Table 1). Among patients with VFs, 7 (53.8%) had either osteoporosis or “low BMD form age” and 6 (46.2%) had either osteopenia or normal BMD (p = 0.05 vs. non-fractured patients).
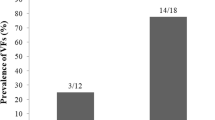
Patients with CS had significantly higher BMF as compared to control subjects (52.0%, range: 11–84 vs. 27.0%, range: 10–58; p < 0.01). In CS, BMF was significantly associated with patients’s age (rho 0.48; p = 0.03), 24-hours urine free cortisol values (rho: 0.48; p = 0.03), midnight serum cortisol values (rho: 0.50; p = 0.02) and serum CTX (rho: 0.54; p = 0.01). No significant association was found between BMF and lumbar spine BMD (p = 0.13 for both T-score and Z-score). BMF resulted to be significantly (p = 0.03) higher in patients with VFs as compared to those who did not fracture (Fig. 1). These latter patients showed no significant difference in BMF vs. controls subjects (Fig. 1).
Bone marrow fat (BMF) content in vertebra L3 of Cushing’s syndrome (CS) patients with or without vertebral fractures (VFs) as compared to control subjects. Data were presented as median, 25th and 75th percentile and range. Data were compared by non-parametric tests. *p < 0.05 CS with VFs vs. CS without VFs and control subjects. The difference between CS without VFs and controls was not statistically significant
The ROC analysis showed that BMF have enough accuracy in identifying patients with VFs (area under the ROC curve: 0.797). The cut-off with the best compromise between sensitivity (61.5%) and specificity (71.4%) was set at 52%.
Looking at the individual data and stratifying the patients for BMD categories (Table 2), fractured patients with either normal BMD or osteopenia showed comparable BMF to fractured patients with either osteoporosis or “low BMD for age” (66.0%, range: 38–84 vs 59.0%, range: 27-84; p = 0.71). When the analysis was restricted to patients with either normal BMD or osteopenia (Table 2), VFs were still significantly associated with higher BMF (66.0%, range: 38–84 vs. 24.0%, range: 11–66; fractured vs. non-fractured patients, p = 0.05).
Discussion
This study showed that patients with active CS and VFs had higher BMF as compared to patients who did not fracture.
In vitro studies have demonstrated that glucocorticoids are essential for the differentiation of mesenchymal cells (usually derived from bone marrow) into mature osteoblasts [33]. However, when glucocorticoids are in excess, osteoblastogenesis is impaired and the differentiation of stromal cells is redirected toward adipogenesis [4]. Mechanisms involved are induction of peroxisome proliferator activated receptor γ2, the regulation of nuclear factors of the CAAT enhancer-binding protein family [34, 35], inhibition of Wnt/beta-catenin signaling and repression of BMP-2 [36, 37]. A recent study reported high bone marrow adiposity in patients with active hypercortisolism [26]. This finding was confirmed by our study which also reported a significant association between BMF and the severity of hypercortisolism, consistently with the concept that glucocorticoid excess was directly responsible for the increased number of adipocytes in the bone microenvironment. Noteworthy, the increase in BMF in our patients was demonstrated using a less sensitive but more widespread MR machine than those used in the previous study [26], suggesting that the spectroscopy analysis of bone marrow adiposity may be a feasible diagnostic tool in the real-life clinical practice.
Applying a morphometric approach, more than 60% of patients were found to have VFs, seven of them being either severe or multiple. This finding is remarkable if considering the potential negative effects of VFs on quality of life of patients with CS [7], such as already demonstrated in the general population [38]. Although the small size of study group did not allow to reach the statistical significance, we found a clinically significant difference in midnight serum cortisol values between fractured and non-fractured patients, consistent with the concept that skeletal fragility and VFs were a direct consequence of hypercortisolism. For the first time, we reported an association between VFs and higher BMF at lumbar spine, providing a first evidence that bone marrow adiposity may be a marker of skeletal fragility in patients with CS. This hypothesis was also supported by the finding of association between BMF and CTX, a reliable marker of bone resorption [39, 40], suggesting that bone marrow adiposity may influence not only osteoblastogenesis but also osteoclastogenesis and bone resorption [41].
Lumbar spine BMD was shown to be one of the predictors of fractures in untreated CS [7]. Consistently with this finding, overall our fractured patients had lower lumbar spine BMD as compared to patients who did not fracture. However, looking at the individual data about one-half of our patients with VFs had low-normal or even normal BMD values. Similarly to other forms of secondary osteoporosis [42,43,44], the prediction of VFs in CS is a clinical challenge [45]. As a matter of fact, DXA analysis of BMD does not allow to capture the abnormalities of bone quality induced by glucocorticoid excess. In fact, trabecular [12, 18, 46] and cortical [16] bone microstructure was shown to be deteriorated more than BMD in patients with endogenous hypercortisolism. Noteworthy, abnormalities in trabecular bone structure as measured by trabecular bone score (TBS), that is a gray-level textural metric extracted from the two-dimensional lumbar spine DXA images [47], were shown to be associated with higher risk of fractures in patients with endogenous hypercortisolism regardless of BMD values [18, 48]. Consistently with this finding, in our patients with active disease BMF was not associated with BMD and fractured patients showed higher BMF even in presence of normal and low-normal BMD.
The present study has some limitations. Firstly, the cross-sectional design did not allow to investigate the timing of VFs development and the temporal relationship between the increase in BMF and the occurrence of fractures. Since information on body composition were not available, we cannot completely rule out that BMF values in our patients may be influenced by the increase in visceral fat induced by glucocorticoid excess [49, 50]. However, the exclusion of obese patients from the study may have weakened the potential effect of visceral fat on bone marrow adiposity. Moreover, the contribution of menopause to BMF in CS women with fractures cannot be quantified although it’s worth of noting that 4 out of 5 post-menopausal women had osteopenia. An uncoupled low-bone formation and slightly increase in bone resorption was reported in patients with CS [46, 51], but the impact of this biochemical phenotype on fracture risk is unknown. In our study, no statistically significant differences in osteocalcin and CTX between fractured and non-fractured patients were found. However, unexpectedly, median osteocalcin was shown to be more than twice higher in patients with VFs as compared to those who did not fracture. This finding may reflect the heterogeneity of study group in terms of age, gonadal status and etiology of CS which did not allow to properly analyze the diagnostic value of biochemical markers of bone turnover in identifying patients with skeletal fragility. Indeed, the use of bone markers in clinical practice is still complicated mainly due to analytical variability of these substances [52]. Furthermore, the small number of patients did not allow to perform a multivariate analysis to reliably assess the effect of BMF on risk of fractures independent of BMD, age, and severity of hypercortisolism which were shown to be associated with VFs in the univariate analysis. We partially resolved this methodological shortcoming by analyzing the patients stratified for BMD values. Such an approach allowed us to hypothesize that MRS measurement of BMF may be more informative than DXA measurement of BMD in identifying patients with skeletal fragility induced by glucocorticoid excess. Specifically, based on the results of this study, MRS measurement of BMF may be useful in CS patients with either osteopenia or normal BMD in order to identify subjects with otherwise undiagnosed by DXA skeletal fragility who are at high risk of fractures. Moreover, in these cases, MRI images may be also used for morphometric diagnosis of VFs [53].
In conclusion, this preliminary study provides first evidence that vertebral adiposity is a marker of hypercortisolism-induced skeletal fragility. Future prospective studies on larger CS populations are needed to assess the accuracy of MRS in the diagnostic work-up of skeletal fragility induced by glucocorticoid excess.
References
R. Pivonello, A.M. Isidori, M.C. De Martino, J. Newell-Price, B.M. Biller, A. Colao, Complications of Cushing’s syndrome: state of the art. Lancet Diabetes Endocrinol. 4, 611–629 (2016). https://doi.org/10.1016/S2213-8587(16)00086-3
F. Ferrau, M. Korbonits, Metabolic syndrome in Cushing’s syndrome patients. Front. Horm. Res. 49, 85–103 (2018). https://doi.org/10.1159/000486002
A.M. Isidori, C. Graziadio, R.M. Paragliola, A. Cozzolino, A.G. Ambrogio, A. Colao, S.M. Corsello, R. Pivonello, A.B.C.S. Group, The hypertension of Cushing’s syndrome: controversies in the pathophysiology and focus on cardiovascular complications. J. Hypertens. 33, 44–60 (2015). https://doi.org/10.1097/HJH.0000000000000415
E. Canalis, G. Mazziotti, A. Giustina, J.P. Bilezikian, Glucocorticoid-induced osteoporosis: pathophysiology and therapy. Osteoporos. Int. 18, 1319–1328 (2007). https://doi.org/10.1007/s00198-007-0394-0
G. Mazziotti, A. Delgado, F. Maffezzoni, A. Formenti, A. Giustina, Skeletal fragility in endogenous hypercortisolism. Front. Horm. Res. 46, 66–73 (2016). https://doi.org/10.1159/000443866
A. Scillitani, G. Mazziotti, C. Di Somma, S. Moretti, A. Stigliano, R. Pivonello, A. Giustina, A. Colao, Treatment of skeletal impairment in patients with endogenous hypercortisolism: when and how? Osteoporos. Int. 25, 441–446 (2014). https://doi.org/10.1007/s00198-013-2588-y
L. Tauchmanova, R. Pivonello, C. Di Somma, R. Rossi, M.C. De Martino, L. Camera, M. Klain, M. Salvatore, G. Lombardi, A. Colao, Bone demineralization and vertebral fractures in endogenous cortisol excess: role of disease etiology and gonadal status. J. Clin. Endocrinol. Metab. 91, 1779–1784 (2006). https://doi.org/10.1210/jc.2005-0582
Schousboe, J.T., Shepherd, J.A., Bilezikian, J.P., Baim, S. Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on bone densitometry. J. Clin. Densitom. 16, 455–466 (2013). https://doi.org/10.1016/j.jocd.2013.08.004
G. Mazziotti, J. Bilezikian, E. Canalis, D. Cocchi, A. Giustina, New understanding and treatments for osteoporosis. Endocrine 41, 58–69 (2012). https://doi.org/10.1007/s12020-011-9570-2
L. Trementino, G. Appolloni, L. Ceccoli, G. Marcelli, C. Concettoni, M. Boscaro, G. Arnaldi, Bone complications in patients with Cushing’s syndrome: looking for clinical, biochemical, and genetic determinants. Osteoporos. Int. 25, 913–921 (2014). https://doi.org/10.1007/s00198-013-2520-5
E. Valassi, A. Santos, M. Yaneva, M. Toth, C.J. Strasburger, P. Chanson, J.A. Wass, O. Chabre, M. Pfeifer, R.A. Feelders, S. Tsagarakis, P.J. Trainer, H. Franz, K. Zopf, S. Zacharieva, S.W. Lamberts, A. Tabarin, S.M. Webb, The European Registry on Cushing’s syndrome: 2-year experience. Baseline demographic and clinical characteristics. Eur. J. Endocrinol. 165, 383–392 (2011). https://doi.org/10.1530/eje-11-0272
Z.E. Belaya, D. Hans, L.Y. Rozhinskaya, N.V. Dragunova, N.I. Sasonova, A.G. Solodovnikov, T.T. Tsoriev, L.K. Dzeranova, G.A. Melnichenko, I.I. Dedov, The risk factors for fractures and trabecular bone-score value in patients with endogenous Cushing’s syndrome. Arch. Osteoporos. 10, 44 (2015). https://doi.org/10.1007/s11657-015-0244-1
G. Mazziotti, A. Angeli, J.P. Bilezikian, E. Canalis, A. Giustina, Glucocorticoid-induced osteoporosis: an update. Trends Endocrinol. Metab. 17, 144–149 (2006). https://doi.org/10.1016/j.tem.2006.03.009
H. Tsugeno, B. Goto, T. Fujita, M. Okamoto, T. Mifune, F. Mitsunobu, K. Ashida, Y. Hosaki, T. Tsuji, Y. Tanizaki, Oral glucocorticoid-induced fall in cortical bone volume and density in postmenopausal asthmatic patients. Osteoporos. Int. 12, 266–270 (2001). https://doi.org/10.1007/s001980170115
L. Dalle Carbonare, M.E. Arlot, P.M. Chavassieux, J.P. Roux, N.R. Portero, P.J. Meunier, Comparison of trabecular bone microarchitecture and remodeling in glucocorticoid-induced and postmenopausal osteoporosis. J. Bone Miner. Res. 16, 97–103 (2001). https://doi.org/10.1359/jbmr.2001.16.1.97
C.V. dos Santos, L. Vieira Neto, M. Madeira, M.C. Alves Coelho, L.M. de Mendonca, P. Paranhos-Neto Fde, I.C. Lima, M.R. Gadelha, M.L. Farias, Bone density and microarchitecture in endogenous hypercortisolism. Clin. Endocrinol. 83, 468–474 (2015). https://doi.org/10.1111/cen.12812
G. Mazziotti, S. Frara, A. Giustina, Pituitary diseases and bone. Endocr. Rev. 39, 440–488 (2018). https://doi.org/10.1210/er.2018-00005
C. Eller-Vainicher, V. Morelli, F.M. Ulivieri, S. Palmieri, V.V. Zhukouskaya, E. Cairoli, R. Pino, A. Naccarato, A. Scillitani, P. Beck-Peccoz, I. Chiodini, Bone quality, as measured by trabecular bone score in patients with adrenal incidentalomas with and without subclinical hypercortisolism. J. Bone Miner. Res. 27, 2223–2230 (2012). https://doi.org/10.1002/jbmr.1648
C.J. Rosen, C. Ackert-Bicknell, J.P. Rodriguez, A.M. Pino, Marrow fat and the bone microenvironment: developmental, functional, and pathological implications. Crit. Rev. Eukaryot. Gene Expr. 19, 109–124 (2009)
E.J. Moerman, K. Teng, D.A. Lipschitz, B. Lecka-Czernik, Aging activates adipogenic and suppresses osteogenic programs in mesenchymal marrow stroma/stem cells: the role of PPAR-gamma2 transcription factor and TGF-beta/BMP signaling pathways. Aging Cell 3, 379–389 (2004). https://doi.org/10.1111/j.1474-9728.2004.00127.x
F.W. Wehrli, J.A. Hopkins, S.N. Hwang, H.K. Song, P.J. Snyder, J.G. Haddad, Cross-sectional study of osteopenia with quantitative MR imaging and bone densitometry. Radiology 217, 527–538 (2000). https://doi.org/10.1148/radiology.217.2.r00nv20527
J. Justesen, K. Stenderup, E.N. Ebbesen, L. Mosekilde, T. Steiniche, M. Kassem, Adipocyte tissue volume in bone marrow is increased with aging and in patients with osteoporosis. Biogerontology 2, 165–171 (2001)
A.V. Schwartz, S. Sigurdsson, T.F. Hue, T.F. Lang, T.B. Harris, C.J. Rosen, E. Vittinghoff, K. Siggeirsdottir, G. Sigurdsson, D. Oskarsdottir, K. Shet, L. Palermo, V. Gudnason, X. Li, Vertebral bone marrow fat associated with lower trabecular BMD and prevalent vertebral fracture in older adults. J. Clin. Endocrinol. Metab. 98, 2294–2300 (2013). https://doi.org/10.1210/jc.2012-3949
J.F. Griffith, D.K. Yeung, G.E. Antonio, F.K. Lee, A.W. Hong, S.Y. Wong, E.M. Lau, P.C. Leung, Vertebral bone mineral density, marrow perfusion, and fat content in healthy men and men with osteoporosis: dynamic contrast-enhanced MR imaging and MR spectroscopy. Radiology 236, 945–951 (2005). https://doi.org/10.1148/radiol.2363041425
E.B. Geer, W. Shen, E. Strohmayer, K.D. Post, P.U. Freda, Body composition and cardiovascular risk markers after remission of Cushing’s disease: a prospective study using whole-body MRI. J. Clin. Endocrinol. Metab. 97, 1702–1711 (2012). https://doi.org/10.1210/jc.2011-3123
F. Maurice, A. Dutour, C. Vincentelli, I. Abdesselam, M. Bernard, H. Dufour, Y. Le Fur, T. Graillon, F. Kober, P. Cristofari, E. Jouve, L. Pini, R. Fernandez, C. Chagnaud, T. Brue, F. Castinetti, B. Gaborit, Active cushing syndrome patients have increased ectopic fat deposition and bone marrow fat content compared to cured patients and healthy subjects: a pilot 1H-MRS study. Eur. J. Endocrinol. 179, 307–317 (2018). https://doi.org/10.1530/eje-18-0318
G.M. Blake, J.F. Griffith, D.K. Yeung, P.C. Leung, I. Fogelman, Effect of increasing vertebral marrow fat content on BMD measurement, T-Score status and fracture risk prediction by DXA. Bone 44, 495–501 (2009). https://doi.org/10.1016/j.bone.2008.11.003
L.K. Nieman, B.M. Biller, J.W. Findling, M.H. Murad, J. Newell-Price, M.O. Savage, A. Tabarin, Treatment of Cushing’s Syndrome: an Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 100, 2807–2831 (2015). https://doi.org/10.1210/jc.2015-1818
G. Mazziotti, E. Canalis, A. Giustina, Drug-induced osteoporosis: mechanisms and clinical implications. Am. J. Med. 123, 877–884 (2010). https://doi.org/10.1016/j.amjmed.2010.02.028
H.K. Genant, M. Jergas, L. Palermo, M. Nevitt, R.S. Valentin, D. Black, S.R. Cummings, Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis The Study of Osteoporotic Fractures Research Group. J. Bone Miner. Res. 11, 984–996 (1996). https://doi.org/10.1002/jbmr.5650110716
J.C. Crane, M.P. Olson, S.J. Nelson, SIVIC: Open-Source, Standards-Based Software for DICOM MR Spectroscopy Workflows. Int. J. Biomed. Imaging 2013, 169526 (2013). https://doi.org/10.1155/2013/169526
X. Li, D. Kuo, A.L. Schafer, A. Porzig, T.M. Link, D. Black, A.V. Schwartz, Quantification of vertebral bone marrow fat content using 3 Tesla MR spectroscopy: reproducibility, vertebral variation, and applications in osteoporosis. J. Magn. Reson. Imaging 33, 974–979 (2011). https://doi.org/10.1002/jmri.22489
V. Shalhoub, D. Conlon, M. Tassinari, C. Quinn, N. Partridge, G.S. Stein, J.B. Lian, Glucocorticoids promote development of the osteoblast phenotype by selectively modulating expression of cell growth and differentiation associated genes. J. Cell. Biochem. 50, 425–440 (1992). https://doi.org/10.1002/jcb.240500411
A. Wedel, H.W. Ziegler-Heitbrock, The C/EBP family of transcription factors. Immunobiology 193, 171–185 (1995)
Z. Wu, N.L. Bucher, S.R. Farmer, Induction of peroxisome proliferator-activated receptor gamma during the conversion of 3T3 fibroblasts into adipocytes is mediated by C/EBPbeta, C/EBPdelta, and glucocorticoids. Mol. Cell. Biol. 16, 4128–4136 (1996)
K. Ohnaka, M. Tanabe, H. Kawate, H. Nawata, R. Takayanagi, Glucocorticoid suppresses the canonical Wnt signal in cultured human osteoblasts. Biochem. Biophys. Res. Commun. 329, 177–181 (2005). https://doi.org/10.1016/j.bbrc.2005.01.117
E. Smith, B. Frenkel, Glucocorticoids inhibit the transcriptional activity of LEF/TCF in differentiating osteoblasts in a glycogen synthase kinase-3beta-dependent and -independent manner. J. Biol. Chem. 280, 2388–2394 (2005). https://doi.org/10.1074/jbc.M406294200
A. Oleksik, P. Lips, A. Dawson, M.E. Minshall, W. Shen, C. Cooper, J. Kanis, Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J. Bone Miner. Res. 15, 1384–1392 (2000). https://doi.org/10.1359/jbmr.2000.15.7.1384
S. Vasikaran, R. Eastell, O. Bruyere, A.J. Foldes, P. Garnero, A. Griesmacher, M. McClung, H.A. Morris, S. Silverman, T. Trenti, D.A. Wahl, C. Cooper, J.A. Kanis, Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos. Int. 22, 391–420 (2011). https://doi.org/10.1007/s00198-010-1501-1
S.D. Vasikaran, S.A. Chubb, The use of biochemical markers of bone turnover in the clinical management of primary and secondary osteoporosis. Endocrine 52, 222–225 (2016). https://doi.org/10.1007/s12020-016-0900-2
V. Sottile, K. Seuwen, M. Kneissel, Enhanced marrow adipogenesis and bone resorption in estrogen-deprived rats treated with the PPARgamma agonist BRL49653 (rosiglitazone). Calcif. Tissue Int. 75, 329–337 (2004). https://doi.org/10.1007/s00223-004-0224-8
R. Pedersini, S. Monteverdi, G. Mazziotti, V. Amoroso, E. Roca, F. Maffezzoni, L. Vassalli, F. Rodella, A.M. Formenti, S. Frara, R. Maroldi, A. Berruti, E. Simoncini, A. Giustina, Morphometric vertebral fractures in breast cancer patients treated with adjuvant aromatase inhibitor therapy: a cross-sectional study. Bone 97, 147–152 (2017). https://doi.org/10.1016/j.bone.2017.01.013
T. Mancini, G. Mazziotti, M. Doga, R. Carpinteri, N. Simetovic, P.P. Vescovi, A. Giustina, Vertebral fractures in males with type 2 diabetes treated with rosiglitazone. Bone 45, 784–788 (2009). https://doi.org/10.1016/j.bone.2009.06.006
G. Mazziotti, C. Dordoni, M. Doga, F. Galderisi, M. Venturini, P. Calzavara-Pinton, R. Maroldi, A. Giustina, M. Colombi, High prevalence of radiological vertebral fractures in adult patients with Ehlers-Danlos syndrome. Bone 84, 88–92 (2016). https://doi.org/10.1016/j.bone.2015.12.007
L. Trementino, L. Ceccoli, C. Concettoni, G. Marcelli, G. Michetti, M. Boscaro, G. Arnaldi, Fracture risk assessment before and after resolution of endogenous hypercortisolism: is the FRAX(R) algorithm useful? J. Endocrinol. Invest. 37, 957–965 (2014). https://doi.org/10.1007/s40618-014-0126-1
I. Chiodini, V. Carnevale, M. Torlontano, S. Fusilli, G. Guglielmi, M. Pileri, S. Modoni, A. Di Giorgio, A. Liuzzi, S. Minisola, M. Cammisa, V. Trischitta, A. Scillitani, Alterations of bone turnover and bone mass at different skeletal sites due to pure glucocorticoid excess: study in eumenorrheic patients with Cushing’s syndrome. J. Clin. Endocrinol. Metab. 83, 1863–1867 (1998). https://doi.org/10.1210/jcem.83.6.4880
N.C. Harvey, C.C. Gluer, N. Binkley, E.V. McCloskey, M.L. Brandi, C. Cooper, D. Kendler, O. Lamy, A. Laslop, B.M. Camargos, J.Y. Reginster, R. Rizzoli, J.A. Kanis, Trabecular bone score (TBS) as a new complementary approach for osteoporosis evaluation in clinical practice. Bone 78, 216–224 (2015). https://doi.org/10.1016/j.bone.2015.05.016
Vinolas, H., Grouthier, V., Mehsen-Cetre, N., Boisson, A., Winzenrieth, R., Schaeverbeke, T., Mesguich, C., Bordenave, L., Tabarin, A. Assessment of vertebral microarchitecture in overt and mild Cushing’s syndrome using trabecular bone score. Clin. Endocrinol. (2018). https://doi.org/10.1111/cen.13743
U. Schafroth, K. Godang, T. Ueland, J.P. Berg, J. Bollerslev, Leptin levels in relation to body composition and insulin concentration in patients with endogenous Cushing’s syndrome compared to controls matched for body mass index. J. Endocrinol. Invest. 23, 349–355 (2000). https://doi.org/10.1007/bf03343737
W. Shen, J. Chen, M. Punyanitya, S. Shapses, S. Heshka, S.B. Heymsfield, MRI-measured bone marrow adipose tissue is inversely related to DXA-measured bone mineral in Caucasian women. Osteoporos. Int. 18, 641–647 (2007). https://doi.org/10.1007/s00198-006-0285-9
C. Di Somma, R. Pivonello, S. Loche, A. Faggiano, P. Marzullo, A. Di Sarno, M. Klain, M. Salvatore, G. Lombardi, A. Colao, Severe impairment of bone mass and turnover in Cushing’s disease: comparison between childhood-onset and adulthood-onset disease. Clin. Endocrinol. 56, 153–158 (2002)
M.C. Vlot, M. den Heijer, R.T. de Jongh, M.G. Vervloet, W.F. Lems, R. de Jonge, B. Obermayer-Pietsch, A.C. Heijboer, Clinical utility of bone markers in various diseases. Bone 114, 215–225 (2018). https://doi.org/10.1016/j.bone.2018.06.011
A. Bazzocchi, G. Garzillo, F. Fuzzi, D. Diano, U. Albisinni, E. Salizzoni, G. Battista, G. Guglielmi, Localizer sequences of magnetic resonance imaging accurately identify osteoporotic vertebral fractures. Bone 61, 158–163 (2014). https://doi.org/10.1016/j.bone.2014.01.013
Funding
This work was funded by a grant of the Ministry of Education, University and Research of the Italian Government (PRIN 2015 - Grant number 2015ZHKFTA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
G.M. received consultant fees by Ipsen and Novartis; A.L. received grants from Ipsen, Pfizer, Novartis and speaker honoraria from Ipsen and Pfizer; S.C. served in medical advisory boards of HRA. The remaining authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ferraù, F., Giovinazzo, S., Messina, E. et al. High bone marrow fat in patients with Cushing’s syndrome and vertebral fractures. Endocrine 67, 172–179 (2020). https://doi.org/10.1007/s12020-019-02034-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-02034-4