Abstract
Vertebral fractures are an emerging complication of acromegaly but their prediction is still difficult occurring even in patients with normal bone mineral density. In this study we evaluated the ability of high-resolution cone-beam computed tomography to provide information on skeletal abnormalities associated with vertebral fractures in acromegaly. 40 patients (24 females, 16 males; median age 57 years, range 25–72) and 21 healthy volunteers (10 females, 11 males; median age 60 years, range: 25–68) were evaluated for trabecular (bone volume/trabecular volume ratio, mean trabecular separation, and mean trabecular thickness) and cortical (thickness and porosity) parameters at distal radius using a high-resolution cone-beam computed tomography system. All acromegaly patients were evaluated for morphometric vertebral fractures and for mineral bone density by dual-energy X-ray absorptiometry at lumbar spine, total hip, femoral neck, and distal radius. Acromegaly patients with vertebral fractures (15 cases) had significantly (p < 0.05) lower bone volume/trabecular volume ratio, greater mean trabecular separation, and higher cortical porosity vs. nonfractured patients, without statistically significant differences in mean trabecular thickness and cortical thickness. Fractured and nonfractured acromegaly patients did not have significant differences in bone density at either skeletal site. Patients with acromegaly showed lower bone volume/trabecular volume ratio (p = 0.003) and mean trabecular thickness (p < 0.001) and greater mean trabecular separation (p = 0.02) as compared to control subjects, without significant differences in cortical thickness and porosity. This study shows for the first time that abnormalities of bone microstructure are associated with radiological vertebral fractures in acromegaly. High-resolution cone-beam computed tomography at the distal radius may be useful to evaluate and predict the effects of acromegaly on bone microstructure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acromegaly is an insidious disorder characterized by excessive secretion of growth hormone (GH) generally caused by a pituitary adenoma, resulting in elevations of circulating levels of GH and insulin-like growth factor (IGF-I) [1]. Acromegaly is associated with an average 10-year reduction in life expectancy and a double standardized mortality rate as compared to the general population [2]. Skeletal fragility is an emerging complication of acromegaly [3] deriving from a chronic stimulation of bone turnover induced by GH excess [4–6]. As a matter of fact, over the last 10 years several studies have reported high prevalence [7–9] and incidence [10, 11] of vertebral fractures (VFs) in patients with acromegaly. However, bone mineral density (BMD) is low in only a minority of acromegaly patients [5] and VFs were shown to occur even in patient with normal BMD [7, 8]. Indeed, there is evidence that GH hypersecretion causes deleterious effects on trabecular microarchitecture whereas cortical bone density tends to be increased as effect of GH on periostal ossification [12, 13]. Dual-energy X-ray absorptiometry (DXA) does not distinguish between the cortical and trabecular bone and the densitometric results are greatly influenced by the variable distribution of these compartments in the different skeletal sites. Moreover, DXA does not quantify some of the factors that contribute to bone strength, such as the bone-tissue properties, morphology, and microarchitecture. Many of the limitations of areal DXA measurement can be overcome by computed tomography techniques that allow higher spatial resolution, improved delineation of bone architecture, and acquisition of near isotropic volumetric datasets [14]. However, only few clinical studies were carried out with tomography techniques in acromegaly [12, 15] and they did not investigate the correlation between abnormalities of bone microstructures and fragility fractures in this clinical setting. In this cross-sectional study, we aimed at characterizing for the first time the specific abnormalities of cortical and trabecular bone structures associated with radiological VFs in patients with acromegaly. Bone microstructure was evaluated at distal radius using high-resolution cone-beam computed tomography (HR-CBCT) [16].
Materials and methods
Subjects
This cross-sectional study included patients attending our out-patient endocrine clinic. Inclusion criteria were: (1) diagnosis of acromegaly and (2) age older than 18 years. Exclusion criteria were: (1) neoplastic diseases in progression; (2) treatment with anti-osteoporotic drugs except for calcium and vitamin D; (3) treatment with drugs causing osteoporosis [17], as glucocorticoids (except of those used to replace hypopituitarism), aromatase inhibitors, thiazolinediones, selective serotonin reuptake inhibitors, anticonvulsants, and anti-retroviral drugs; (4) prolonged immobilization; (5) trauma; (6) surgical intervention on the spine.
Acromegaly was diagnosed by failure of suppression of serum GH concentrations below 1 ng/ml after a 75-g oral glucose load together with fasting plasma IGF-1 concentrations above the normal ranges for age [18]. Among 44 acromegaly patients consecutively attending our out-patient endocrine clinic in the period June 2013 and December 2015, 40 patients (24 females, 16 males; median age 57, range 25–72) who met the inclusion criteria were included in the study. Fourteen patients had been already enrolled in our previously published cross-sectional e prospective studies [7, 8, 10].
At the study entry, 7 patients were cured after neurosurgery, 13 had controlled disease by somatostatin analog (12 cases) or pegvisomant (1 patient) treatment, whereas the remaining 20 patients had active acromegaly disease notwithstanding different treatments [19]. Patients under somatostatin analogs were evaluated by measurement of serum random GH and IGF-I, those under pegvisomant were evaluated by serum IGF-I alone, whereas patients treated with neurosurgery alone were evaluated also by serum GH after a 75-g oral glucose tolerance test [19]. Acromegaly was defined controlled if IGF-I values were in the reference ranges for age and, in patients under somatostatin analogs and after neurosurgery, random GH was below 1.0 ng/ml. When oral glucose tolerance test was performed, GH values equal or below 0.4 ng/ml were considered expression of cured disease [20].
In all patients, the median duration of active disease was estimated on the basis of clinical history, i.e., when the patient recalled appearance of signs and symptoms of the disease, and duration of uncontrolled disease during medical treatment.
At the study entry, 7 patients had glucocorticoid deficiency, 14 had hypothyroidism and 25 were hypogonadal (16 post-menopausal women, 2 pre-menopausal women and 7 males). All patients with glucocorticoid deficiency and hypothyroidism were on replacement therapy, whereas only 6 out of 25 patients with hypogonadism (5 men and 1 pre-menopausal woman) were adequately replaced for this deficiency. Patients with diagnosis of hypogonadism under replacement treatment with sex steroids were considered eugonadal if treatment was started at least 12 months prior the study entry. Vitamin D status of acromegaly patients was retrospectively assessed using 25-hydroxyvitamin D values measured within 1 month before the enrollment and available in the clinical files. Hypovitaminosis D was defined by serum 25-hydroxyvitamin D values below 30 ng/ml. All patients had an history of hypovitaminosis D and were on treatment with cholecalciferol ± calcium at the time of study entry. At the study entry, 28 had persistent hypovitaminosis D notwithstanding vitamin D replacement therapy. Ten patients were affected by diabetes mellitus [21].
Twenty-one healthy volunteers (10 females and 11 males; median age 60 years, range: 25–68) were enrolled as controls for the evaluation of cortical and trabecular bone structure by HR-CBCT. The control subjects were consecutively recruited among the hospital staff after the enrollment of acromegaly patients. The criteria used to select control subjects were: (1) age and sex distribution consistent with that of acromegaly patients; (2) no personal history of pituitary diseases and osteoporosis; (3) no treatment with drugs potentially causing osteoporosis [17]; (4) no familiar history of osteoporosis and fragility fractures; (5) willingness to perform HR-CBCT evaluation. The recruitment was stopped when the control group was comparable for sex and age to acromegaly patients. Control subjects did not undergo DXA scan and morphometric evaluations since the additional radiation exposure, although minimal, was not considered ethically justified in view of the aims of the study (see below). The patients and control subjects gave informed consent to the study that was approved by local Ethical Committee.
Study Protocol
The main end-point of the study was to evaluate whether prevalent VFs in acromegaly patients were associated with abnormalities of trabecular and/or cortical cortical bone, as assessed by HR-CBCT at distal radius. As secondary end-points, we evaluated: (1) the differences in CBCT bone parameters between acromegaly and control subjects and (2) the determinants of CBCT parameters in patients with acromegaly.
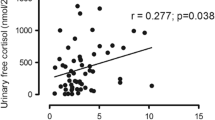
Geometric trabecular parameters and cortical thickness were measured at the distal radius using a high-resolution CBCT system (Newtom 5G; QR, Verona, Italy) with an isotropic voxel size of 75 microns and a fixed tube voltage of 110 kV. Forearms were scanned with 8 × 8 cm2 FOV starting from the styloid process of the radius (Supplementary Fig. 1). Images were imported to ImageJ 1.48v (Rasband, W.S., ImageJ, U.S. National Institutes of Health, Bethesda, MD, USA). The BoneJ 1.3.9 program [22] was applied to measure five bone structural parameters: bone volume/trabecular volume ratio (BV/TV), mean trabecular thickness (Th.mean), mean trabecular separation (Sp.mean), cortical thickness and cortical porosity. According to literature guidelines [23–25], the analysis was performed on a volume of 9.0 mm (120 slices) ending 9.5 mm proximal to the distal epiphysis border (Supplementary Fig. 1; more details on the methodology were provided in the supplemental material). A validation analysis was performed comparing HR-CBCT to micro-computed tomography (micro-CT) procedures [26]. Specifically, four specimens of trabecular bone with different trabecular content were prepared and scanned with both HR-CBCT and micro-CT (Skyscan model 1072 installed at Rizzoli Orthopaedic Institute, Bologna, Italy). A fixed threshold value was applied and a good correlation between HR-CBCT and micro-CT was observed for all trabecular parameters (Fig. 1) [22].
The assessment of VFs was performed with a morphometric X-ray absorptiometry method using images of the spine (T5-L4) acquired by DXA [27]. According to quantitative morphometric approach, the fractures were defined mild, moderate, and severe based on a height decrease of 20–25 %, 26–40 %, and more than 40 %, respectively [28].
BMD at the lumbar spine, total hip, femoral neck, and distal radius was measured in patients with acromegaly by DXA (Explorer Hologic Inc., Waltham, MA). Fractured vertebrae, assessed by the above reported method, were excluded from the lumbar BMD analysis. In patients aged 50 years or older, BMD was expressed as T-score, comparing the results with those obtained in a sex-matched Caucasian population at peak of bone mass [29]. A T-score less than or equal to −2.5 SD at the hip or spine was defined as osteoporosis, whereas osteopenia was defined as a T-score between −1 and −2.5 SD. In younger than 50 years patients, the results were expressed as Z-score, comparing the results with those obtained in an age and sex-matched Caucasian population [29]. A Z-score of −2.0 SD or lower was used to define a BMD “below the expected range for age” [29].
Patients were also evaluated for their body mass index (BMI: weight/height2).
Blood samples were collected after an overnight fast. GH and IGF-1 were measured by Immulite 2000 (DPC, Los Angeles, CA). For IGF-I, normal ranges were 116–358 ng/ml, 109–307 ng/ml, 94–267 ng/ml, 81–225 ng/ml, and 55–212 ng/ml for patients aged 21–30 years, 31–40 years, 41–50 years, 51–60 years, and 61–85 years, respectively.
Statistical analysis
All data were expressed as median and range. Un-paired data and frequencies were compared using Mann–Whitney and χ 2 tests, respectively. Spearman rank order correlation was performed to identify the determinants of CBCT parameters in patients with acromegaly. Statistical significance was assumed when p-values were equal or less than 0.05.
Results
DXA and morphometric analyses
In patients aged 50 years or older (26 cases), osteopenia and osteoporosis at any skeletal site were found in 8 (30.8 %) and 7 (26.9 %) patients, respectively. Only one acromegaly patient younger than 50 years (7.5 %) had BMD “below the expected range for age”. In the whole acromegaly group, 24 patients (60.0 %) had normal BMD at all skeletal sites. The prevalence of pathological BMD (i.e., osteoporosis or osteopenia or BMD “below the expected range for age”) was significantly higher in patients with untreated hypogonadism as compared to eugonadal patients (57.9% vs. 23.8 %; p = 0.03).
VFs were found in 15 patients (37.5 %). VFs were mild, moderate, and severe in 6, 8, and 1 patient, respectively, while multiple VFs occurred in 10 patients. Patients with VFs were older, had longer duration of active acromegaly and higher prevalence of untreated hypogonadism as compared to patients who did not fracture, without significant differences in sex, controlled/cured acromegaly, BMI, BMD at any skeletal site and prevalence of diabetes, persistent hypovitaminosis D, treated hypoadrenalism and hypothyroidism between the two groups (Table 1).
CBCT analyses
Representative HR-CBCT images and their qualitative differences between control subjects and acromegaly patients with and without VFs are shown in Fig. 2.
Quantitatively, patients with acromegaly showed at HR-CBCT lower BV/TV, smaller Th.mean, and greater Sp.mean, without significant differences in cortical thickness and porosity as compared to control subjects (Table 2). Acromegaly patients with VFs had significantly lower BV/TV (Fig. 3a), greater Sp.mean (Fig. 3b), and higher cortical porosity (Fig. 3c) as compared with non-fractured patients, without statistically significant differences in Th.mean (p = 0.25) and cortical thickness (p = 0.11). Statistical significance for trabecular parameters BV/TV and Sp.mean was verified over a wide of threshold values around the selected one (gray level 39).
In control group, males showed higher BV/TV (p = 0.02), greater Th.mean (p = 0.01) and lower Sp.mean (p = 0.03) as compared to females, without statistically significant differences in cortical thickness (p = 0.06) and porosity (p = 0.13). Moreover, either trabecular or cortical parameters did not correlate significantly with age of control subjects (data not shown).
In acromegaly, males showed greater Th.mean (p = 0.02) as compared to females, without significant differences in BV/TV (p = 0.11) and Sp.mean (p = 0.13). Moreover, trabecular parameters were associated with the age of patients (Table 3), since older patients had lower BV/TV and greater Sp.mean as compared to younger ones. Although no significant differences were found between active and controlled/cured acromegaly at the time of study entry (data not shown), trabecular parameters were significantly associated with duration of active disease (Table 3). In fact, longer duration of active acromegaly was associated with lower BV/TV and greater Sp.mean.
Acromegaly patients with untreated hypogonadism showed lower BV/TV (0.71 %, range: 0.35–0.94 vs. 0.87 %, range: 0.62–0.94; p = 0.005) and greater Sp.mean (0.41 mm, range 0.26–0.72 vs. 0.33 mm, range: 0.21–0.53; p = 0.004) as compared to eugonadal patients. Eugonadal patients did not show any significant differences in trabecular parameters as compared to control subjects (data not shown). However, eugonadal acromegaly patients were significantly younger as compared to patients with untreated hypogonadism (48 years, range: 25–72 vs. 62 years, range: 46–71; p = 0.001) and control subjects (48 years, range: 25–72 vs. 60 years, range: 25–68; p = 0.05).
Cortical thickness and porosity were significantly associated with age of patients (i.e., older patients had lower cortical thickness and higher porosity as compared to younger patients) (Table 3). Moreover, patients with untreated hypogonadism had higher porosity than eugonadal patients (0.35 %, range: 0.23–0.53 vs. 0.27 %, range: 0.15–0.52; p = 0.02). Furthermore, both cortical thickness and porosity were significantly associated with diabetes (Table 3), since lower cortical thickness (0.78 mm, range: 0.65–1.12 vs. 1.1 mm, range: 0.61–1.78; p = 0.004) and higher cortical porosity (0.47 %, range: 0.31–0.53 vs. 0.29 %, range: 0.15–0.53; p = 0.001) were found in acromegaly patients with diabetes as compared to those without diabetes. Finally, cortical thickness and porosity were significantly correlated with BMD as measured by DXA at distal radius (Table 3). No significant differences in cortical thickness (p = 0.28) and porosity (p = 0.54) were found between males and females in acromegaly.
Trabecular and cortical CBCT parameters were not significantly associated with treated hypoadrenalism and hypothyroidism (data not shown).
Discussion
In this cross-sectional study, acromegaly patients with VFs were found to have abnormal trabecular and cortical bone microstructure as compared to acromegaly patients who did not fracture.
In patients with various forms of secondary osteoporosis, bone strength and quality are compromised independently of bone density [30–32]. Moreover, trabecular and cortical bone respond differently to GH excess [4, 12, 13]. Consistently with previous reports [5], more than half of our acromegaly patients had normal BMD and only 20 % of them had either densitometric osteoporosis (>50 years) or BMD “below the expected range for age” (<50 years of age). Despite these reassuring densitometric findings, in the last decades high prevalence and incidence of VFs even in acromegaly patients with normal BMD were consistently reported [7–11].
Riggs and colleagues, more than 40 years ago, showed that acromegaly patients had increased bone width, increased cortical remodeling, and normal or increased cortical bone but decreased trabecular bone mass [33]. More recently, convincing evidence that bone microstructure may be compromised in acromegaly was reported [6, 12, 34]. Moreover, biomechanical competence and apparent density of trabecular framework were shown to be reduced in acromegaly patients evaluated by iliac crest biopsy [6]. Consistently, a recent clinical study with high-resolution peripheral computed tomography showed lower trabecular volume and greater trabecular separation in eugonadal patients with acromegaly as compared to control subjects [12]. However, so far no study has investigated the possible role of bone microarchitecture abnormalities in the determinism of fragility fractures in acromegaly. In this respect, the original methodological aspect in our study was that, for the first time, we analyzed bone microstructure in acromegaly using HR-CBCT, a multitask tomography technique characterized by low radiation dose and costs, reduced scanning time and 3D modalities in evaluating bone structure [16]. In fact, HR-CBCT has high isotropic resolution (i.e., voxel size 75 µm), with the ability to define independently trabecular and cortical microstructures [16], and has been recently proposed as a tool for the assessment of bone microstructure in patients with osteoporosis [16, 35]. Using this technique, we confirmed that acromegaly patients have a compromised trabecular bone framework and architecture (BV/TV, Sp.mean, Th.mean) as compared to control subjects [12]. The significant association between trabecular bone parameters and duration of active disease suggests that GH hypersecretion was the main determinant of bone trabecular abnormalities in acromegaly [34].
The main original finding of our study was the association between radiological VFs and bone microstructure abnormalities at distal radius in acromegaly. Specifically, HR-CBCT analysis showed that patients with VFs had decreased trabecular bone volume and greater trabecular separation in distal radius as compared to patients who did not fracture, consistently with the working hypothesis that VFs in acromegaly are caused by a specific and generalized deterioration of trabecular bone microarchitecture [6, 12, 34]. Interestingly, VFs were found to be associated also with higher cortical porosity. Although cortical porosity may have been underestimated by HR-CBCT, which could capture only pores larger than 150 µm, our results may suggest that even abnormalities in cortical structure may contribute to skeletal fragility in acromegaly [34, 36, 37]. In agreement with previous observations already performed in non-acromegaly patients [38, 39], in our study reduced cortical thickness and higher cortical porosity were shown to occur in older patients and in those with diabetes mellitus.
Some limitations of this study merit mention. The cross-sectional design did not allow to investigate the timing of VFs development and the value of HR-CBCT data in prospectively predicting the fracture risk in acromegaly patients. Hypogonadism has been reported to play a role in bone microstructure deterioration in acromegaly [12, 40]. In our study, both VFs and CBCT parameters were associated with age of patients, untreated hypogonadism and duration of active acromegaly, but the small size of study group did not allow us to investigate the independent impact of these factors on skeletal fragility. However, when the analysis was restricted to eugonadal subjects, the differences in HR-CBCT parameters between acromegaly patients and control subjects were lost possibly because the two groups were small and had significantly different ages. Using HR-CBCT, we were able to assess bone microstructure in the radius but not at the spine level where fractures occurred. However, the use of high-resolution quantitative computed tomography for the analysis of architecture of the vertebrae in vivo is limited by relatively high radiation dose and most studies have been so far performed at peripheral site, demonstrating that this approach may provide reliable information on skeletal fragility and fracture risk in different clinical settings [12, 25, 37–39, 41, 42]. The reliability and reproducibility of HR-CBCT results have been recently questioned due to the lack of clinically relevant parameter ranges and potentially high variability of trabecular bone measurements [43]. Specifically, BV/TV was shown to be the most consistent bone parameter evaluated by HR-CBCT, whereas high variability was already reported for the other trabecular parameters measured by this technique [43]. The highest achievable spatial resolution for HR-CBCT (around 150 μm) is lower than the one available with micro-CT—the standard for trabecular bone structure evaluation—which ranges between 7 and 35 μm [26, 44–46]. In fact, CBCT systematically overestimates trabecular thickness with respect to micro-CT [26] as confirmed by our validation analysis. This may explain why VFs in our acromegaly patients were associated with bone trabecular volume and separation but not with trabecular thickness. However, all these parameters were clearly different between acromegaly patients and control subjects supporting the concept that HR-CBCT may be reliable in evidencing impaired skeletal structure in acromegaly. On the other hand, this study did not provide information on the role of HR-CBCT in predicting VFs in non-acromegaly patients with osteoporosis, since our control group included healthy subjects in whom DXA evaluations were not performed. In our study, VFs were evaluated using DXA technique in order to reduce radiation exposure in patients with acromegaly. Although some underestimation of VFs has been reported with this technique especially when fractures were mild and involved upper thoracic vertebrae [47], the use of DXA assessment of VFs showed reasonable agreement with morphometry performed on standard X-ray [48] and was recommended as a viable alternative to conventional radiography to detect VFs in osteoporosis [29].
Besides the above mentioned limitations, the results of this study provide the first evidence that HR-CBCT at the distal radius may be an useful tool to evaluate and measure the deleterious effects of GH excess on trabecular and cortical bone microarchitecture predisposing to VFs in acromegaly patients. Based on these data, it is reasonable to hypothesize that in the next future HR-CBCT may replace DXA in stratifying the fracture risk of patients with acromegaly.
References
A. Giustina, M.D. Bronstein, F.F. Casanueva, P. Chanson, E. Ghigo, K.K. Ho, A. Klibanski, S. Lambert, P. Trainer, S. Melmed, Current management practices for acromegaly: an international survey. Pituitary 14, 125–133 (2011)
O.M. Dekkers, N.R. Biermasz, A.M. Pereira, J.A. Romijn, J.P. Vandenbroucke, Mortality in acromegaly: a metaanalysis. J. Clin. Endocrinol. Metab. 93, 61–67 (2008)
S. Melmed, F.F. Casanueva, A. Klibanski, M.D. Bronstein, P. Chanson, S.W. Lamberts, C.J. Strasburger, J.A. Wass, A. Giustina, A consensus on the diagnosis and treatment of acromegaly complications. Pituitary 16, 294–302 (2013)
A. Giustina, G. Mazziotti, E. Canalis, Growth hormone, insulin-like growth factors, and the skeleton. Endocr. Rev. 29, 535–559 (2008)
G. Mazziotti, E. Biagioli, F. Maffezzoni, M. Spinello, V. Serra, R. Maroldi, I. Floriani, A. Giustina, Bone turnover, bone mineral density, and fracture risk in acromegaly: a meta-analysis. J. Clin. Endocrinol. Metab. 100, 384–394 (2015)
T. Ueland, E.N. Ebbesen, J.S. Thomsen, L. Mosekilde, K. Brixen, A. Flyvbjerg, J. Bollerslev, Decreased trabecular bone biomechanical competence, apparent density, IGF-II and IGFBP-5 content in acromegaly. Eur. J. Clin. Invest. 32, 122–128 (2002)
S. Bonadonna, G. Mazziotti, M. Nuzzo, A. Bianchi, A. Fusco, L. De Marinis, A. Giustina, Increased prevalence of radiological spinal deformities in active acromegaly: a cross-sectional study in postmenopausal women. J. Bone Miner. Res. 20, 1837–1844 (2005)
G. Mazziotti, A. Bianchi, S. Bonadonna, V. Cimino, I. Patelli, A. Fusco, A. Pontecorvi, L. De Marinis, A. Giustina, Prevalence of vertebral fractures in men with acromegaly. J. Clin. Endocrinol. Metab. 93, 4649–4655 (2008)
M.J. Wassenaar, N.R. Biermasz, N.A. Hamdy, M.C. Zillikens, J.B. van Meurs, F. Rivadeneira, A. Hofman, A.G. Uitterlinden, M.P. Stokkel, F. Roelfsema, M. Kloppenburg, H.M. Kroon, J.A. Romijn, A.M. Pereira, High prevalence of vertebral fractures despite normal bone mineral density in patients with long-term controlled acromegaly. Eur. J. Endocrinol. 164, 475–483 (2011)
G. Mazziotti, A. Bianchi, T. Porcelli, M. Mormando, F. Maffezzoni, A. Cristiano, A. Giampietro, L. De Marinis, A. Giustina, Vertebral fractures in patients with acromegaly: a 3-year prospective study. J. Clin. Endocrinol. Metab. 98, 3402–3410 (2013)
K.M. Claessen, H.M. Kroon, A.M. Pereira, N.M. Appelman-Dijkstra, M.J. Verstegen, M. Kloppenburg, N.A. Hamdy, N.R. Biermasz, Progression of vertebral fractures despite long-term biochemical control of acromegaly: a prospective follow-up study. J. Clin. Endocrinol. Metab. 98, 4808–4815 (2013)
M. Madeira, L.V. Neto, F. de Paula Paranhos Neto, I.C. Barbosa Lima, L.M. Carvalho de Mendonça, M.R. Gadelha, M.L. Fleiuss de Farias, Acromegaly has a negative influence on trabecular bone, but not on cortical bone, as assessed by high-resolution peripheral quantitative computed tomography. J. Clin. Endocrinol. Metab. 98, 1734–41 (2013)
F. Jockenhövel, S. Rohrbach, S. Deggerich, D. Reinwein, C. Reiners, Differential presentation of cortical and trabecular peripheral bone mineral density in acromegaly. Eur. J. Med. Res. 1, 377–382 (2013)
J.F. Griffith, H.K. Genant, New advances in imaging osteoporosis and its complications. Endocrine 42, 39–51 (2012)
C. Battista, I. Chiodini, S. Muscarella, G. Guglielmi, M.L. Mascia, V. Carnevale, A. Scillitani, Spinal volumetric trabecular bone mass in acromegalic patients: a longitudinal study. Clin. Endocrinol. 70, 378–382 (2009)
J. Van Dessel, Y. Huang, M. Depypere, I. Rubira-Bullen, F. Maes, R. Jacobs, A comparative evaluation of cone beam CT and micro-CT on trabecular bone structures in the human mandible. Dentomaxillofacial Rad. 42, 20130145 (2013)
G. Mazziotti, E. Canalis, A. Giustina, Drug-induced osteoporosis: mechanisms and clinical implications. Am. J. Med. 123, 877–884 (2010)
A. Giustina, A. Barkan, F.F. Casanueva, F. Cavagnini, L. Frohman, K. Ho, J. Veldhuis, J. Wass, K. Von Werder, S. Melmed, Criteria for cure of acromegaly: a consensus statement. J. Clin. Endocrinol. Metab. 85, 526–529 (2000)
A. Giustina, A. Barkan, P. Chanson, A. Grossman, A. Hoffman, E. Ghigo, F. Casanueva, A. Colao, S. Lamberts, M. Sheppard, S. Melmed, Pituitary Society; European Neuroendocrine Association: guidelines for the treatment of growth hormone excess and growth hormone deficiency in adults. J. Endocrinol. Invest. 31, 820–838 (2008)
A. Giustina, P. Chanson, M.D. Bronstein, A. Klibanski, S. Lamberts, F.F. Casanueva, P. Trainer, E. Ghigo, K. Ho, S. Melmed, A consensus on criteria for cure of acromegaly. J. Clin. Endocrinol. Metab. 95, 3141–3148 (2010)
American Diabetes Association, Standard of medical care in diabetes. Diabetes Care 36, S11–S66 (2013)
M. Doube, M.M. Klosowski, I. Arganda-Carreras, F.P. Cordelières, R.P. Dougherty, J.S. Jackson, B. Schmid, J.R. Hutchinson, S.J. Shefelbine, BoneJ: Free and extensible bone image analysis in Image. J. Bone 47, 1076–1079 (2010)
R. Krug, A.J. Burghardt, S. Majumdar, T.M. Link, High-resolution imaging techniques for the assessment of osteoporosis. Radiol. Clin. North Am. 48, 601–621 (2010)
S. Boutroy, M.L. Bouxsein, F. Munoz, P.D. Delmas, In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J. Clin. Endocrinol. Metab. 90, 6508–6515 (2005)
E. Sornay-Rendu, S. Boutroy, F. Munoz, P.D. Delmas, Alterations of cortical and trabecular architecture are associated with fractures in postmenopausal women, partially independent of decreased BMD measured by DXA: The OFELY Study. J. Bone Miner. Res. 22, 425–433 (2007)
J.T. Ho, J. Wu, H.L. Huang, M.Y.C. Chen, L.J. Fuh, J.T. Hsu, Trabecular bone structural parameters evaluated using dental cone-beam computed tomography: cellular synthetic bones. BioMed. Eng. OnLine. 12, 115 (2013)
T. Fuerst, C. Wu, H.K. Genant, G. von Ingersleben, Y. Chen, C. Johnston, M.J. Econs, N. Binkley, T.J. Vokes, G. Crans, B.H. Mitlak, Evaluation of vertebral fracture assessment by dual X-ray absorptiometry in a multicenter setting. Osteopor. Int. 20, 1199–1205 (2009)
H.K. Genant, M. Jergas, L. Palermo, M. Nevitt, R.S. Valentin, D. Black, S.R. Cummings, Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis. The Study of Osteoporotic Fractures Research Group. J. Bone Min. Res. 11, 984–996 (1996)
J.T. Schousboe, J.A. Shepherd, J.P. Bilezikian, S. Baim, Executive summary of the 2013 International Society for Clinical Densitometry position development conference on bone densitometry. J. Clin. Densitom. 16, 455–466 (2013)
G. Mazziotti, J. Bilezikian, E. Canalis, D. Cocchi, A. Giustina, New understanding and treatments for osteoporosis. Endocrine 41, 58–69 (2012)
F.M. Ulivieri, B.C. Silva, F. Sardanelli, D. Hans, J.P. Bilezikian, R. Caudarella, Utility of the trabecular bone score (TBS) in secondary osteoporosis. Endocrine 47, 435–448 (2014)
G. Mazziotti, M. Doga, S. Frara, F. Maffezzoni, T. Porcelli, L. Cerri, R. Maroldi, A. Giustina, Incidence of morphometric vertebral fractures in adult patients with growth hormone deficiency. Endocrine 52, 103–110 (2016)
L. Riggs, R.V. Randall, H.W. Wanner, J. Jowsey, P.J. Kelly, M. Singh, The nature of metabolic bone disorder in acromegaly. J. Clin. Endocrinol. Metab. 34, 911–918 (1972)
S.V. Lim, M. Marenzana, M. Hopkinson, E.O. List, J.J. Kopchick, M. Pereira, B. Javaheri, J.P. Roux, P. Chavassieux, M. Korbonits, C. Chenu, Excessive growth hormone expression in male GH transgenic mice adversely alters bone architecture and mechanical strength. Endocrinology 156, 1362–1371 (2015)
K.J. Koh, K.A. Kim, Utility of the computed tomography indices on cone beam computed tomography images in the diagnosis of osteoporosis in women. Imag. Sci. Dent. 41, 101–106 (2015)
Y.N. Yeni, C.U. Brown, Z. Wang, T.L. Norman, The influence of bone morphology on fracture toughness of the human femur and tibia. Bone 21, 453–459 (1997)
R. Voide, P. Schneider, M. Stauber, P. Wyss, M. Stampanoni, U. Sennhauser, G.H. van Lenthe, R. Müller, Time-lapsed assessment of microcrack initiation and propagation in murine cortical bone at submicrometer resolution. Bone 45, 164–173 (2009)
K.M. Nicks, S. Amin, E.J. Atkinson, B.L. Riggs, L.J. Melton 3rd, S. Khosla, Relationship of age to bone microstructure independent of areal bone mineral density. J. Bone Min. Res. 27, 637–644 (2012)
A.J. Burghardt, A.S. Issever, A.V. Schwartz, K.A. Davis, U. Masharani, S. Majumdar, T.M. Link, High-resolution peripheral quantitative computed tomographic imaging of cortical and trabecular bone microarchitecture in patients with type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 95, 5045–5055 (2010)
A.R. Hong, J.H. Kim, S.W. Kim, S.Y. Kim, C.S. Shin, Trabecular bone score as a skeletal fragility index in acromegaly patients. Osteoporos. Int. 27, 1123–1129 (2016)
L. Vico, M. Zouch, A. Amirouche, D. Frère, N. Laroche, B. Koller, A. Laib, T. Thomas, C. Alexandre, High-resolution pQCT analysis at the distal radius and tibia discriminates patients with recent wrist and femoral neck fractures. J. Bone Miner. Res. 23, 1741–1750 (2008)
N. Dalzell, S. Kaptoge, N. Morris, A. Berthier, B. Koller, L. Braak, B. van Rietbergen, J. Reeve, Bone micro-architecture and determinants of strength in the radius and tibia: age-related changes in a population-based study of normal adults measured with high-resolution pQCT. Osteopor. Int. 20, 1683–1694 (2009)
S. Panmekiate, N. Ngonphloy, T. Charoenkarn, T. Faruangsaeng, R. Pauwels, Comparison of mandibular bone microarchitecture between micro-CT and CBCT images. Dentomaxillofac Rad. 44, 20140322 (2015)
H.L. Huang, J.T. Hsu, M.Y.C. Chen, C. Liu, C.H. Chang, Y.F. Li, K.T. Chen, Microcomputed tomography analysis of particular autogenous bone graft in sinus augmentation at 5 months: differences on bone mineral density and 3D trabecular structure. Clin. Oral Invest. 17, 535–542 (2013)
C.M. Bagi, E. Berryman, M.R. Moalli, Comparative bone anatomy of commonly used laboratory animals: implications for drug discovery. Comp. Med. 61, 76–85 (2011)
R. González-García, F. Monje, Is micro-computed tomography reliable to determine the microstructure of the maxillary alveolar bone?. Clin. Oral Impl. Res. 24, 730–737 (2013)
J.A. Rea, J. Li, G.M. Blake, P. Steiger, H.K. Genant, I. Fogelman, Visual assessment of vertebral deformity by X-ray absorptiometry: a highly predictive method to exclude vertebral deformity. Osteoporos. Int. 11, 660–668 (2000)
H. Hoyer-Kuhn, K. Knoop, O. Semler, K. Kuhr, M. Hellmich, E. Schoenau, F. Koerber, Comparison of DXA scans and conventional X-rays for spine morphometry and bone age determination in children. J. Clin. Densitom. 19, 208–215 (2016)
Funding
This study was partially supported by GIOSEG, University of Brescia and MIUR.
Author Contributions
F.M., M.Ma., G.M., R.M., and A.G. designed the study, did the analyses, interpreted the findings, and wrote and revised the report. S.F., M.Me., I.Z., and F.D. contributed to data collection and data preparation. F.B. contributed to technical support. All authors contributed to critical reading and revision of the draft report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
G.M. received consultant fees from Novartis Farma and Ipsen and received lecture fee from Ipsen A.G. is a consultant for Ipsen, Novartis, and Pfizer. F.M., M.M., S.F., M.M., I.Z., F.B., F.D., and R.M. have nothing to disclose.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Maffezzoni, F., Maddalo, M., Frara, S. et al. High-resolution-cone beam tomography analysis of bone microarchitecture in patients with acromegaly and radiological vertebral fractures. Endocrine 54, 532–542 (2016). https://doi.org/10.1007/s12020-016-1078-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-1078-3