Abstract
Purpose
to assess bone damage and metabolic abnormalities in patients with Addison’s disease given replacement doses of glucocorticoids and mineralocorticoids.
Methods
A total of 87 patients and 81 age-matched and sex-matched healthy controls were studied. The following parameters were measured: urinary cortisol, serum calcium, phosphorus, creatinine, 24-h urinary calcium excretion, bone alkaline phosphatase, parathyroid hormone, serum CrossLaps, 25 hydroxyvitamin D, and 1,25 dihydroxyvitamin D. Clear vertebral images were obtained with dual-energy X-ray absorptiometry in 61 Addison’s disease patients and 47 controls and assessed using Genant’s classification.
Results
Nineteen Addison’s disease patients (31.1%) had at least one morphometric vertebral fracture, as opposed to six controls (12.8%, odds ratio 3.09, 95% confidence interval 1.12–8.52). There were no significant differences in bone mineral density parameters at any site between patients and controls. In Addison’s disease patients, there was a positive correlation between urinary cortisol and urinary calcium excretion. Patients with fractures had a longer history of disease than those without fractures. Patients taking fludrocortisone had a higher bone mineral density than untreated patients at all sites except the lumbar spine.
Conclusions
Addison’s disease patients have more fragile bones irrespective of any decrease in bone mineral density. Supra-physiological doses of glucocorticoids and longer-standing disease (with a consequently higher glucocorticoid intake) might be the main causes behind patients’ increased bone fragility. Associated mineralocorticoid treatment seems to have a protective effect on bone mineral density.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adrenal insufficiency, or Addison’s disease (AD), is due to an adrenal hypofunction or dysfunction (primary adrenal insufficiency), or to a deficiency in hypothalamic corticotropin-releasing hormone or pituitary adrenocorticotropic hormone (ACTH) (secondary adrenal insufficiency) [1,2,3,4]. Autoimmune AD is the most common form of primary hypoadrenalism in the white adult population of developed countries, accounting for about 80–90% of all forms of AD [2, 4]. The condition can occur alone or in association with other autoimmune diseases, in various combinations that are classified as autoimmune polyendocrine syndromes (APS-1, APS-2, and APS-4) [5,6,7,8,9,10,11,12].
Treatment for AD consists of two or three daily oral doses of the specific hormones that patients lack. The daily dose distribution is intended to mimic the physiological circadian rhythm of cortisol secretion, but it has its drawbacks in that it induces serum cortisol peaks beyond physiological levels, and it does not reflect the normal rise in serum cortisol levels after the nadir occurring during the night. This impairs patients’ quality of life due to their temporary underdosing or overdosing, and long-term overdosing can cause weight gain, glucose intolerance, and abnormal bone metabolism, leading to osteoporosis [13,14,15,16].
It is well known that glucocorticoids (GC) have a negative effect on bone, both directly by increasing bone resorption and inhibiting bone formation, and indirectly by inhibiting vitamin D-dependent intestinal calcium absorption and increasing renal calcium excretion. In primary adrenal insufficiency, the lack of adrenal androgens is an additional factor that carries a risk of osteoporosis [17]. Although the bone damage associated with the therapeutic use of GC has long been known, the effect of GC given as a replacement therapy is less clear and rarely studied [18,19,20,21,22,23]. Data on bone mineral density (BMD) and on the incidence and prevalence of fragility fractures in primary adrenal insufficiency are scanty and controversial. The potential impact of different therapeutic regimens on fracture risk in primary adrenal insufficiency is also still unclear. Over-replacement therapy for secondary adrenal insufficiency is known to be associated with high prevalence of radiologically-evident vertebral fractures [24], providing the rationale for addressing the same issue in patients with primary adrenal insufficiency. The aim of our study was therefore to assess bone damage—in terms of BMD and prevalence of vertebral fractures—in patients with primary adrenal insufficiency treated with replacement doses of GC. Our cases were also compared with a normal control group.
Materials and methods
Patients
Our sample consisted of 87 patients with primary autoimmune AD on GC replacement therapy referring to the Endocrinology Unit at the University Hospital in Padua. The female/male ratio was 59/28. The patients ranged in age from 20 to 77 years (median: 44 years). Twenty-five women aged from 26 to 77 years (median: 55 years) had been postmenopausal for 1–47 years (median: 13 years), and their age at menopause ranged from 16 to 53 years (median: 45 years). Seven patients developed early menopause (at 40-year-old or younger) due to premature ovarian failure. The patients in the sample had a history of AD spanning from 0.5 to 55 years (median: 9 years). Seventy-three patients were being treated with cortisone acetate, one with dexamethasone, and 13 with hydrocortisone. Twenty-four patients had AD alone, nine had APS-1, and 54 had APS-2. The control group consisted of 81 healthy subjects, matched for sex and age, recruited from the medical and technical staff at our department and from subjects without any chronic diseases or concomitant use of drugs interfering with bone metabolism, who underwent dual-energy X-ray absorptiometry (DXA) as part of a check-up. The group ranged from 23 to 78 years of age (median: 45 years), and the female/male ratio was 58/23. Twenty-three women aged from 49 to 78 years (median: 56 years) had been postmenopausal for 1–27 years (median: 3 years), and their age at menopause ranged from 43 to 59 years (median: 51 years).
Sixty-six AD patients (16 males and 50 females) had one or more comorbidities.
The various doses of GC being used were standardized by converting them into equivalent doses of hydrocortisone adopting the following ratios: 30 mg hydrocortisone = 0.75 mg dexamethasone = 37.5 mg cortisone acetate. GC replacement therapy was expressed in terms of the daily dose (mg/day), daily dose by body weight (mg/kg), daily dose by body surface area (mg/m2), and cumulative dose (g). Body surface area was calculated using the Mosteller method, (height in cm × weight in kg/3600)½ [25]. Seventy-five patients were taking fludrocortisone acetate (FCA) and 12 were not. Twenty-nine patients were given cholecalciferol 1000–2000 IU/day; patients with APS-1 were also given calcitriol 0.5–3 µg/day. Among the postmenopausal AD patients, 15 out of 25 had experienced early menopause (≤40 years of age), and six of them had used hormone replacement therapy. None of the male AD patients had hypogonadism.
All procedures performed in this study complied with the ethical standards of our institutional research committee, and with the 1964 Helsinki Declaration and its subsequent amendments. All participants gave their informed consent to the study and to the use of their personal data.
Bone mineral density and vertebral fracture assessment
BMD at the lumbar spine (L1–L4) and proximal femur, and body composition (particularly the amount of adipose tissue) were evaluated with DXA in all patients and healthy controls using a Hologic Delphi device (Hologic Inc, Bedford, MA, USA). The in vitro coefficient of variation, measured by analyzing an anthropomorphic phantom reproducing the lumbar vertebrae (provided by the manufacturer) ten times, was 0.6%. In vivo reproducibility was measured by obtaining five scans in 1 week in ten healthy volunteers: the coefficient of variation [CV] was 1.2% for the lumbar spine, 2.1% for the whole femur, and 1.8% for the femoral neck.
The morphometric study to identify any vertebral deformities according to Genant’s classification [26] was performed in all subjects, but clear images were only obtained for 61 AD patients (18 men, 27 premenopausal and 16 postmenopausal women), and for 47 healthy controls (11 men, 23 premenopausal and 13 postmenopausal women).
The morphometric analysis was performed using the specific densitometer software. The subject was positioned in the right lateral decubitus and the pointing laser was placed just above the left iliac crest. During the scan, patients were asked to hold their breath at the point of maximum inspiration. In all patients and controls, the height of the vertebrae was measured on the D5-L4 segment, excluding Schmorl nodes and osteophytes from the overall vertebral height measurement. Any wedge and biconcave vertebral deformities were calculated from the ratio of the mid- or anterior height to the posterior height. Crush deformities were calculated from the ratio between the three heights of the deformed vertebra and those of the adjacent vertebrae. The vertebral heights were measured on the vertebrae with an evidently deformed morphology, as judged by two independent operators, and only the vertebrae judged to be deformed by both examiners were taken into account. In accordance with Genant’s classification, we considered deformities with a 20–25% reduction in the central or anterior height vis-à-vis the posterior height of the same vertebra as mild, reductions of 26–40% as moderate, and reductions >40% as severe.
Biochemical tests
Fasting blood samples were collected at 8.00 a.m. (AD patients had only taken their therapy at least 1 h beforehand); and a 24-h urine collection was provided at the same time. The following parameters were measured: urinary cortisol, serum calcium (Ca), phosphorus (P), creatinine (Cr), 24-h urinary calcium excretion (uCa), bone alkaline phosphatase (bALP), parathyroid hormone (PTH), serum CrossLaps (CTx), 25 hydroxyvitamin D (25OHD), and 1,25 dihydroxyvitamin D (1,25[OH]2D).
Serum Ca, P, Cr and bALP were measured by means of a colorimetric assay using common automated laboratory methods on a Cobas 8000 instrument (Roche Diagnostics). Serum CTx were assayed by enzyme immunoassay using Serum CrossLaps ELISA® (Nordic Bioscience Diagnostics). Serum PTH was measured with the LIAISON® N-tact TMPTH kit that exploits the chemiluminescence technology in an immunoassay for the quantitative measurement of intact human PTH in the serum (the detection limit [DL] is 10 pg/mL; and the inter-assay and intra-assay coefficients of variation (CV) are 4 and 3.5%, respectively). Serum 25OHD concentrations were measured with the direct competitive method using a chemiluminescence immunoassay (DiaSorin, Italy) automated on the LIAISON XL instrument (DL: 1.5 nmol/L; inter-assay and intra-assay CV: 9%). Serum 1,25(OH)2D was measured with the 1,25[OH]2D IDS RIA® kit (DL: 5 pmol/L; inter-assay and intra-assay CV: 8.6–16.6% and 11.9–20%, respectively). Urinary cortisol was tested by radioimmunoassay using the commercial cortisol BRIDGE kit (Adaltis, Rome, Italy).
Statistical analysis
Results are presented as counts and percentages in the case of categorical variables, and as median and range (minimum and maximum values) for quantitative variables. Normality of the quantitative variables was checked graphically with quantile–quantile plots and with the Shapiro Wilk test.
AD patients versus controls, and AD patients with versus without fractures were compared with the Χ 2 test in the case of categorical variables, and with non-parametric Mann–Whitney test in the case of quantitative variables. Data were entered in an EXCEL spreadsheet and analyzed with GraphPad Prism version 5.00 for Windows, GraphPad Software, San Diego California USA (www.graphpad.com). Significance was set at a p value ≤ 0.5.
Results
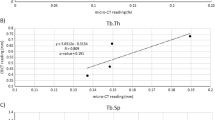
All the data collected for the AD patients and healthy controls are summarized in Table 1. Age at menopause was significantly lower in the AD group (median; min–max: 45; 16–53 years) than in the control group (51; 43–59 years) (p < 0.0001), so the years since menopause were significantly higher in the former (13; 1–47 years) than in the latter (3; 1–27 years) (p = 0.0032). There were no significant differences between patients and controls in any of the DXA parameters. Urinary cortisol concentrations were higher in AD patients (309; 6–1380 nmol/24 h) than in controls (254; 23–744 nmol/24 h), but the difference was not statistically significant. AD patients had lower 24-h urinary Ca excretion levels (3.04; 0.52–17.10 mmol/24 h) than controls (4.6; 1.43–11.85 mmol/24 h) (p = 0.0031). There were no significant differences between the two groups as regards serum Ca, P, bALP, CTx, 25OHD, and PTH. No significant correlations emerged in the AD patients between duration of disease and urinary cortisol, and the various densitometric and laboratory parameters. Finally, AD patients showed a significant positive correlation between urinary cortisol and urinary Ca excretion (Fig. 1).
The majority of patients were taking FCA. BMD was significantly higher in FCA-treated patients at all sites except for the lumbar spine. In contrast, there was no difference in any of the demographic, anthropometric or laboratory parameters between the patients who were or were not taking FCA. The GC doses and duration of disease were also similar in these two groups (Table 2).
Patients with comorbidities had a lower age at menopause, body weight and BMI than patients without comorbidities, but there were no differences between these two groups in terms of their DXA parameters (Table 3).
Our series was tested for the potential skeletal impact of different GC formulations. Seventy-three AD patients were given cortisone acetate while 13 took hydrocortisone. The patients treated with cortisone acetate were older (45; 20–77 years) than those given hydrocortisone (32; 21–56 years) (p = 0.016). The former also received a higher cumulative dose (137; 6–753 g vs 61.6; 3.6–370 g of hydrocortisone equivalent) (p = 0.048). No significant differences were found between the two groups’ BMD values at any site.
Vertebral assessment
Ten AD patients and 6 healthy controls had a history of traumatic fractures. Nineteen AD patients (31.2%; 6 males, 8 premenopausal and 5 postmenopausal women) revealed at least one morphometric vertebral fracture: 4 had two, and 1 had three. Fifteen fractures were mild according to Genant’s classification, 6 were moderate, and 3 were severe. Eighteen fractures were in the thoracic spine and 6 in the lumbar spine. Two patients (51 and 77 year-old) who had experienced early menopause had morphometric vertebral fractures. In the control group, 6 subjects (12.8%; 1 male, 5 post-menopausal women) revealed at least one morphometric vertebral fracture: 5 had a single fracture, 1 had two. Six fractures were classified as mild, and 1 as moderate (there were no severe fractures). Five fractures were in the thoracic spine, and 2 in the lumbar spine. The difference between the cases of fracture in the AD patient versus control group was statistically significant (p = 0.025), with an odds ratio (OR) of 3.09 (95% confidence interval [CI]: 1.12–8.52).
Among the 19 AD patients revealing vertebral fractures, 16 were taking FCA and 3 were not. Among the AD patients without vertebral fractures, 35 were taking FCA and 8 were not (OR 1.22; 95% CI: 0.285–5.211; p = 0.789).
Among the AD patients who underwent vertebral morphometry, 44 had one or more comorbidities, and 12 of them (5 males and 7 females) had at least one vertebral fracture, while 32 (12 males and 20 females) did not. The other 17 patients who underwent vertebral morphometry had no comorbidities, and 7 of them (3 males and 4 females) revealed vertebral fractures, while 10 (5 males and 5 females) did not. There was no significant difference in morphometric vertebral fracture rate between the AD patients with and without comorbidities (OR 0.97; 95% CI: 0.41–2.31; p = 0.946).
In our sample, 11 of the 13 AD patients with early menopause underwent vertebral morphometry, and 3 of them revealed vertebral fractures. Our sample included 7 patients with type I diabetes (4 males and 3 females, aged from 23 to 54 years): 4 of them underwent vertebral morphometry and none had vertebral fractures. There were 5 patients with type II diabetes (1 male and 4 females, aged from 21 to 73 years), 3 of them underwent vertebral morphometry, and 2 revealed vertebral fractures (one 45-year-old male, and one 73-year-old female). When patients with early menopause and/or diabetes of either type were considered together in the group that underwent vertebral morphometry, no differences emerged in terms of the vertebral fracture rate between patients with and without these comorbidities (OR 1.006; 95% CI: 0.294–3.448; p = 0.992).
Patients who revealed vertebral fractures had a longer history of AD (12; 2–55 years) than those who did not (7; 0.5–30 years) (p = 0.018). GC doses and the anthropometric and laboratory parameters considered here identified no other significant differences between these two groups (Table 4).
Discussion
The most relevant finding emerging from this study concerns the morphometric assessment used to identify vertebral deformities in AD patients according to Genant’s method.
The value of assessing vertebral fractures using DXA has now been validated by several studies. The method correctly identified 94% of moderate and severe fractures, and 96% of vertebrae without fractures [27,28,29]. The drawback of the method lies in that the vertebrae above T7 are difficult to read. On the other hand, atraumatic fractures occurring in the first stretch of the thoracic spine are known to account for less than 5% of all prevalent vertebral fractures [30].
In our sample, the risk of morphometric vertebral fractures was found to be three times higher in AD patients than in a healthy control population. Most of the studies that examined the effect of GC replacement therapy on bone status in AD patients did not check for the presence of vertebral fractures. In a cross-sectional study involving 292 patients from Norway, the UK and New Zealand, Lovas et al. found no difference in the prevalence of vertebral fractures by comparison with those reported in a Norwegian reference population, despite a significant reduction in vertebral and femoral BMD in the AD patients [31]. Björnsdóttir et al. conducted a large study on 3,219 Swedish AD patients compared with 31,557 sex-matched and age-matched controls, finding an increase in the prevalence of hip fractures in the AD patients (6.9 vs. 2.7%), who carried a significantly higher fracture risk (hazard ratio: 1.8; 95% CI: 1.6–2.1; p < 0.001) [32]. Koetz et al. found vertebral fractures in 6.9% of female and 3.6% of male AD patients; fractures (of any type) occurred in 32.5% of the females and 11.8% of the males beyond the age of 50 years. No comparison was drawn with a normal population, but postmenopausal female patients had a higher fracture risk than premenopausal women or men [22]. In the present study, spinal morphometry in our AD and healthy control groups identified significantly more AD patients with morphometric vertebral fractures than controls, and the fracture risk was three times higher in the former. The M/F ratio in the populations with and without vertebral fractures was much the same in the AD and control groups. When females were considered alone, however, none of the premenopausal women in the control group had fractures, whereas 7 of the 13 premenopausal AD patients had fractures. This finding suggests a major role for GC replacement therapy—rather than estrogen deficiency—in the genesis of atraumatic vertebral fractures in AD patients.
The higher fracture risk is not related to a reduction in BMD at any site. The effect of GC replacement therapy on BMD has been examined in several studies, generating different results [33,34,35,36,37,38,39,40,41]. These conflicting results might be due to differences in the etiology of hypoadrenalism: in almost all studies, patients with autoimmune disease, pituitary insufficiency, and surgical adrenalectomy were considered together, and very few studies had a control group.
Our sample only included AD patients with an autoimmune etiology, and that is why many of the women with AD had been considerably younger at menopause than those in the control group. In terms of hydrocortisone equivalents, the daily dose of GCs administered to our sample was 0.5 ± 0.15 mg/kg (and 18.69 ± 5 mg/m2 of body surface area), which was higher than the doses mentioned in other studies [31, 38,39,40]. On the other hand, the urinary cortisol excretion levels measured in our AD patients (which reflects the dose of GC they took) did not differ significantly from those of controls. We surmise that the slightly higher urinary cortisol excretion levels identified in our cases may be the consequence of two or three peaks in circulating cortisol, rather than a true overdose of GC. This impression seems to be confirmed by the fact that all the patients evaluated had a normal blood pressure, normal laboratory parameters (including Na, K, and glucose), and a normal BMI. ACTH was not considered because its plasma levels fluctuate considerably due to the pulsatile secretion of this hormone. In an open cross-sectional study on men with severe ACTH deficiency, Behan et al. found that the lower dose of hydrocortisone replacement that they used was actually associated with an increased bone formation and a positive bone remodeling balance [41]. Schulz et al. were the first to demonstrate that reducing the daily hydrocortisone equivalent dose from 30.8 ± 8.5 to 21.4 ± 7.2 mg led to an increase in BMD with no associated increase in the risk of adrenal crisis, whereas incremental doses lowered patients’ BMD [42]. Although our patients received slightly higher GC replacement doses than elsewhere in the literature, we found no difference in BMD between patients and controls. There were also no significant differences in our data relating to mineral metabolism and bone turnover, apart from uCa excretion, which was significantly lower in AD patients. GC excess is believed to raise uCa excretion levels by reducing renal tubular calcium reabsorption [43]. Consistently with this assumption, we found a positive correlation between urinary calcium and urinary cortisol in AD patients. In our study, however, AD patients had lower daily renal Ca excretion levels than controls. Their reduced uCa excretion may be partly due to their associated mineralcorticoid (MC) treatment. Few studies are available on the effect of these hormones on calcium excretion, and most of them were conducted in experimental animals. While one study on seven healthy men [44] identified a reduced uCa excretion in the early stage of MC treatment, many other experimental and clinical studies found that MCs induced a clear increase in uCa excretion [45,46,47,48,49]. In our sample, we found no difference between patients who were treated with FCA and those who were not. These discrepancies might therefore suggest that any decline in uCa excretion is a consequence of a metabolic disorder rather than a direct effect of corticosteroid therapy on the kidney.
Surprisingly, our patients treated with FCA had significantly higher densitometric values at all sites except for the lumbar spine. This would indicate that the beneficial effect of FCA, if any, is more evident on cortical than on trabecular bone. To our knowledge, this is the first study to demonstrate a difference in BMD between AD patients treated or not treated with FCA. It is well known that there are GC receptors (GRα and GRβ) and mineralocorticoid receptors (MR) in the cells of osteoblast and osteoclast lineage. Glucocorticoid receptors occur in trabecular and cortical osteoblasts, in the osteocytes newly incorporated in mineralizing osteoid, and in the lining cells of osteons in cortical bone. GRβ may modulate the response of osteoblasts to GC by heterodimerizing with GRα and antagonizing its transcriptional activity. This would explain why osteoblasts respond differently to low or high concentrations of GC: physiological concentrations increase osteoblast differentiation and collagen synthesis, while higher concentrations inhibit osteoblastogenesis and increase osteoblast apoptosis [50,51,52,53]. Osteoclasts mainly, if not exclusively, express GRβ, and GC can stimulate bone resorption either directly or by increasing the synthesis of receptor activator NF-kB ligand by osteoblasts [54, 55]. MR are expressed in osteoblasts and osteoclasts, but their function is not clearly understood. The pharmacological inhibition of MR with eplerenone results in an increasing bone mass, the suppression of bone resorption, and an increase in cortical thickness. Aldosterone significantly enhances the proliferation of osteoblastic cells from rat calvarias, and inhibits the activity of alkaline phosphatase, which is a marker of the osteoblastic phenotype [56, 57]. The simultaneous presence of MR, GRα and GRβ in bone cells suggests that these receptors may act in synergy, and influence the activity of osteoblasts and osteoclasts in different ways, depending on their concentrations. Given the small number of patients not treated with FCA in our sample, and the novelty of our finding, we cannot speculate on these results, which will need to be confirmed in a larger population.
Björnsdóttir et al. [32] found that AD patients were at the highest risk of hip fractures in the first year before and the first year after their diagnosis. Their data correlated with low cortisol levels in the year before the diagnosis (responsible for a poor osteoblast differentiation), and supra-physiological doses after starting GC treatment (responsible for an greater osteoclastic activity induced by a pronounced increase in bone turnover). We cannot advance any hypotheses on the timing of the higher risk of vertebral fracture in our AD patients, though the longer history of disease among patients revealing spinal fractures suggests that a lengthier exposure to GC could have an important role in the genesis of vertebral fractures.
Supra-physiological doses of GC may not be the only culprit responsible for bone damage in AD patients. Another cause could be a shortage of adrenal androgens [17] since other studies identified a positive correlation between low BMD and low circulating levels of dehydroepiandrosterone (DHEA) in patients with hypopituitarism [58]. Koetz et al. reported that women treated with DHEA for this condition showed no spontaneous vertebral fractures, whereas fractures were identified in 9.8% of the untreated patients [22]. Although there was no difference in serum glucose levels between our AD patients and controls, we cannot exclude the possibility of long-term supra-physiological doses of GC causing an excessive glycosylation of collagen, which impairs the mechanical characteristics and disrupts the normal, regular deposition of hydroxyapatite crystals. Such alterations may lead to a loss of bone strength unrelated to the amount of mineral deposited or, ultimately, to BMD [59,60,61]. The fact that we found no difference in BMD between our patients with and without fractures is consistent with this hypothesis, which suggests that the increased risk of fractures in AD patients would be due to qualitative rather than quantitative bone damage.
We cannot exclude the possibility of adrenal insufficiency itself, (as well as its replacement therapy) causing functional growth hormone deficiency, which may be involved in the pathogenesis of skeletal fragility in this clinical setting [62].
Among the various comorbidities seen in AD patients, early menopause and diabetes are the most often associated with vertebral fractures [63,64,65]. Such comorbidities did not influence BMD or fracture risk of our patients: we assume that they had all received appropriate treatment.
Finally, bone impairment in various autoimmune diseases might also be seen as the consequence of an immunoregulatory imbalance altering homeostatic mechanisms, which would lead to an imbalanced osteoclast activity [66, 67].
In conclusion, AD patients on chronic mineralocorticoid and GC replacement therapy have a higher prevalence of vertebral fractures unrelated to any decrease in BMD. Supra-physiological doses of GC, a longer history of disease, and a consequently higher GC intake might be the main reasons why their bones become more fragile. We cannot exclude the possibility of other pathophysiological mechanisms related to adrenal insufficiency and autoimmune disease being involved in the genesis of AD patients’ fractures. The influence of FCA on bone metabolism warrants further investigation.
References
W. Arlt, B. Allolio, Adrenal insufficiency. Lancet 361, 1881–1893 (2003)
C. Betterle, L. Morlin, Autoimmune Addison’s disease. Endocrine. Development 20, 161–172 (2011)
M. Quinkler, F. Beuschlein, S. Hahner, G. Meyer, C. Schöfl, G.K. Stalla, Adrenal cortical insufficiency - a life threatening illness with multiple etiologies. Dtsch. Arztebl. Int. 110, 882–888 (2013)
M.M. Erichsen, K. Lovas, B. Skinningsrud, A.B. Wolff, D.E. Undlien, J. Svartberg, K.J. Fougner, T.J. Berg, J. Bollerslev, B. Mella, J.A. Carlson, H. Erlich, E.S. Husebye, Clinical, immunological, and genetic features of autoimmune primary adrenal insufficiency: observations from a Norwegian registry. J. Clin. Endocr. Metab. 94, 4882–4890 (2009)
C. Betterle, R. Scarpa, S. Garelli, L. Morlin, F. Lazzarotto, F. Presotto, G. Coco, S. Masiero, A. Parolo, M.P. Albergoni, R. Favero, S. Barollo, M. Salvà, D. Basso, S. Chen, B. Rees Smith, J. Furmaniak, F. Mantero, Addison’s disease: a survey on 633 patients in Padova. Eur. J. Endocrinol. 169, 773–784 (2013)
C. Betterle, C. Dal Pra, F. Mantero, R. Zanchetta, Autoimmune adrenal insufficiency and autoimmune polyendocrine syndromes: autoantibodies, autoantigens, and their applicability in diagnosis and disease prediction. Endocr. Rev. 23, 327–364 (2002)
G.S. Eisenbarth, P.A. Gottlieb, Autoimmune polyendocrine syndromes. New Engl. J. Med. 13, 2068–2079 (2004)
A. Soderbergh, O. Winqvist, I. Norheim, F. Rorsman, E.S. Husebye, O. Dolva, F.A. Karlsson, O. Kämpe, Adrenal autoantibodies and organ-specific autoimmunity in patients with Addison’s disease. Clin. Endocrinol. 45, 453–460 (1996)
M. Fichna, P. Fichna, M. Gryczynska, J. Walkowiak, M. Zurawek, J. Sowinski, Screening for associated autoimmune disorders in Polish patients with Addison’s disease. Endocrine 37, 349–360 (2010)
A. Soderbergh, A.G. Myhre, O. Ekwall, G. Gebre-Medhin, H. Hedstrand, E. Landgren, A. Miettinen, P. Eskelin, M. Halonen, T. Tuomi, J. Gustafsson, E.S. Husebye, J. Perheentupa, M. Gylling, M.P. Manns, F. Rorsman, O. Kämpe, T. Nilsson, Prevalence and clinical associations of 10 defined autoantibodies in autoimmune polyendocrine syndrome type I. J. Clin. Endocr. Metab. 89, 557–562 (2004)
E.S. Husebye, J. Perheentupa, R. Rautemaa, O. Kämpe, Clinical manifestations and management of patients with autoimmune polyendocrine syndrome type I. J. Intern. Med 265, 514–529 (2009)
Ø. Bruserud, B.E. Oftedal, A.B. Wolff, E.S. Husebye, AIRE-mutations and autoimmune disease. Curr. Opin. Immunol. 6, 8–15 (2016)
E.S. Husebye, B. Allolio, W. Arlt, K. Badenhoop, S. Bensing, C. Betterle, A. Falorni, E.H. Gan, A.L. Hulting, A. Kasperlik-Zaluska, O. Kämpe, K. Løvås, G. Meyer, S.H. Pearce, Consensus statement on the diagnosis, treatment and follow-up of patients with primary adrenal insufficiency. J. Intern. Med. 275, 104–115 (2014)
A. Grossman, G. Johannsson, M. Quinkler, P. Zelissen, Therapy of endocrine disease. Perspectives on the management of adrenal insufficiency: clinical insights from across Europe. Eur. J. Endocrinol. 21, R165–R175 (2013)
A. Falorni, V. Minarelli, S. Morelli, Therapy of adrenal insufficiency: an update. Endocrine 43, 514–528 (2013)
G. Johannsson, iA. Falorn, S. Skrtic, H. Lennernäs, M. Quinkler, J.P. Monson, P.M. Stewart, Adrenal insufficiency: review of clinical outcomes with current GC replacement therapy. Clin. Endocrinol. (Oxf.) 82, 2–11 (2015)
J.P. Devogelaer, J. Crabbé; Nagant de Deuxchaisnes, C, Bone mineral density in Addison’s disease: evidence for an effect of adrenal androgens on bone mass. Brit. Med. J. (Clin. Res Ed.) 294, 798–800 (1987)
P.M. Zelissen, R.J. Croughs, P.P. van Rijk, J.A. Raymakers, Effect of MC replacement therapy on bone mineral density in patients with Addison disease. Ann. Intern. Med. 120, 207–210 (1994)
M.A. Valero, M. Leon, M.P. Ruiz Valdepeñas, L. Larrodera, M.B. Lopez, K. Papapietro, A. Jara, F. Hawkins, Bone density and turnover in Addison’s disease: effect of glucocorticoid treatment. Bone Miner. 26, 9–17 (1994)
F. Heureux, D. Maiter, Y. Boutsen, J.P. Devogelaer, J. Jamart, J. Donckier, Evaluation of corticosteroid replacement therapy and its effect on bones in Addison’s disease. Ann. Endocrinol. (Paris) 61, 179–183 (2000)
E. Jódar, M.P. Valdepeñas, G. Martinez, A. Jara, F. Hawkins, Long-term follow-up of bone mineral density in Addison’s disease. Clin. Endocrinol. (Oxf.) 58, 617–620 (2003)
K.R. Koetz, M. Ventz, S. Diederich, M. Quinkler, Bone mineral density is not significantly reduced in adult patients on low-dose glucocorticoid replacement therapy. J. Clin. Endocr. Metab. 97, 85–92 (2012)
D.D. Chandy, E. Bhatia, Bone mineral density in patients with Addison disease on replacement therapy with prednisolone. Endocr. Pract. 22, 434–439 (2016)
G. Mazziotti, T. Porcelli, A. Bianchi, V. Cimino, I. Patelli, C. Mejia, A. Fusco, A. Giampietro, L. De Marinis, A. Giustina, Glucocorticoid replacement therapy and vertebral fractures in hypopituitary adult males with GH deficiency. Eur. J. Endocrinol. 163, 15–20 (2010)
R.D. Mosteller, Simplified calculation of body surface area. N. Engl. J. Med. 317, 1098 (1987)
H.K. Genant, M. Jergas, L. Palermo, M. Nevitt, R.S. Valentin, D. Black, S.R. Cummings, Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis. The study of osteoporotic fractures research group. J. Bone Miner. Res. 11, 984–996 (1996)
N. Binkley, D. Krueger, R. Gangnon, H.K. Genant, M.K. Drezner, Lateral vertebral assessment: a valuable technique to detect clinically significant vertebral fractures. Osteoporos. Int. 16, 1513–8 (2005)
I.C. Hospers, J.G. van der Laan, C.J. Zeebregts, P. Nieboer, B.H. Wolffenbuttel, R.A. Dierckx, H.G. Kreeftenberg, P.L. Jager, R.H. Slart, Vertebral fracture assessment in supine position: comparison by using conventional semiquantitative radiography and visual radiography. Radiology 251, 822–828 (2009)
T. Fuerst, C. Wu, H.K. Genant, G. von Ingersleben, Y. Chen, C. Johnston, M.J. Econs, N. Binkley, T.J. Vokes, G. Crans, B.H. Mitlak, Evaluation of vertebral fracture assessment by dual X-ray absorptiometry in a multicenter setting. Osteoporos. Int. 20, 1199–1205 (2009)
P.L. Jager, S. Jonkman, W. Koolhaas, A. Stiekema, B.H. Wolffenbuttel, R.H. Slart, Combined vertebral fracture assessment and bone mineral density measurement: a new standard in the diagnosis of osteoporosis in academic populations. Osteoporos. Int. 22, 1059–1068 (2011)
K. Løvås, C.G. Gjesdal, M. Christensen, A.B. Wolff, B. Almås, J. Svartberg, K.J. Fougner, U. Syversen, J. Bollerslev, J.A. Falch, P.J. Hunt, V.K. Chatterjee, E.S. Husebye, Glucocorticoid replacement therapy and pharmacogenetics in Addison’s disease: effects on bone. Eur. J. Endocrinol. 160, 993–1002 (2009)
S. Björnsdottir, M. Sääf, S. Bensing, O. Kämpe, K. Michaëlsson, J.F. Ludvigsson, Risk of hip fracture in Addison’s disease: a population-based cohort study. J. Intern. Med 270, 187–195 (2011)
F. Heureux, D. Maiter, Y. Boutsen, J.P. Devogelaer, Jamar,t J., Donckier J.: evaluation of corticosteroid replacement therapy and its effect on bones in Addison’s disease. Ann. Endocrinol. (Paris) 61, 179–183 (2000)
E. Jódar, M.P. Valdepeñas, G. Martinez, A. Jara, F. Hawkins, Long-term follow-up of bone mineral density in Addison’s disease. Clin. Endocrinol. (Oxf.) 58, 617–620 (2003)
G.D. Braatvedt, M. Joyce, M. Evans, J. Clearwater, I.R. Reid, Bone mineral density in patients with treated Addison’s disease. Osteoporos. Int 10, 435–440 (1999)
C.M. Florkowski, S.J. Holmes, J.R. Elliot, R.A. Donald, E.A. Espiner, Bone mineral density is reduced in female but not male subjects with Addison’s disease. N. Z. Med. J. 107, 52–53 (1994)
D.D. Chandy, E. Bhatia, Bone mineral density in patients with Addison’s disease on replacement therapy with prednisolone. Endocr. Pract. 22, 434–439 (2016)
P.M. Zelissen, R.J. Croughs, P.P. van Rijk, J.A. Raymakers, Effect of glucocorticoid replacement therapy on bone mineral density in patients with Addison disease. Ann. Intern. Med. 120, 207–210 (1994)
N. Chikada, T. Imaki, M. Hotta, K. Sato, K. Takano, An assessment of bone mineral density in patients with Addison’s disease and isolated ACTH deficiency treated with glucocorticoid. Endocr. J. 51, 355–360 (2004)
M.A. Valero, M. Leon, M.P. Ruiz Valdepeñas, L. Larrodera, M.B. Lopez, K. Papapietro, A. Jara, F. Hawkins, Bone density and turnover in Addison’s disease: effect of glucocorticoid treatment. Bone Miner. 26, 9–17 (1994)
L.A. Behan, G. Kelleher, M.J. Hannon, J.J. Brady, B. Rogers, W. Tormey, D. Smith, C.J. Thompson, M.J. McKenna, A. Agha, Low-dose hydrocortisone replacement therapy is associated with improved bone remodelling balance in hypopituitary male patients. Eur. J. Endocrinol. 170, 141–150 (2013)
J. Schulz, K.R. Frey, M.S. Cooper, K. Zopf, M. Ventz, S. Diederich, M. Quinkler, Reduction in daily hydrocortisone dose improves bone health in primary adrenal insufficiency. Eur. J. Endocrinol. 174, 531–538 (2016)
G. Mazziotti, A. Angeli, J.P. Bilezikian, E. Canalis, A. Giustina, Glucocorticoid-induced osteoporosis: an update. Trends Endocrinol. Metab. 7, 144–149 (2006)
F.P. Cappuccio, N.D. Markandu, G.A. MacGregor, Renal handling of calcium and phosphate during mineralocorticoid administration in normal subjects. Nephron 48, 280–283 (1988)
W.N. Suki, R.S. Schwettmann, F.C. Rector Jr, D.W. Seldin, Effect of chronic mineralocorticoid administration on calcium excretion in the rat. Am. J. Physiol. 215, 71–74 (1968)
E. Rossi, C. Sani, F. Perazzoli, M.C. Casoli, A. Negro, C. Dotti, Alterations of calcium metabolism and of parathyroid function in primary aldosteronism, and their reversal by spironolactone or by surgical removal of aldosterone-producing adenomas. Am. J. Hypertens. 8, 884–893 (1995)
L. Ceccoli, V. Ronconi, L. Giovannini, M. Marcheggiani, F. Turchi, M. Boscaro, G. Giacchetti, Bone health and aldosterone excess. Osteoporos. Int. 24, 2801–2807 (2013)
L.Petramala, L.Zinnamosca, A.Settevendemmie, C.Marinelli, M.Nardi, A.Concistrè, F.Corpaci, G.Tonnarini, G.De Toma, C.Letizia Bone and Mineral metabolism in patients with primary aldosteronism.Int. J. Endocrinol (2014). doi:10.1155/2014/836529
Y. Zhang, B. Feng, Association of serum parathyrine and calcium levels with primary aldosteronism: a meta-analysis. Int. J. Clin. Exp. Med. 8, 14625–14633 (2015)
S. Beavan, A. Horner, S. Bord, D. Ireland, J. Compston, Colocalization of glucocorticoid and mineralocorticoid receptors in human bone. J. Bone Miner. Res. 16, 1496–1504 (2001)
N.Z. Lu, J.B. Collins, S.F. Grissom, J.A. Cidlowski, Selective regulation of bone cell apoptosis by translational isoforms of the glucocorticoid receptor. Mol. Cell Biol. 27, 7143–7160 (2007)
R. La Corte, F. Trotta, S. Adami, Glucocorticoid receptors and bone. Curr. Pharm. Des. 16, 3586–3592 (2010)
C.M. Jewell, A.B. Scoltock, B.L. Hamel, M.R. Yudt, J.A. Cidlowski, Complex human glucocorticoid receptor dim mutations define glucocorticoid-induced apoptotic resistance in bone cells. Mol. Endocrinol. 26, 244–256 (2012)
P. Moutsatsou, E. Kassi, A.G. Papavassiliou, Glucocorticoid receptor signaling in bone cells. Trends Mol. Med. 18, 348–359 (2012)
H.H. Conaway, P. Henning, A. Lie, J. Tuckermann, U.H. Lerner, Activation of dimeric glucocorticoid receptors in osteoclast progenitors potentiates RANKL-induced mature osteoclast bone resorbing activity. Bone 93, 43–54 (2016)
M.K. Agarwal, F. Mirshahi, M. Mirshahi, S. Bracq, J. Chentoufi, M. Hott, A. Jullienne, P.J. Marie, Evidence for receptor-mediated mineralocorticoid action in rat osteoblastic cells. Am. J. Physiol. 270, C1088–C1095 (1996)
T. Fumoto, K.A. Ishii, M. Ito, S. Berger, G. Schütz, K. Ikeda, Mineralocorticoid receptor function in bone metabolism and its role in glucocorticoid-induced osteopenia. Biochem. Biophys. Res. Commun. 447, 407–412 (2014)
K.K. Miller, B.M. Biller, J. Hier, E. Arena, A. Klibanski, Androgens and bone density in women with hypopituitarism. J. Clin. Endocr. Metab. 87, 2770–2776 (2002)
L.J. Dominguez, M. Barbagallo, L. Moro, Collagen overglycosylation: a biochemical feature that may contribute to bone quality. Biochem. Biophys. Res. Commun. 330, 1–4 (2005)
E. Seeman, P.D. Delmas, Bone quality - the material and structural basis of bone strength and fragility. N. Engl. J. Med. 354, 2250–2261 (2006)
E. Canalis, G. Mazziotti, A. Giustina, J.P. Bilezikian, Glucocorticoid-induced osteoporosis: pathophysiology and therapy. Osteoporos. Int. 18, 1319–1328 (2007)
G. Mazziotti, A. Giustina, Glucocorticoids and the regulation of growth hormone secretion. Nat. Rev. Endocrinol. 9, 265–276 (2013)
O. Svejme, H.G. Ahlborg, J.Å. Nilsson, M.K. Karlsson, Early menopause and risk of osteoporosis, fracture and mortality: a 34-year prospective observational study in 390 women. Br. J. Obstet. Gynaecol. 119, 810–816 (2012)
V.N. Shah, C.S. Shah, J.K. Snell-Bergeon, Type 1 diabetes and risk of fracture: meta-analysis and review of the literature. Diabet. Med. 32, 1134–1142 (2015)
W. Rathmann, K. Kostev, Fracture risk in patients with newly diagnosed type 2 diabetes: a retrospective database analysis in primary care. J. Diabetes Complicat. 29, 766–770 (2015)
D.L. Kamen, J.D. Alele, Skeletal manifestations of systemic autoimmune diseases. Curr. Opin. Endocrinol. Diabetes Obes. 17, 540–545 (2010)
F. Lombardi, A. Franzese, D. Iafusco, A. del Puente, A. Esposito, F. Prisco, R. Troncone, G. Valerio, Bone involvement in clusters of autoimmune diseases: just a complication? Bone 46, 551–555 (2010)
Funding
This study was supported in part by a grant from the EU 7th Framework Programme, EurAdrenal project: Pathophysiology and Natural Course of Autoimmune Adrenal Failure in Europe. Grant No. 2008-201167; and by a grant ex 60% from the of University of Padua.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committees and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Camozzi, V., Betterle, C., Frigo, A.C. et al. Vertebral fractures assessed with dual-energy X-ray absorptiometry in patients with Addison’s disease on glucocorticoid and mineralocorticoid replacement therapy. Endocrine 59, 319–329 (2018). https://doi.org/10.1007/s12020-017-1380-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-017-1380-8