Abstract
There are possibly millions of mold species on earth. The vast majority of these mold spores live in harmony with humans, rarely causing disease. The rare species that does cause disease does so by triggering allergies or asthma, or may be involved in hypersensitivity diseases such as allergic bronchopulmonary aspergillosis or allergic fungal sinusitis. Other hypersensitivity diseases include those related to occupational or domiciliary exposures to certain mold species, as in the case of Pigeon Breeder’s disease, Farmer’s lung, or humidifier fever. The final proven category of fungal diseases is through infection, as in the case of onchomycosis or coccidiomycosis. These diseases can be treated using anti-fungal agents. Molds and fungi can also be particularly important in infections that occur in immunocompromised patients. Systemic candidiasis does not occur unless the individual is immunodeficient. Previous reports of “toxic mold syndrome” or “toxic black mold” have been shown to be no more than media hype and mass hysteria, partly stemming from the misinterpreted concept of the “sick building syndrome.” There is no scientific evidence that exposure to visible black mold in apartments and buildings can lead to the vague and subjective symptoms of memory loss, inability to focus, fatigue, and headaches that were reported by people who erroneously believed that they were suffering from “mycotoxicosis.” Similarly, a causal relationship between cases of infant pulmonary hemorrhage and exposure to “black mold” has never been proven. Finally, there is no evidence of a link between autoimmune disease and mold exposure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mold is a common name for a visible group of fungi that grow as multicellular filaments or hyphae, which then aggregate into web-like structures or mycelia. To date, approximately 100,000 fungi have been described, but true fungal diversity is likely to be at least 7- to 10-fold greater. According to other estimates, as many as 5 million fungal species may await study, description, and classification [1], but the true figure is likely to be somewhere in between [2]. Fungi living in the soil and on plants have vital roles in decomposing organic matter thereby making essential nutrients such as nitrogen and phosphorus available to other organisms. Indeed, the majority of plants would not survive without mycorrhiza, i.e., the symbiotic relationship between the mycelium of a fungus with the roots of the plant, which helps in supplying the plant with water and other necessary nutrients. For humans, yeasts (unicellular fungi) and molds are invaluable in the production of various foods (breads, certain cheeses) and beverages (e.g., beer and wine) and as sources of medications (e.g., antibiotics, immunosuppressants, and statins). Both outdoor and indoor environments contain highly diverse and somewhat different mycobiomes, even if the distribution of species and their levels indoor are greatly influenced by their outdoor counterparts. This means that molds and other fungi are ubiquitous. Indeed, they even live in and on every human being; the human mouth alone may harbor >20 of the >100 species of fungi that have been detected in the oral cavity. In those patients who do have problems attributable to mold, there are well-established biophysiological mechanisms through which disease can occur, namely by inducing hypersensitivity reactions and infection in susceptible individuals. Some examples of this would be the uncommon diseases such as farmer’s lung and pigeon breeder’s disease, patients characterized by fever, dramatic swelling of lymph nodes, and infiltrates in the lung. If untreated, they will likely die. There is also the possibility of a systemic infection and this would be found in individuals who are immunocompromised, e.g., patients with HIV or patients born with a deficient immune system. There is also the potential for allergy to mold, and in those individuals with asthma (who are allergic to mold), there is the potential for asthma exacerbation during exposure. These exacerbations are, however, completely reversible and do not cause any lasting problems. It should be noted that there is a long list of poorly defined health effects that some have complained are secondary to mold exposure, but these observations are flawed, they lack controls, and are non-specific and lack credible medical plausibility. In this review, we will discuss in detail the concept and the relationship between mold and human health.
Methods for Assessing Fungal Concentrations
There are a great number of methods that measure the concentrations of total molds or individual mold species in indoor and outdoor environments. One method for assessing the levels of airborne fungi is to collect a sample over several hours (at least 8 h are recommended) and count spores microscopically to estimate total fungal spores. Another approach is to use fungal cell wall constituents such as ergosterol or (1-3, 1-6)-β-D-glucans as markers of total fungal biomass, but this does not even allow the determination of spore counts and none of these methods provide information on the genera and species present. To identify fungal species, the classical method is based on culturing spores collected from the air or dust. Fungi are ubiquitous and airborne-viable fungal spores are detectable in nearly all indoor environments, though with considerable variation both over short- and long-term observation periods and between geographic areas [3]. Outdoor levels of total culturable fungi range from nearly undetectable to 105 colony-forming units (CFU)/m3. In unselected homes, indoor air concentrations generally vary from below the detection limit to >2 × 103 CFU/m3 [4–7] and similar ranges have been reported for non-residential environments [3, 8].
The culture-based quantification of airborne fungi has some major drawbacks. The duration of sampling has to be very short (generally <5 min) in order to prevent sampler overload. Fungal spores differ in their cultivability and culture requirements; hence, only a few species grow on the commonly used culture media. In addition, non-viable spores and other fungal materials (fragments) can contribute to allergen [9], mycotoxin [10], and polysaccharide exposure [11], but are not captured by culture-based methods. Not surprisingly, the number of CFU per square meter of air obtained by culture methods is at least 10-fold lower than the corresponding fungal spore counts [3].
More recently, quantitative polymerase chain reaction (qPCR) has been used to measure indoor fungal concentrations. This is a very sensitive method that is much faster than culture, does not require great expertise in identifying fungal genera or species, and assesses both viable and non-viable fungal material. In direct comparisons with culture-based results, the levels of cell equivalents obtained with qPCR for individual species or assay groups are generally two to three orders of magnitude higher compared to the CFU values both in air [12] and in dust [13]. If sufficient numbers of fungal species are targeted, qPCR can reveal a much greater diversity of the indoor fungal biome in terms of the number of detected species compared to fungal culture. However, the requirement of pre-selecting the targeted fungi means that the results of qPCR-based studies can rarely be compared directly because they frequently target different numbers of species or assay groups. This requirement also makes qPCR unsuitable for appreciating the true diversity of the fungal biome in a given environment. For this purpose, other culture-independent methods relying on internal transcribed spacer region sequencing are more appropriate. Though less sensitive than qPCR, they have nonetheless revealed the indoor mycobiome to be much more diverse than previously appreciated in terms of the number of detected species [14, 15].
Health Effects of Fungi
Allergy
Sensitization
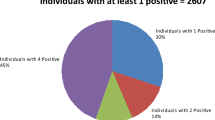
According to the WHO/International Union of Immunological Societies (IUIS) Allergen Nomenclature subcommittee, there are 111 officially approved fungal allergens from 22 species of Ascomycota (86 allergens), 6 species of Basidiomycota (23 allergens), and 1 species of Zygomycota (2 allergens) (see www.allergen.org). However, the actual list of fungal allergens is far longer, particularly when only partially characterized ones are included [16, 17] and is likely to grow further once the true diversity of the indoor and outdoor fungal populations and the allergenicity of the newly recognized species becomes more fully appreciated [1, 18] (see Table 1 for sensitization rates to some infrequently tested fungal antigens). Currently, the most widely acknowledged allergenic mold species are members of the genera Alternaria and Cladosporium among those considered to be outdoor molds, and Aspergillus and Penicillium among those considered to be indoor molds.
In the general population, the frequency of sensitization to Alternaria ranges from 0.2–14.4%; the corresponding figures for Cladosporium are 0–11.9% [20, 21]. The overall sensitization rate to fungal allergens was estimated to be 8.3% in a population-based study of German children, but is considerably higher in atopic subjects, particularly in patients with severe asthma [16]. The true sensitization rate remains unknown not only because many indoor fungal species remain to be identified [14, 15] but also because few fungal extracts are commercially available and these are not standardized and vary widely in their antigen contents and IgE-binding capacity [22]. This in turn is attributable to the complex growth habits of fungi, the variability in allergen expression between different strains of the same species, the shifts in the protein expression profile between different growth stages and in response to different substrates and nutrient availability, and the extensive cross-reactivity of fungal antigens, all of which make the development of standardized reference extracts difficult if not impossible. It is important to note that allergens differ in their potency. For example, at the same dose, exposure to peanut alone is much more likely to induce anaphylaxis than exposure to multiple pollens in individuals with allergies to both peanut and olive tree pollens. The most potent allergens are those found in food, followed by cat, then house dust, and the very end of the list is mold. In other words, exposure to mold is much less likely at the equivalent dose to induce a clinically significant allergic reaction than other allergens.
Asthma and Rhinitis
In numerous epidemiological studies, sensitization to fungi and subsequent exposure to outdoor airborne fungal allergens, in particular Alternaria alternata and Cladosporium herbarum, is associated with the development of asthma, its persistence from childhood into early adulthood, and the severity of its symptoms. Interestingly, there is no evidence that this extends to indoor mold exposure. Sensitization to fungal allergens has also been demonstrated in patients with allergic rhinitis and atopic dermatitis, but it has not been conclusively proven that exposure to airborne mold, whether indoors or outdoors, is responsible for their clinical manifestations. The relative lack of influence of indoor mold on the induction and sensitization is very likely due to the overwhelming outdoor exposure that all individuals will have throughout their life spans. This is illustrated by the observations that there are no significant differences in allergies and asthma in patients who live in humid environments versus those that live in a dry environment; all, at some point or another, have continual exposure to the ubiquitous fungal allergens found in air.
Allergic Bronchopulmonary Aspergillosis and Allergic Fungal Rhinosinusitis
One of the most severe, if rare, fungus-induced allergic diseases is allergic bronchopulmonary aspergillosis (ABPA). It is caused by hypersensitivity to Aspergillus fumigatus and occurs in patients with asthma, cystic fibrosis, or chronic obstructive pulmonary disease (COPD). Several other fungi, mainly Candida, Bipolaris spp., Schizophyllum commune, and Curvularia spp. are capable of causing a clinical entity similar to ABPA, which is then called allergic bronchopulmonary mycosis (ABPM) [23]. It appears to be associated with asthma much less frequently than ABPA.
Since germination of conidia into mycelium is associated with greater production and release of allergens [24], colonization with Aspergillus is thought to be required for sensitization and the generation of Aspergillus-specific IgE as well as IgG antibodies [25]. In keeping with the presence of both classes of antibodies, type I as well as type III hypersensitivity reactions contributes to the pathogenesis of ABPA. It is the tissue dysfunction induced by pre-existing airway damage, mucus hypersecretion, and defective clearance that allows the germination of fungal spores within the lung and, thus, colonization and chronic exposure to fungal allergens. This makes ABPA an allergic rather than an infectious disease, even if it is occasionally listed with the infectious fungal diseases [26].
Allergic fungal sinusitis or rhinosinusitis (AFRS) is a localized hypersensitivity reaction similar to that seen in ABPA and first described in patients with ABPA [27]. It can occur when fungi colonize the sinuses of subjects with underlying allergic disease and impaired tissue drainage. While A. fumigatus continues to be the most frequently isolated mold species, it has since been recognized that other Aspergillus species, dematiaceous fungi (dark pigmented fungi, such as members of the genera Bipolaris, Exserohilum, Curvularia, and Alternaria), and various other fungal species can cause AFRS [28].
Of particular note, fungal colonization of the lungs is common in patients with asthma, cystic fibrosis, or COPD, and fungal colonization in the sinuses is seen even in the vast majority of healthy subjects; yet only some of them develop ABPA or AFRS. The reasons for this are currently unclear, but genetic as well as other predisposing factors are likely to play a major role [25]. Also note that A. fumigatus is a common outdoor mold, even if it has been associated with building moisture in some studies. Likewise, most of the molds and yeasts implicated in ABPM and AFRS are found primarily outdoors or detected with near equal frequency in outdoor and indoor environments. There is nothing to conclusively link indoor mold exposure to the development of ABPA, ABPM, or AFRS.
Hypersensitivity Pneumonitis
Hypersensitivity pneumonitis (HP), also called extrinsic allergic alveolitis, is an interstitial granulomatous lung disease that occurs in susceptible individuals who have become sensitized to a triggering antigen as a result of repeated inhalation exposure to organic dust [29]. Prolonged and/or high-dose exposure is required for sensitization to occur and symptoms to develop. The presentation of HP is traditionally subdivided into acute, subacute, and chronic, but considerable overlap between these forms of presentation is increasingly recognized. A CT scan can be utilized to identify these forms, as acute HP may show pulmonary edema, while subacute HP may show a ground glass appearance. Chronic HP usually demonstrates bronchiectasis or signs of pulmonary fibrosis such as reticulation on CT scan [30].
It is very important to recognize this disease in its earliest stages, when antigen removal is often sufficient for recovery. If antigen exposure continues, chronic HP with irreversible pulmonary fibrosis can develop. Hypersensitivity pneumonitis is most frequently caused by bird proteins (pigeon breeders’ disease or bird fancier’s HP) and bacteria. For example, one of the most frequent causes of farmer’s lung, another designation of HP, are thermophilic actinomycetes. However, a variety of fungal antigens also have been implicated in various forms of occupational HP, including A. alternata, Aspergillus spp., and Penicillium spp. along with other molds and mushrooms [29, 31].
Patients with HP usually have high levels of antigen-specific IgG antibodies, preferably detected as precipitins in double diffusion tests. Whether these IgG antibodies merely represent a marker of exposure or actively participate in the pathogenesis of the disease remains uncertain, but it is generally believed that HP involves a combination of types III and IV hypersensitivity reactions. In the settings where HP occurs, many people may be exposed to the same levels of the causative antigens and some of those may actually become sensitized, as indicated by the presence of specific IgG antibodies in their serum. Yet, only a few of these individuals actually develop HP. This strongly suggests that genetic susceptibility or gene-environment interactions play a major role.
It had long been felt that exposure levels commonly encountered in the home or white-collar work environment would be unlikely to cause HP. One well-known exception has been a seasonal form of HP that occurs mainly in Japan and is caused by members of the genus Trichosporon. Each summer after the rainy season, this summer-type HP affects some residents of homes south of latitude of 40° north. However, there is an increasing number of reports linking other types of household or office mold exposure to the development of HP [32, 33]. These include cases of humidifier lung, which may involve fungi, ameba, thermophilic bacteria, or mixtures of all three, as are found on humidifiers, dehumidifiers, or contaminated air conditioners. Fungal species implicated in HP due to home or office exposures include Cladosporium cladosporioides, C. herbarum [34], A. fumigatus [35], Bjerkandera adusta [36], and Fusarium vasinfectum [37]. A fatal outcome of HP after “home exposure” to mold has been reported [38], but the exposure level was unusually high because the patient did the renovation of his severely mold-damaged mobile home. F. vasinfectum was isolated from wall scrapings in his home, suggesting that the patient had been chronically exposed to this mold, followed by very high levels of exposure during the renovation, which led to an acute exacerbation of his symptoms. Death is believed to have resulted from a complication of an open lung biopsy performed in the context of continuously declining lung function.
Fungal Infections
Infections constitute another well-established way in which fungi can affect human health. It has been estimated that approximately 300–600 fungal species can be pathogenic to humans, but only about 30 of those are responsible for the vast majority of fungal infections. In healthy, immunocompetent individuals, fungal infections mostly remain superficial, i.e., affect the skin (tinea), nails (onychomycosis), or mucosal surfaces (thrush). A limited number of fungal pathogens can cause more serious disease in healthy subjects. These include several dimorphic fungi, meaning fungi that generally grow as yeasts at body temperature, but as molds at room temperature. Four types of these pathogenic dimorphic fungi are endemic in the USA, namely Blastomyces dermatitides, Coccidioides immitis, Histoplasma capsulatum, and Cryptococcus gattii (see also Table 2 for the diseases they cause and their areas of endemicity). It is noteworthy that infection with any one of these endemic species does not invariably cause symptomatic disease (see also Table 2), indicating that individual susceptibility is a decisive factor. Chronic pulmonary aspergillosis may not only occur in the context of an intact immune system but also in patients who have pre-existing lung disease, such as tuberculosis, non-tuberculous mycobacterial disease, asthma, COPD, pneumothorax, or sarcoidosis.
Other invasive fungal infections are caused by opportunistic fungal pathogens, i.e., fungi that are commensals or are ubiquitous in the environment, do not cause disease in healthy individuals, but have the ability to cause severe, frequently fatal, disease in subjects who are in some way immunocompromised. For example, several species of the yeast Candida, in particular Candida albicans, are ubiquitous commensal organisms that live on human mucosal surfaces, but account for about 80% of major systemic fungal infections in immunocompromised patients. Unlike mucosal candida infections, “systemic candidiasis” is a condition that only occurs in people with specific risk factors, such as HIV, immunosuppressed individuals, hospitalized individuals, or the presence of a central line or other invasive foreign body. Unfortunately, many healthy individuals often claim to have systemic candidiasis without any evidence of positive cultures, or identification of the presence of candida by DNA analysis.
Cryptococcus neoformans is a yeast with a worldwide distribution found in the soil and trees, but also associated with bird guano. It most commonly infects the central nervous system, lung, or skin and affects patients with immune deficiencies, in particular those with HIV infection or AIDS. In addition to yeasts, molds can also cause serious infections. Foremost among these is, once again, A. fumigatus, the primary cause of invasive aspergillosis, although other species of Aspergillus have been implicated as well [39]. This invasive fungal infection used to occur mainly in neutropenic hosts, but is now increasingly diagnosed in non-neutropenic hosts—i.e., subjects who are immunocompromised because of corticosteroid use, chemotherapy, or immunosuppressive therapy after hematopoetic stem cell transplants or solid organ transplants. A variety of Fusarium species can also cause invasive and disseminated disease in immunocompromised hosts, with the greatest risk of dissemination in patients with acute leukemia, severe neutropenia, and recipients of hematopoetic stem cell transplants [40]. It must be underscored that fungi, including the potentially pathogenic yeasts and molds are ubiquitous, and this makes it virtually impossible to prevent immunocompromised patients from being exposed to them.
Toxicity
Certain fungal genera can produce mycotoxins, defined as secondary metabolites that can cause a toxic response in vertebrates when ingested in sufficient doses [41, 42]. When such toxins harm bacteria, we choose to call them antibiotics. As secondary metabolites, mycotoxins are not required for primary growth or reproduction, and their precise role remains to be elucidated. Several hundred mycotoxins have been identified to date. Only a limited number of mycotoxins impact global agriculture by reducing crop yield and endangering food security. These are mainly produced by members of the genera Aspergillus, Penicillium, and Fusarium and include the major aflatoxins, namely aflatoxin (AF) B1, AFB2, AFG1, and AFG2; ochratoxin A (OTA); certain trichothecenes such as deoxynivalenol (DON), nivalenol, T-2 toxin and HT-2 toxin; the fumonisins B1 (FB1) and FB2; and zearalenone (see also Table 3 for a selected list of mycotoxins and some of their major producers). Mycotoxicosis in humans and animals is due to the ingestion of contaminated food and feed. Therefore, the maximum concentration of the major mycotoxins in the most frequently affected foodstuffs is regulated in the majority of countries, and acceptable dietary intake levels have been established. As a result, acute toxicoses are rare even in developing countries, but an example is the outbreak of aflatoxicosis in Kenya in 2004 during which 317 cases of acute liver failure occurred and at least 125 people eventually died [43]. Even in industrialized countries, chronic mycotoxicosis may not be completely preventable in certain groups with high consumption of specific dietary items. Humans exhibit substantial differences in susceptibility due to genetic differences in the enzymatic pathways involved in the bioactivation and metabolism of mycotoxins and differential influences of age, sex, weight, dietary factors, nutritional status, presence of chronic infections, and possibly other lifestyle and environmental aspects [41]. Such differences in susceptibility are also seen between and within animal species. Overall, mycotoxins can affect essentially every organ and tissue in the body [42]. Yet, individual mycotoxins show some specificity in the mechanisms of toxicity and also in the tissues they affect, even if these may differ between species. Many mycotoxins are genotoxic and carcinogenic in animals, and chronic mycotoxicosis in humans may also manifest as cancer [41, 42]. The International Agency for Research on Cancer (IARC) has classified the major aflatoxins (AFB1, AFB2, AFG1, AFG2 and the metabolite AFM1) as human carcinogens. As Table 3 shows, several other mycotoxins are considered potential human carcinogens, and yet others cannot currently be classified as to their carcinogenicity.
The only plausible basis for mycotoxicosis would be from ingestion. Although there have been inhalation cases reported, they are very poorly documented and not plausible [44–46]. Organic dust toxic syndrome (ODTS) represents a toxicosis resulting from massive exposure to highly diverse mixtures of fungi, bacteria, and their toxins and other constituents [27, 47, 48]. Exposure levels exceeding 1 × 107 CFU/m3 or and likely even ≥1 × 1010 spores/m3 seem to be required for the occurrence of ODTS [47, 48].
Does Dampness Mean Mold?
Associations between Dampness/Mold and Respiratory Health
Respiratory symptoms are the most frequent symptoms reported by occupants of certain buildings with poor indoor air quality and subsumed under the designation of “Sick building syndrome” (SBS), which also includes eye, nose, or throat irritation, cough, dry or itchy skin, nausea, headaches, dizziness, difficulties concentrating, and fatigue. This term is a misnomer since the building is not sick, but its occupants report feeling sick while in the building. In addition, the symptoms it encompasses do not fulfill the definition of a syndrome; hence, a better term would be non-specific building-related symptoms. Investigators generally are unable to find any specific cause for the reported symptoms and a medical diagnosis is equally difficult. However, a large variety of physical causes and psychosocial factors have been linked to such non-specific building-related symptoms; one should consider insufficient ventilation, certain chemical emissions, and dampness or evidence of moisture damage.
As reviewed by several scientific bodies, including the Institute of Medicine (IOM) and the WHO [24, 49–53], a long list of studies from a variety of geographic areas quite consistently show signs of building dampness or mold to be associated with a variety of adverse health effects. These associations are seen both in domestic and public building environments and they are present whether the signs of dampness/mold are reported by the occupants or assessed by an inspector. They are particularly detected in allergic individuals, but also in non-atopic subjects. There have been far fewer attempts to link exposure to dampness or mold to symptoms typically associated with the so-called sick building syndrome, i.e., irritation of eyes, skin, mucous membranes, fatigue, nausea, headache, insomnia, and difficulty concentrating. The results have been quite inconsistent and in the majority of cases, no significant associations could be detected [49].
It needs to be underscored that the agents responsible for the statistical associations between indicators of building dampness and respiratory symptoms have not been identified. The assessment of “dampness or mold” most commonly relies on answers of the building occupants to questions that may cover anything from condensation on the windowpanes to visible mold or mold odor. The fact that these descriptors often yield similar risk estimates for many types of respiratory symptoms has been taken as an indication that indoor molds could be responsible. So far, this has proven impossible to conclusively demonstrate. With a few exceptions [6, 54–57], indicators of dampness or mold are not associated with total viable fungi in air [4, 13, 15, 58–61] or dust [4, 13, 15, 61]. The associations may even differ between two rooms within the same household [5], suggesting that they are chance findings—in part due to the lack of correction for multiple comparisons. Correlations between signs and dampness and other potential measures of fungal exposure, such as total fungal cell equivalents obtained by qPCR [15], ergosterol, or β-glucans also are mostly weak or entirely absent [61–63]. When attempts are made to link specific fungal genera, species or assay groups identified via qPCR analyses to moisture damage the results differ not only from those obtained by culture-based methods in the same study [13], but also from those of other investigations [15, 64–66]. Furthermore, the various measures of fungal exposure rarely correlate with each other [4, 15], including airborne and dustborne levels of total viable fungi [4, 5]. Even using qPCR and a sampling time of 6–8 h for air samples, no correlation could be detected between dustborne and airborne concentrations of 36 mold species and the few exceptions showed correlation estimates of ≤0.34 [64].
Most importantly, studies that attempted to correlate specific measures of microbial exposures to health outcomes have yielded inconsistent and, at times, contradictory results [53]. Among the most recent investigations, there is at least one report of an association between airborne-viable mold levels ≥300 CFU/m3 in schools and an increased risk of dry cough at night, persistent cough, and rhinitis [8]. Importantly, however, studies failed to reveal any significant correlations between viable airborne mold and asthma or allergy in children [58, 67], “SBS” symptoms in adults [54], or respiratory health in the elderly [68]. A similar lack of association was noted between dustborne concentrations of culturable mold, ergosterol, β-glucans, or fungal DNA cell equivalents (by qPCR) in homes, schools, or both and allergic disease, asthma, respiratory symptoms, or lung function in children [61, 69–72]. Finally, others detected a protective effect of total viable airborne fungi on throat and respiratory symptoms and a similar protective effect was seen for the genus Cladosporium, while Penicillium was inversely associated with skin symptoms [73]. The presence of significant correlations appears to depend quite strongly on the precise nature of the sample. [7, 8, 73, 74]. This is illustrated by a series of publications arising from the same dataset obtained by analyzing different types of dust samples from Malaysian schools [75–77]. Wheeze and daytime attacks of breathlessness were found to correlate with Aspergillus versicolor DNA concentrations in dust collected in Petri dishes kept on top of book shelves over a period of 7 days, but not with A. versicolor DNA in dust samples swabbed from the top of the classroom blackboard [75]. Similarly, Streptomyces DNA from Petri dishes, but not from swab samples, was associated with doctor-diagnosed asthma. Total as well as specific fungal DNA measured in settled dust (vacuumed from the floor and other higher surfaces) was essentially not related with self-reported weekly symptoms of rhinitis or various types of SBS symptoms (i.e., ocular, throat, dermal symptoms, headache, tiredness) [76]. Yet, when total fungal DNA was measured in swab samples of dust from the top of the blackboard associations with rhinitis, eye and throat symptoms were detected, but not in dust collected in Petri dishes [76].
Are Mold Spores the Relevant Exposure?
Such discrepancies raise the questions of whether (a) molds constitute the relevant exposure and (b) this exposure is assessed in a meaningful way. The first question cannot be answered at this time, in part because the answer to the second question is a resounding “no.” It has been largely ignored that there can be enormous within-day and day-to-day variability in the levels of total culturable fungi in indoor air [78], even if the variation may not to be statistically significant in all regions [79]. In addition, total viable spore counts in indoor air show marked variation over longer periods of time [56], particularly during different seasons [80]. Season has also been identified as an important determinant of airborne fungal levels in cross-sectional studies [5–7, 60, 80]. It has been calculated that 11 samples would have to be obtained on separate days and at different times of the day in order to characterize the true (within the 95% confidence interval) mean airborne-viable fungal concentration of a normal residence, at least in a subarctic climate. Yet, the vast majority of studies that attempted to correlate fungal measurement with reported dampness or mold or with respiratory symptoms relied on one single measurement of airborne fungal levels. Further tape lifts for mold evaluation and quantitation are statistically flawed and not clinically useful.
It is frequently claimed that dust—whether floor dust or airborne settled dust—provides a time-integrated or cumulative measure of fungal exposure [5, 12, 61, 81]. However, there are data suggesting that dustborne fungi represent a unique population and, therefore, are not representative of fungal exposure in the breathing zone [4]. In addition, tape lifts for mold evaluation and quantitation are flawed and do not provide meaningful data. Furthermore, considerable variation over time is also seen in dustborne mold concentrations, whether assessed as total viable fungi [82, 83], total fungal biomass as represented by ergosterol concentrations [62], or as the concentrations of individual fungal genera, species, or assay groups determined by PCR [81]. Most importantly, the variation over time is greater within homes than between homes for both airborne and dustborne mold concentrations [56, 82]. According to calculations based on the ratio of the within-home to between-home variance, at least nine repeated measurements of dustborne culturable fungal concentrations would be necessary to keep the measurement bias below 20% [56, 82]. Can it really be more than chance, then, if the combined levels of three mold species (among a total of 36 species tested) detected in a single dust sample supposedly predict the development of asthma 6 years later [11]?
In view of the considerable short-term variation in fungal levels, it seems far more likely that the use of a single dust or air sample leads to massive exposure misclassification, particularly if one considers that sampling times as short as 1 min are common for the assessment of airborne viable fungi. This means that, when the concentrations of total indoor fungi or individual fungal species are derived from a single sample, their associations with health effects represent chance findings. It should also be remembered that culturable fungi represent only a small fraction of the total fungal biome and provide little insight into its true diversity and complexity. It is recommended to obtain an outdoor air sample at the same time as the indoor air sample so that the composition of the diversity of the mycobiomes and the rank order and concentrations of individual species in the two compartments can be compared in order to determine whether there is an indoor source for the species under investigation. However, since outdoor mold levels fluctuate to a similar or even greater extent compared to indoor concentrations, multiple measurements, including morning and afternoon samples, will be necessary in order to prevent misclassification [84].
Biomonitoring Is Not a Valid Measure of Mold Exposure
Serum IgG against mold is a much abused test. It is helpful in HP, but otherwise, it is to be expected that all individuals will have IgG antibodies against mold, just as they have IgG antibodies against an enormous number of other microbes. In fact, even in subjects with the same high occupational exposure level to molds, the specific IgG value is highly variable; conversely, even healthy individuals can have high levels of specific IgG [3]. Therefore, group mean concentrations in highly exposed workers constitute a marker of exposure, but the use of individual serum concentrations of specific IgG antibodies is not a validated indicator of exposure. The levels of mold-specific IgG detected in environmentally exposed subjects are at least 10 times lower compared to those found in patients with HP [85] and do not show associations with various measures of indoor mold exposure [86–88] or with symptoms attributed to this exposure [85, 89]. The problems discussed in the context of determining mold-specific IgE antibodies also hold for IgG, i.e., the lack of standardized fungal extracts and the extensive cross-reactivity between molds.
Other Potential Explanation for the Associations between Dampness and Respiratory Health
The vast majority of studies that attempt to link respiratory and other health outcomes to building-related factors, including investigations that encompass other SBS symptoms, are cross-sectional and rely on self-reported measures of both exposures and symptoms or health outcomes. This makes them particularly vulnerable to reporting bias. Indeed, both logistic regression analysis and structural equation analysis of longitudinal data strongly suggest that the direction of the causal pathway between the perceived indoor environment and self-reported symptoms is opposite to what is generally assumed. In other words, perceived health problems may lead to complaints about the indoor environment rather than the reverse [90, 91].
Among the physical factors that could mediate an effect of dampness on health, the exclusive focus on molds is difficult to comprehend given the high complexity of the indoor environment even when there is no excess moisture. In addition to a large variety of molds, there is likely to be a similar variety of bacteria; volatile organic compounds (VOC, which can be of microbial origin or gassed off by building materials, furniture, carpeting, etc.); semivolatile organic compounds (sVOC); and other chemicals; along with allergens given off by pets, house dust mites, and possibly even rodents. In damp indoor environments, the concentrations of many of these substances are likely to be elevated because not only certain fungi require high moisture levels for optimal growth but certain bacteria and even dust mites also thrive and reproduce more rapidly at a higher relative humidity [24]. Yet, the potential effects of dampness on changes in the bacterial biome and the impact of these changes on health outcomes have rarely been investigated and the few existing studies have yielded contradictory results [24, 63, 72]. Of note, the same methodological issues that severely limit the validity of the results from fungal studies also apply to bacterial investigations, including the great diversity and temporal as well as spatial variability of bacterial populations both outdoor [92] and indoor [93].
Even though moisture is expected to increase the number of microbes, microbes do not appear to greatly contribute to the indoor air concentrations of total VOC [94]. Nonetheless, moisture accelerates the process of chemical or biological degradation, thereby resulting in the release of chemicals [24]. In addition, increases in the relative humidity are associated with higher concentrations of VOC, possibly because of competition between the water and the VOC for sites of adsorption on certain materials [95]. The low concentrations at which VOC and most other chemicals individually are present in indoor environments are unlikely to represent a direct health hazard [96, 97]. Yet, it should be kept in mind that even relatively simple mixtures of substances may have more than additive, possibly synergistic, but also antagonistic, effects [96, 98]. In slightly more complex mixtures, even when substances are used at concentrations below the carefully determined “no observed effect” level, their combinations may have measurable effects [99]. Also note that even simple combinations of a mold, a bacterium, and a protozoon can have pro-inflammatory and cytotoxic effects that go beyond mere additivity [100–102], with the precise nature of the outcome depending on the proportion in which the individual microorganisms are present [103]. Most remarkably, a mixture of fungal and bacterial spores derived from co-cultivation of their respective microorganisms can have different effects compared to co-exposure to the separately cultivated spores [103–105]. This should make it clear that the focus of attention should be widened to include fungi, bacteria, chemicals, and, above all, their interactions, even if that is likely to be a daunting task with the currently available tools. But, instead, the focus has all too often narrowed from molds in general to “toxic mold.”
Toxic Mold
Toxic Mold Syndrome
In the early 1990s, an unusual cluster of cases of pulmonary hemorrhage in infants occurred in Cleveland, OH [106]. Although early reports seemed to suggest a link between these cases and inhalation of mycotoxins produced by Stachybotrys chartarum, in particular, satratoxins, later epidemiological studies failed to confirm any causal relationship [107]. By that time, however, the initial reports had triggered widespread media coverage and the coining of the term “toxic mold syndrome.” Patients who present with what they consider mold-induced illness report a variety of non-specific symptoms (including upper and lower respiratory tract symptoms, headache, and fatigue) greatly resembling those subsumed under the term “SBS” [108, 109]. Indeed, “toxic mold syndrome” or simply “toxic mold” are terms that now are frequently used as synonymous with “sick building syndrome.” This implies that all of the non-specific symptoms that some people report in association with exposure to a certain building environment are blamed on mycotoxins, and many people think of mycotoxins as meaning satratoxins produced by S. chartarum. This is incorrect.
Toxigenic and Non-toxigenic Strains
In order to show conclusively that mycotoxins in general, or satratoxins in particular, are responsible for any effects on human health, it would have to be demonstrated that they are present and can be absorbed in sufficient amounts within a reasonably short time frame. Inhalation represents the most likely route of exposure to mycotoxins in indoor environments. The first thing to consider is that, in general, not all strains of a particular mycotoxin-producing species are toxigenic, i.e., have the ability to produce mycotoxins [110–112]. S. chartarum is a prime example: only 30–40% of its strains produce macrocyclic trichothecenes, including the highly toxic satratoxins G and H, while the other strains are characterized by atranone production [113, 114]. The two types of strains are classified as chemotypes S and A, respectively. Secondly, even if a strain is capable of producing a particular mycotoxin in vitro, the indoor environment from which the strain was isolated does not necessarily contain detectable levels of this mycotoxin [115]. This reflects that mycotoxin production depends on a large variety of factors, including the growth medium or substrate, the growth stage of the fungus, temperature, water activity, pH, and the presence of other fungi and bacteria [104, 111, 116]. Moisture-damaged buildings invariably contain complex mixtures of fungi and bacteria and these may compete for the same substrates and nutrients or may elaborate substances capable of inhibiting the toxin production of other microbes. This means that the mere presence of a toxigenic fungal species does not prove the presence of mycotoxins.
Airborne Mycotoxins
Mycotoxins are not volatile, but can become airborne on conidia [117, 118]. S. chartarum and other fungi are capable of exuding mycotoxins in fluid droplets in a process called guttation [119], but the clinical relevance of this ability remains untested. The conidia of S. chartarum are formed inside a sticky polysaccharide matrix and, therefore, not easily aerosolized. As a consequence, the presence of S. chartarum in air samples is difficult to demonstrate by culture-dependent or -independent methods, and the reported CFU or cell equivalent values are invariably low [8, 120, 121], even in homes with very heavy mold contamination [122]. Detection frequencies via qPCR in dust samples may be considerably higher, but even then the reported levels are very low [8, 123, 124].
Conidia or spores are not the only means of rendering fungal toxins airborne. Most fungal genera, including S. chartarum, also release smaller fragments, and there are data suggesting that these conidial and hyphal fragments can carry mycotoxins [10]. Hardin et al. [125] showed that the volume of 20,000 fragments with a spherical shape and a diameter of 0.3 μm would be required to make up the volume of a single spore. Based on the data available at the time, which showed that fragments outnumbered spores by 320:1 to 500:1, it was not plausible to claim that such fragments made a significant contribution to mycotoxin levels in the air. Since the surface area to volume ratio increases as the size of a sphere decreases, only 100 fragments would have the same surface area as one spore. In a recent field study, such fungal fragments were measured in moldy houses and found to outnumber spores by a factor of 103 to 106 to 111.
Exposure Levels and Risk Assessment
Exposure Levels
As summarized in Table 4, a variety of mycotoxins have been detected in indoor air in picogram per cubic meter concentrations, but with wide variations between studies and between buildings within studies [126–128], while dust contains levels of <1–43 pg/mg. The only reliable data on the detection of satratoxins in indoor air come from LC-MS/MS analysis and show concentrations of satratoxin G and satratoxin H of 0.25 and 0.43 ng/m3, respectively [126]. Assuming this data is even correct, breathing in such air at a respiratory minute volume of 6 L/min over a period of 8 h would result in the inhalation of only 0.72 ng of satratoxin G and 1.2 ng of satratoxin H; as per discussion above and below this is far less than the quantities humans are exposed to in normal activities, including ingestion of food.
Biomonitoring
Biomarkers of internal exposure were first developed for AB1 and more recently for OTA, while such markers are under development or in the process of validation for DON, and FB1 [42, 131]. Serum AFB1-albumin adducts are commonly used as a measure of chronic dietary exposure [42]. Such adduct formation has also been demonstrated after exposure via inhalation (with a possible contribution from dermal absorption) in workers exposed to AFB1 in various highly contaminated occupational settings [44–46, 131–133]. Only the highest exposure levels seem to results in detectable AFB1-albumin adduct concentrations after inhalation. It has been claimed that similar adducts between satratoxin G and albumin were present in serum of three adult subjects who were reportedly exposed to S. chartarum in their homes [134]. However, others have already criticized the ELISA employed for the detection of satratoxin as non-specific and unvalidated [125], and the results have not been replicated or independently confirmed since then.
Toxicokinetics
Data on the toxicokinetics of mycotoxins are limited, particularly after inhalation exposure, based on direct and high-dose administration, suggest that airway exposure may result in greater bioavailability and toxicity compared to oral or parenteral routes of administration [135–137], but this is not a consistent finding [138]. The toxicokinetic patterns of essentially all orally administered mycotoxins investigated to date show considerable variation between animal species and between strains within species. This raises the question of whether and to what extent animal data can be extrapolated to humans. In airway exposure studies, the issue is further complicated by the widespread practice of giving experimental animals high doses of pure mycotoxins as a bolus via intratracheal instillation. It seems unlikely that this, in any way, captures the pattern of human exposure, which generally would be expected to consist of chronic low doses of mycotoxins associated with spores or fungal fragments mycotoxins.
Based on all available data on airborne concentrations of mycotoxins in residential and agricultural environments, spore counts in these environments, and levels of mycotoxins per fungal spore, it is predicted that exposure levels to mycotoxins in non-agricultural indoor environments will remain below the “concentration of no toxicological concern,” which was calculated as 30 ng/m3 taking into account additional routes of exposure and assuming complete bioavailability [125]. The concentration of no toxicological concern is based on the concept of “threshold of toxicological concern” originally developed for dietary exposures and extends it to inhaled substances. An earlier modeling study essentially yielded the same conclusion [139].
The Toxicity of S. chartarum Spores of Chemotypes A and S
There are some animal studies showing S. chartarum spores to have detrimental health effects [3]. However, in all of these studies, S. chartarum was administered via intratracheal or intranasal instillation and mostly in very high doses. When similar protocols are used, almost any fungal spore will induce comparable responses. Compared to inhalation exposure, intratracheal and intranasal instillation increases the number of spores that reach the alveolar region. According to an overall comparison of the available animal data, this may give rise to greater inflammatory responses and granuloma formation in the lung and dissemination of the spores to other tissues [3].
Unlike fungal spores of other species, S. chartarum at very high doses and given into the airways directly can cause pulmonary hemorrhage, but this is seen with both chemotypes, suggesting that this effect is not, or at least not exclusively, attributable to the satratoxins or other macrocyclic trichothecenes [3]. It also requires spore doses that are not likely to occur in indoor environments [140]. However, because of the problems associated with the use of intratracheal or intranasal instillation, animal models based on these routes of administration should not form the basis for extrapolating dose-response relationships to humans [3]. In experimental animals, clear differences in satratoxin susceptibility exist between species and between strains within a species [141, 142]. At somewhat lower doses than were used in the early experiments, differences between the two chemotypes of S. chartarum may become apparent. However, they depend on the duration of the experimental treatment, the spore dose and the outcome measures, and they appear to be of a quantitative or pharmacokinetic rather than of a qualitative nature [141, 143, 144]. Most of the differences between treated and control animals were associated with the instillation of any fungal spores (S. chartarum of chemotype A or S or C. cladosporioides), with minor contributions from the species and toxigenicity of the spores.
There is no evidence that S. chartarum or its satratoxins have inflammatory effects in humans. We note that (1) its presence in the breathing zone is difficult to demonstrate and its detection on building materials is not sufficient, (2) the contribution of other fungi and bacteria in a contaminated building is a major confounder, and (3) there are no validated biomarkers for internal exposure assessment. As a consequence, even when the home or work environment is proven to be contaminated with S. chartarum, it is not possible to causally link the presence of this mold to the symptoms experienced by the occupants [89]. It should be pointed out, however, that mold-specific allergy may be the cause of mold-related symptoms in patients using an allergy panel of molds [108]. In others, the symptoms attributed to mold exposure may be due to allergic reactions to other aeroallergens, including some derived from the patients’ own pets [109]. Other pre-existing disorders or conditions may underlie the symptomatology in the majority of the remaining cases [109]. Importantly, a contribution from exposures that were not even considered much less investigated cannot be ruled out in any of these subjects.
Is there a Relationship between Mold and Autoimmunity?
Autoimmunity is a broad category of diseases in which the human body targets its own tissues. The presence of antibodies may be pathogenic, but in many cases may simply be an epiphenomenon [145]. The origin of autoimmune diseases is probably a combination of genetic [146, 147], epigenetic [148–150], and environmental factors [151–157], which interact in some chaotic or stochastic manner to produce these diseases in a way that we do not completely understand.
More recently, the microbiome has been targeted as a possible contributor to the development of autoimmunity [158, 159], but molds generally are not part of such investigations [159]. Even the role of probiotics in autoimmune diseases has been studied [161, 162], but again, there is no link between molds and autoimmunity.
Although it has been suggested that there is a relationship between mold exposure and autoimmunity, most of these reports are unfounded and are not based on solid scientific evidence. Unfortunately, many non-scientific and non-medical websites have been spreading false information about mold and autoimmune diseases such as chronic inflammatory demyelinating polyneuropathy (CIDP). CIDP is a disease that resembles Guillain-Barre syndrome, but there is no evidence that mold exposure is even remotely associated with this disease. In fact, a search of PubMed revealed that there are no studies confirming an association between CIDP and mold. There are numerous well-designed studies in recent years on the pathogenesis of autoimmune diseases, ranging from genetic predisposition [146, 147, 163, 164] to environmental triggers [165, 166], and yet none of them remotely suggest that molds can be a contributing factor to autoimmunity. Specific cellular [167] and humoral [168, 169] factors of both the innate [170] and adaptive [171–173] immune systems have been demonstrated to play roles in the development of the various autoimmune diseases. The cytokine milieu and the balance of T cells such as Treg and Th17 cells [167, 174], as well as various other cytokines [175–180] and cellular processes such as autophagy [181, 182] have been attributed to the development of autoimmune diseases, yet molds have never been shown to impact these pathways in a clinical significant manner.
In particular, one publication from 2003 describes a putative correlation between mold exposure and a myriad of inflammatory markers [183]. The study claims to establish a link between mold exposure and immunological dysfunction and coined the term “mixed mold mycotoxicosis.” However, the study is plagued by poor study design, selection bias, and an inability to establish a cause and effect relationship. Moreover, the clinical symptoms reported are vague and subjective and bear no relationship to autoimmunity with the exception of fibromyalgia [184], illustrating the disconnection between what is observed in the laboratory and what is clinically significant.
The closest anyone has come to uncovering an association between molds and autoimmunity is perhaps a paper describing anti-Saccharomyces cerevisiae antibodies in patients with Crohn’s disease and other autoimmune diseases. The role, if any, of these autoantibodies in Crohn’s disease is not clear. It is postulated that there could be a pathogenic mechanism involving molecular mimicry between yeast mannan and autoantibodies that may play a role in autoimmune diseases, such as anti-U2snRNP B*, although much research has to be done to confirm any cause and effect relationship between the presence of these autoantibodies directed against a molecule that is predominately found in Baker’s yeast [185].
Conclusion
Molds and fungi are ubiquitous and generally live in harmony with human beings. Only rare molds have been associated with human disease. The diseases that molds can cause are restricted to allergies, hypersensitivity pneumonitis and infection. There is no validity to the hype of “toxic black mold” and “mycotoxicosis.” Humans are not exposed to enough mycotoxins to develop illness, unless they ingest toxic quantities of mycotoxins or become exposed to intense organic dust storms.
With regard to sick building syndrome, it is highly probable that each building has its own unique microbiome with ever-varying combinations of bacterial, fungal, and chemical compounds that are likely to interact [15]. Sick building syndrome has been proven to be more about mass hysteria than any physiological illness. Fungi alone are almost certainly not responsible for the many health effects attributed to them, much less a single fungal species like S. chartarum.
References
Blackwell M (Mar 2011) The fungi: 1, 2, 3 ... 5.1 million species? Am J Bot 98(3):426–438
Tedersoo L, Bahram M, Ryberg M, Otsing E, Koljalg U, Abarenkov K (2014) Global biogeography of the ectomycorrhizal/sebacina lineage (fungi, Sebacinales) as revealed from comparative phylogenetic analyses. Mol Ecol 23(16):4168–4183
Eduard W (2009) Fungal spores: a critical review of the toxicological and epidemiological evidence as a basis for occupational exposure limit setting. Crit Rev Toxicol 39(10):799–864
Chew GL, Rogers C, Burge HA, Muilenberg ML, Gold DR (2003) Dustborne and airborne fungal propagules represent a different spectrum of fungi with differing relations to home characteristics. Allergy 58(1):13–20
Dallongeville A, Le Cann P, Zmirou-Navier D et al (2015) Concentration and determinants of molds and allergens in indoor air and house dust of French dwellings. Sci Total Environ 536:964–972
Dassonville C, Demattei C, Detaint B, Barral S, Bex-Capelle V, Momas I (2008) Assessment and predictors determination of indoor airborne fungal concentrations in Paris newborn babies’ homes. Environ Res 108(1):80–85
Rosenbaum PF, Crawford JA, Anagnost SE et al (2010) Indoor airborne fungi and wheeze in the first year of life among a cohort of infants at risk for asthma. J Expo Sci Environ Epidemiol 20(6):503–515
Simoni M, Cai GH, Norback D et al (2011) Total viable molds and fungal DNA in classrooms and association with respiratory health and pulmonary function of European schoolchildren. Pediatr Allergy Immunol 22(8):843–852
Green BJ, Sercombe JK, Tovey ER (2005) Fungal fragments and undocumented conidia function as new aeroallergen sources. J Allergy Clin Immunol 115(5):1043–1048
Brasel TL, Martin JM, Carriker CG, Wilson SC, Straus DC (2005) Detection of airborne Stachybotrys chartarum macrocyclic trichothecene mycotoxins in the indoor environment. Appl Environ Microbiol 71(11):7376–7388
Reponen T, Seo SC, Grimsley F, Lee T, Crawford C, Grinshpun SA (2007) Fungal fragments in moldy houses: a field study in homes in New Orleans and southern Ohio. Atmos Environ (1994) 41(37):8140–8149
Meklin T, Reponen T, McKinstry C et al (2007) Comparison of mold concentrations quantified by MSQPCR in indoor and outdoor air sampled simultaneously. Sci Total Environ 382(1):130–134
Lignell U, Meklin T, Rintala H et al (2008) Evaluation of quantitative PCR and culture methods for detection of house dust fungi and streptomycetes in relation to moisture damage of the house. Lett Appl Microbiol 47(4):303–308
Pitkaranta M, Meklin T, Hyvarinen A et al (2008) Analysis of fungal flora in indoor dust by ribosomal DNA sequence analysis, quantitative PCR, and culture. Appl Environ Microbiol 74(1):233–244
Pitkaranta M, Meklin T, Hyvarinen A et al (2011) Molecular profiling of fungal communities in moisture damaged buildings before and after remediation—a comparison of culture-dependent and culture-independent methods. BMC Microbiol 11:235
Crameri R (2011) The problem of cross-reactivity in the diagnosis of fungal allergy. Clin Exp Allergy 41(3):302–304
Green BJ, Tovey ER, Beezhold DH et al (2009) Surveillance of fungal allergic sensitization using the fluorescent halogen immunoassay. J Mycol Med 19(4):253–261
Beezhold DH, Green BJ, Blachere FM et al (2008) Prevalence of allergic sensitization to indoor fungi in West Virginia. Allergy Asthma Proc 29(1):29–34
Szewzyk R, Becker K, Hunken A, Pick-Fus H, Kolossa-Gehring M. Bundesumweltamt. Kinder-Umwelt-Survey (KUS) 2003/06. Sensibiliserungen Gegenuber Innenraumschimmelpilzen (German environmental survey for children 2003/06. Sensitization towards indoor molds). Dessau-Roblau, Germany. Bundesumweltamt (Federal Environment Agency). 2011.
Bousquet PJ, Chinn S, Janson C, Kogevinas M, Burney P, Jarvis D (2007) Geographical variation in the prevalence of positive skin tests to environmental aeroallergens in the European Community respiratory health survey I. Allergy 62(3):301–309
Chu LM, Rennie DC, Cockcroft DW et al (2014) Prevalence and determinants of atopy and allergic diseases among school-age children in rural Saskatchewan Canada. Ann Allergy Asthma Immunol. 113(4):430–439
Kespohl S, Maryska S, Zahradnik E, Sander I, Bruning T, Raulf-Heimsoth M (2013) Biochemical and immunological analysis of mould skin prick test solution: current status of standardization. Clin Exp Allergy 43(11):1286–1296
Chowdhary A, Agarwal K, Kathuria S, Gaur SN, Randhawa HS, Meis JF (2014) Allergic bronchopulmonary mycosis due to fungi other than Aspergillus: a global overview. Crit Rev Microbiol 40(1):30–48
WHO. Guidelines for indoor air quality. Dampness and mould. Copenhagen, Denmark 2009.
Denning DW, Pashley C, Hartl D et al (2014) Fungal allergy in asthma-state of the art and research needs. Clin Transl Allergy 4:14
Badiee P, Hashemizadeh Z (2014) Opportunistic invasive fungal infections: diagnosis & clinical management. Indian J Med Res 139(2):195–204
Vacher G, Niculita-Hirzel H, Roger T (2015) Immune responses to airborne fungi and non-invasive airway diseases. Semin Immunopathol 37(2):83–96
Montone KT, Livolsi VA, Feldman MD et al (2012) Fungal rhinosinusitis: a retrospective microbiologic and pathologic review of 400 patients at a single university medical center. Int J Otolaryngol 2012:684835
Quirce S, Vandenplas O, Campo P et al (2016) Occupational hypersensitivity pneumonitis: an EAACI position paper. Allergy 71(6):765–779
Silva CI, Churg A, Muller NL (2007) Hypersensitivity pneumonitis: spectrum of high-resolution CT and pathologic findings. AJR Am J Roentgenol 188(2):334–344
Selman M, Lacasse Y, Pardo A, Cormier Y (2010) Hypersensitivity pneumonitis caused by fungi. Proc Am Thorac Soc 7(3):229–236
Koschel D, Stark W, Karmann F, Sennekamp J, Muller-Wening D (Aug 2005) Extrinsic allergic alveolitis caused by misting fountains. Respir Med 99(8):943–947
Hanak V, Golbin JM, Ryu JH (2007) Causes and presenting features in 85 consecutive patients with hypersensitivity pneumonitis. Mayo Clin Proc 82(7):812–816
Chiba S, Okada S, Suzuki Y et al (2009) Cladosporium species-related hypersensitivity pneumonitis in household environments. Intern Med 48(5):363–367
Enriquez-Matas A, Quirce S, Hernandez E, Vereda A, Carnes J, Sastre J (2007) Hypersensitivity pneumonitis caused by domestic exposure to molds. J Investig Allergol Clin Immunol 17(2):126–127
Katayama N, Fujimura M, Yasui M, Ogawa H, Nakao S (2008) Hypersensitivity pneumonitis and bronchial asthma attacks caused by environmental fungi. Allergol Int 57(3):277–280
Ramirez RM, Jacobs RL (2014) Hypersensitivity pneumonitis by Fusarium vasinfectum in a home environment. J Allergy Clin Immunol Pract 2(4):483–484
Dickson SD, Tankersley MS (2015) Fatal hypersensitivity pneumonitis from exposure to Fusarium vasinfectum in a home environment: a case report. Int Arch Allergy Immunol 166(2):150–153
Kosmidis C, Denning DW (2015) The clinical spectrum of pulmonary aspergillosis. Thorax 70(3):270–277
Nucci M, Anaissie E (2007) Fusarium infections in immunocompromised patients. Clin Microbiol Rev 20(4):695–704
Bennett JW, Klich M (2003) Mycotoxins. Clin Microbiol Rev 16(3):497–516
Marin S, Ramos AJ, Cano-Sancho G, Sanchis V (2013) Mycotoxins: occurrence, toxicology, and exposure assessment. Food Chem Toxicol 60:218–237
Centers for Disease Control and Prevention (CDC) (2004) Outbreak of aflatoxin poisoning—eastern and central provinces, Kenya, January–July 2004. MMWR Morb Mortal Wkly Rep 53(34):790–793
Autrup JL, Schmidt J, Seremet T, Autrup H (1991) Determination of exposure to aflatoxins among Danish workers in animal-feed production through the analysis of aflatoxin B1 adducts to serum albumin. Scand J Work Environ Health 17(6):436–440
Viegas S, Veiga L, Almeida A, dos Santos M, Carolino E, Viegas C (2016) Occupational exposure to aflatoxin B1 in a Portuguese poultry slaughterhouse. Ann Occup Hyg. 60(2):176–183
Viegas S, Veiga L, Figueiredo P, Almeida A, Carolino E, Viegas C (2015) Assessment of workers’ exposure to aflatoxin B1 in a Portuguese waste industry. Ann Occup Hyg 59(2):173–181
Seifert SA, Von Essen S, Jacobitz K, Crouch R, Lintner CP (2003) Organic dust toxic syndrome: a review. J Toxicol Clin Toxicol 41(2):185–193
Madsen AM, Zervas A, Tendal K, Nielsen JL (2015) Microbial diversity in bioaerosol samples causing ODTS compared to reference bioaerosol samples as measured using Illumina sequencing and MALDI-TOF. Environ Res 140:255–267
Institute of Medicine (US) Committee on Damp Indoor Spaces and Health (2004) Damp indoor spaces and health. National Academies Press (US), Washington, DC
Bornehag CG, Blomquist G, Gyntelberg F et al (2001) Dampness in buildings and health. Nordic interdisciplinary review of the scientific evidence on associations between exposure to “dampness” in buildings and health effects (NORDDAMP). Indoor Air 11(2):72–86
Bornehag CG, Sundell J, Bonini S et al (2004) Dampness in buildings as a risk factor for health effects, EUROEXPO: a multidisciplinary review of the literature (1998–2000) on dampness and mite exposure in buildings and health effects. Indoor Air 14(4):243–257
Bornehag CG, Sundell J, Sigsgaard T (2004) Dampness in buildings and health (DBH): report from an ongoing epidemiological investigation on the association between indoor environmental factors and health effects among children in Sweden. Indoor Air 14(Suppl 7):59–66
Mendell MJ, Mirer AG, Cheung K, Tong M, Douwes J (2011) Respiratory and allergic health effects of dampness, mold, and dampness-related agents: a review of the epidemiologic evidence. Environ Health Perspect 119(6):748–756
Sahlberg B, Gunnbjornsdottir M, Soon A et al (2013) Airborne molds and bacteria, microbial volatile organic compounds (MVOC), plasticizers and formaldehyde in dwellings in three north European cities in relation to sick building syndrome (SBS). Sci Total Environ 444:433–440
Verhoeff AP, van Reenen-Hoekstra ES, Samson RA, Brunekreef B, van Wijnen JH (1994) Fungal propagules in house dust. I. Comparison of analytic methods and their value as estimators of potential exposure. Allergy 49(7):533–539
Verhoeff AP, van Wijnen JH, Brunekreef B, Fischer P, van Reenen-Hoekstra ES, Samson RA (1992) Presence of viable mould propagules in indoor air in relation to house damp and outdoor air. Allergy 47(2 Pt 1):83–91
Verhoeff AP, van Wijnen JH, van Reenen-Hoekstra ES, Samson RA, van Strien RT, Brunekreef B (1994) Fungal propagules in house dust. II. Relation with residential characteristics and respiratory symptoms. Allergy 49(7):540–547
Holme J, Hagerhed-Engman L, Mattsson J, Sundell J, Bornehag CG (2010) Culturable mold in indoor air and its association with moisture-related problems and asthma and allergy among Swedish children. Indoor Air 20(4):329–340
Muller A, Lehmann I, Seiffart A et al (2002) Increased incidence of allergic sensitisation and respiratory diseases due to mould exposure: results of the Leipzig allergy risk children study (LARS). Int J Hyg Environ Health 204(5–6):363–365
Ren P, Jankun TM, Belanger K, Bracken MB, Leaderer BP (2001) The relation between fungal propagules in indoor air and home characteristics. Allergy 56(5):419–424
Choi H, Byrne S, Larsen LS et al (2014) Residential culturable fungi, (1-3, 1-6)-beta-d-glucan, and ergosterol concentrations in dust are not associated with asthma, rhinitis, or eczema diagnoses in children. Indoor Air 24(2):158–170
Leppanen HK, Nevalainen A, Vepsalainen A et al (2014) Determinants, reproducibility, and seasonal variation of ergosterol levels in house dust. Indoor Air 24(3):248–259
Park JH, Cox-Ganser JM, Kreiss K, White SK, Rao CY (2008) Hydrophilic fungi and ergosterol associated with respiratory illness in a water-damaged building. Environ Health Perspect 116(1):45–50
Vesper SJ, McKinstry C, Yang C et al (2006) Specific molds associated with asthma in water-damaged homes. J Occup Environ Med 48(8):852–858
Vesper SJ, Varma M, Wymer LJ, Dearborn DG, Sobolewski J, Haugland RA (2004) Quantitative polymerase chain reaction analysis of fungi in dust from homes of infants who developed idiopathic pulmonary hemorrhaging. J Occup Environ Med 46(6):596–601
Chew GL, Douwes J, Doekes G et al (2001) Fungal extracellular polysaccharides, beta (1-->3)-glucans and culturable fungi in repeated sampling of house dust. Indoor Air 11(3):171–178
Madureira J, Paciencia I, Cavaleiro-Rufo J, Fernandes EO (2016) Indoor air risk factors for schoolchildren’s health in Portuguese homes: results from a case-control survey. J Toxicol Environ Health A. 79(20):938–953
Mendes A, Papoila AL, Carreiro-Martins P et al (2016) The impact of indoor air quality and contaminants on respiratory health of older people living in long-term care residences in Porto. Age Ageing 45(1):136–142
Celtik C, Okten S, Okutan O et al (2011) Investigation of indoor molds and allergic diseases in public primary schools in Edirne city of Turkey. Asian Pac J Allergy Immunol 29(1):42–49
Holst GJ, Host A, Doekes G et al (2016) Allergy and respiratory health effects of dampness and dampness-related agents in schools and homes: a cross-sectional study in Danish pupils. Indoor Air 26(6):880–891
Jacobs J, Borras-Santos A, Krop E et al (2014) Dampness, bacterial and fungal components in dust in primary schools and respiratory health in schoolchildren across Europe. Occup Environ Med 71(10):704–712
Tischer C, Zock JP, Valkonen M et al (2015) Predictors of microbial agents in dust and respiratory health in the Ecrhs. BMC Pulm Med 15:48
Saijo Y, Kanazawa A, Araki A et al (2011) Relationships between mite allergen levels, mold concentrations, and sick building syndrome symptoms in newly built dwellings in Japan. Indoor Air 21(3):253–263
Bundy KW, Gent JF, Beckett W et al (2009) Household airborne Penicillium associated with peak expiratory flow variability in asthmatic children. Ann Allergy Asthma Immunol. 103(1):26–30
Cai GH, Hashim JH, Hashim Z et al (2011) Fungal DNA, allergens, mycotoxins and associations with asthmatic symptoms among pupils in schools from Johor Bahru, Malaysia. Pediatr Allergy Immunol 22(3):290–297
Norback D, Hashim JH, Markowicz P et al (2016) Endotoxin, ergosterol, muramic acid and fungal DNA in dust from schools in Johor Bahru, Malaysia—associations with rhinitis and sick building syndrome (SBS) in junior high school students. Sci Total Environ 545-546:95–103
Norback D, Hashim JH, Cai GH et al (2016) Rhinitis, ocular, throat and dermal symptoms, headache and tiredness among students in schools from Johor Bahru, Malaysia: associations with fungal DNA and mycotoxins in classroom dust. PLoS One 11(2):e0147996
LeBouf R, Yesse L, Rossner A (2008) Seasonal and diurnal variability in airborne mold from an indoor residential environment in northern New York. J Air Waste Manag Assoc. 58(5):684–692
Mentese S, Rad AY, Arisoy M, Gullu G (2012) Multiple comparisons of organic, microbial, and fine particulate pollutants in typical indoor environments: diurnal and seasonal variations. J Air Waste Manag Assoc 62(12):1380–1393
Su HJ, Wu PC, Chen HL, Lee FC, Lin LL (Feb 2001) Exposure assessment of indoor allergens, endotoxin, and airborne fungi for homes in southern Taiwan. Environ Res 85(2):135–144
Kaarakainen P, Rintala H, Vepsalainen A, Hyvarinen A, Nevalainen A, Meklin T (2009) Microbial content of house dust samples determined with qPCR. Sci Total Environ 407(16):4673–4680
Cho SJ, Ramachandran G, Grengs J, Ryan AD, Eberly LE, Adgate JL (2008) Longitudinal evaluation of allergen and culturable fungal concentrations in inner-city households. J Occup Environ Hyg 5(2):107–118
Heinrich J, Holscher B, Douwes J et al (2003) Reproducibility of allergen, endotoxin and fungi measurements in the indoor environment. J Expo Anal Environ Epidemiol 13(2):152–160
Spicer R, Gangloff H (2005) Establishing site specific reference levels for fungi in outdoor air for building evaluation. J Occup Environ Hyg 2(5):257–266
Makkonen K, Viitala KI, Parkkila S, Niemela O (2001) Serum IgG and IgE antibodies against mold-derived antigens in patients with symptoms of hypersensitivity. Clin Chim Acta 305(1–2):89–98
Hyvarinen A, Husman T, Laitinen S et al (May 2003) Microbial exposure and mold-specific serum IgG levels among children with respiratory symptoms in 2 school buildings. Arch Environ Health 58(5):275–283
Immonen J, Laitinen S, Taskinen T, Pekkanen J, Nevalainen A, Korppi M (2002) Mould-specific immunoglobulin G antibodies in students from moisture- and mould-damaged schools: a 3-year follow-up study. Pediatr Allergy Immunol 13(2):125–128
Taskinen TM, Laitinen S, Nevalainen A et al (2002) Immunoglobulin G antibodies to moulds in school-children from moisture problem schools. Allergy 57(1):9–16
Mussalo-Rauhamaa H, Nikulin M, Koukila-Kahkola P, Hintikka EL, Malmberg M, Haahtela T (2010) Health effects of residents exposed to Stachybotrys in water-damaged houses in Finland. Indoor Built Environ 19(4):476–485
Brauer C, Budtz-Jorgensen E, Mikkelsen S (2008) Structural equation analysis of the causal relationship between health and perceived indoor environment. Int Arch Occup Environ Health 81(6):769–776
Brauer C, Kolstad H, Orbaek P, Mikkelsen S (2006) The sick building syndrome: a chicken and egg situation? Int Arch Occup Environ Health 79(6):465–471
Brodie EL, DeSantis TZ, Parker JP, Zubietta IX, Piceno YM, Andersen GL (2007) Urban aerosols harbor diverse and dynamic bacterial populations. Proc Natl Acad Sci U S A 104(1):299–304
Rintala H, Pitkaranta M, Toivola M, Paulin L, Nevalainen A (2008) Diversity and seasonal dynamics of bacterial community in indoor environment. BMC Microbiol 8:56
Schleibinger H, Laussmann D, Bornehag CG, Eis D, Rueden H (2008) Microbial volatile organic compounds in the air of moldy and mold-free indoor environments. Indoor Air 18(2):113–124
Markowicz P, Larsson L (2015) Influence of relative humidity on VOC concentrations in indoor air. Environ Sci Pollut Res Int 22(8):5772–5779
Korpi A, Jarnberg J, Pasanen AL (2009) Microbial volatile organic compounds. Crit Rev Toxicol 39(2):139–193
Lorentzen JC, Juran SA, Nilsson M, Nordin S, Johanson G (2016) Chloroanisoles may explain mold odor and represent a major indoor environment problem in Sweden. Indoor Air 26(2):207–218
Dennison JE, Bigelow PL, Mumtaz MM, Andersen ME, Dobrev ID, Yang RS (2005) Evaluation of potential toxicity from co-exposure to three CNS depressants (toluene, ethylbenzene, and xylene) under resting and working conditions using PBPK modeling. J Occup Environ Hyg 2(3):127–135
Silva E, Rajapakse N, Kortenkamp A (2002) Something from “nothing”—eight weak estrogenic chemicals combined at concentrations below NOECs produce significant mixture effects. Environ Sci Technol 36(8):1751–1756
Huttunen K, Pelkonen J, Nielsen KF, Nuutinen U, Jussila J, Hirvonen MR (2004) Synergistic interaction in simultaneous exposure to Streptomyces californicus and Stachybotrys chartarum. Environ Health Perspect 112(6):659–665
Murtoniemi T, Penttinen P, Nevalainen A, Hirvonen MR (2005) Effects of microbial cocultivation on inflammatory and cytotoxic potential of spores. Inhal Toxicol 17(12):681–693
Yli-Pirila T, Huttunen K, Nevalainen A, Seuri M, Hirvonen MR (2007) Effects of co-culture of amoebae with indoor microbes on their cytotoxic and proinflammatory potential. Environ Toxicol 22(4):357–367
Penttinen P, Huttunen K, Pelkonen J, Hirvonen MR (2005) The proportions of Streptomyces californicus and Stachybotrys chartarum in simultaneous exposure affect inflammatory responses in mouse RAW264.7 macrophages. Inhal Toxicol 17(2):79–85
Penttinen P, Pelkonen J, Huttunen K, Hirvonen MR (2006) Co-cultivation of Streptomyces californicus and Stachybotrys chartarum stimulates the production of cytostatic compound(s) with immunotoxic properties. Toxicol Appl Pharmacol 217(3):342–351
Penttinen P, Pelkonen J, Huttunen K, Toivola M, Hirvonen MR (2005) Interactions between Streptomyces californicus and Stachybotrys chartarum can induce apoptosis and cell cycle arrest in mouse RAW264.7 macrophages. Toxicol Appl Pharmacol 202(3):278–288
1994) Acute pulmonary hemorrhage/hemosiderosis among infants—Cleveland, January 1993–November 1994. MMWR Morb Mortal Wkly Rep 43(48):881–883
2000) Update: pulmonary hemorrhage/hemosiderosis among infants—Cleveland, Ohio, 1993–1996. MMWR Morb Mortal Wkly Rep 49(9):180–184
Edmondson DA, Nordness ME, Zacharisen MC, Kurup VP, Fink JN (2005) Allergy and “toxic mold syndrome”. Ann Allergy Asthma Immunol. 94(2):234–239
Khalili B, Montanaro MT, Bardana EJ Jr (2005) Inhalational mold toxicity: fact or fiction? A clinical review of 50 cases. Ann Allergy Asthma Immunol 95(3):239–246
Hong SB, Lee M, Kim DH, Chung SH, Shin HD, Samson RA (2013) The proportion of non-aflatoxigenic strains of the Aspergillus flavus/oryzae complex from meju by analyses of the aflatoxin biosynthetic genes. J Microbiol 51(6):766–772
Panaccione DG, Coyle CM (2005) Abundant respirable ergot alkaloids from the common airborne fungus Aspergillus fumigatus. Appl Environ Microbiol 71(6):3106–3111
Razzaghi-Abyaneh M, Shams-Ghahfarokhi M, Allameh A et al (2006) A survey on distribution of Aspergillus section Flavi in corn field soils in Iran: population patterns based on aflatoxins, cyclopiazonic acid and sclerotia production. Mycopathologia 161(3):183–192
Andersen B, Nielsen KF, Jarvis BB (2002) Characterization of Stachybotrys from water-damaged buildings based on morphology, growth, and metabolite production. Mycologia 94(3):392–403
Andersen B, Nielsen KF, Thrane U, Szaro T, Taylor JW, Jarvis BB (2003) Molecular and phenotypic descriptions of Stachybotrys chlorohalonata sp. nov. and two chemotypes of Stachybotrys chartarum found in water-damaged buildings. Mycologia 95(6):1227–1238
Engelhart S, Loock A, Skutlarek D et al (2002) Occurrence of toxigenic Aspergillus versicolor isolates and sterigmatocystin in carpet dust from damp indoor environments. Appl Environ Microbiol 68(8):3886–3890
Calvo AM, Wilson RA, Bok JW, Keller NP (2002) Relationship between secondary metabolism and fungal development. Microbiol Mol Biol Rev 66(3):447–459
Skaug MA, Eduard W, Stormer FC (2001) Ochratoxin A in airborne dust and fungal conidia. Mycopathologia 151(2):93–98
Sorenson WG, Frazer DG, Jarvis BB, Simpson J, Robinson VA (1987) Trichothecene mycotoxins in aerosolized conidia of Stachybotrys atra. Appl Environ Microbiol 53(6):1370–1375
Gareis M, Gottschalk C (Aug 2014) Stachybotrys spp. and the guttation phenomenon. Mycotoxin Res 30(3):151–159
Bellanger AP, Reboux G, Roussel S et al (2009) Indoor fungal contamination of moisture-damaged and allergic patient housing analysed using real-time PCR. Lett Appl Microbiol 49(2):260–266
Shelton BG, Kirkland KH, Flanders WD, Morris GK (2002) Profiles of airborne fungi in buildings and outdoor environments in the United States. Appl Environ Microbiol 68(4):1743–1753
Chew GL, Wilson J, Rabito FA et al (2006) Mold and endotoxin levels in the aftermath of hurricane Katrina: a pilot project of homes in New Orleans undergoing renovation. Environ Health Perspect 114(12):1883–1889
Bloom E, Grimsley LF, Pehrson C, Lewis J, Larsson L (2009) Molds and mycotoxins in dust from water-damaged homes in New Orleans after hurricane Katrina. Indoor Air 19(2):153–158
Iossifova Y, Reponen T, Sucharew H, Succop P, Vesper S (2008) Use of (1-3)-beta-d-glucan concentrations in dust as a surrogate method for estimating specific fungal exposures. Indoor Air 18(3):225–232
Hardin BD, Robbins CA, Fallah P, Kelman BJ (2009) The concentration of no toxicologic concern (CoNTC) and airborne mycotoxins. J Toxicol Environ Health A 72(9):585–598
Gottschalk C, Bauer J, Meyer K (2008) Detection of satratoxin G and H in indoor air from a water-damaged building. Mycopathologia 166(2):103–107
Pottier D, Andre V, Rioult JP, Bourreau A, Duhamel C, Bouchart VK (2014) Airborne molds and mycotoins in Serpula lacrymans-damaged homes. Atmos Pollut Res 5(2):325–334
Polizzi V, Delmulle B, Adams A et al (2009) JEM spotlight: fungi, mycotoxins and microbial volatile organic compounds in mouldy interiors from water-damaged buildings. J Environ Monit 11(10):1849–1858
Bloom E, Bal K, Nyman E, Must A, Larsson L (2007) Mass spectrometry-based strategy for direct detection and quantification of some mycotoxins produced by Stachybotrys and Aspergillus spp. in indoor environments. Appl Environ Microbiol 73(13):4211–4217
Degen H (2011) Tools for investigating workplace-related risks from mycotoxin exposure. World Mycotoxin J 4(3):315–327
Mo X, Lai H, Yang Y et al (2014) How does airway exposure of aflatoxin B1 affect serum albumin adduct concentrations? Evidence based on epidemiological study and animal experimentation. J Toxicol Sci 39(4):645–653
Viegas S, Veiga L, Malta-Vacas J et al (2012) Occupational exposure to aflatoxin (AFB (1)) in poultry production. J Toxicol Environ Health A. 75(22–23):1330–1340
Yike I, Distler AM, Ziady AG, Dearborn DG (2006) Mycotoxin adducts on human serum albumin: biomarkers of exposure to Stachybotrys chartarum. Environ Health Perspect 114(8):1221–1226
Amuzie CJ, Harkema JR, Pestka JJ (2008) Tissue distribution and proinflammatory cytokine induction by the trichothecene deoxynivalenol in the mouse: comparison of nasal vs. oral exposure. Toxicology 248(1):39–44
Creasia DA, Thurman JD, Jones LJ (1987) 3rd, et al. acute inhalation toxicity of T-2 mycotoxin in mice. Fundam Appl Toxicol 8(2):230–235
Creasia DA, Thurman JD, Wannemacher RW Jr, Bunner DL (1990) Acute inhalation toxicity of T-2 mycotoxin in the rat and guinea pig. Fundam Appl Toxicol 14(1):54–59
Coulombe RA Jr, Sharma RP (1985) Clearance and excretion of intratracheally and orally administered aflatoxin B1 in the rat. Food Chem Toxicol 23(9):827–830
Kelman BJ, Robbins CA, Swenson LJ, Hardin BD (2004) Risk from inhaled mycotoxins in indoor office and residential environments. Int J Toxicol 23(1):3–10
Hardin BD, Kelman BJ, Saxon A (2003) Adverse human health effects associated with molds in the indoor environment. J Occup Environ Med 45(5):470–478
Flemming J, Hudson B, Rand TG (2004) Comparison of inflammatory and cytotoxic lung responses in mice after intratracheal exposure to spores of two different Stachybotrys chartarum strains. Toxicol Sci 78(2):267–275
Rosenblum Lichtenstein JH, Molina RM, Donaghey TC et al (2016) Repeated mouse lung exposures to Stachybotrys chartarum shift immune response from type 1 to type 2. Am J Respir Cell Mol Biol 55(4):521–531
Hudson B, Flemming J, Sun G, Rand TG (2005) Comparison of immunomodulator mRNA and protein expression in the lungs of Stachybotrys chartarum spore-exposed mice. J Toxicol Environ Health A. 68(15):1321–1335
Leino M, Makela M, Reijula K et al (2003) Intranasal exposure to a damp building mould, Stachybotrys chartarum, induces lung inflammation in mice by satratoxin-independent mechanisms. Clin Exp Allergy 33(11):1603–1610
Yaniv G, Twig G, Shor DB et al (2015) A volcanic explosion of autoantibodies in systemic lupus erythematosus: a diversity of 180 different antibodies found in SLE patients. Autoimmun Rev 14(1):75–79
Seldin MF (2015) The genetics of human autoimmune disease: a perspective on progress in the field and future directions. J Autoimmun 64:1–12
Teruel M, Alarcon-Riquelme ME (2016) The genetic basis of systemic lupus erythematosus: what are the risk factors and what have we learned. J Autoimmun 74:161–175
Zhang Z, Zhang R (2015) Epigenetics in autoimmune diseases: pathogenesis and prospects for therapy. Autoimmun Rev 14(10):854–863
Pollock RA, Abji F, Gladman DD. Epigenetics of psoriatic disease: a systematic review and critical appraisal. J Autoimmun. 2016.
Wu H, Zhao M, Tan L, Lu Q (2016) The key culprit in the pathogenesis of systemic lupus erythematosus: aberrant DNA methylation. Autoimmun Rev 15(7):684–689
Floreani A, Leung PS, Gershwin ME (2016) Environmental basis of autoimmunity. Clin Rev Allergy Immunol 50(3):287–300
Wu H, Zhao M, Yoshimura A, Chang C, Lu Q (2016) Critical link between epigenetics and transcription factors in the induction of autoimmunity: a comprehensive review. Clin Rev Allergy Immunol. 50(3):333–344
Shu Y, Hu Q, Long H, Chang C, Lu Q, Xiao R. Epigenetic Variability of CD4+CD25+ Tregs contributes to the pathogenesis of autoimmune diseases. Clin Rev Allergy Immunol. 2016.
Bao Y, Cao X (2016) Epigenetic control of B cell development and B cell-related immune disorders. Clin Rev Allergy Immunol. 50(3):301–311
Selmi C (2016) Autoimmunity in 2015. Clin Rev Allergy Immunol. 51(1):110–119
Hirschfield GM, Siminovitch KA (2015) Genetics in PBC: what do the “risk genes” teach us? Clin Rev Allergy Immunol. 48(2–3):176–181
Qian Y, Culton DA, Jeong JS, Trupiano N, Valenzuela JG, Diaz LA (2016) Non-infectious environmental antigens as a trigger for the initiation of an autoimmune skin disease. Autoimmun Rev 15(9):923–930
Kadowaki A, Miyake S, Saga R, Chiba A, Mochizuki H, Yamamura T (2016) Gut environment-induced intraepithelial autoreactive CD4(+) T cells suppress central nervous system autoimmunity via LAG-3. Nat Commun 7:11639
Onuora S (2016) Autoimmunity: human gut bacteria induce TH17 cells. Nat Rev Rheumatol 13(1):2
Shamriz O, Mizrahi H, Werbner M, Shoenfeld Y, Avni O, Koren O (2016) Microbiota at the crossroads of autoimmunity. Autoimmun Rev 15(9):859–869
Dwivedi M, Kumar P, Laddha NC, Kemp EH (2016) Induction of regulatory T cells: a role for probiotics and prebiotics to suppress autoimmunity. Autoimmun Rev 15(4):379–392
Uusitalo U, Liu X, Yang J et al (2016) Association of early exposure of probiotics and islet autoimmunity in the TEDDY study. JAMA Pediatr 170(1):20–28
Tomer Y, Dolan LM, Kahaly G et al (2015) Genome wide identification of new genes and pathways in patients with both autoimmune thyroiditis and type 1 diabetes. J Autoimmun 60:32–39
Webb GJ, Hirschfield GM (2016) Using GWAS to identify genetic predisposition in hepatic autoimmunity. J Autoimmun 66:25–39
Jeltsch-David H, Muller S (2016) Autoimmunity, neuroinflammation, pathogen load: a decisive crosstalk in neuropsychiatric SLE. J Autoimmun 74:13–26
Onuora S (2016) Autoimmunity: TFH cells link gut microbiota and arthritis. Nat Rev Rheumatol 12(3):133
Zhu Y, Zou L, Liu YC (2016) T follicular helper cells, T follicular regulatory cells and autoimmunity. Int Immunol 28(4):173–179
Audia S, Rossato M, Trad M et al (2017) B cell depleting therapy regulates splenic and circulating T follicular helper cells in immune thrombocytopenia. J Autoimmun 77:89–95
Doherty DG (2016) Immunity, tolerance and autoimmunity in the liver: a comprehensive review. J Autoimmun 66:60–75
Yang CA, Chiang BL (2015) Inflammasomes and human autoimmunity: a comprehensive review. J Autoimmun 61:1–8
Franks SE, Getahun A, Hogarth PM, Cambier JC (2016) Targeting B cells in treatment of autoimmunity. Curr Opin Immunol 43:39–45
Domeier PP, Chodisetti SB, Soni C et al (2016) IFN-gamma receptor and STAT1 signaling in B cells are central to spontaneous germinal center formation and autoimmunity. J Exp Med 213(5):715–732
Thompson G, John M, Chopra A (2016) Triple threats: tracking antigen-specific T cells in a case of concurrent autoimmunity, infectious disease and possible malignancy. Pathology 48(Suppl 1):S44
Anderson AC, Sullivan JM, Tan DJ, Lee DH, Kuchroo VK (2015) A T cell extrinsic mechanism by which IL-2 dampens Th17 differentiation. J Autoimmun 59:38–42
Hou L, Cooley J, Swanson R et al (2015) The protease cathepsin L regulates Th17 cell differentiation. J Autoimmun 65:56–63
Hou MS, Huang ST, Tsai MH et al (2015) The interleukin-15 system suppresses T cell-mediated autoimmunity by regulating negative selection and nT (H)17 cell homeostasis in the thymus. J Autoimmun 56:118–129
Hua C, Audo R, Yeremenko N et al (2016) A proliferation inducing ligand (APRIL) promotes IL-10 production and regulatory functions of human B cells. J Autoimmun 73:64–72
Isailovic N, Daigo K, Mantovani A, Selmi C (2015) Interleukin-17 and innate immunity in infections and chronic inflammation. J Autoimmun 60:1–11
Jones SA, Perera DN, Fan H, Russ BE, Harris J, Morand EF (2015) GILZ regulates Th17 responses and restrains IL-17-mediated skin inflammation. J Autoimmun 61:73–80
Lu X, Tang Q, Lindh M, et al. The host defense peptide LL-37 a possible inducer of the type I interferon system in patients with polymyositis and dermatomyositis. J Autoimmun. 2016.
Barbati C, Alessandri C, Vomero M et al (2015) Autoantibodies specific to D4GDI modulate rho GTPase mediated cytoskeleton remodeling and induce autophagy in T lymphocytes. J Autoimmun 58:78–89
Leventhal JS, Ross MJ (2016) LAPping up dead cells to prevent lupus nephritis: a novel role for noncanonical autophagy in autoimmunity. Kidney Int 90(2):238–239
Gray MR, Thrasher JD, Crago R et al (2003) Mixed mold mycotoxicosis: immunological changes in humans following exposure in water-damaged buildings. Arch Environ Health 58(7):410–420
Borchers AT, Gershwin ME (Oct 2015) Fibromyalgia: a critical and comprehensive review. Clin Rev Allergy Immunol. 49(2):100–151
Rinaldi M, Perricone R, Blank M, Perricone C, Shoenfeld Y (2013) Anti-Saccharomyces cerevisiae autoantibodies in autoimmune diseases: from bread baking to autoimmunity. Clin Rev Allergy Immunol. 45(2):152–161
Bloom E, Bal K, Nyman E, Larsson L (2007) Optimizing a GC-MS method for screening of Stachybotrys mycotoxins in indoor environments. J Environ Monit 9(2):151–156
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Borchers, A.T., Chang, C. & Eric Gershwin, M. Mold and Human Health: a Reality Check. Clinic Rev Allerg Immunol 52, 305–322 (2017). https://doi.org/10.1007/s12016-017-8601-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-017-8601-z