Abstract
With the advancements in the field of adult stem and progenitor cells grows the recognition that the motility of primitive cells is a pivotal aspect of their functionality. There is accumulating evidence that the recruitment of tissue-resident and circulating cells is critical for organ homeostasis and effective injury responses, whereas the pathobiology of degenerative diseases, neoplasm and aging, might be rooted in the altered ability of immature cells to migrate. Furthermore, understanding the biological machinery determining the translocation patterns of tissue progenitors is of great relevance for the emerging methodologies for cell-based therapies and regenerative medicine. The present article provides an overview of studies addressing the physiological significance and diverse modes of stem and progenitor cell trafficking in adult mammalian organs, discusses the major microenvironmental cues regulating cell migration, and describes the implementation of live imaging approaches for the exploration of stem cell movement in tissues and the factors dictating the motility of endogenous and transplanted cells with regenerative potential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Orchestrated movement of cells is fundamental for the organ development, postnatal growth and adequate performance at the different stages of adulthood. For many years, the complex pathways regulating cell migration in the physiology of adult organism and with various pathologies are subject matters of intense investigations [1–4], https://www.cellmigration.org/science/. Yet, the journey to uncover the mechanisms controlling the directional translocation of tissue-specific stem and progenitor cells and the importance of immature cell trafficking for organ homeostasis and repair is at the exciting beginning.
It is postulated that in order to preserve organ integrity, the adult tissue-specific primitive stem cells or their undifferentiated progeny [5] migrate to the sites of tissue repair, compensating for the “wear and tear” or supporting the wound healing [4, 6–9]. Consequently, along with the potency to generate cells of diverse lineages and capacity for self-renewal, cell motility is a vital property of stem and progenitor cells, which evidently changes with pathologies and aging. Hence, the knowledge of the pathways that guide the immature cell trafficking is essential for elucidating the origins and evolution of diseases in stem-cell regulated organs. Moreover, the targeted movement of transplanted cells from the sites of administration to the foci of injury is key for the success of cell-based regenerative treatments [10–12].
The research into the mechanisms of adult stem cell migration has evolved in the course of the past decade as a result of cumulative efforts to better understand the intricate nature of stem cell behavior and augment its function in therapeutic purposes. This review, dedicated to mammalian stem and progenitor cells, describes documented examples and biological relevance of the immature cell movement in adult organs, examines the implications of the alterations in stem cell motility, and summarizes the recognized features of the primitive cell environment that govern the migratory responses. Additionally, the use of live imaging is discussed as a compelling tool for the studies of stem cell migratory activity in vitro and in vivo.
Biological Significance of the Stem and Progenitor Cell Movement in Adult Tissues
The most studied manifestation of the adult mammalian stem cell migration is the trafficking of hematopoietic stem and progenitor cells between the bone marrow, blood circulation and peripheral organs (for comprehensive reviews on the hematopoietic stem cell trafficking, see [7, 13–20]). In adults, the primitive hematopoietic cells reside in specialized bone marrow niches (the concept of bone marrow niches was recently reviewed in [8, 21–24]). It is established that the immature cells of the hematopoietic system constantly emigrate from and return to the bone marrow [25–27]. For instance, the circadian rhythm creates cycles of the hematopoietic progenitor cell mobilization to the blood, with maximal cell release during the resting period [28–30], which presumably occurs in the absence of injury in purpose of homeostatic surveillance of peripheral tissues by stem cells. Furthermore, plethora of stresses, such as inflammation or damage to distant organs, significantly increases the numbers of circulating progenitors [18, 31, 32]. These emergency responses by undifferentiated hematopoietic cells have been observed after trauma and hemorrhagic shock [33], wounding of the liver [34, 35], stroke [36], and myocardial infarction [37, 38]. Remarkably, even following infusion into the bloodstream, the transplanted hematopoietic stem and progenitors exhibit tropism towards the host bone marrow and are capable of engrafting into the supporting niches. The astonishing migratory ability of immature hematopoietic cells is widely employed in everyday clinical practices for the bone marrow transplantation in patients with hematological malignancies, as well as novel therapies for regenerative medicine [39–42].
Another well-known process of the stem cell movement in adult organs involves stem cell emigration from the storage niches as a step in their differentiation program. For example, the intestinal epithelial stem cells are situated at or near the bottom of crypts formed by the convolution of the epithelial sheet, where stem cells proliferate and give rise to progenitor cells. While moving to ascend the crypt axis, the stem cell progeny divide and further mature, acquiring terminally differentiated phenotype (recently reviewed in [5, 43–46]). Multiple studies have demonstrated that proper communication of the primitive intestinal cells with their microenvironment is essential for the prevention of unrestrained growth and development of neoplasms [47–50]. In this regard, it was found that the abnormalities in signal transduction pathways involved in the immature cell migration contribute to tumorigenesis at all stages of intestinal cancer [51].
The different populations of primitive cell types in the skin also leave their specialized niches located in the hair follicles, basal layer of interfollicular epidermis, and other skin compartments, in order to differentiate and participate in the tissue maintenance cycles and wound re-epithelization (for recent reviews on the skin stem cells, see [52–58]). Specifically, it is described that in the basal layer of the epidermis, the progenitor cells, or their transient-amplifying progeny, detach from the underlying basement membrane and migrate towards the skin outmost layer. Their movement is accompanied by progressive maturation. Unlike the epidermis, which regenerates continuously, the hair follicles undergo cycles of growth, degeneration and rest. The position of primitive cells in the bulge of the hair follicle and hair germ region is strictly controlled, and shifts in their placement relative to other cells affect the lineage commitment and self-renewal potential. Importantly, after skin wounding, cells from both the hair follicles and interfollicular epidermis migrate to the site of tissue damage [59–63]. Of interest, there is evidence that the activity of telomerase promotes the egress of stem cells from hair follicles in response to chemical injury, whereas telomerase deficiency interferes with the stem cell recruitment, and might constitute a mechanism for prevention of skin cancers in old tissues [64]. Also the melanocyte stem cells, which are normally present in the hair follicle, exit from the bulge when the skin is wounded or exposed to UV-radiation, partaking in the re-pigmentation and renewal of the epidermis. It is suggested that in these conditions the stem cell emigration is not compensated by proliferation, which might lead to melanocyte stem cell depletion and deficient injury repair [65].
The immature cells of the skeletal muscle are likewise required to migrate for tissue maintenance and regeneration. The dedicated muscle stem cells, often referred as satellite cells, are maintained in a quiescent state in the supporting niches, localized between the sarcolemma of myofibers and surrounding basal lamina. Growth-promoting stimuli or muscle injury induce satellite cell activation, egress from the niches, commitment to differentiation and movement towards the target site, where the myogenic progenitors align in preparation for the cell-cell fusion into muscle fibers (diverse aspects of the satellite cell biology are reviewed in [5, 66–73]). Sub-optimal migration of the immature myogenic cells and lack of proper alignment prior to fusion hinder the organ’s ability to correctly repair the damage [74], and are speculated to contribute to the etiology of muscular dystrophy [75] and aging [76].
Further, the immature neurogenic cells in the central nervous system also have to leave their birthplace in order to differentiate, reach the target locations, and appropriately integrate into the neural network. In the adult brain, a category of neural stem cells is reported to occupy the neurogenic niches concentrated in the subventricular zone adjacent to the lateral ventricles, and the subgranular zone within the hippocampal dentate gyrus (detailed reviews of the adult neural stem cells and their niches are provided in [6, 7, 77–80]). In the subventricular zone, activated neural stem cells give rise to transiently amplifying progenitors, which, in turn, become neuroblasts. Neuroblasts collectively migrate rostrally into olfactory bulb, where they change the type of movement to radial and then terminally differentiate. The primitive cells in subgranular zone also produce progenitors that generate neuroblasts, which disperse into the granule cell layer and complete the differentiation there. Conceivably, the aberrant translocation of primitive cells is associated with neuropathology [78, 79, 81, 82]. For example, the traumatic brain injury alters the movement of adult-born neurons in the hippocampus [83], while progressive reduction in the neuroblast migration with aging limits the maturation and lineage-commitment of newly-generated neurons, and might be causative of the senescence-related neurological impairments [84]. Additionally, there are documentations that when transplanted at a locus distant from a brain lesion, cells with the properties of neural progenitors migrate to the injured area [85–87]; and methodologies are considered for cell-replacement therapies with neurogenic cells to ameliorate neurodegenerative diseases and stroke (the challenges and future directions in this field are discussed in [87–90]).
Thus, the motility of stem and progenitor cells in adult organs is crucial for the preservation of tissue health and functionality, and, potentially, for the success of cell-based regenerative approaches.
Molecular Mechanisms Involved in Stem and Progenitor Cell Trafficking
The movement of cells in tissues is a combinatorial outcome of multiple signaling inputs from the cell close surroundings and the remote sites. The stem cell niches, that is functional units of the stem cell maintenance and activation, are proposed to dictate the responses of the primitive cells to the changing needs of the organ [9], greatly impacting the stem cell decision to migrate. The niche constituents, although varied by the stem cell class, are believed to generally include the mature cells of the same lineage, the undifferentiated stem cell progeny and even heterologous stem cells, as well as endothelial cells of the vasculature, mesenchymal cells that are characteristic to a given tissue type, and neural and inflammatory cells. The non-cellular materials, such as extracellular matrix proteins, are also integral to the stem cell niche (for up-to-date reviews on the stem cell niches, see [21–24, 56, 91–97]). In the stem-cell regulated organs, tissue injury evokes multifarious short- and long-range feedbacks to the niches, deploying programs for stem cell activation and mobilization. Some of the major molecular systems mediating these processes are discussed below.
Signaling by Secreted Mediators
Commonly, changes in the cell migratory behavior occur in response to variations in local concentration of secreted agents, such as cytokines and bioactive lipids.
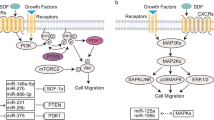
Chemotactic Cytokines and Growth Factors
Chemotaxis is directional movement of cells according to concentration gradient of soluble chemical factors. Chemotaxis is arguably one of the most explored mechanisms governing cell translocation, indispensable for any biological phenomenon relying on cell migration [2, 3, 98–100], and for the stem and progenitor cell trafficking. Over the years, a multitude of growth factor and cytokines was described as motility-inducing agents for the different categories of primitive cells, guiding their migration and recruitment to the site of tissue repair. For example, the chemotaxis towards the cytokine CXCL12 (a.k.a., SDF-1) is a major pathway regulating immature hematopoietic cell circulation to and from the bone marrow (recently reviewed in [16, 19, 101, 102]). CXCR4 and CXCR7 are two identified receptors for CXCL12, although the expression and function of CXCR7 in normal hematopoietic cells is less studied. Since the initial report on the necessity of CXCL12/CXCR4 system for the hematopoietic stem cell migration and bone marrow engraftment in adults [103], hundreds investigations addressed the various biological processes modulating CXCL12/CXCR4 axis in health and disease, as well as its translational applications for the mobilization of primitive hematopoietic cells and bone marrow transplantation procedures. Moreover, it is now understood that CXCL12/CXCR4-mediated signaling plays a central role in hematopoietic progenitor cell migration to the organs other than the bone marrow, such as the injured liver [35]; or the recruitment of other stem cell types, as shown for endothelial [104] and neural [105] precursors.
Of interest, in primitive hematopoietic cells, the cytokine stem cell factor (SCF) has a synergistic effect with CXCL12 [35]. SCF also stimulates dental pulp progenitor migration, and is suggested to act as a homing factor for immature cells in the course of dental pulp regeneration [106]. Another well-documented stem cell chemoattractant is hepatocyte growth factor, HGF (known as scatter factor), which binds and activates c-Met receptor. HGF/c-Met pathway induces migration of hematopoietic progenitors and facilitates stress-induced mobilization from the bone marrow [35, 107, 108]. HGF/c-Met promotes chemotaxis of satellite cells as well [109–113], which is required for myoblast directional motility and myocyte fusion during adult skeletal muscle restoration [113].
Although substantial knowledge has been already accumulated on the necessity of cytokines and growth factors for the regulation of stem cell migration, with the progress of the research into the trafficking of immature cells, new pathways driving adult stem cell translocation are coming into focus.
Bioactive Lipids
In addition to soluble proteins, the diverse groups of bioactive lipids constitute an important mechanism for the cell communication with the surroundings. As exemplified by sphingosine 1-phosphate (S1P) and lysophosphatidic acid (LPA), the signaling evoked by bioactive lipids via respective receptors is crucial for multiple aspects of cell behavior (for recent reviews, see [114–119]). Intriguingly, it was demonstrated that the expression of the LPA receptor by itself serves as a specific functional marker of hippocampal precursor cells in the adult brain [120]. The migratory responses of stem and progenitor cells are likewise dictated by these molecules (reviewed in [38, 118, 121, 122]). It is demonstrated that S1P acts as a chemoattractant for primitive hematopoietic cells, affecting their mobilization and homing to the bone marrow and the circulation to other organs [26, 123–126]. There is also indication that S1P and LPA stimulate the motility of skeletal muscle satellite cells [127, 128], which might improve progenitor recruitment to the site of damage. S1P is involved in the migration between blood and bone of osteoclast precursors, thus fine-tuning their localization to the bone surface and balancing bone remodeling [129, 130]. Further, the activation of a neural-specific subtype of S1P receptors antagonizes the motility of immature oligodendrocytes [131], while treatments that inhibit S1P signaling potentiate the migration of endogenous neural progenitors in the brain [132] and transplanted neural progenitors in the spinal cord [133].
As it is the case with virtually any stimulus received by the cell, the intracellular signaling cascades evoked by bioactive lipids frequently converge with other pathways governing stem cell trafficking, for example, CXCL12-induced chemotaxis [121, 133]. Such a complex and multifaceted regulation of the tissue progenitor cell motility likely enables coordinated and measured reactions to the environmental changes. Moreover, as discussed in the following sections, physical contacts with the neighboring cells and extracellular components are critical as well for the optimal stem cell movement and recruitment to the site of injury repair.
Juxtacrine Signaling
Along with the secreted factors, the stem cell migratory behavior within and outside the niches is determined by direct binding to the various surrounding cell types and the properties of the extracellular milieu. Several classes of adhesion molecules mediate these interactions and are considered fundamental for the control of stem and progenitor migration.
Eph and Ephrins
Widely implicated in determining cell positioning is a large and versatile family of receptor tyrosine kinases called Eph (the name is derived from the erythropoietin-producing human hepatocellular carcinoma cell line, from which the first member was isolated), and their membrane-tethered ligands, ephrins. Ephrin/Eph axis directs processes requiring immediate changes in cell morphology, adhesion and motility (for recent comprehensive reviews on the ephrin and Eph signaling and function, see [134–145]). This cell contact-dependent communication is bi-directional, namely, the message is transduced into the Eph receptor-expressing cells (“forward signaling”) as well as the ephrin ligand-presenting cells (“reverse signaling”). Since multiple members of the ligand and receptor families are often co-expressed on the same cell, the ephrin/Eph axis is subjected to an additional level of regulation by “cis”-binding, which may antagonize the effect induced by the associations in “trans” to a partner on an opposing membrane. Extensive cross-talk with other signaling pathways and a kinase-independent activity of Eph receptors further contribute to the diversity of the possible downstream cascades.
It is increasingly recognized that ephrin/Eph axis plays a vital role in the biology and migratory behavior of adult stem and progenitor cells. In the hematopoietic system, the activation of ephrin A5 potentiates immature hematopoietic cell adhesion in the bone marrow niche, and can be manipulated to diminish their retention and enhance mobilization to the blood [146]. Moreover, binding to EphB4 on the bone marrow stroma modulates ephrin B2 expression in the primitive hematopoietic cells, impacting the stem cell ability to translocate beneath the stromal layer and colonize the niches [147–149]. Likewise, in the adult dental tissue, EphB and ephrin B proteins are involved in the interactions of the primitive cells with the microenvironment: ephrin B1 and ephrin B3 expression on the pulp cells restricts the progenitor attachment and migration in the niche in homeostatic conditions [150] and after tooth injury [151].
Diverse ephrin/Eph-mediated pathways are extensively described in the development of the nervous system, and there are numerous findings corroborating their direct involvement in adult neurogenesis, and the control of migratory behavior of the immature cells in the brain: it is documented that EphB receptors and ephrin B1-3 ligands are expressed in the sub-ventricular zone, potentiating the proliferation and migration of neuroblasts [152]; and in the dentate gyrus, where the EphB2 forward signaling is necessary for the migration of the sub-ventricular zone progenitors [153]. Also in the hippocampus, the proliferation, polarity and positioning of immature cells are altered in animals lacking the EphB1 receptor or ephrin B3 ligand [154]. In contrast, ephrin A2 and EphA7 knockouts are characterized by amplified progenitor cell proliferation and neuron formation with no obvious migratory defects [155]. Furthermore, an intriguing study by Parrinello and colleagues shows that after transection of the sciatic nerve, EphB forward signaling, by inducing progenitor cell separation from surrounding cells, directs peripheral nerve regeneration [156]. Specifically, the immature Schwann cells that migrate into the wound present EphB2, which is activated by ephrin B on fibroblasts; this causes augmentation of the N-cadherin-mediated homotypic adhesion between the moving cells and the formation of Schwann cell cords that support the regrowth of neurons.
In the skeletal muscle, ephrins and Ephs were previously suggested to guide the migrating myoblasts from the storing niches to the site of injury [111, 112, 157]. Indeed, a recent study by Gu et al. provides in vivo evidence that the immature muscle cells, moving towards the end of extending myofibers, bind ephrin A5, which is abundantly presented on the adjacent interstitial cells [158]. Although the specific Eph receptors controlling the behavior of satellite cells and their progeny remains to be determined, ephrin A5 is essential for the activation of the directional translocation of myoblasts and neonatal muscle growth [158].
Ephrin A proteins are also important in the adult heart: undifferentiated cells in the myocardial parenchyma preferentially express EphA2 [159, 160], whereas ephrin A1, one of the EphA2 ligands, is highly represented in cardiomyocytes [159–161]. EphA2 stimulation by ephrin A1 promotes cell motility in the infarcted tissue [159, 160], and there are reports indicating that the ephrin A1/EphA2 signaling is beneficial for cardiac recovery after ischemic injury [159, 161–163]. Intriguingly, with cellular aging, EphA2 is subjected to post-translational modifications, which hinder its kinase activity, interfering with the cell chemotaxis towards HGF in vitro and the ephrin A1-induced motility of transplanted cells in the infarcted myocardium [160]. Ephrin A1 protein level is also somewhat reduced in the old heart tissue [160]. Hence, it is tempting to speculate the existence of an interrelationship between the age-associated decline in the ephrin A1 and EphA2 functionality and the weakened performance of the senescent heart. In the same way, the aging progenitor cells of the tendon display a downregulation of the ephrin B1, EphA4, EphB2 and EphB4, accompanied by diminished ability to migrate, which can be ameliorated by enhancing EphA4 and EphB2 reverse signaling [164].
Of note, the complementary expression pattern of the Eph receptors in the primitive cells and the ephrin ligands in the differentiated progeny of those cells, is widely described in epithelial tissues, in which EphB receptors and B type ephrins are essential for the correct cell positioning [62, 165–170]. For instance, the highest level of EphB2 and EphB3 is detected in the immature cells residing in the intestinal crypt, whereas dividing and differentiating cells that move upward the crypt gradually lose EphBs and acquire ephrins B, e.g., ephrin B1 and ephrin B2. Consequently, there is a counter-gradient of EphB and ephrin B proteins along the crypt axis, with the most Eph receptors in stem and progenitor cells at the crypt base, and the ephrin ligands in the mature cells, situated at the crypt boundary with the villus. It is assumed that the EphB receptors generate repulsive cues, which prevent an untimely migration of precursors into the ephrin-enriched zone of the more differentiated cells. Interfering with the EphB forward signaling alters the location of cells in the crypt and reduces their proliferation. Interestingly, there are indications that the Eph mitogenic activity in stem cells, controlled by Abl/cyclin D1 pathway, is distinct from the receptor downstream signaling via PI3 kinase, which is involved in cell positioning [166, 168, 171]. In a similar manner, in the course of branching morphogenesis, ephrin A1/EphA axis concomitantly evokes two independent pathways correspondingly triggering cell proliferation and inhibiting the formation of HGF-induced cellular protrusions [172]. It is important to point out that the activity of ephrin/Eph family is known to frequently modulate other processes required for progenitor cell translocation, especially, the primitive cell responses to chemotactic stimuli by cytokines and growth factors [111, 112, 159, 172–174].
In conclusion, owing to an extraordinary ability of facilitating direct communication between heterogeneous cell types, the capacity of simultaneously eliciting responses in the ligand and receptor bearing cells, and great versatility of the downstream signaling modes, the ephrin/Eph axis is central for the patterning of stem and progenitor cell translocation in adult tissues.
Other Modules of Direct Cell-to-Cell Communication
One can envisage that in the stem cell microenvironment, additional mechanisms mediating the cell-to-cell binding impact the propensity of immature cells to migrate. For example, the cadherins constitute a large family of intercellular adhesion molecules that regulate multiple biological processes, including determination of the cell polarity and collective cell migration (the cadherin family is extensively reviewed elsewhere [175–179]). Recent studies indicate that cadherin-containing adherens junctions enable the attachment of primitive cells to other cellular constituents of the niche, as well as homotypic adhesion between the stem cells themselves, which helps to preserve their quiescence [180–183]. Thus, inhibition of cadherin-mediated binding might be required to antagonize stem cell dormancy and promote emigration from the niches. In support, there are findings that N-cadherin protein on neural progenitor cells is cleaved in response to tissue injury, leading to cell activation [182, 184], egress from the sub-ventricular zone, and translocation into demyelinated lesions [184].
Also gap junctional proteins, connexins, are described in the context of stem cell interactions with the neighboring tissue cells (reviewed in [185–187]). Interestingly, whereas connexin 43 deficiency in osteoblasts and osteogenic progenitors in the bone marrow niches does not impair the steady state hematopoiesis, it disrupts the trans-stromal migration of immature hematopoietic cells, which consequently impedes their mobilization and homing [188]. However, these alterations might not result from the changes in connexin-mediated cell-to-cell adhesion, but rather be triggered by the elevated level of CXCL12 in the connexin 43-knockout cells [188]. Indeed, it was shown that CXCL12 secretion by bone marrow stroma is cell contact-dependent and involves gap junctions built by connexin 43 and connexin 45 [189].
Additional group of the cell-cell adhesion receptors participating in the trafficking of primitive cells includes P- and E-selectins, which are required for the initial tethering of circulating hematopoietic progenitors to the endothelium of bone marrow vasculature, thus constituting the first critical step in the homing process (reviewed in [20, 190, 191]). Recently, selectins have been credited with a significant function in the hematopoietic stem cell communications with the bone marrow niche [192, 193]. Whether selectins are involved in the migration of adult progenitors of non-hematopoietic origins remains to be established.
The adhesion molecules of the integrin family are essential mediators of both cell-to-cell and cell-to-substrate binding. Integrins are discussed in details below in the section on the extracellular matrix. Importantly, integrins are key players in the hematopoietic stem and progenitor cell migration. Several integrin subtypes, e.g., α4β1, have been implicated in the hematopoietic cell attachment to the endothelium and subsequent trans-endothelial migration during homing to the bone marrow [20, 190, 191] and, possibly, in the course of hematopoietic and endothelial progenitor cell recruitment to ischemic tissues [194].
The CD44 antigen is another major receptor performing multiple tasks for the interaction of cells with microenvironment. Of special interest is a distinct selectin-binding glycoform of CD44, termed HCELL (for Hematopoietic Cell E-selectin/L-selectin Ligand), which is uniquely expressed on the immature human hematopoietic population. HCELL facilitates hematopoietic stem cell adhesion to the endothelium and bone marrow homing (reviewed in [195, 196]). Notably, a novel technology has been developed to transform CD44 into the HCELL glycoprotein in other progenitor types that lack native HCELL expression. This approach has the potential of improving cell binding to activated endothelial cells and, as a result, the targeting of intravascularly administered progenitors to the sites of injury and inflammation [197, 198].
It is plausible that the diverse modalities of cell-to-cell communication have evolved to address the complex and dynamic processes of stem cell activation and translocation in response to the changes in immediate tissue environment. In a similar manner, physical interactions with the non-cellular tissue components are pivotal for the immature cell trafficking.
Extracellular Matrix and Mechanical Cues
The term extracellular matrix (ECM) broadly refers to the non-cellular constituents of the tissue milieu, in which the cells are embedded. ECM consists from the network of fibrous proteins, sugar moieties, immobilized cytokines and growth factors, and other molecules secreted by the cells. The composition and structural properties of the ECM are highly specific to each organ and substantially vary in the presence of pathologies and with aging [199–204]. In addition to providing scaffolding, ECM fulfils instructive roles by transducing biochemical and biomechanical signals to the cells and being a substrate for cell adhesion and migration [6, 202, 205–208].
It is demonstrated that the contacts of immature cells with the ECM in niches determine the stem cell behavior: the molecular complexity of the ECM, its microscale topography, degree of elasticity, and amplitude and frequency of static and dynamic deformations, are all influencing the stem cell choices of quiescence versus proliferation, self-renewal versus differentiation, and death versus survival (for the discussion on these topics, see the following recent reviews [199, 205, 206, 208–213]).
How the ECM conveys information to the cells? The binding of cells to the ECM primarily occurs via integrins. Integrins are heterodimer transmembrane proteins composed of α subunit and β subunit, each has multiple variants. The combinations of subunits confer specificity to the cell recognition of the diverse ECM proteins, such as fibronectin, laminin or collagen, and the specific epitopes within the protein sequence. Intracellularly, integrins are associated with the cytoskeleton and a panel of signaling molecules. Integrins mediate inside-out and outside-in communication between the cell and the physical neighbors and, therefore, are vital for the processes of cell migration, differentiation, and tissue morphogenesis and maintenance in the adult (for comprehensive reviews on integrin structure and function, see [214–220]).
As expected, integrin-mediated adhesion to the ECM impacts stem and progenitor cell motility. For example, integrin αvβ1 is postulated to control translocation of oligodendrocyte precursors in the central nervous system, whereas downregulation of this receptor is associated with the cell maturation and changes in the migratory phenotype [221]. Likewise, epithelial progenitor cells in the hair follicles require β1 integrin signaling for the adhesion and migration of their progeny, and, of note, the various sub-classes of immature endothelial cells exhibit disparate responses to the changes in the β1 activity [222]. In the populations of primitive hematopoietic cells, the adhesion to fibronectin via integrin α4β1 is functionally linked to the cytokine-induced chemotaxis [223]. Intriguingly, whereas cytokines activate the movement of resting progenitors, the cell migration speed is modified by the fibronectin concentration [224]. The immature hematopoietic cells also exhibit variations in the integrin α6β1-mediated adhesion and movement when presented with distinct isoforms of laminin [225]. Interestingly, it was noticed that the contribution of different integrin α chains to the substrate binding by hematopoietic progenitors is donor-dependent [226].
Further, mechanosensing is an important function of the integrins (reviewed in [208, 214, 218, 220, 227–229]). There are accumulating confirmations, mainly from the studied on developmental morphogenesis, that mechanical forces, applied by the microenvironment to the primitive cells, control their activity [202, 205–207, 230]. The progenitors in the adult tissues are equally subjected to the changes in shear stresses, tension, or periodical stretches, which, as mentioned above, significantly impact cell fate decisions [199, 205, 206, 208–213]. Surprisingly, considerably less data are available on the role of biomechanical cues in the adult tissue stem and progenitor cell translocation. Yet, there are indications that immature hematopoietic cells attach and migrate better on stiffer substrates [231, 232], which might be relevant for the homing and engraftment in the bone marrow. Similarly, the migration of osteoblast precursors is highly dependent on the matrix stiffness [233]. Along with the ECM rigidity, the technological advances in bioengineering approaches brought to light the significance of surface nanotopography for the regulation of cell binding and locomotion [210]. It was shown that primitive hematopoietic cells change the tendency to adhere to fibronectin- or osteopontin-derived peptides according to the nanometer scale variations in the spacing of these elements [226]. Cell’s perception of the nanoscale substrate distribution and structure, e.g., existence of pillars and grooves, is also known to dictate the alignment and polarization of immature neural cells [234], which might enhance their differentiations [234–236]. Moreover, dissimilar motility responses are observed when undifferentiated neural stem cells and astrocyte progeny, and the stem cell-derived neurons, are concomitantly exposed to laminin-coated micropatterned surfaces, allowing in vitro separation of newborn astrocytes and neurons [237].
It must be indicated that mechanosensory functions are not limited to integrin-mediated adhesions to the ECM. Forces are transmitted via cadherins in the adherens junctions and other types of cell-to-cell attachments [238–240]. Hence, the disruption of the intercellular connections after tissue injury or in pathological states might cause aberrations in the migratory pattern of progenitor cells.
Moreover, there are receptors outside the integrin family that are required for the cell contacts with the ECM and control of primitive cell translocation. For example, the different isoforms of the CD44 protein are critically implicated in the adhesion to bone marrow matrix and the lodgment of normal and malignant hematopoietic progenitors to specialized endosteal niches, which are rich in the ECM protein, hyaluronic acid (reviewed in [15, 19, 241]). In the hematopoietic stem cell niche, CD44 and CXCL12/CXCR4 pathways cross-react: interference with the CD44 activity impairs CXCL12-induced chemotaxis, whereas treatment with CXCL12 potentiates CD44-mediated ECM binding and niche engraftment of immature hematopoietic cells [242]. In the course of hematopoietic progenitor cell mobilization, CD44 is cleaved by matrix metalloproteinases, facilitating cell egress from the bone marrow [243].
Curiously, the CD34 molecule, a primary marker of the primitive hematopoietic cells in humans, is also an adhesion receptor. The function of the CD34 protein in early hematopoietic progenitors is insufficiently known: on the one hand, ectopically expressed human CD34 increases murine hematopoietic cell interactions with the human bone marrow stroma [244], on the other hand, there are studies pointing to the anti-adhesive and pro-migratory roles of CD34 [245]. CD34 is also highly present in endothelial and skeletal muscle progenitors, and the CD34 knockout impairs satellite cell proliferation and motility [246].
A striking confirmation of the essential and multiplex involvement of the ECM in the contact-dependent guidance of progenitor cells for tissue repair was recently provided by live imaging of the satellite cell translocation in injured skeletal muscles [74]. This study revealed that following myofiber death and degradation, the remaining ECM structures, coined by authors the “ghost fibers”, direct the muscle regenerative response by orienting the migration and subsequent division of activated myogenic progenitors along the longitudinal axis of the fiber ECM. Alterations in the positioning of these ECM arrangements disturb the migratory path and division plane of satellite cells, causing disorganization of the newly - formed myofibers. Interestingly, the satellite cells from an uninjured fiber are not mobilized from their location to the affected area, suggesting that the myofiber ECM acts as autonomous architectural unit necessary for proportionate regeneration of the tissue.
To summarize, based on the extensive research, spanning the matrix features from nanoscale to whole-organ level, it is apparent that the diverse modes of immature cell interactions with the substrate evoke multitude of biochemical and mechanical signals, operating in tandem to coordinate the motile behavior of stem and progenitor cells. Furthermore, cellular behavior is highly context-specific: the propensity of stem cells to migrate is regulated by copious mechanisms and is dictated by the tissue composition, disease state and age. Importantly, the processes of cell movement are dynamic by nature. Thus, as discussed in the next section, imaging approaches for the visualization of live cells in their microenvironment are among most powerful tools employed today for the studies of immature cell trafficking in different organs.
Live Imaging for the Investigations of Stem and Progenitor Cell Motility
There are diverse biological imaging platforms enabling observations of isolated cells, as well as visualization of endogenous or transplanted cells in vivo. These methodologies range from monitoring single-cell behavior in an artificial environment to the longitudinal analysis of the distribution of cells in live organisms. The resolution of each approach depends on the type of label (for instance, fluorescence, bioluminescence, nuclear, or magnetic), the corresponding imaging modality (namely, light imaging, positron emission tomography, or magnetic resonance imaging), as well as the nature of examined samples (e.g., in vitro cell analysis versus studies of cells in organs). The technological details and relative advantages of the currently employed procedures for the stem cell imaging are extensively discussed in the literature [11, 247–252]. The present paper focuses on the light imaging using fluorescence microscopy, since it is one of the better established and commonly used methods for the identification of stem cells in situ and exploration of their motility.
The migration of stem and progenitors cells is frequently examined by observing the behavior of isolated cells in vitro. Many of the findings on the juxtacrine and paracrine signaling in the stem cell translocation, as described in the above sections, were obtained by this methodology. For example, the live imaging of cells from a skeletal myoblast line has revealed that fibronectin promotes integrin- and cadherin-mediated cell-to-cell alignment and collective movement, which facilitates ensuing myoblast fusion [253]. Also, by microscopic observations of primary muscle progenitors, it was established that Wnt7a/Fzd7 axis increases cell polarity and directional migration, and has a beneficial effect on the myogenic cell engraftment after transplantation [254]. Similarly, by monitoring live cell motility in collagen gel cultures, HGF was identified as a major chemoattractant for satellite cells [112]. In the same study, the live imaging of the endogenous cells in the explanted whole myofibers emphasized the intricacy of the mechanisms regulating stem cell migratory behavior, impacted by a host of environmental inputs [112]. Thus, while in vitro imaging is particularly instrumental for establishing specific chemoattractants for the immature cells, or pinpointing the fine characteristics of the substrate that influence cell migration, the extreme complexity of the stem cell native environment is only partially reflected in these setups. Consequently, intravital imaging, that is live imaging of cells in the animal organs [248, 255–257], is invaluable for elucidating the pathways orchestrating stem cell migratory responses in the conditions that are close to physiological.
A pioneering work implementing intravital imaging for the studies of stem cell trafficking was performed by Mazo and colleagues, who developed a methodology for the live observations of transfused, fluorescent dye-labeled hematopoietic progenitor cells in the bone marrow of the mouse calvarium [258]. Using this approach, they demonstrated for the first time that the unique expression pattern of P-/E-selectins and the vascular cell adhesion molecule-1 on the bone marrow microvasculature enables adhesion of circulating hematopoietic progenitors and facilitates their homing. The intravital microscopy of the mouse calvarium for the studies of homing and retention of transplanted hematopoietic stem and progenitors was subsequently applied by other groups, who introduced new platforms of monitoring primitive cell behavior after engraftment in the bone marrow niches with differentially labeled stromal cell populations, modified dyes for the stem cell tracking, and advanced technologies for image acquisition and quantitative analysis [259–263]. These methodologies hold promise to accelerate the research into the molecular mechanisms governing hematopoietic stem cell trafficking after transplantation. Indeed, in a recent work by Itkin et al., the observations of mouse bone marrow by live imaging led to the documentation of distinct vascular compartments, i.e., high-permeability sinusoids, functioning as dedicated sites for immature hematopoietic cell transmigration [264]. The activation of cell motility occurs in these locations due to exposure to the peripheral blood plasma, which, on the other hand, antagonizes bone marrow stem cell quiescence and hampers self-renewing and long-term repopulating potentials. These findings bring forth new considerations of manipulating vascular integrity and adjusting the degree of plasma penetration via blood-bone marrow barrier for the clinical mobilization and transplantation protocols.
The migration of skeletal muscle satellite cells was also addressed by intravital imaging. In confirmation of the in vitro studies, it was documented by live observations that exogenous HGF induces cell migration in the rat soleus muscle [110], where the cells are prompted to move by the tissue damage [265]. However, in these works no specific markers of the myogenic progenitors were utilized. A more recent study by Webster et al. introduced intravital imaging in a transgenic mouse with the progeny of muscle stem cells tagged by the expression of a fluorescent protein: in this model, the live imaging of muscle progenitor migration was crucial for the identification of the specific ECM structures remained after the myofiber death that guide the directional translocation of activated myogenic cells for adequate tissue repair [74].
In the adult brain, intravital imaging was recently used to study the trafficking of newly-born neurons: by infecting the endogenous cells with fluorescent protein-expressing lentivirus, and introducing fluorescent calcium indicators, the functional incorporation of migrated cells in the olfactory bulb was evaluated [266]. This work suggests that in addition to intrinsic spontaneous activity of neuronal circuits, extrinsic sensory-driven signals propel the integration of immature stem cell progeny within the adult nervous system.
A critical insight on the stem cell behavior during hair follicle regeneration originated from a series of intravital imaging studies performed by the group of Greco and collaborators [56, 255, 267–270]. To visualize the hair follicle constituents, several fluorescent reporters were combined in a transgenic mouse model in order to differentially label epithelial and mesenchymal populations, and repeated observations of the ear skin were conducted. By this approach, it was demonstrated that the migration, as well as commitment, proliferation, death and clearance of primitive and maturing cells, are spatially restricted events within the sub-compartments of hair follicle epithelium, and these processes are determined by the cell proximity to mesenchymal dermal papilla niche.
Despite the implicit importance of monitoring stem cell behavior in the natural environment of a live organism, the number of published studies implementing intravital imaging of adult organs in rodents is relatively limited, as this type of investigations presents extreme technical challenges. Some of the confiding factors include the need in advanced and elaborated equipment, as well as an expertise in image acquisition and quantitative analysis. Further, the imaging has to be performed in anesthetized animals for the extent of hours, while the imaged tissue is exposed for the optical observations. This entails development of complex surgery protocols and imaging set-ups aiming at maintaining organ function, minimizing tissue injury and attenuating its deterioration, diminishing light-induced damage to the imaged cells and their environment, and avoiding motion artifacts. Moreover, transgenic animals or other modalities for the specific expression of fluorescent protein/s in population/s of interest are required, whereas for many types of stem cells, a single marker is insufficient for faithfully discrimination of primitive cells from other cell cohorts. Additionally, in some tissues, the location of stem cells is uncertain, or their sites are inaccessible to the light due to the organ size (for example, sub-ventricular zone in the brain or the marrow of long bones).
Consequently, alternative approaches for exploring stem cell motility in tissues using ex vivo organotypic cultures have been used. For instance, by imaging of brain slices, the characteristics of the sub-ventricular zone neuroblast movement were examined by several groups [271–274], showing that contrary to the expectations, the neuroblast migratory chains remain stable and immotile for relatively long periods of time. Interestingly, in these settings, it was found that physiological electrical signals promote the chain migration of neuroblasts by augmenting purinergic receptors and enhancing cell adhesion [275]. Additionally, imaging of the excised perfused hearts has been utilized to demonstrate the involvement of the ephrin A1/EphA2 pathway in the control of cardiac progenitor cell movement after transplantation into the acutely infarcted myocardial parenchyma [159, 160]. Likewise, live observations of the isolated myofibers were instrumental in uncovering the role of various cytokines, ECM components and adhesion molecules in directing satellite cell translocation [112, 246].
Therefore, by combining different methodologies for the live imaging in vitro, in vivo and ex vivo, one can achieve a better comprehension of the complex mechanisms defining the stem cell trafficking in the course of tissue homeostasis and after injury.
Concluding Remarks
The rapidly expanding field of adult stem cells prompted investigations into the molecular underpinnings of the migratory behavior of immature cells, leading to considerable advancements in elucidating the elements in tissue microenvironment that impact the stem cell trafficking. Among the key factors are secreted mediators, direct contacts of primitive cells with their neighbors, and biochemical and physical characteristics of the extra-cellular matrix, all acting in concert to optimally coordinate the stem cell movement. While these regulatory pathways are not unique to stem cells, it is argued that the intricate responses of the immature cells address in a specific manner the needs of organ maintenance and repair, and could be exploited for regenerative approaches of modulating the translocation of endogenous or transplanted progenitors. Moreover, there is evidence that the abnormalities in the migratory ability of stem cells are causative of pathological changes in tissues, which occur with age and diseases. Future research in this area, facilitated by the implementation of innovative live imaging platforms and other new technological tools for the studies of immature cell biology and function, will improve our understanding of the multifaceted processes governing cell recruitment to the site of injury and hold great promises for the success of cell-based regenerative therapeutics.
References
Devreotes, P., & Horwitz, A. R. (2015). Signaling networks that regulate cell migration. Cold Spring Harbor Perspectives in Biology, 7(8), a005959.
Haeger, A., Wolf, K., Zegers, M. M., & Friedl, P. (2015). Collective cell migration: guidance principles and hierarchies. Trends in Cell Biology, 25(9), 556–566.
Lara Rodriguez, L., & Schneider, I. C. (2013). Directed cell migration in multi-cue environments. Integrative Biology: Quantitative Biosciences from Nano to Macro, 5(11), 1306–1323.
Shaw, T. J., & Martin, P. (2016). Wound repair: a showcase for cell plasticity and migration. Current Opinion in Cell Biology, 42, 29–37.
Visvader, J. E., & Clevers, H. (2016). Tissue-specific designs of stem cell hierarchies. Nature Cell Biology, 18(4), 349–355.
Lalli, G. (2014). Extracellular signals controlling neuroblast migration in the postnatal brain. Advances in Experimental Medicine and Biology, 800, 149–180.
Magnon, C., Lucas, D., & Frenette, P. S. (2011). Trafficking of stem cells. Methods in Molecular Biology (Clifton, NJ), 750, 3–24.
Urao, N., & Ushio-Fukai, M. (2013). Redox regulation of stem/progenitor cells and bone marrow niche. Free Radical Biology & Medicine, 54, 26–39.
Xin, T., Greco, V., & Myung, P. (2016). Hardwiring stem cell communication through tissue structure. Cell, 164(6), 1212–1225.
Fox, I. J., Daley, G. Q., Goldman, S. A., Huard, J., Kamp, T. J., & Trucco, M. (2014). Stem cell therapy. Use of differentiated pluripotent stem cells as replacement therapy for treating disease. Science, 345(6199), 1247391.
Nguyen, P. K., Riegler, J., & Wu, J. C. (2014). Stem cell imaging: from bench to bedside. Cell Stem Cell, 14(4), 431–444.
Srijaya, T. C., Ramasamy, T. S., & Kasim, N. H. (2014). Advancing stem cell therapy from bench to bedside: lessons from drug therapies. Journal of Translational Medicine, 12, 243.
Bonig, H., & Papayannopoulou, T. (2013). Hematopoietic stem cell mobilization: updated conceptual renditions. Leukemia, 27(1), 24–31.
Boulais, P. E., & Frenette, P. S. (2015). Making sense of hematopoietic stem cell niches. Blood, 125(17), 2621–2629.
Golan, K., Vagima, Y., Goichberg, P., Gur-Cohen, S., & Lapidot, T. (2011). MT1-MMP and RECK: opposite and essential roles in hematopoietic stem and progenitor cell retention and migration. Journal of Molecular Medicine (Berlin, Germany), 89(12), 1167–1174.
Gur-Cohen, S., Kollet, O., Graf, C., Esmon, C.T., Ruf, W., Lapidot, T. (2016). Regulation of long-term repopulating hematopoietic stem cells by EPCR/PAR1 signaling. Annals of the New York Academy of Sciences. doi:10.1111/nyas.13013.
Hoggatt, J., Speth, J. M., & Pelus, L. M. (2013). Concise review: sowing the seeds of a fruitful harvest: hematopoietic stem cell mobilization. Stem Cells (Dayton, Ohio), 31(12), 2599–2606.
Kollet, O., Canaani, J., Kalinkovich, A., & Lapidot, T. (2012). Regulatory cross talks of bone cells, hematopoietic stem cells and the nervous system maintain hematopoiesis. Inflammation & Allergy: Drug Targets, 11(3), 170–180.
Lapid, K., Glait-Santar, C., Gur-Cohen, S., Canaani, J., Kollet, O., & Lapidot, T. (2008). Egress and mobilization of hematopoietic stem and progenitor cells: A dynamic multi-facet process. Cambridge, MA: StemBook.
Mazo, I. B., Massberg, S., & von Andrian, U. H. (2011). Hematopoietic stem and progenitor cell trafficking. Trends in Immunology, 32(10), 493–503.
Birbrair, A., Frenette, P.S. (2016). Niche heterogeneity in the bone marrow. Annals of the New York Academy of Sciences. doi:10.1111/nyas.13016.
Mendelson, A., & Frenette, P. S. (2014). Hematopoietic stem cell niche maintenance during homeostasis and regeneration. Nature Medicine, 20(8), 833–846.
Morrison, S. J., & Scadden, D. T. (2014). The bone marrow niche for haematopoietic stem cells. Nature, 505(7483), 327–334.
Scadden, D. T. (2014). Nice neighborhood: emerging concepts of the stem cell niche. Cell, 157(1), 41–50.
Abkowitz, J. L., Robinson, A. E., Kale, S., Long, M. W., & Chen, J. (2003). Mobilization of hematopoietic stem cells during homeostasis and after cytokine exposure. Blood, 102(4), 1249–1253.
Massberg, S., Schaerli, P., Knezevic-Maramica, I., Kollnberger, M., Tubo, N., Moseman, E. A., et al. (2007). Immunosurveillance by hematopoietic progenitor cells trafficking through blood, lymph, and peripheral tissues. Cell, 131(5), 994–1008.
Wright, D. E., Wagers, A. J., Gulati, A. P., Johnson, F. L., & Weissman, I. L. (2001). Physiological migration of hematopoietic stem and progenitor cells. Science, 294(5548), 1933–1936.
Casanova-Acebes, M., Pitaval, C., Weiss, L. A., Nombela-Arrieta, C., Chevre, R., A-González, N., et al. (2013). Rhythmic modulation of the hematopoietic niche through neutrophil clearance. Cell, 153(5), 1025–1035.
Kollet, O., Vagima, Y., D’Uva, G., Golan, K., Canaani, J., Itkin, T., et al. (2013). Physiologic corticosterone oscillations regulate murine hematopoietic stem/progenitor cell proliferation and CXCL12 expression by bone marrow stromal progenitors. Leukemia, 27(10), 2006–2015.
Mendez-Ferrer, S., Lucas, D., Battista, M., & Frenette, P. S. (2008). Haematopoietic stem cell release is regulated by circadian oscillations. Nature, 452(7186), 442–447.
Kobayashi, H., Suda, T., & Takubo, K. (2016). How hematopoietic stem/progenitors and their niche sense and respond to infectious stress. Experimental Hematology, 44(2), 92–100.
Schuettpelz, L. G., & Link, D. C. (2013). Regulation of hematopoietic stem cell activity by inflammation. Frontiers in Immunology, 4, 204.
Badami, C. D., Livingston, D. H., Sifri, Z. C., Caputo, F. J., Bonilla, L., Mohr, A. M., & Deitch, E. A. (2007). Hematopoietic progenitor cells mobilize to the site of injury after trauma and hemorrhagic shock in rats. The Journal of Trauma, 63(3), 596–600. discussion 600–592.
Dalakas, E., Newsome, P. N., Harrison, D. J., & Plevris, J. N. (2005). Hematopoietic stem cell trafficking in liver injury. FASEB Journal: Official Publication of the Federation of American Societies for Experimental Biology, 19(10), 1225–1231.
Kollet, O., Shivtiel, S., Chen, Y. Q., Suriawinata, J., Thung, S. N., Dabeva, M. D., et al. (2003). HGF, SDF-1, and MMP-9 are involved in stress-induced human CD34+ stem cell recruitment to the liver. The Journal of Clinical Investigation, 112(2), 160–169.
Mocco, J., Afzal, A., Ansari, S., Wolfe, A., Caldwell, K., Connolly, E. S., & Scott, E. W. (2014). SDF1-a facilitates Lin-/Sca1+ cell homing following murine experimental cerebral ischemia. PloS One, 9(1), e85615.
Dutta, P., Sager, H. B., Stengel, K. R., Naxerova, K., Courties, G., Saez, B., et al. (2015). Myocardial Infarction Activates CCR2(+) Hematopoietic Stem and Progenitor Cells. Cell Stem Cell, 16(5), 477–487.
Klyachkin, Y. M., Karapetyan, A. V., Ratajczak, M. Z., & Abdel-Latif, A. (2014). The role of bioactive lipids in stem cell mobilization and homing: novel therapeutics for myocardial ischemia. BioMed Research International, 2014, 653543.
Cipriani, P., Ruscitti, P., & Giacomelli, R. (2015). Stem cell therapies for systemic sclerosis. British Journal of Haematology, 168(3), 328–337.
Maeshima, A., Nakasatomi, M., & Nojima, Y. (2014). Regenerative medicine for the kidney: renotropic factors, renal stem/progenitor cells, and stem cell therapy. BioMed Research International, 2014, 595493.
Margini, C., Vukotic, R., Brodosi, L., Bernardi, M., & Andreone, P. (2014). Bone marrow derived stem cells for the treatment of end-stage liver disease. World Journal of Gastroenterology, 20(27), 9098–9105.
Porada, C. D., Atala, A. J., & Almeida-Porada, G. (2015). The hematopoietic system in the context of regenerative medicine. Methods, 99, 44–61.
Barker, N. (2014). Adult intestinal stem cells: critical drivers of epithelial homeostasis and regeneration. Nature Reviews Molecular Cell Biology, 15(1), 19–33.
Clevers, H. (2013). The intestinal crypt, a prototype stem cell compartment. Cell, 154(2), 274–284.
Stange, D. E., & Clevers, H. (2013). Concise review: the yin and yang of intestinal (cancer) stem cells and their progenitors. Stem Cells (Dayton, Ohio), 31(11), 2287–2295.
Vanuytsel, T., Senger, S., Fasano, A., & Shea-Donohue, T. (2013). Major signaling pathways in intestinal stem cells. Biochimica et Biophysica Acta, 1830(2), 2410–2426.
Sancho, R., Cremona, C. A., & Behrens, A. (2015). Stem cell and progenitor fate in the mammalian intestine: Notch and lateral inhibition in homeostasis and disease. EMBO Reports, 16(5), 571–581.
Tan, S., & Barker, N. (2015). Epithelial stem cells and intestinal cancer. Seminars in Cancer Biology, 32, 40–53.
Vermeulen, L., & Snippert, H. J. (2014). Stem cell dynamics in homeostasis and cancer of the intestine. Nature Reviews Cancer, 14(7), 468–480.
Zeuner, A., Todaro, M., Stassi, G., & De Maria, R. (2014). Colorectal cancer stem cells: from the crypt to the clinic. Cell Stem Cell, 15(6), 692–705.
Sakthianandeswaren, A., Christie, M., D’Andreti, C., Tsui, C., Jorissen, R. N., Li, S., et al. (2011). PHLDA1 expression marks the putative epithelial stem cells and contributes to intestinal tumorigenesis. Cancer Research, 71(10), 3709–3719.
Arwert, E. N., Hoste, E., & Watt, F. M. (2012). Epithelial stem cells, wound healing and cancer. Nature Reviews Cancer, 12(3), 170–180.
Blanpain, C., & Fuchs, E. (2014). Stem cell plasticity. Plasticity of epithelial stem cells in tissue regeneration. Science, 344(6189), 1242281.
Hsu, Y. C., Li, L., & Fuchs, E. (2014). Emerging interactions between skin stem cells and their niches. Nature Medicine, 20(8), 847–856.
Kretzschmar, K., Watt, F.M. (2014). Markers of epidermal stem cell subpopulations in adult mammalian skin. Cold Spring Harbor Perspectives in Medicine. doi:10.1101/cshperspect.a013631.
Mesa, K. R., Rompolas, P., & Greco, V. (2015). The dynamic Duo: niche/stem cell interdependency. Stem Cell Reports, 4(6), 961–966.
Plikus, M. V., Gay, D. L., Treffeisen, E., Wang, A., Supapannachart, R. J., & Cotsarelis, G. (2012). Epithelial stem cells and implications for wound repair. Seminars in Cell & Developmental Biology, 23(9), 946–953.
Rompolas, P., & Greco, V. (2014). Stem cell dynamics in the hair follicle niche. Seminars in Cell & Developmental Biology, 25–26, 34–42.
Ito, M., Liu, Y., Yang, Z., Nguyen, J., Liang, F., Morris, R. J., & Cotsarelis, G. (2005). Stem cells in the hair follicle bulge contribute to wound repair but not to homeostasis of the epidermis. Nature Medicine, 11(12), 1351–1354.
Mascre, G., Dekoninck, S., Drogat, B., Youssef, K. K., Brohee, S., Sotiropoulou, P. A., et al. (2012). Distinct contribution of stem and progenitor cells to epidermal maintenance. Nature, 489(7415), 257–262.
Page, M. E., Lombard, P., Ng, F., Gottgens, B., & Jensen, K. B. (2013). The epidermis comprises autonomous compartments maintained by distinct stem cell populations. Cell Stem Cell, 13(4), 471–482.
Tumbar, T., Guasch, G., Greco, V., Blanpain, C., Lowry, W. E., Rendl, M., & Fuchs, E. (2004). Defining the epithelial stem cell niche in skin. Science, 303(5656), 359–363.
Wu, X., Shen, Q. T., Oristian, D. S., Lu, C. P., Zheng, Q., Wang, H. W., & Fuchs, E. (2011). Skin stem cells orchestrate directional migration by regulating microtubule-ACF7 connections through GSK3beta. Cell, 144(3), 341–352.
Flores, I., Cayuela, M. L., & Blasco, M. A. (2005). Effects of telomerase and telomere length on epidermal stem cell behavior. Science, 309(5738), 1253–1256.
Chou, W. C., Takeo, M., Rabbani, P., Hu, H., Lee, W., Chung, Y. R., et al. (2013). Direct migration of follicular melanocyte stem cells to the epidermis after wounding or UVB irradiation is dependent on Mc1r signaling. Nature Medicine, 19(7), 924–929.
Almada, A. E., & Wagers, A. J. (2016). Molecular circuitry of stem cell fate in skeletal muscle regeneration, ageing and disease. Nature Reviews Molecular Cell Biology, 17(5), 267–279.
Blau, H. M., Cosgrove, B. D., & Ho, A. T. (2015). The central role of muscle stem cells in regenerative failure with aging. Nature Medicine, 21(8), 854–862.
Brack, A. S., & Munoz-Canoves, P. (2015). The ins and outs of muscle stem cell aging. Skeletal Muscle, 6, 1.
Cerletti, M., Shadrach, J. L., Jurga, S., Sherwood, R., & Wagers, A. J. (2008). Regulation and function of skeletal muscle stem cells. Cold Spring Harbor Symposia on Quantitative Biology, 73, 317–322.
Conboy, I. M., & Rando, T. A. (2005). Aging, stem cells and tissue regeneration: lessons from muscle. Cell Cycle, 4(3), 407–410.
Dumont, N. A., Bentzinger, C. F., Sincennes, M. C., & Rudnicki, M. A. (2015). Satellite cells and skeletal muscle regeneration. Comprehensive Physiology, 5(3), 1027–1059.
Sincennes, M. C., Brun, C. E., & Rudnicki, M. A. (2016). Concise review: epigenetic regulation of myogenesis in health and disease. Stem Cells Translational Medicine, 5(3), 282–290.
Tierney, M.T., Sacco, A. (2016). Satellite cell heterogeneity in skeletal muscle homeostasis. Trends in Cell Biology. doi:10.1016/j.tcb.2016.02.004.
Webster, M. T., Manor, U., Lippincott-Schwartz, J., & Fan, C. M. (2016). Intravital imaging reveals ghost fibers as architectural units guiding myogenic progenitors during regeneration. Cell Stem Cell, 18(2), 243–252.
Neuhaus, P., Oustanina, S., Loch, T., Kruger, M., Bober, E., Dono, R., et al. (2003). Reduced mobility of fibroblast growth factor (FGF)-deficient myoblasts might contribute to dystrophic changes in the musculature of FGF2/FGF6/mdx triple-mutant mice. Molecular and Cellular Biology, 23(17), 6037–6048.
Collins-Hooper, H., Woolley, T. E., Dyson, L., Patel, A., Potter, P., Baker, R. E., et al. (2012). Age-related changes in speed and mechanism of adult skeletal muscle stem cell migration. Stem Cells (Dayton, Ohio), 30(6), 1182–1195.
Bond, A. M., Ming, G. L., & Song, H. (2015). Adult mammalian neural stem cells and neurogenesis: five decades later. Cell Stem Cell, 17(4), 385–395.
Capilla-Gonzalez, V., Lavell, E., Quinones-Hinojosa, A., & Guerrero-Cazares, H. (2015). Regulation of subventricular zone-derived cells migration in the adult brain. Advances in Experimental Medicine and Biology, 853, 1–21.
De Filippis, L., & Binda, E. (2012). Concise review: self-renewal in the central nervous system: neural stem cells from embryo to adult. Stem Cells Translational Medicine, 1(4), 298–308.
Lim, D. A., & Alvarez-Buylla, A. (2014). Adult neural stem cells stake their ground. Trends in Neurosciences, 37(10), 563–571.
Maki, T., Liang, A. C., Miyamoto, N., Lo, E. H., & Arai, K. (2013). Mechanisms of oligodendrocyte regeneration from ventricular-subventricular zone-derived progenitor cells in white matter diseases. Frontiers in Cellular Neuroscience, 7, 275.
Merino, J. J., Bellver-Landete, V., Oset-Gasque, M. J., & Cubelos, B. (2014). Review: CXCR4/CXCR7 molecular involvement in neuronal and neural progenitor migration: focus in CNS repair. Journal of Cellular Physiology, 230(1), 27–42.
Ibrahim, S., Hu, W., Wang, X., Gao, X., He, C., & Chen, J. (2016). Traumatic brain injury causes aberrant migration of adult-born neurons in the hippocampus. Scientific Reports, 6, 21793.
Capilla-Gonzalez, V., Herranz-Perez, V., & Garcia-Verdugo, J. M. (2015). The aged brain: genesis and fate of residual progenitor cells in the subventricular zone. Frontiers in Cellular Neuroscience, 9, 365.
Aboody, K. S., Brown, A., Rainov, N. G., Bower, K. A., Liu, S., Yang, W., et al. (2000). Neural stem cells display extensive tropism for pathology in adult brain: evidence from intracranial gliomas. Proceedings of the National Academy of Sciences of the United States of America, 97(23), 12846–12851.
Carney, B. J., & Shah, K. (2011). Migration and fate of therapeutic stem cells in different brain disease models. Neuroscience, 197, 37–47.
Vishwakarma, S. K., Bardia, A., Tiwari, S. K., Paspala, S. A., & Khan, A. A. (2014). Current concept in neural regeneration research: NSCs isolation, characterization and transplantation in various neurodegenerative diseases and stroke: A review. Journal of Advanced Research, 5(3), 277–294.
Chou, C. H., Fan, H. C., & Hueng, D. Y. (2015). Potential of neural stem cell-based therapy for Parkinson’s disease. Parkinson’s Disease, 2015, 571475.
Dunnett, S. B., & Rosser, A. E. (2014). Challenges for taking primary and stem cells into clinical neurotransplantation trials for neurodegenerative disease. Neurobiology of Disease, 61, 79–89.
Goldman, S. A. (2016). Stem and progenitor cell-based therapy of the central nervous system: hopes, hype, and wishful thinking. Cell Stem Cell, 18(2), 174–188.
Bentzinger, C. F., Wang, Y. X., Dumont, N. A., & Rudnicki, M. A. (2013). Cellular dynamics in the muscle satellite cell niche. EMBO Reports, 14(12), 1062–1072.
Bjornsson, C. S., Apostolopoulou, M., Tian, Y., & Temple, S. (2015). It takes a village: constructing the neurogenic niche. Developmental Cell, 32(4), 435–446.
Choi, H. R., Byun, S. Y., Kwon, S. H., & Park, K. C. (2015). Niche interactions in epidermal stem cells. World Journal of Stem Cells, 7(2), 495–501.
DeCarolis, N.A., Kirby, E.D., Wyss-Coray, T., Palmer, T.D. (2015). The role of the microenvironmental niche in declining stem-cell functions associated with biological aging. Cold Spring Harbor Perspectives in Medicine. doi:10.1101/cshperspect.a025874.
Lane, S. W., Williams, D. A., & Watt, F. M. (2014). Modulating the stem cell niche for tissue regeneration. Nature Biotechnology, 32(8), 795–803.
Tan, D. W., & Barker, N. (2014). Intestinal stem cells and their defining niche. Current Topics in Developmental Biology, 107, 77–107.
Thomas, K., Engler, A. J., & Meyer, G. A. (2015). Extracellular matrix regulation in the muscle satellite cell niche. Connective Tissue Research, 56(1), 1–8.
Bear, J. E., & Haugh, J. M. (2014). Directed migration of mesenchymal cells: where signaling and the cytoskeleton meet. Current Opinion in Cell Biology, 30, 74–82.
Sarris, M., & Sixt, M. (2015). Navigating in tissue mazes: chemoattractant interpretation in complex environments. Current Opinion in Cell Biology, 36, 93–102.
Wang, J., & Knaut, H. (2014). Chemokine signaling in development and disease. Development, 141(22), 4199–4205.
Karpova, D., & Bonig, H. (2015). Concise review: CXCR4/CXCL12 signaling in immature hematopoiesis--lessons from pharmacological and genetic models. Stem Cells (Dayton, Ohio), 33(8), 2391–2399.
Nagasawa, T. (2015). CXCL12/SDF-1 and CXCR4. Frontiers in Immunology, 6, 301.
Peled, A., Petit, I., Kollet, O., Magid, M., Ponomaryov, T., Byk, T., et al. (1999). Dependence of human stem cell engraftment and repopulation of NOD/SCID mice on CXCR4. Science, 283(5403), 845–848.
Gallagher, K. A., Liu, Z. J., Xiao, M., Chen, H., Goldstein, L. J., Buerk, D. G., et al. (2007). Diabetic impairments in NO-mediated endothelial progenitor cell mobilization and homing are reversed by hyperoxia and SDF-1 alpha. The Journal of Clinical Investigation, 117(5), 1249–1259.
Jaerve, A., Schira, J., & Muller, H. W. (2012). Concise review: the potential of stromal cell-derived factor 1 and its receptors to promote stem cell functions in spinal cord repair. Stem Cells Translational Medicine, 1(10), 732–739.
Pan, S., Dangaria, S., Gopinathan, G., Yan, X., Lu, X., Kolokythas, A., et al. (2013). SCF promotes dental pulp progenitor migration, neovascularization, and collagen remodeling - potential applications as a homing factor in dental pulp regeneration. Stem Cell Reviews, 9(5), 655–667.
Jalili, A., Shirvaikar, N., Marquez-Curtis, L. A., Turner, A. R., & Janowska-Wieczorek, A. (2010). The HGF/c-Met axis synergizes with G-CSF in the mobilization of hematopoietic stem/progenitor cells. Stem Cells and Development, 19(8), 1143–1151.
Tesio, M., Golan, K., Corso, S., Giordano, S., Schajnovitz, A., Vagima, Y., et al. (2011). Enhanced c-Met activity promotes G-CSF-induced mobilization of hematopoietic progenitor cells via ROS signaling. Blood, 117(2), 419–428.
Bischoff, R. (1997). Chemotaxis of skeletal muscle satellite cells. Developmental Dynamics: an Official Publication of the American Association of Anatomists, 208(4), 505–515.
Ishido, M., & Kasuga, N. (2012). In vivo real-time imaging of exogenous HGF-triggered cell migration in rat intact soleus muscles. Acta Histochemica et Cytochemica, 45(3), 193–199.
Li, J., & Johnson, S. E. (2013). Ephrin-A5 promotes bovine muscle progenitor cell migration before mitotic activation. Journal of Animal Science, 91(3), 1086–1093.
Siegel, A. L., Atchison, K., Fisher, K. E., Davis, G. E., & Cornelison, D. D. (2009). 3D timelapse analysis of muscle satellite cell motility. Stem Cells (Dayton, Ohio), 27(10), 2527–2538.
Webster, M. T., & Fan, C. M. (2013). c-MET regulates myoblast motility and myocyte fusion during adult skeletal muscle regeneration. PloS One, 8(11), e81757.
Binder, B. Y., Williams, P. A., Silva, E. A., & Leach, J. K. (2015). Lysophosphatidic acid and sphingosine-1-phosphate: a concise review of biological function and applications for tissue engineering. Tissue Engineering. Part B, Reviews, 21(6), 531–542.
Kunkel, G. T., Maceyka, M., Milstien, S., & Spiegel, S. (2013). Targeting the sphingosine-1-phosphate axis in cancer, inflammation and beyond. Nature Reviews Drug Discovery, 12(9), 688–702.
Maceyka, M., Harikumar, K. B., Milstien, S., & Spiegel, S. (2012). Sphingosine-1-phosphate signaling and its role in disease. Trends in Cell Biology, 22(1), 50–60.
Proia, R. L., & Hla, T. (2015). Emerging biology of sphingosine-1-phosphate: its role in pathogenesis and therapy. The Journal of Clinical Investigation, 125(4), 1379–1387.
Ratajczak, M. Z., Suszynska, M., Borkowska, S., Ratajczak, J., & Schneider, G. (2014). The role of sphingosine-1 phosphate and ceramide-1 phosphate in trafficking of normal stem cells and cancer cells. Expert Opinion on Therapeutic Targets, 18(1), 95–107.
Tsujiuchi, T., Hirane, M., Dong, Y., & Fukushima, N. (2014). Diverse effects of LPA receptors on cell motile activities of cancer cells. Journal of Receptor and Signal Transduction Research, 34(3), 149–153.
Walker, T. L., Overall, R. W., Vogler, S., Sykes, A. M., Ruhwald, S., Lasse, D., et al. (2016). Lysophosphatidic acid receptor is a functional marker of adult hippocampal precursor cells. Stem Cell Reports, 6(4), 552–565.
Golan, K., Kollet, O., & Lapidot, T. (2013). Dynamic cross talk between S1P and CXCL12 regulates hematopoietic stem cells migration, development and bone remodeling. Pharmaceuticals (Basel, Switzerland), 6(9), 1145–1169.
Pebay, A., Bonder, C. S., & Pitson, S. M. (2007). Stem cell regulation by lysophospholipids. Prostaglandins & Other Lipid Mediators, 84(3–4), 83–97.
Adamiak, M., Borkowska, S., Wysoczynski, M., Suszynska, M., Kucia, M., Rokosh, G., et al. (2015). Evidence for the involvement of sphingosine-1-phosphate in the homing and engraftment of hematopoietic stem cells to bone marrow. Oncotarget, 6(22), 18819–18828.
Bendall, L. J., & Basnett, J. (2013). Role of sphingosine 1-phosphate in trafficking and mobilization of hematopoietic stem cells. Current Opinion in Hematology, 20(4), 281–288.
Golan, K., Vagima, Y., Ludin, A., Itkin, T., Cohen-Gur, S., Kalinkovich, A., et al. (2012). S1P promotes murine progenitor cell egress and mobilization via S1P1-mediated ROS signaling and SDF-1 release. Blood, 119(11), 2478–2488.
Karapetyan, A. V., Klyachkin, Y. M., Selim, S., Sunkara, M., Ziada, K. M., Cohen, D. A., et al. (2013). Bioactive lipids and cationic antimicrobial peptides as new potential regulators for trafficking of bone marrow-derived stem cells in patients with acute myocardial infarction. Stem Cells and Development, 22(11), 1645–1656.
Calise, S., Blescia, S., Cencetti, F., Bernacchioni, C., Donati, C., & Bruni, P. (2012). Sphingosine 1-phosphate stimulates proliferation and migration of satellite cells: role of S1P receptors. Biochimica et Biophysica Acta, 1823(2), 439–450.
Cencetti, F., Bruno, G., Blescia, S., Bernacchioni, C., Bruni, P., & Donati, C. (2014). Lysophosphatidic acid stimulates cell migration of satellite cells. A role for the sphingosine kinase/sphingosine 1-phosphate axis. The FEBS Journal, 281(19), 4467–4478.
Ishii, M., Egen, J. G., Klauschen, F., Meier-Schellersheim, M., Saeki, Y., Vacher, J., Proia, R. L., & Germain, R. N. (2009). Sphingosine-1-phosphate mobilizes osteoclast precursors and regulates bone homeostasis. Nature, 458(7237), 524–528.
Ishii, M., Kikuta, J., Shimazu, Y., Meier-Schellersheim, M., & Germain, R. N. (2010). Chemorepulsion by blood S1P regulates osteoclast precursor mobilization and bone remodeling in vivo. The Journal of Experimental Medicine, 207(13), 2793–2798.
Novgorodov, A. S., El-Alwani, M., Bielawski, J., Obeid, L. M., & Gudz, T. I. (2007). Activation of sphingosine-1-phosphate receptor S1P5 inhibits oligodendrocyte progenitor migration. FASEB Journal: Official Publication of the Federation of American Societies for Experimental Biology, 21(7), 1503–1514.
Kimura, A., Ohmori, T., Kashiwakura, Y., Ohkawa, R., Madoiwa, S., Mimuro, J., et al. (2008). Antagonism of sphingosine 1-phosphate receptor-2 enhances migration of neural progenitor cells toward an area of brain. Stroke; A Journal of Cerebral Circulation, 39(12), 3411–3417.
Blanc, C. A., Grist, J. J., Rosen, H., Sears-Kraxberger, I., Steward, O., & Lane, T. E. (2015). Sphingosine-1-phosphate receptor antagonism enhances proliferation and migration of engrafted neural progenitor cells in a model of viral-induced demyelination. The American Journal of Pathology, 185(10), 2819–2832.
Boyd, A. W., Bartlett, P. F., & Lackmann, M. (2014). Therapeutic targeting of EPH receptors and their ligands. Nature Reviews Drug Discovery, 13(1), 39–62.
Coulthard, M. G., Morgan, M., Woodruff, T. M., Arumugam, T. V., Taylor, S. M., Carpenter, T. C., et al. (2012). Eph/Ephrin signaling in injury and inflammation. The American Journal of Pathology, 181(5), 1493–1503.
Gucciardo, E., Sugiyama, N., & Lehti, K. (2014). Eph- and ephrin-dependent mechanisms in tumor and stem cell dynamics. Cellular and Molecular Life Sciences: CMLS, 71(19), 3685–3710.
Kania, A., & Klein, R. (2016). Mechanisms of ephrin-Eph signalling in development, physiology and disease. Nature Reviews Molecular Cell Biology, 17(4), 240–256.
Klein, R., & Kania, A. (2014). Ephrin signalling in the developing nervous system. Current Opinion in Neurobiology, 27C, 16–24.
Laussu, J., Khuong, A., Gautrais, J., & Davy, A. (2014). Beyond boundaries--Eph:ephrin signaling in neurogenesis. Cell Adhesion & Migration, 8(4), 349–359.
Lisabeth, E.M., Falivelli, G., Pasquale, E.B. (2013). Eph receptor signaling and ephrins. Cold Spring Harbor Perspectives in Biology. doi:10.1101/cshperspect.a009159.
Nikolov, D. B., Xu, K., & Himanen, J. P. (2014). Homotypic receptor-receptor interactions regulating Eph signaling. Cell Adhesion & Migration, 8(4), 360–365.
Park, I., & Lee, H. S. (2015). EphB/ephrinB signaling in cell adhesion and migration. Molecules and Cells, 38(1), 14–19.
Pasquale, E. B. (2010). Eph receptors and ephrins in cancer: bidirectional signalling and beyond. Nature Reviews Cancer, 10(3), 165–180.
Pitulescu, M. E., & Adams, R. H. (2010). Eph/ephrin molecules--a hub for signaling and endocytosis. Genes & Development, 24(22), 2480–2492.
Wilkinson, D. G. (2014). Regulation of cell differentiation by Eph receptor and ephrin signaling. Cell Adhesion & Migration, 8(4), 339–348.
Ting, M. J., Day, B. W., Spanevello, M. D., & Boyd, A. W. (2010). Activation of ephrin A proteins influences hematopoietic stem cell adhesion and trafficking patterns. Experimental Hematology, 38(11), 1087–1098.
Nguyen, T.M., Arthur, A., Gronthos, S. (2016). The role of Eph/ephrin molecules in stromal-hematopoietic interactions. International Journal of Hematology, 103(2), 145–154.
Nguyen, T. M., Arthur, A., Panagopoulos, R., Paton, S., Hayball, J. D., Zannettino, A. C., et al. (2015). EphB4 expressing stromal cells exhibit an enhanced capacity for hematopoietic stem cell maintenance. Stem Cells (Dayton, Ohio), 33(9), 2838–2849.
Okubo, T., Yanai, N., & Obinata, M. (2006). Stromal cells modulate ephrinB2 expression and transmigration of hematopoietic cells. Experimental Hematology, 34(3), 330–338.
Stokowski, A., Shi, S., Sun, T., Bartold, P. M., Koblar, S. A., & Gronthos, S. (2007). EphB/ephrin-B interaction mediates adult stem cell attachment, spreading, and migration: implications for dental tissue repair. Stem Cells (Dayton, Ohio), 25(1), 156–164.
Arthur, A., Koblar, S., Shi, S., & Gronthos, S. (2009). Eph/ephrinB mediate dental pulp stem cell mobilization and function. Journal of Dental Research, 88(9), 829–834.
Conover, J. C., Doetsch, F., Garcia-Verdugo, J. M., Gale, N. W., Yancopoulos, G. D., & Alvarez-Buylla, A. (2000). Disruption of Eph/ephrin signaling affects migration and proliferation in the adult subventricular zone. Nature Neuroscience, 3(11), 1091–1097.
Catchpole, T., & Henkemeyer, M. (2011). EphB2 tyrosine kinase-dependent forward signaling in migration of neuronal progenitors that populate and form a distinct region of the dentate niche. Journal of Neuroscience, 31(32), 11472–11483.
Chumley, M. J., Catchpole, T., Silvany, R. E., Kernie, S. G., & Henkemeyer, M. (2007). EphB receptors regulate stem/progenitor cell proliferation, migration, and polarity during hippocampal neurogenesis. Journal of Neuroscience, 27(49), 13481–13490.
Holmberg, J., Armulik, A., Senti, K. A., Edoff, K., Spalding, K., Momma, S., et al. (2005). Ephrin-A2 reverse signaling negatively regulates neural progenitor proliferation and neurogenesis. Genes & Development, 19(4), 462–471.
Parrinello, S., Napoli, I., Ribeiro, S., Wingfield Digby, P., Fedorova, M., Parkinson, D. B., et al. (2010). EphB signaling directs peripheral nerve regeneration through Sox2-dependent Schwann cell sorting. Cell, 143(1), 145–155.
Stark, D. A., Karvas, R. M., Siegel, A. L., & Cornelison, D. D. (2011). Eph/ephrin interactions modulate muscle satellite cell motility and patterning. Development, 138(24), 5279–5289.
Gu, J. M., Wang, D. J., Peterson, J. M., Shintaku, J., Liyanarachchi, S., Coppola, V., et al. (2016). An NF-kappaB - EphrinA5-Dependent Communication between NG2(+) Interstitial Cells and Myoblasts Promotes Muscle Growth in Neonates. Developmental Cell, 36(2), 215–224.
Goichberg, P., Bai, Y., D’Amario, D., Ferreira-Martins, J., Fiorini, C., Zheng, H., et al. (2011). The ephrin A1-EphA2 system promotes cardiac stem cell migration after infarction. Circulation Research, 108(9), 1071–1083.
Goichberg, P., Kannappan, R., Cimini, M., Bai, Y., Sanada, F., Sorrentino, A., et al. (2013). Age-associated defects in EphA2 signaling impair the migration of human cardiac progenitor cells. Circulation, 128(20), 2211–2223.
Dries, J. L., Kent, S. D., & Virag, J. A. (2011). Intramyocardial administration of chimeric ephrinA1-Fc promotes tissue salvage following myocardial infarction in mice. The Journal of Physiology, 589(Pt 7), 1725–1740.
DuSablon, A., Kent, S., Coburn, A., & Virag, J. (2014). EphA2-receptor deficiency exacerbates myocardial infarction and reduces survival in hyperglycemic mice. Cardiovascular Diabetology, 13, 114.
O’Neal, W. T., Griffin, W. F., Kent, S. D., Faiz, F., Hodges, J., Vuncannon, J., & Virag, J. A. (2014). Deletion of the EphA2 receptor exacerbates myocardial injury and the progression of ischemic cardiomyopathy. Frontiers in Physiology, 5, 132.
Popov, C., Kohler, J., & Docheva, D. (2015). Activation of EphA4 and EphB2 Reverse Signaling Restores the Age-Associated Reduction of Self-Renewal, Migration, and Actin Turnover in Human Tendon Stem/Progenitor Cells. Frontiers in Aging Neuroscience, 7, 246.
Batlle, E., Henderson, J. T., Beghtel, H., van den Born, M. M., Sancho, E., Huls, G., et al. (2002). Beta-catenin and TCF mediate cell positioning in the intestinal epithelium by controlling the expression of EphB/ephrinB. Cell, 111(2), 251–263.
Genander, M., & Frisen, J. (2010). Eph receptors tangled up in two: Independent control of cell positioning and proliferation. Cell Cycle, 9(10), 1865–1866.
Genander, M. (2012). Eph and ephrins in epithelial stem cell niches and cancer. Cell Adhesion & Migration, 6(2), 126–130.
Holmberg, J., Genander, M., Halford, M. M., Anneren, C., Sondell, M., Chumley, M. J., et al. (2006). EphB receptors coordinate migration and proliferation in the intestinal stem cell niche. Cell, 125(6), 1151–1163.
Perez White, B. E., & Getsios, S. (2014). Eph receptor and ephrin function in breast, gut, and skin epithelia. Cell Adhesion & Migration, 8(4), 327–338.
Wijeratne, D. T., Rodger, J., Wood, F. M., & Fear, M. W. (2016). The role of Eph receptors and Ephrins in the skin. International Journal of Dermatology, 55(1), 3–10.
Genander, M., Halford, M. M., Xu, N. J., Eriksson, M., Yu, Z., Qiu, Z., et al. (2009). Dissociation of EphB2 signaling pathways mediating progenitor cell proliferation and tumor suppression. Cell, 139(4), 679–692.
Miao, H., Nickel, C. H., Cantley, L. G., Bruggeman, L. A., Bennardo, L. N., & Wang, B. (2003). EphA kinase activation regulates HGF-induced epithelial branching morphogenesis. The Journal of Cell Biology, 162(7), 1281–1292.
Lu, Q., Sun, E. E., Klein, R. S., & Flanagan, J. G. (2001). Ephrin-B reverse signaling is mediated by a novel PDZ-RGS protein and selectively inhibits G protein-coupled chemoattraction. Cell, 105(1), 69–79.
Vaught, D., Chen, J., & Brantley-Sieders, D. M. (2009). Regulation of mammary gland branching morphogenesis by EphA2 receptor tyrosine kinase. Molecular Biology of the Cell, 20(10), 2572–2581.
Dejana, E., & Giampietro, C. (2012). Vascular endothelial-cadherin and vascular stability. Current Opinion in Hematology, 19(3), 218–223.
Geiger, B., & Ayalon, O. (1992). Cadherins. Annual Review of Cell Biology, 8, 307–332.
Lecuit, T., & Yap, A. S. (2015). E-cadherin junctions as active mechanical integrators in tissue dynamics. Nature Cell Biology, 17(5), 533–539.
Miyamoto, Y., Sakane, F., & Hashimoto, K. (2015). N-cadherin-based adherens junction regulates the maintenance, proliferation, and differentiation of neural progenitor cells during development. Cell Adhesion & Migration, 9(3), 183–192.
van Roy, F. (2014). Beyond E-cadherin: roles of other cadherin superfamily members in cancer. Nature Reviews Cancer, 14(2), 121–134.
Chen, J. Y., Miyanishi, M., Wang, S. K., Yamazaki, S., Sinha, R., Kao, K. S., et al. (2016). Hoxb5 marks long-term haematopoietic stem cells and reveals a homogenous perivascular niche. Nature, 530(7589), 223–227.
Lay, K., Kume, T., Fuchs, E. (2016). FOXC1 maintains the hair follicle stem cell niche and governs stem cell quiescence to preserve long-term tissue-regenerating potential. Proceedings of the National Academy of Sciences of the United States of America, 13(11), E1506–E1515.
Porlan, E., Marti-Prado, B., Morante-Redolat, J. M., Consiglio, A., Delgado, A. C., Kypta, R., et al. (2014). MT5-MMP regulates adult neural stem cell functional quiescence through the cleavage of N-cadherin. Nature Cell Biology, 16(7), 629–638.
Zhang, J., Niu, C., Ye, L., Huang, H., He, X., Tong, W. G., et al. (2003). Identification of the haematopoietic stem cell niche and control of the niche size. Nature, 425(6960), 836–841.
Klingener, M., Chavali, M., Singh, J., McMillan, N., Coomes, A., Dempsey, P. J., et al. (2014). N-cadherin promotes recruitment and migration of neural progenitor cells from the SVZ neural stem cell niche into demyelinated lesions. Journal of Neuroscience, 34(29), 9590–9606.
Gonzalez-Nieto, D., Chang, K. H., Fasciani, I., Nayak, R., Fernandez-Garcia, L., Barrio, L. C., & Cancelas, J. A. (2015). Connexins: intercellular signal transmitters in lymphohematopoietic tissues. International Review of Cell and Molecular Biology, 318, 27–62.
Meier, C., & Rosenkranz, K. (2014). Cx43 expression and function in the nervous system-implications for stem cell mediated regeneration. Frontiers in Physiology, 5, 106.
Salmina, A. B., Morgun, A. V., Kuvacheva, N. V., Lopatina, O. L., Komleva, Y. K., Malinovskaya, N. A., & Pozhilenkova, E. A. (2014). Establishment of neurogenic microenvironment in the neurovascular unit: the connexin 43 story. Reviews in the Neurosciences, 25(1), 97–111.
Gonzalez-Nieto, D., Li, L., Kohler, A., Ghiaur, G., Ishikawa, E., Sengupta, A., et al. (2012). Connexin-43 in the osteogenic BM niche regulates its cellular composition and the bidirectional traffic of hematopoietic stem cells and progenitors. Blood, 119(22), 5144–5154.
Schajnovitz, A., Itkin, T., D’Uva, G., Kalinkovich, A., Golan, K., Ludin, A., et al. (2011). CXCL12 secretion by bone marrow stromal cells is dependent on cell contact and mediated by connexin-43 and connexin-45 gap junctions. Nature Immunology, 12(5), 391–398.
Papayannopoulou, T. (2003). Bone marrow homing: the players, the playfield, and their evolving roles. Current Opinion in Hematology, 10(3), 214–219.
Sahin, A. O., & Buitenhuis, M. (2012). Molecular mechanisms underlying adhesion and migration of hematopoietic stem cells. Cell Adhesion & Migration, 6(1), 39–48.
Leiva, M., Quintana, J. A., Ligos, J. M., & Hidalgo, A. (2016). Haematopoietic ESL-1 enables stem cell proliferation in the bone marrow by limiting TGFbeta availability. Nature Communications, 7, 10222.
Winkler, I. G., Barbier, V., Nowlan, B., Jacobsen, R. N., Forristal, C. E., Patton, J. T., et al. (2012). Vascular niche E-selectin regulates hematopoietic stem cell dormancy, self renewal and chemoresistance. Nature Medicine, 18(11), 1651–1657.
Chavakis, E., & Dimmeler, S. (2011). Homing of progenitor cells to ischemic tissues. Antioxidants & Redox Signaling, 15(4), 967–980.
Sackstein, R. (2011). The biology of CD44 and HCELL in hematopoiesis: the ‘step 2-bypass pathway’ and other emerging perspectives. Current Opinion in Hematology, 18(4), 239–248.
Sackstein, R. (2012). Engineering cellular trafficking via glycosyltransferase-programmed stereosubstitution. Annals of the New York Academy of Sciences, 1253, 193–200.
Abdi, R., Moore, R., Sakai, S., Donnelly, C. B., Mounayar, M., & Sackstein, R. (2015). HCELL expression on murine MSC licenses pancreatotropism and confers durable reversal of autoimmune diabetes in NOD mice. Stem Cells (Dayton, Ohio), 33(5), 1523–1531.
Merzaban, J. S., Imitola, J., Starossom, S. C., Zhu, B., Wang, Y., Lee, J., et al. (2015). Cell surface glycan engineering of neural stem cells augments neurotropism and improves recovery in a murine model of multiple sclerosis. Glycobiology, 25(12), 1392–1409.
Akhmanova, M., Osidak, E., Domogatsky, S., Rodin, S., & Domogatskaya, A. (2015). Physical, spatial, and molecular aspects of extracellular matrix of in vivo niches and artificial scaffolds relevant to stem cells research. Stem Cells International, 2015, 167025.
Frantz, C., Stewart, K. M., & Weaver, V. M. (2010). The extracellular matrix at a glance. Journal of Cell Science, 123(Pt 24), 4195–4200.
Freedman, B. R., Bade, N. D., Riggin, C. N., Zhang, S., Haines, P. G., Ong, K. L., & Janmey, P. A. (2015). The (dys)functional extracellular matrix. Biochimica et Biophysica Acta, 1853(11 Pt B), 3153–3164.
Handorf, A. M., Zhou, Y., Halanski, M. A., & Li, W. J. (2015). Tissue stiffness dictates development, homeostasis, and disease progression. Organogenesis, 11(1), 1–15.
Hynes, R. O., & Naba, A. (2012). Overview of the matrisome--an inventory of extracellular matrix constituents and functions. Cold Spring Harbor Perspectives in Biology, 4(1), a004903.
Theocharis, A. D., Skandalis, S. S., Gialeli, C., & Karamanos, N. K. (2016). Extracellular matrix structure. Advanced Drug Delivery Reviews, 97, 4–27.
Daley, W. P., & Yamada, K. M. (2013). ECM-modulated cellular dynamics as a driving force for tissue morphogenesis. Current Opinion in Genetics & Development, 23(4), 408–414.
Happe, C. L., & Engler, A. J. (2016). Mechanical forces reshape differentiation cues that guide cardiomyogenesis. Circulation Research, 118(2), 296–310.
Mammoto, T., Mammoto, A., & Ingber, D. E. (2013). Mechanobiology and developmental control. Annual Review of Cell and Developmental Biology, 29, 27–61.
Walters, N. J., & Gentleman, E. (2015). Evolving insights in cell-matrix interactions: elucidating how non-soluble properties of the extracellular niche direct stem cell fate. Acta Biomaterialia, 11, 3–16.
Chandra, P., & Lee, S. J. (2015). Synthetic extracellular microenvironment for modulating stem cell behaviors. Biomarker Insights, 10(Suppl 1), 105–116.
Chen, W., Shao, Y., Li, X., Zhao, G., & Fu, J. (2014). Nanotopographical surfaces for stem cell fate control: engineering mechanobiology from the bottom. Nano Today, 9(6), 759–784.
Dalby, M. J., Gadegaard, N., & Oreffo, R. O. (2014). Harnessing nanotopography and integrin-matrix interactions to influence stem cell fate. Nature Materials, 13(6), 558–569.
Dingal, P. C., & Discher, D. E. (2014). Combining insoluble and soluble factors to steer stem cell fate. Nature Materials, 13(6), 532–537.
Faissner, A., & Reinhard, J. (2015). The extracellular matrix compartment of neural stem and glial progenitor cells. Glia, 63(8), 1330–1349.
Humphrey, J. D., Dufresne, E. R., & Schwartz, M. A. (2014). Mechanotransduction and extracellular matrix homeostasis. Nature Reviews Molecular Cell Biology, 15(12), 802–812.
Huttenlocher, A., & Horwitz, A. R. (2011). Integrins in cell migration. Cold Spring Harbor Perspectives in Biology, 3(9), a005074.
Hynes, R. O. (2002). Integrins: bidirectional, allosteric signaling machines. Cell, 110(6), 673–687.
Miranti, C. K., & Brugge, J. S. (2002). Sensing the environment: a historical perspective on integrin signal transduction. Nature Cell Biology, 4(4), E83–E90.
Schwartz, M. A. (2010). Integrins and extracellular matrix in mechanotransduction. Cold Spring Harbor Perspectives in Biology, 2(12), a005066.
Winograd-Katz, S. E., Fassler, R., Geiger, B., & Legate, K. R. (2014). The integrin adhesome: from genes and proteins to human disease. Nature Reviews Molecular Cell Biology, 15(4), 273–288.
Wolfenson, H., Lavelin, I., & Geiger, B. (2013). Dynamic regulation of the structure and functions of integrin adhesions. Developmental Cell, 24(5), 447–458.
Milner, R., Edwards, G., Streuli, C., & Ffrench-Constant, C. (1996). A role in migration for the alpha V beta 1 integrin expressed on oligodendrocyte precursors. Journal of Neuroscience, 16(22), 7240–7252.
Ernst, N., Yay, A., Biro, T., Tiede, S., Humphries, M., Paus, R., & Kloepper, J. E. (2013). beta1 integrin signaling maintains human epithelial progenitor cell survival in situ and controls proliferation, apoptosis and migration of their progeny. PloS One, 8(12), e84356.
Schofield, K. P., Rushton, G., Humphries, M. J., Dexter, T. M., & Gallagher, J. T. (1997). Influence of interleukin-3 and other growth factors on alpha4beta1 integrin-mediated adhesion and migration of human hematopoietic progenitor cells. Blood, 90(5), 1858–1866.
Strobel, E. S., Mobest, D., von Kleist, S., Dangel, M., Ries, S., Mertelsmann, R., & Henschler, R. (1997). Adhesion and migration are differentially regulated in hematopoietic progenitor cells by cytokines and extracellular matrix. Blood, 90(9), 3524–3532.
Gu, Y. C., Kortesmaa, J., Tryggvason, K., Persson, J., Ekblom, P., Jacobsen, S. E., & Ekblom, M. (2003). Laminin isoform-specific promotion of adhesion and migration of human bone marrow progenitor cells. Blood, 101(3), 877–885.
Muth, C. A., Steinl, C., Klein, G., & Lee-Thedieck, C. (2013). Regulation of hematopoietic stem cell behavior by the nanostructured presentation of extracellular matrix components. PloS One, 8(2), e54778.
Bershadsky, A., Kozlov, M., & Geiger, B. (2006). Adhesion-mediated mechanosensitivity: a time to experiment, and a time to theorize. Current Opinion in Cell Biology, 18(5), 472–481.
Doyle, A.D., Yamada, K.M. (2016). Mechanosensing via cell-matrix adhesions in 3D microenvironments. Experimental Cell Research, 343(1), 60–66.
Geiger, B., Spatz, J. P., & Bershadsky, A. D. (2009). Environmental sensing through focal adhesions. Nature Reviews Molecular Cell Biology, 10(1), 21–33.
Bellas, E., & Chen, C. S. (2014). Forms, forces, and stem cell fate. Current Opinion in Cell Biology, 31, 92–97.
Holst, J., Watson, S., Lord, M. S., Eamegdool, S. S., Bax, D. V., Nivison-Smith, L. B., et al. (2010). Substrate elasticity provides mechanical signals for the expansion of hemopoietic stem and progenitor cells. Nature Biotechnology, 28(10), 1123–1128.
Lee-Thedieck, C., Rauch, N., Fiammengo, R., Klein, G., & Spatz, J. P. (2012). Impact of substrate elasticity on human hematopoietic stem and progenitor cell adhesion and motility. Journal of Cell Science, 125(Pt 16), 3765–3775.
Ehrbar, M., Sala, A., Lienemann, P., Ranga, A., Mosiewicz, K., Bittermann, A., et al. (2011). Elucidating the role of matrix stiffness in 3D cell migration and remodeling. Biophysical Journal, 100(2), 284–293.
Yang, K., Jung, K., Ko, E., Kim, J., Park, K. I., & Cho, S. W. (2013). Nanotopographical manipulation of focal adhesion formation for enhanced differentiation of human neural stem cells. ACS Applied Materials & Interfaces, 5(21), 10529–10540.
Magnusson, A. K., Linderholm, P., Vieider, C., Ulfendahl, M., & Erlandsson, A. (2008). Surface protein patterns govern morphology, proliferation, and expression of cellular markers but have no effect on physiological properties of cortical precursor cells. Journal of Neuroscience Research, 86(11), 2363–2375.
Ruiz, A., Buzanska, L., Gilliland, D., Rauscher, H., Sirghi, L., Sobanski, T., et al. (2008). Micro-stamped surfaces for the patterned growth of neural stem cells. Biomaterials, 29(36), 4766–4774.
Joo, S., Kim, J. Y., Lee, E., Hong, N., Sun, W., & Nam, Y. (2015). Effects of ECM protein micropatterns on the migration and differentiation of adult neural stem cells. Scientific Reports, 5, 13043.
DeMali, K. A., Sun, X., & Bui, G. A. (2014). Force transmission at cell-cell and cell-matrix adhesions. Biochemistry, 53(49), 7706–7717.
Gasparski, A. N., & Beningo, K. A. (2015). Mechanoreception at the cell membrane: More than the integrins. Archives of Biochemistry and Biophysics, 586, 20–26.
Priya, R., & Yap, A. S. (2015). Active tension: the role of cadherin adhesion and signaling in generating junctional contractility. Current Topics in Developmental Biology, 112, 65–102.
Zoller, M. (2015). CD44, hyaluronan, the hematopoietic stem cell, and leukemia-initiating cells. Frontiers in Immunology, 6, 235.
Avigdor, A., Goichberg, P., Shivtiel, S., Dar, A., Peled, A., Samira, S., et al. (2004). CD44 and hyaluronic acid cooperate with SDF-1 in the trafficking of human CD34+ stem/progenitor cells to bone marrow. Blood, 103(8), 2981–2989.
Vagima, Y., Avigdor, A., Goichberg, P., Shivtiel, S., Tesio, M., Kalinkovich, A., et al. (2009). MT1-MMP and RECK are involved in human CD34+ progenitor cell retention, egress, and mobilization. The Journal of Clinical Investigation, 119(3), 492–503.
Healy, L., May, G., Gale, K., Grosveld, F., Greaves, M., & Enver, T. (1995). The stem cell antigen CD34 functions as a regulator of hemopoietic cell adhesion. Proceedings of the National Academy of Sciences of the United States of America, 92(26), 12240–12244.
Nielsen, J. S., & McNagny, K. M. (2009). CD34 is a key regulator of hematopoietic stem cell trafficking to bone marrow and mast cell progenitor trafficking in the periphery. Microcirculation, 16(6), 487–496.
Alfaro, L. A., Dick, S. A., Siegel, A. L., Anonuevo, A. S., McNagny, K. M., Megeney, L. A., et al. (2011). CD34 promotes satellite cell motility and entry into proliferation to facilitate efficient skeletal muscle regeneration. Stem Cells (Dayton, Ohio), 29(12), 2030–2041.
Ettinger, A., & Wittmann, T. (2014). Fluorescence live cell imaging. Methods in Cell Biology, 123, 77–94.
Fink, J., Andersson-Rolf, A., & Koo, B. K. (2015). Adult stem cell lineage tracing and deep tissue imaging. BMB Reports, 48(12), 655–667.
Kupfer, M. E., & Ogle, B. M. (2015). Advanced imaging approaches for regenerative medicine: Emerging technologies for monitoring stem cell fate in vitro and in vivo. Biotechnology Journal, 10(10), 1515–1528.
Vande Velde, G., Couillard-Despres, S., Aigner, L., Himmelreich, U., & van der Linden, A. (2012). In situ labeling and imaging of endogenous neural stem cell proliferation and migration. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology, 4(6), 663–679.
Wang, J., & Jokerst, J. V. (2016). Stem cell imaging: tools to improve cell delivery and viability. Stem Cells International, 2016, 9240652.
Weissleder, R., & Nahrendorf, M. (2015). Advancing biomedical imaging. Proceedings of the National Academy of Sciences of the United States of America, 112(47), 14424–14428.
Vaz, R., Martins, G. G., Thorsteinsdottir, S., & Rodrigues, G. (2012). Fibronectin promotes migration, alignment and fusion in an in vitro myoblast cell model. Cell and Tissue Research, 348(3), 569–578.
Bentzinger, C. F., von Maltzahn, J., Dumont, N. A., Stark, D. A., Wang, Y. X., Nhan, K., et al. (2014). Wnt7a stimulates myogenic stem cell motility and engraftment resulting in improved muscle strength. The Journal of Cell Biology, 205(1), 97–111.
Brown, S., & Greco, V. (2014). Stem cells in the wild: understanding the World of stem cells through intravital imaging. Cell Stem Cell, 15(6), 683–686.
Pittet, M. J., & Weissleder, R. (2011). Intravital imaging. Cell, 147(5), 983–991.
Weigert, R. (2014). Advances in intravital microscopy: from basic to clinical research. Netherlands: Springer.
Mazo, I. B., Gutierrez-Ramos, J. C., Frenette, P. S., Hynes, R. O., Wagner, D. D., & von Andrian, U. H. (1998). Hematopoietic progenitor cell rolling in bone marrow microvessels: parallel contributions by endothelial selectins and vascular cell adhesion molecule 1. The Journal of Experimental Medicine, 188(3), 465–474.
Carlson, A. L., Fujisaki, J., Wu, J., Runnels, J. M., Turcotte, R., Spencer, J. A., et al. (2013). Tracking single cells in live animals using a photoconvertible near-infrared cell membrane label. PloS One, 8(8), e69257.
Khorshed, R. A., Hawkins, E. D., Duarte, D., Scott, M. K., Akinduro, O. A., Rashidi, N. M., et al. (2015). Automated Identification and Localization of Hematopoietic Stem Cells in 3D Intravital Microscopy Data. Stem Cell Reports, 5(1), 139–153.
Lo Celso, C., Fleming, H. E., Wu, J. W., Zhao, C. X., Miake-Lye, S., Fujisaki, J., et al. (2009). Live-animal tracking of individual haematopoietic stem/progenitor cells in their niche. Nature, 457(7225), 92–96.
Lo Celso, C., Lin, C. P., & Scadden, D. T. (2011). In vivo imaging of transplanted hematopoietic stem and progenitor cells in mouse calvarium bone marrow. Nature Protocols, 6(1), 1–14.
Scott, M. K., Akinduro, O., & Lo Celso, C. (2014). In vivo 4-dimensional tracking of hematopoietic stem and progenitor cells in adult mouse calvarial bone marrow. Journal of Visualized Experiments: JoVE, 91, e51683.
Itkin, T., Gur-Cohen, S., Spencer, J. A., Schajnovitz, A., Ramasamy, S. K., Kusumbe, A. P., et al. (2016). Distinct bone marrow blood vessels differentially regulate haematopoiesis. Nature, 532(7599), 323–328.
Ishido, M., & Kasuga, N. (2011). In situ real-time imaging of the satellite cells in rat intact and injured soleus muscles using quantum dots. Histochemistry and Cell Biology, 135(1), 21–26.
Kovalchuk, Y., Homma, R., Liang, Y., Maslyukov, A., Hermes, M., Thestrup, T., et al. (2015). In vivo odourant response properties of migrating adult-born neurons in the mouse olfactory bulb. Nature Communications, 6, 6349.
Mesa, K. R., Rompolas, P., Zito, G., Myung, P., Sun, T. Y., Brown, S., et al. (2015). Niche-induced cell death and epithelial phagocytosis regulate hair follicle stem cell pool. Nature, 522(7554), 94–97.
Pineda, C. M., Park, S., Mesa, K. R., Wolfel, M., Gonzalez, D. G., Haberman, A. M., et al. (2015). Intravital imaging of hair follicle regeneration in the mouse. Nature Protocols, 10(7), 1116–1130.
Rompolas, P., Deschene, E. R., Zito, G., Gonzalez, D. G., Saotome, I., Haberman, A. M., & Greco, V. (2012). Live imaging of stem cell and progeny behaviour in physiological hair-follicle regeneration. Nature, 487(7408), 496–499.
Rompolas, P., Mesa, K. R., & Greco, V. (2013). Spatial organization within a niche as a determinant of stem-cell fate. Nature, 502(7472), 513–518.
Nam, S. C., Kim, Y., Dryanovski, D., Walker, A., Goings, G., Woolfrey, K., et al. (2007). Dynamic features of postnatal subventricular zone cell motility: a two-photon time-lapse study. The Journal of Comparative Neurology, 505(2), 190–208.
James, R., Kim, Y., Hockberger, P. E., & Szele, F. G. (2011). Subventricular zone cell migration: lessons from quantitative two-photon microscopy. Frontiers in Neuroscience, 5, 30.
Ortega, F., & Costa, M. R. (2016). Live imaging of adult neural stem cells in rodents. Frontiers in Neuroscience, 10, 78.
Sonego, M., Zhou, Y., Oudin, M.J., Doherty, P., Lalli, G. (2013). In vivo postnatal electroporation and time-lapse imaging of neuroblast migration in mouse acute brain slices. Journal of visualized experiments: JoVE. doi:10.3791/50905.
Cao, L., Pu, J., Scott, R. H., Ching, J., & McCaig, C. D. (2015). Physiological electrical signals promote chain migration of neuroblasts by up-regulating P2Y1 purinergic receptors and enhancing cell adhesion. Stem Cell Reviews, 11(1), 75–86.
Acknowledgments
This work was supported by the Grant-in-Aid from the American Heart Association. The author thanks Dr. Tsvee Lapidot from the Weizmann Institute of Science, Rehovot, Israel and Dr. Marcello Rota from the New York Medical College, Valhalla, NY for their critical reading of the manuscript and insightful comments. The author apologizes to authors whose work was not cited due to space limitations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The author indicates no potential conflicts of interest.
Rights and permissions
About this article
Cite this article
Goichberg, P. Current Understanding of the Pathways Involved in Adult Stem and Progenitor Cell Migration for Tissue Homeostasis and Repair. Stem Cell Rev and Rep 12, 421–437 (2016). https://doi.org/10.1007/s12015-016-9663-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-016-9663-7