Abstract
Data on the effects of selenium supplementation on clinical signs and metabolic profiles in women at risk for intrauterine growth restriction (IUGR) are scarce. This study was designed to assess the effects of selenium supplementation on clinical signs and metabolic status in pregnant women at risk for IUGR. This randomized double-blind placebo-controlled clinical trial was performed among 60 women at risk for IUGR according to abnormal uterine artery Doppler waveform. Participants were randomly assigned to intake either 100 μg selenium supplements as tablet (n = 30) or placebo (n = 30) for 10 weeks between 17 and 27 weeks of gestation. After 10 weeks of selenium administration, a higher percentage of women in the selenium group had pulsatility index (PI) of <1.45) (P = 0.002) than of those in the placebo group. In addition, changes in plasma levels of total antioxidant capacity (TAC) (P < 0.001), glutathione (GSH) (P = 0.008), and high-sensitivity C-reactive protein (hs-CRP) (P = 0.004) in the selenium group were significant compared with the placebo group. Additionally, selenium supplementation significantly decreased serum insulin (P = 0.02), homeostasis model of assessment-estimated insulin resistance (HOMA-IR) (P = 0.02), and homeostatic model assessment for B-cell function (HOMA-B) (P = 0.02) and significantly increased quantitative insulin sensitivity check index (QUICKI) (P = 0.04) and HDL-C levels (P = 0.02) compared with the placebo. We did not find any significant effect of selenium administration on malondialdehyde (MDA), nitric oxide (NO), fasting plasma glucose (FPG), and other lipid profiles. Overall, selenium supplementation in pregnant women at risk for IUGR resulted in improved PI, TAC, GSH, hs-CRP, and markers of insulin metabolism and HDL-C levels, but it did not affect MDA, NO, FPG, and other lipid profiles.
Clinical trial registration number http://www.irct.ir: IRCT201601045623N64.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intrauterine growth restriction (IUGR), a main cause of perinatal morbidity and mortality [1], is considered as the consequence of a disease process within one or more of the three compartments that control the fetal growth: maternal, placenta, and fetus [2]. This status affects 10–15% of pregnant women [3]. Recent evidence suggests that increased oxidative stress and inflammatory markers are involved in the pathophysiology of IUGR [4]. IUGR is associated with an increased risk of developing obesity, insulin resistance, reduced lean body mass, and cardiovascular disease (CVD) in adulthood [5]. Therefore, selenium supplementation due to protecting trophoblast cells from mitochondrial oxidative stress may be important in treating some placental pathology [6].
Previous studies have reported controversial results between selenium levels and recurrent abortions, preeclampsia, and IUGR [7–9]. In addition, few studies have shown that selenium supplementation had beneficial effects on the metabolic profiles in patients with gestational diabetes mellitus (GDM) [10] and on markers of risk of preeclampsia in pregnant women [11]. Current data supports the favorable effects of selenium on coronary artery disease (CVD) [12], diabetic nephropathy [13], and polycystic ovary syndrome [14, 15]. In a study conducted by Alizadeh et al. [16], it was observed that supplementation with 200 μg/day selenium for 6 weeks led to a significant decrease in serum insulin levels and insulin resistance among women with central obesity. Furthermore, high-dose selenium supplementation for 14 days resulted in a significant decrease in C-reactive protein (CRP) levels in subjects with systemic inflammatory response syndrome [17]. However, in another study by Savory et al. [18], it was seen that 200 μg selenium administration daily for 3 weeks did not influence biomarkers of oxidative stress including total antioxidant status (TAS) and glutathione (GSH) levels among overweight adults.
Selenium intake might benefit in women at risk for IUGR through its effects on decreased free radical production and lipid hydroperoxides [19], inflammation and oxidative stress, and inhibiting the production of advanced glycation end products [20]. As there is evidence that selenium supplementation may have antioxidant and anti-inflammatory effects [21, 22], we hypothesized that selenium supplementation might help women at risk for IUGR to have a better clinical response and biomarkers of oxidative stress and inflammation and metabolic profiles. The objective of this study, therefore, was to evaluate the effects of selenium intake on clinical signs and metabolic status in women at risk for IUGR.
Subjects and Methods
Trial Design
This research was a prospective randomized double-blind placebo-controlled clinical trial.
Participants
This study was conducted among 60 pregnant women primigravida, aged 18–40 years old, at risk for IUGR according to abnormal uterine artery Doppler waveform with a mean pulsatility index (PI) of >1.45 [23], who were referred to the Naghavi Clinic in Kashan, Iran, from January 2016 to May 2016. Participants who consumed selenium supplements during the past 3 months; with hypothyroidism and hyperthyroidism, urinary tract infection, preeclampsia, hypertension, diseases related to increased inflammation, and kidney or liver diseases; and who were smokers were not included in the current study.
Ethics Statements
This trial was done according to the guidelines laid down in the Declaration of Helsinki. This study was approved by the ethics committee of Kashan University of Medical Sciences (KUMS) and registered on the Iranian registry of clinical trials website (http://www.irct.ir: IRCT201601045623N64). All subjects provided informed written consent before recruitment.
Study Design
At first, all women were matched based on pretreatment of BMI (<25 and ≥25 kg/m2) and age (<30 and ≥30 years). Subjects were then randomly divided into two groups to take either selenium supplements (n = 30) or placebo (n = 30) for 10 weeks. Subjects were requested not to change their ordinary physical activity and not to take any nutritional supplements during the 10-week intervention. All subjects completed 3-day food records and three physical activity records at the initial of the study, during weeks 3 and 6, and at the end of the treatment. Daily macronutrient and micronutrient intakes were analyzed by nutritionist IV software (First Databank, San Bruno, CA). In this clinical trial, physical activity was described as metabolic equivalents (METs) in hours per day. To determine the METs for each patient, we multiplied the times (in hour per day) reported for each physical activity by its related METs coefficient by standard tables [24]. The used tool to measure physical activity was questionnaire. Subjects of the current study were randomly assigned to use either 100 μg selenium supplements as selenium yeast or placebo (starch) daily for 10 weeks from 17 to 27 weeks of gestation. Selenium supplements and placebos tablets were similar in shape and size and manufactured by Nature Made (CA, USA) and Barij Essence (Kashan, Iran), respectively. Quality control of selenium supplements was conducted in the laboratory of Food and Drug Administration in Tehran, Iran, by atomic absorption spectroscopy (AAS) method. Following quality control, we found that the amount of selenium in the prescribed tablets was at the range of 95–110 μg.
Treatment Adherence
Every 5 weeks, subjects were given enough supplements to last until 3 days after their next scheduled visit and were instructed to return all the unused supplements at each visit. During the 10-week period of the study, subjects were followed by phone or via short message service (SMS) twice a week to remind them of the instructions.
Assessment of Anthropometric Measures
Weight and height of pregnant women were determined in an overnight fasting status using a standard scale (Seca, Hamburg, Germany) at the initial of the study and after the 10-week intervention. BMI was calculated as weight in kilograms divided by height in meters squared.
Assessment of Outcomes
In this research, PI and biomarkers of oxidative stress were considered as the primary outcome measurements and biomarkers of inflammation, markers of insulin metabolism, and lipid profiles were considered as the secondary outcome measurements.
Clinical Assessment
Measurement of the PI was performed in the subjects by the same sonographist, at study baseline and after the 10-week intervention using a Doppler ultrasonography device (Samsung Medison V20, Seoul, Korea). The physician was blinded to any clinical information of the subjects. The uterine artery blood velocity waveforms were recorded from both uterine arteries at the apparent crossover of the uterine and external iliac arteries with an insonation angle of <30°, velocity of >60 cm/s, and a sample volume of 2.0 mm [23].
Biochemical Assessment
At first and after the end of the treatment, 10-mL of blood samples was taken from each subject at the Kashan reference laboratory in an early morning after an overnight fast. Blood was collected in two separate tubes: (1) one without EDTA to separate the serum, in order to determine serum insulin, lipid profiles, and high sensitivity C-reactive protein (hs-CRP) concentrations and (2) another one containing EDTA to examine plasma nitric oxide (NO) and biomarkers of oxidative stress. Fasting plasma glucose (FPG) and lipid profiles were measured on the day of blood collection. Blood samples were immediately centrifuged (Hettich D-78532, Tuttlingen, Germany) at 3500 rpm for 10 min to separate serum. Then, the samples were stored at −80 °C before analysis at the KUMS reference laboratory. Plasma total antioxidant capacity (TAC) obtained using ferric-reducing antioxidant power developed by Benzie and Strain [25], GSH using the method of Beutler et al. [26], and malondialdehyde (MDA) concentrations using the thiobarbituric acid reactive substance spectrophotometric test [27] using a Cecil 2021 spectrophotometer (Milton, United Kingdom) with a temperature-controlled cuvette holder (Cecil) were evaluated. Coefficient variances (CVs) for plasma TAC, GSH, and MDA were 1.5, 2.6, and 3.5%, respectively. Serum hs-CRP concentrations were quantified by commercial ELISA kit (LDN, Nordhorn, Germany) with intra-assay and interassay CVs of 3.6 and 5.5%, respectively. Plasma NO concentrations were assessed using Griess method [28] using a Cecil 2021 spectrophotometer (Milton, UK). CVs for NO concentrations were 2.5%. Serum insulin levels were evaluated using available ELISA kit (DiaMetra, Milano, Italy) with intra-assay and interassay CVs of 3.0 and 4.8%, respectively. The homeostasis model of assessment-insulin resistance (HOMA-IR), the β-cell function (HOMA-B), and the quantitative insulin sensitivity check index (QUICKI) were determined according to the suggested formulas [29]. Enzymatic kits (Pars Azmun, Tehran, Iran) were used to quantify FPG; serum triglycerides; and VLDL-, total-, LDL- and HDL-C fractions with interassay and intra-assay CVs less than 5%.
Sample Size
To determine the sample size, we used a parallel randomized clinical trial sample size formula where type one (α) and type two errors (β) were 0.05 and 0.20 (power = 80%), respectively. Based on a prior study [10], we considered 118.4 mmol/L as standard deviation (SD) and 95.0 mmol/L as the difference in mean (d) of plasma TAC as a main variable. Therefore, we needed 25 subjects in each group. Considering 5 dropouts in each group; the final sample size was determined to be 30 persons each group.
Randomization and Blinding
In this trial, randomization and allocation were used with the baseline data of the patients as blindness by a trained member who did not had a role in the treatment of the participants. Random assignment was performed using computer-generated random numbers.
Statistical Analysis
We used the Kolmogrov-Smirnov test to evaluate the normal distribution of variables. Independent samples student’s t test was used to determine differences in general characteristics and dietary intakes between the two groups. To compare categorical variables, we used Pearson chi-square test. To determine the effects of selenium supplementation on metabolic status, we used one-way repeated measures analysis of variance. To evaluate confounding variables including baseline values of biochemical markers, maternal age, and baseline BMI, we used analysis of covariance (ANCOVA). P < 0.05 was considered as statistically significant. All statistical analyses were done using the Statistical Package for Social Science version 17 (SPSS Inc., Chicago, Illinois, USA).
Results
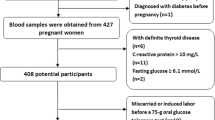
At the eligibility phase, 690 pregnant women were invited. Six hundred thirty subjects of the 690 invited subjects were excluded (due to not meeting the inclusion criteria) from the first visit. In the current study, 60 subjects [selenium (n = 30) and placebo (n = 30)] completed the trial. On average, the rate of compliance in this trial was high, such that 100% of capsules were taken throughout the study in both groups. No side effects were reported following supplementation with selenium in women at risk for IUGR.
Mean age, height, weight, and BMI of the study participants at the study baseline and end-of-trial, educational levels and job status were not significantly different between the two groups (Table 1). After 10 weeks of selenium administration, higher percentage of women in the selenium group had pulsatility index (PI) of <1.45 (P = 0.002) than in the placebo group.
Based on the 3-day dietary records obtained throughout the treatment, no statistically significant difference was seen between the two groups in terms of dietary intakes of macronutrients and micronutrients; magnesium; selenium; and vitamins C, E and A (Data not shown).
Changes in plasma levels of TAC (P < 0.001), GSH (P = 0.008), and serum insulin (P = 0.02) in the selenium group were significant compared with the placebo group (Fig. 1).
Selenium supplementation significantly decreased serum hs-CRP (P = 0.004), HOMA-IR (P = 0.02), and HOMA-B (P = 0.02) and significantly increased QUICKI (P = 0.04) and HDL-C levels (P = 0.02) compared with the placebo (Table 2). We did not find any significant effect of selenium administration on MDA, NO, FPG, and other lipid profiles.
Baseline levels of plasma TAC, GSH, and NO were significant between the two groups. Thus, we controlled the analyses for the baseline levels of biochemical variables, age, and baseline BMI. When we adjusted the analysis for baseline values of biochemical parameters, age, and baseline BMI, plasma GSH (P = 0.08), HOMA-B (P = 0.05), and QUICKI (P = 0.06) became non-significant, and other findings were not altered (Table 3).
Discussion
We found that selenium supplementation in pregnant women at risk for IUGR had beneficial effects on PI, TAC, GSH, hs-CRP, markers of insulin metabolism, and HDL-C levels, but it did not affect MDA, NO, FPG, and other lipid profiles. To our knowledge, this study is the first examining the effects of selenium supplementation on clinical signs and metabolic status among pregnant women at risk for IUGR. It must be kept in mind that the high standard deviations (SDs) of dependent variables in some cases might make the interpretation of our findings difficult. Such high SDs might be explained by the small number of subjects in the study, which was a limitation in our study. In our study, no side effects were seen after selenium intake in pregnant women at risk for IUGR throughout the study. It must be considered that mean dietary plus supplemental selenium intake in our study subjects was lower than upper limits (400 μg). However, data on the toxic effects of selenium on human health are conflicting. For example, Burk et al. [30] demonstrated that intake of moderate- (200 μg/day) to large-dose (600 μg/day) selenium for 16 weeks was safe among volunteers aged ≥18 years. In another study, hair loss, gastrointestinal symptoms, and memory difficulties were reported as the adverse effects of selenium intake [31]. Nonetheless, further studies are needed about potential toxicity/teratogenicity of long-term increased selenium intake in pregnant women at risk for IUGR. In the current study, we used 100 μg of selenium supplements per day for 10 weeks in pregnant women at risk for IUGR, which was lower than the used dosage by others [16]. Although the beneficial effects of selenium (≤100 μg/day) during pregnancy were reported [11, 32], we believe that further studies are needed to confirm our findings.
Pregnant women at risk for IUGR are susceptible to increased risk of developing obesity, insulin resistance, and CVD in adulthood [5]. We found that selenium administration after 10 weeks in women at risk for IUGR had beneficial effects on PI compared with the placebo. Some studies have indicated that selenium deficiency influences both pregnancy and fetal development [33, 34]. In addition, in a study by Zadrozna et al. [9], significant inverse correlation was established between selenium level and cytochrome c oxidase (CCO) activity and between selenium level and placental weight. Previous studies have also demonstrated that selenium supplementation can protect trophoblast cells from both endogenously and exogenously applied oxidative stress [35, 36]. In another study, Bogden et al. [37] demonstrated that low-normal serum selenium in the first or second trimester of pregnancy was associated with low birth weight. Increased cellular expression and activity of the seleno-dependent antioxidant enzyme glutathione peroxidase (GPx) and decreased production of ROS by selenium [6] may result in beneficial effects in pregnant women at risk for IUGR.
The current study demonstrated that selenium intake for 10 weeks in women at risk for IUGR resulted in a significant rise in plasma TAC and GSH, and a significant reduction in serum hs-CRP levels compared with the placebo, but unchanged plasma MDA and NO levels. It must be kept in mind that MDA analyses should have performed in erythrocytes instead of plasma, because oxidation occurs in lipids, proteins, and nucleic acids. However, due to some limitations, we could not perform these analyses. Therefore, our findings should be interpreted with caution. In addition, in the current study, some mean values such as TAC and GSH were too high according to reference values, which is in accordance with other studies [38, 39]. This may be due to the characteristics of study patients. We have previously shown that selenium supplementation at a dosage of 200 μg per day among women with GDM led to improved biomarkers of oxidative stress and inflammation [10]. Likewise, TAS and GSH levels had significant increase following supplementation with selenium after 45 days in subjects with epilepsy and refractory epilepsy [40]. However, in a study conducted by Savory et al. [18], selenium supplementation at a dosage of 200 μg daily for 3 weeks among overweight adults did not alter TAS and GSH concentrations. In addition, in our study among patients with CIN, no significant effect was observed on serum hs-CRP and plasma NO concentrations following supplementation with selenium for 6 months [41].
Elevated levels of MDA and significant depletion in antioxidant capacity were demonstrated in many previous studies, including preeclamptic and diabetic pregnancies [42, 43]. Wiktor et al. [44] observed increased MDA concentrations in placentas of subjects with pregnancies complicated by severe preeclampsia and IUGR. Bowen et al. [45] proposed that increased levels of MDA in cord plasma might indicate the dispersion of MDA from the placenta to the umbilical cord. These authors suggested that the placenta indeed might be more effective in removing MDA; thus, MDA levels might be a better marker of oxidative stress [45]. In addition, in another study, GSH levels and expression of GPx in the placenta were lower in subjects with preeclampsia as compared with control [46]. Therefore, selenium supplements due to their useful effects on GSH may be useful to decrease oxidative stress in pregnant women at risk for IUGR. Selenium intake may decrease oxidative stress and inflammation through increasing selenoprotein biosynthesis [47], inhibiting production of reactive oxygen species/reactive nitrogen species [48], and the inhibition of nuclear factor kappa light-chain-enhancer of activated B cells (NF-kappa B) by modulating selenoprotein gene expressions [49].
Our study indicated that taking selenium supplements for 10 weeks in women at risk for IUGR resulted in significant decreases in serum insulin levels, HOMA-IR and HOMA-B, and significant rises in QUICKI and HDL-C levels compared with the placebo but did not affect FPG and other lipid fractions. Some studies have evaluated the effects of selenium administration on parameters of glucose homeostasis and lipid profiles. In accordance with our findings, in a study done by Alizadeh et al. [16], it was seen that the intake of 200 μg/day selenium supplements for 6 weeks significantly decreased serum insulin levels and HOMA-IR among subjects with central obesity. Furthermore, we have previously demonstrated that selenium supplementation among women with GDM for 6 weeks improved glycemic control and HDL-C levels; however, it did not influence other lipid fractions [10]. In contrast to our study, some researchers did not see any favorable effect of selenium supplementation on glucose homeostasis. For instance, a 12-week administration with selenium supplements in diabetic subjects did not influence serum insulin concentrations as well as led to increased FPG levels [50]. In addition, Boskabadi et al. [51] observed that the consumption of 100 μg selenium supplements in pregnant women did not affect cord-blood total-, LDL-, and HDL-C levels and increased serum triglycerides concentrations. Impaired insulin metabolism during pregnancy can predict the progression to type 2 diabetes mellitus (T2DM) later in life and neonatal complications [52]. In addition, impaired insulin function in pregnant women can result in adverse long-term maternal outcomes and increased perinatal morbidity such as macrosomia and preeclampsia [53]. In addition, increased lipid fractions during pregnancy would result in increased risk of cardiovascular disease in later life of the mother [54] and in its offspring’s [55]. Therefore, selenium intake due to their useful effects on glycemic status may be useful to control metabolic symptoms. The baseline characteristics of the study persons as well as the dosage of selenium supplements along with the study duration might result in some explanations for the different findings of the current study with other studies. Selenium supplementation may improve glycemic control and HDL-C levels via the regulating expression of genes responsible for synthesis of the enzymes involved in the insulin metabolism, increased uptake of the glucose by tissues and improved insulin sensitivity [56], and the inhibition of inflammatory variables [57].
Overall, selenium supplementation in pregnant women at risk for IUGR resulted in improved PI, TAC, GSH, hs-CRP, markers of insulin metabolism, and HDL-C levels but did not affect MDA, NO, FPG, and other lipid profiles.
Change history
28 February 2020
The Editors-in-Chief are currently investigating this article [Mesdaghinia, E., Rahavi, A., Bahmani, F. et al. Clinical and Metabolic Response to Selenium Supplementation in Pregnant Women at Risk for Intrauterine Growth Restriction: Randomized, Double-Blind, Placebo-Controlled Trial. Biol Trace Elem Res 178, 14–21 (2017). https://doi.org/10.1007/s12011-016-0911-0] as concerns have been raised about integrity of the clinical trial reported here. There is also an ongoing investigation by the Iranian National Committee for Ethics in Biomedical Researches. Further editorial action will be taken as appropriate once the investigation into the concerns is complete and all parties have been given an opportunity to respond in full.
References
Jarvis S, Glinianaia SV, Torrioli MG et al (2003) Cerebral palsy and intrauterine growth in single births: European collaborative study. Lancet 362:1106–1111
Cetin I, Foidart JM, Miozzo M et al (2004) Fetal growth restriction: a workshop report. Placenta 25:753–757
Dikbas L, Yapca OE, Dikbas N, Gundogdu C (2016) Paraoxonase-2 and paraoxonase-3: comparison of mRNA expressions in the placentae of unexplained intrauterine growth restricted and noncomplicated pregnancies. J Matern Fetal Neonatal Med 1–7. doi:10.1080/14767058.2016.1209480
Takagi Y, Nikaido T, Toki T et al (2004) Levels of oxidative stress and redox-related molecules in the placenta in preeclampsia and fetal growth restriction. Virchows Arch 444:49–55
Beauchamp B, Thrush AB, Quizi J et al (2015) Undernutrition during pregnancy in mice leads to dysfunctional cardiac muscle respiration in adult offspring. Biosci Rep 35. doi:10.1042/BSR20150007
Khera A, Vanderlelie JJ, Holland O, Perkins AV (2016) Overexpression of endogenous anti-oxidants with selenium supplementation protects trophoblast cells from reactive oxygen species-induced apoptosis in a Bcl-2-dependent manner. Biol Trace Elem Res. doi:10.1007/s12011-016-0870-5
Mistry HD, Broughton Pipkin F, Redman CW, Poston L (2012) Selenium in reproductive health. Am J Obstet Gynecol 206:21–30
Rayman MP, Bode P, Redman CW (2003) Low selenium status is associated with the occurrence of the pregnancy disease preeclampsia in women from the United Kingdom. Am J Obstet Gynecol 189:1343–1349
Zadrozna M, Gawlik M, Nowak B et al (2009) Antioxidants activities and concentration of selenium, zinc and copper in preterm and IUGR human placentas. J Trace Elem Med Biol 23:144–148
Asemi Z, Jamilian M, Mesdaghinia E, Esmaillzadeh A (2015) Effects of selenium supplementation on glucose homeostasis, inflammation, and oxidative stress in gestational diabetes: randomized, double-blind, placebo-controlled trial. Nutrition 31:1235–1242
Rayman MP, Searle E, Kelly L et al (2014) Effect of selenium on markers of risk of pre-eclampsia in UK pregnant women: a randomised, controlled pilot trial. Br J Nutr 112:99–111
Schnabel R, Lubos E, Messow CM et al (2008) Selenium supplementation improves antioxidant capacity in vitro and in vivo in patients with coronary artery disease the selenium therapy in coronary artery disease patients (SETCAP) study. Am Heart J 156(1201):e1201–e1211
Bahmani F, Kia M, Soleimani A, Mohammadi AA, Asemi Z (2016) The effects of selenium supplementation on biomarkers of inflammation and oxidative stress in patients with diabetic nephropathy: a randomised, double-blind, placebo-controlled trial. Br J Nutr 116:1222–1228
Jamilian M, Razavi M, Fakhrie Kashan Z, Ghandi Y, Bagherian T, Asemi Z (2015) Metabolic response to selenium supplementation in women with polycystic ovary syndrome: a randomized, double-blind, placebo-controlled trial. Clin Endocrinol 82:885–891
Kose SA, Naziroglu M (2014) Selenium reduces oxidative stress and calcium entry through TRPV1 channels in the neutrophils of patients with polycystic ovary syndrome. Biol Trace Elem Res 158:136–142
Alizadeh M, Safaeiyan A, Ostadrahimi A et al (2012) Effect of L-arginine and selenium added to a hypocaloric diet enriched with legumes on cardiovascular disease risk factors in women with central obesity: a randomized, double-blind, placebo-controlled trial. Ann Nutr Metab 60:157–168
Valenta J, Brodska H, Drabek T, Hendl J, Kazda A (2011) High-dose selenium substitution in sepsis: a prospective randomized clinical trial. Intensive Care Med 37:808–815
Savory LA, Kerr CJ, Whiting P, Finer N, McEneny J, Ashton T (2012) Selenium supplementation and exercise: effect on oxidant stress in overweight adults. Obesity (Silver Spring) 20:794–801
Alissa EM, Bahijri SM, Ferns GA (2003) The controversy surrounding selenium and cardiovascular disease: a review of the evidence. Med Sci Monit 9:RA9–R18
Li YB, Han JY, Jiang W, Wang J (2011) Selenium inhibits high glucose-induced cyclooxygenase-2 and P-selectin expression in vascular endothelial cells. Mol Biol Rep 38:2301–2306
Ozkaya MO, Naziroglu M (2010) Multivitamin and mineral supplementation modulates oxidative stress and antioxidant vitamin levels in serum and follicular fluid of women undergoing in vitro fertilization. Fertil Steril 94:2465–2466
Ozkaya MO, Naziroglu M, Barak C, Berkkanoglu M (2011) Effects of multivitamin/mineral supplementation on trace element levels in serum and follicular fluid of women undergoing in vitro fertilization (IVF). Biol Trace Elem Res 139:1–9
Barati M, Shahbazian N, Ahmadi L, Masihi S (2014) Diagnostic evaluation of uterine artery Doppler sonography for the prediction of adverse pregnancy outcomes. J Res Med Sci 19:515–519
Ainsworth BE, Haskell WL, Whitt MC et al (2000) Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32:S498–S504
Benzie IF, Strain JJ (1996) The ferric reducing ability of plasma (FRAP) as a measure of “antioxidant power”: the FRAP assay. Anal Biochem 239:70–76
Beutler E, Gelbart T (1985) Plasma glutathione in health and in patients with malignant disease. J Lab Clin Med 105:581–584
Janero DR (1990) Malondialdehyde and thiobarbituric acid-reactivity as diagnostic indices of lipid peroxidation and peroxidative tissue injury. Free Radic Biol Med 9:515–540
Tatsch E, Bochi GV, Pereira Rda S et al (2011) A simple and inexpensive automated technique for measurement of serum nitrite/nitrate. Clin Biochem 44:348–350
Pisprasert V, Ingram KH, Lopez-Davila MF, Munoz AJ, Garvey WT (2013) Limitations in the use of indices using glucose and insulin levels to predict insulin sensitivity: impact of race and gender and superiority of the indices derived from oral glucose tolerance test in African Americans. Diabetes Care 36:845–853
Burk RF, Norsworthy BK, Hill KE, Motley AK, Byrne DW (2006) Effects of chemical form of selenium on plasma biomarkers in a high-dose human supplementation trial. Cancer Epidemiol Biomark Prev 15:804–810
Aldosary BM, Sutter ME, Schwartz M, Morgan BW (2012) Case series of selenium toxicity from a nutritional supplement. Clin Toxicol (Phila) 50:57–64
Tara F, Maamouri G, Rayman MP et al (2010) Selenium supplementation and the incidence of preeclampsia in pregnant Iranian women: a randomized, double-blind, placebo-controlled pilot trial. Taiwan J Obstet Gynecol 49:181–187
Osada H, Watanabe Y, Nishimura Y, Yukawa M, Seki K, Sekiya S (2002) Profile of trace element concentrations in the feto-placental unit in relation to fetal growth. Acta Obstet Gynecol Scand 81:931–937
Kantola M, Purkunen R, Kroger P et al (2004) Selenium in pregnancy: is selenium an active defective ion against environmental chemical stress? Environ Res 96:51–61
Watson M, van Leer L, Vanderlelie JJ, Perkins AV (2012) Selenium supplementation protects trophoblast cells from oxidative stress. Placenta 33:1012–1019
Khera A, Dong LF, Holland O et al (2015) Selenium supplementation induces mitochondrial biogenesis in trophoblasts. Placenta 36:863–869
Bogden JD, Kemp FW, Chen X, Stagnaro-Green A, Stein TP, Scholl TO (2006) Low-normal serum selenium early in human pregnancy predicts lower birth weight. Nutr Res 26:497–502
Constans J, Bennetau-Pelissero C, Martin JF et al (2015) Marked antioxidant effect of orange juice intake and its phytomicronutrients in a preliminary randomized cross-over trial on mild hypercholesterolemic men. Clin Nutr 34:1093–1100
Arnal N, Astiz M, de Alaniz MJ, Marra CA (2011) Clinical parameters and biomarkers of oxidative stress in agricultural workers who applied copper-based pesticides. Ecotox environ safe 74:1779–1786
Yurekli VA, Naziroglu M (2013) Selenium and topiramate attenuates blood oxidative toxicity in patients with epilepsy: a clinical pilot study. Biol Trace Elem Res 152:180–186
Karamali M, Nourgostar S, Zamani A, Vahedpoor Z, Asemi Z (2015) The favourable effects of long-term selenium supplementation on regression of cervical tissues and metabolic profiles of patients with cervical intraepithelial neoplasia: a randomised, double-blind, placebo-controlled trial. Br J Nutr 114:2039–2045
Wu JJ (1996) Lipid peroxidation in preeclamptic and eclamptic pregnancies. Eur J Obstet Gynecol Reprod Biol 64:51–54
Suhail M, Patil S, Khan S, Siddiqui S (2010) Antioxidant vitamins and lipoperoxidation in non-pregnant, pregnant, and gestational diabetic women: erythrocytes osmotic fragility profiles. J Clin Med Res 2:266–273
Wiktor H, Kankofer M (2001) Assessment of lipid peroxidation intensification in normal and preeclamptic placentas. Ginekol Pol 72:1217–1221
Bowen RS, Moodley J, Dutton MF, Theron AJ (2001) Oxidative stress in pre-eclampsia. Acta Obstet Gynecol Scand 80:719–725
D’Souza V, Rani A, Patil V et al (2016) Increased oxidative stress from early pregnancy in women who develop preeclampsia. Clin Exp Hypertens 38:225–232
Ozturk IC, Batcioglu K, Karatas F, Hazneci E, Genc M (2008) Comparison of plasma malondialdehyde, glutathione, glutathione peroxidase, hydroxyproline and selenium levels in patients with vitiligo and healthy controls. Indian J Dermatol 53:106–110
Zeng J, Zhou J, Huang K (2009) Effect of selenium on pancreatic proinflammatory cytokines in streptozotocin-induced diabetic mice. J Nutr Biochem 20:530–536
He YT, Liu DW, Ding LY, Li Q, Xiao YH (2004) Therapeutic effects and molecular mechanisms of anti-fibrosis herbs and selenium on rats with hepatic fibrosis. World J Gastroenterol 10:703–706
Faghihi T, Radfar M, Barmal M et al (2014) A randomized, placebo-controlled trial of selenium supplementation in patients with type 2 diabetes: effects on glucose homeostasis, oxidative stress, and lipid profile. Am J Ther 21:491–495
Boskabadi H, Maamouri G, Rezagholizade Omran F et al (2012) Effect of prenatal selenium supplementation on cord blood selenium and lipid profile. Pediatr Neonatol 53:334–339
Greenberg J (2011) The relationship between maternal glycemia and perinatal outcome. Obstet Gynecol 117:1230 author reply 1230-1231
Metzger BE, Lowe LP, Dyer AR et al (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358:1991–2002
Winkler K, Wetzka B, Hoffmann MM et al (2000) Low density lipoprotein (LDL) subfractions during pregnancy: accumulation of buoyant LDL with advancing gestation. J Clin Endocrinol Metab 85:4543–4550
Kusters DM, Homsma SJ, Hutten BA et al (2010) Dilemmas in treatment of women with familial hypercholesterolaemia during pregnancy. Neth J Med 68:299–303
Chen H, Qiu Q, Zou C, Dou L, Liang J (2015) Regulation of hepatic carbohydrate metabolism by selenium during diabetes. Chem Biol Interact 232:1–6
Brigelius-Flohe R, Banning A, Kny M, Bol GF (2004) Redox events in interleukin-1 signaling. Arch Biochem Biophys 423:66–73
Acknowledgments
The current study was founded by a grant from the Vice-chancellor for Research, KUMS, Iran. The authors would like to thank the staff of Naghavi Clinic (Kashan, Iran) for their assistance on this project.
Authors’ Contributions
ZA contributed in the conception, design, statistical analysis, and drafting of the manuscript. EM, AR, and FB contributed in data collection and manuscript drafting. All authors approved the final version for submission. ZA supervised the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Statements
This trial was done according to the guidelines laid down in the Declaration of Helsinki. This study was approved by the ethics committee of Kashan University of Medical Sciences (KUMS) and registered on the Iranian registry of clinical trials website (http://www.irct.ir: IRCT201601045623N64). All subjects provided informed written consent before recruitment.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Mesdaghinia, E., Rahavi, A., Bahmani, F. et al. Clinical and Metabolic Response to Selenium Supplementation in Pregnant Women at Risk for Intrauterine Growth Restriction: Randomized, Double-Blind, Placebo-Controlled Trial. Biol Trace Elem Res 178, 14–21 (2017). https://doi.org/10.1007/s12011-016-0911-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-016-0911-0