Abstract
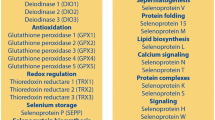
Selenium appears to have a beneficial effect on number of adverse pregnancy health conditions. Higher selenium status has been associated with a lower risk of miscarriage and preterm birth, while there is evidence from randomized controlled trials that selenium supplementation may reduce the risk of pre-eclampsia and post-partum thyroid disease. The ability of selenoproteins to reduce oxidative stress, endoplasmic-reticulum stress and inflammation, and to protect the endothelium, control eicosanoid production, regulate vascular tone and reduce infection, is likely to be important in these apparently protective effects.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
This chapter summarizes what is known about the role of selenium (Se) in adverse health conditions of human pregnancy. However, even in normal pregnancy, oxidative stress rises and there is a systemic inflammatory response, largely triggered by placental events [1, 2]. There is evidence from animal models that Se requirement increases during pregnancy, possibly because of these maternal factors, but also because of the needs of the growing fetus [3]. During normal pregnancy, whole-blood Se concentration falls substantially (e.g., by 12 %) with increasing gestational age [4–6]. Apart from plasma volume expansion, an additional cause of a fall in blood Se concentration throughout pregnancy is likely to be the transfer of Se to the fetus by selenoprotein P (SEPP1) which is expressed in the placenta [7]. In pregnant mice, placental transfer of maternal SEPP1 occurred through the apoE receptor 2 [8]. Even in mice with normal Se status, maternal plasma SEPP1 concentration falls rather dramatically in late pregnancy; hence, pregnancy may be putting similar pressure on the Se stores of pregnant women with marginal Se status. The pregnancy conditions for which most evidence for involvement of Se exists are addressed below.
2 Pre-eclampsia
Pre-eclampsia , a major complication in 2–8 % of pregnancies [9], is associated with high maternal and perinatal morbidity and mortality ; there is currently no cure other than early delivery of the baby [10]. Surviving infants are likely to be small for gestational age and premature, factors that may jeopardize their development and health even into adulthood [9]. Furthermore, pre-eclampsia is linked to an increased risk of maternal coronary heart disease, hypertension and stroke in later life [11].
Deficient placentation in the first half of pregnancy frequently presages the development of pre-eclampsia [1]. Shallow invasion of the trophoblast (embryonic cells that develop into the placenta) and inadequate remodeling of the spiral arteries result in a placenta that is not adequately perfused [1, 12]. Thus, localized areas of ischemia and reperfusion associated with placental oxidative and endoplasmic-reticulum (ER) stress develop [12–15]. This results in increased apoptosis/necrosis of the syncytiotrophoblast layer (outer cells of the placental villi), accompanied by release of anti-angiogenic factors, including soluble vascular-endothelial-growth-factor-receptor-1 (referred to as sFlt-1), that cause endothelial dysfunction, hypertension and proteinuria [1, 16]. Placental microvesicles released into the maternal circulation stimulate a systemic inflammatory response and endothelial activation that characterize pre-eclampsia [1, 17, 18].
2.1 Observational Studies of Se and Pre-eclampsia
A positive correlation between Se status and the incidence of pre-eclampsia has been shown in an epidemiological study of 45 countries [19]. A recent meta-analysis of 13 observational studies found significantly lower blood/plasma/serum Se concentrations in women with pre-eclampsia than in control pregnant women [mean difference −8.25 μg/L, 95 % confidence interval (CI) −12.89, −3.61; P = 0.0005] ([20] and personal communication, Min Xu, February 2016). A case-control study published since that meta-analysis similarly found that serum Se concentration was significantly lower in pre-eclampsia (P < 0.05) with a further significant difference between mild and severe cases (P < 0.05) [21]. Pre-eclampsia has also been shown to be associated with lower plasma glutathione peroxidase (GPx ) activity than normal pregnancy [22, 23], while significantly lower levels of GPx and thioredoxin reductase (TrxR ) have been found in placentae from pre-eclamptic women than from matched healthy controls [23, 24]. A case-control study found that the concentration of Se in toenails (laid down from 3 to 12 months previously) of women with pre-eclampsia was significantly lower than that of controls matched for age, gestational age and parity (P = 0.001) [25]. Women in the bottom tertile of toenail Se were 4.4-times [95 % CI 1.6, 14.9] more likely to have pre-eclampsia.
2.2 Se Supplementation in Pregnancy
Following the results of the case-control study discussed above, a randomized controlled trial (RCT) of Se supplementation in pregnancy was set up in the UK to assess whether a nutritional dose of Se could reduce the risk of pre-eclampsia, as measured by biomarkers of pre-eclamptic risk [26]. In a double-blind, placebo-controlled, pilot trial (SPRINT, Se in PRegnancy INTervention), 230 primiparous pregnant women were randomized to Se (60 μg/day, Se-yeast) or placebo-yeast from 12 to 14 weeks of gestation until delivery. Whole-blood Se was measured at baseline and 35 weeks, plasma SEPP1 at 35 weeks. The primary outcome measure was the anti-angiogenic factor, sFlt-1 (see above). Between 12 and 35 weeks, whole-blood Se concentration increased significantly in the Se-treatment group, but fell significantly in the placebo group. At 35 weeks, plasma SEPP1 concentration was significantly higher in the Se-treated group than in the placebo group. In line with the study hypothesis that Se supplementation would reduce sFlt-1 in women of low Se status, sFlt-1 was significantly lower at 35 weeks in the Se-treated group than in the placebo group in participants in the lowest quartile of Se status at baseline (P = 0.039) [6].
Further analysis of data and samples from that trial showed that the risk of pre-eclampsia and/or the related condition, pregnancy-induced hypertension , was significantly reduced in women with higher toenail Se (Odds Ratio 0.38, 95 % CI 0.17, 0.87; P = 0.021) [26]. As toenail Se is a likely biomarker of early pregnancy/pre-pregnancy Se status, this result suggests that having an adequate Se intake from very early pregnancy or even pre-pregnancy is important for the health of mother and baby.
There have been two other small trials of Se supplementation (100 μg/day) in the prevention of pre-eclampsia [27, 28]. The three trials have been entered into a meta-analysis [20]. Using a random-effects model , the relative risk for pre-eclampsia with Se supplementation was 0.28 (95 % CI 0.09, 0.84); P = 0.02 (see Fig. 30.1).
Forest plot of meta-analysis of the effect of Se supplementation on incidence of pre-eclampsia in three RCTs (RR = relative risk) (modified with permission from Xu et al. 2015 [20])
2.3 How Might Se Lower the Risk of Pre-eclampsia?
Se/selenoproteins can: i) protect endothelial cells, trophoblasts (and thereby the placenta) from oxidative stress [29–37]; ii) protect the endothelium and regulate vascular tone by controlling eicosanoid production [30, 38, 39]; and iii) help in the production of anti-inflammatory eicosanoid mediators [40] and repress inflammatory gene expression [40–42].
Se/selenoenzymes are also important to the heme-oxygenase (HO) system , which has been linked to antioxidant effects, successful placentation, inhibition of sFlt-1 release, uterine quiescence, placental hemodynamic control, and regulation of the apoptotic and inflammatory cascades in trophoblast cells [43–45]. Se has been shown to upregulate HO-1 by a number of pathways that involve Se or the thioredoxin/TrxR system either directly or indirectly, resulting in reduced expression of pro-inflammatory genes [46–49].
Perhaps the most important role of Se in affecting the risk of pre-eclampsia is its role in selenoprotein S1 (SEPS1 ), an ER membrane protein involved in the control of inflammation and ER stress [31, 50]. It helps remove stressor-induced misfolded proteins from the ER [31, 50], preventing their accumulation and the subsequent stress response that leads to activation of NF-kB, proinflammatory cytokine gene transcription and the inflammation cascade. Genetic variation in SEPS1 has been shown to influence the inflammatory response [51]. A retrospective study in a large Norwegian case-control cohort compared maternal genotype and allele frequencies of the SEPS1 g.-105G > A polymorphism in pre-eclamptic and control pregnant women [52]. Women with pre-eclampsia were 1.34 times more likely to have the GA or AA genotype (P = 0.0039; 95 % CI, 1.09, 1.64) suggesting that SEPS1 has a role in protection from pre-eclampsia in that population.
3 Miscarriage
First-trimester pregnancy loss affects up to 15 % of clinically recognized pregnancies but 2–4 % of couples will suffer recurrent losses, often with no identifiable cause [53]. Idiopathic miscarriage has been shown to be associated with Se deficiency in a range of human studies. In interpreting the results of such studies, it is important to be aware that excessive inflammation is a probable part of the picture in miscarriage [54] and will lower circulating Se [55, 56].
Significantly lower serum Se was found in 40 UK women who miscarried in the first trimester than in 40 control pregnant women of similar gestational age [57]. In a later study, the same investigators found significantly lower serum Se in 25 women who miscarried in the first trimester (52.1 μg/L) than in 12 (non-pregnant) recurrent aborters (67.1 μg/L) and 25 non-pregnant controls (76.6 μg/L) [58]. An Indonesian study of 46 women with normal pregnancies and 25 women with spontaneous abortion found significantly higher mean serum Se in those with normal pregnancies than in those with spontaneous abortion (76.36 ± 18.22 μg/L, vs. 66.71 ± 13.55 μg/L; P = 0.023), though serum GPx activity did not differ between the groups [59]. An Indian study found significantly lower red-cell Se in 20 (non-pregnant) women with ≥ 3 recurrent pregnancy losses than in a similar number of non-pregnant controls with no history of miscarriage [mean (SD) 119.55 (32.94) μg/L vs. 150.85 (37.63) μg/L, respectively; P < 0.01] [60]. Although a further UK study found significantly lower mean hair Se in 26 women with a history of recurrent miscarriage than in a control group of 18 women with good reproductive performance (mean (SD) 0.14 (0.09) μg/g vs. 0.34 (0.25) μg/g, P < 0.001), there was no difference in serum Se between the groups [61]. However, the method used to prepare the serum samples was inadequate and no certified reference material was used to validate the results .
Not all studies have found associations: whole-blood and plasma concentrations of Se were no different in Polish women who had just miscarried than in women of the same gestational age with viable pregnancies, though their red-cell and plasma GPx activiti es were significantly lower [62]. A Scottish study found lower plasma Se in non-pregnant women having recurrent miscarriage than in controls, but the difference did not reach significance [63]. However, the control group in that study did not exclude women who had had a miscarriage. A South African study found no difference in hair Se concentration in women with recurrent pregnancy loss and controls (median (range) 0.80 (0.19–4.15) μg/g vs. 0.68 (0.43–3.76) μg/g, respectively; P = 0.74) [64]. Hair Se concentration in these South African women, however, was considerably higher than in the earlier UK study that found a difference between groups [61]. Though on balance, there appears to be an association between low Se status and miscarriage, surprisingly, population Se status does not seem to be the discriminator.
Miscarriage resembles pre-eclampsia to some extent, i.e., failure/partial failure of immunoregulatory mechanisms, defective placentation, impaired placental perfusion, excessive placental oxidative stress and inflammation [54, 65]. At the extreme, the outcome is pregnancy loss; if the pregnancy continues, the result may be pre-eclampsia [65]. Thus, many of the mechanisms discussed above in relation to the effect of Se on the risk of pre-eclampsia will also be relevant to its potential effect on miscarriage.
HO-1 is likely to be important in the context of miscarriage: upregulation of HO-1 expression diminished fetal rejection and abortion rates in a murine abortion model [66]. Furthermore, HO-1 upregulation may also augment the levels of regulatory T cells, improving immune suppression [66]. Se/TrxR may upregulate the expression of HO-1 by a number of pathways that would be protective against abortion [46–49].
4 Preterm Birth
Preterm birth , i.e., birth before 37 weeks of gestation, occurs in 5–13 % of pregnancies and is the most important cause of perinatal morbidity and mortality [67]. Short- and long-term outcomes include cerebral palsy, respiratory-distress syndrome, neurodevelopmental impairment, difficulties with schooling and behavioral problems [68].
Se concentrations in blood components have been compared between term and preterm mothers. Four studies found no difference between the term and preterm groups [69–72], while two others found significantly lower Se in the preterm group [73, 74]. The discordant results cannot be rationalized on the basis of the Se status of the countries in which the studies took place. Inadequate sample size may well be part of the explanation for the disparity in results.
By far, the largest study to date was carried out in the Netherlands: 1129 pregnant women were followed prospectively from 12-weeks of gestation, of whom 60 (5.3 %) gave birth preterm [75]. The commonest causes of preterm delivery were preterm premature rupture of membranes (PPROM , n = 21) and pre-eclampsia (n = 13), together accounting for 57 % of the preterm births. Those who delivered preterm had significantly lower serum Se at 12 weeks gestation than those who delivered at term [mean (SD): 75.8 (11.1) μg/L and 80.5 (10.3) μg/L, respectively, P = 0.001] [75]. The percentages of women with preterm birth by quartile of serum Se at 12 weeks were significantly different (P < 0.05). Even after adjusting for the occurrence of pre-eclampsia, which is associated both with Se status (see above [25, 26]) and with preterm birth, women in the lowest quartile of serum Se at 12-weeks of gestation had twice the risk of preterm birth as the rest (adjusted OR 2.18; 95 % CI 1.25–3.77). Results also suggest that low Se status in early gestation may increase the risk of PPROM, a major cause of preterm birth [69].
The above study does not show that low Se status caused preterm birth. Both preterm birth and low plasma Se may have been joint outcomes, for instance, of increased inflammation [77]. Plasma Se concentration decreases in proportion to the magnitude of the inflammatory response [57, 58]. However, the significant reduction also seen in the incidence of PPROM with Se supplementation in a small RCT in Iran suggests that Se status may indeed be relevant [76].
4.1 How Might Se Affect the Risk of Preterm Birth?
Se status in the Netherlands is relatively low [77]. Se (probably as selenoproteins) has a number of protective effects that are directly relevant to pathways implicated in preterm birth or its sub-categories, PPROM and pre-eclampsia . These pathways include infection, inflammation, defective placentation, placental ischemia-reperfusion, oxidative stress, the presence of anti-thyroid antibodies, and premature extracellular-matrix-degradation of fetal membranes [67–80].
Se is required for an adequate immune response [81], so low Se status in either the mother or the fetus is a risk factor for infection, a major cause of preterm birth [67]. Inflammation may be an underlying factor linking many of these pathways as suggested by the fact that polymorphisms that affect the magnitude or duration of the inflammatory response were associated with the risk of preterm birth [82]. Se is capable of attenuating the excessive inflammatory response associated with adverse pregnancy outcomes by a number of mechanisms that have already been discussed [30, 40–43, 46–49, 52, 83–85]. Defective placentation and placental ischemia-reperfusion are both counteracted by HO-1, which is upregulated by a number of pathways that involve Se or the thioredoxin/TrxR system, either directly or indirectly [46–49]. Oxidative stress is counteracted by the GPxs [30], by SEPP1 (which scavenges peroxynitrite) [30, 36] and by the antioxidant effects of the products of HO-1 (biliverdin and/or bilirubin) [43, 44, 84]. Higher Se status or supplementation with Se appears to be able to reduce the titer of antithyroid antibodies, in particular, thyroid peroxidase autoantibodies (TPO-Ab ) [86] (see next section).
5 Autoimmune Thyroid Disease
Autoimmune thyroid disease has a prevalence ranging between 5 and 20 % and is the main cause of hypothyroidism in pregnant women [87]. While the incidence of gestational hypothyroidism is 2.4 %, thyroid autoantibodies are present in 55–80 % of these women [87]. Some 6 % of pregnant women have TPO-Ab [88] though the titer tends to decrease towards term, reflecting the down-regulation of the immune system during gestation [89]. An elevated TPO-Ab titer is associated with poor obstetric outcome including an increased risk of miscarriage [90], perinatal mortality [91], placental abruption [88] and PPROM [92].
Se is important to the thyroid. Not only is it a component of the iodothyronine deiodinase selenoenzymes that convert thyroxine (T4) to tri-iodothyronine (T3) and reverse T3, but it is also a component of GPx3 which protects thyroid cells from the hydrogen peroxide that is generated there [93]. This protective function may be the basis of the beneficial effect of Se supplementation found in patients with autoimmune thyroiditis in a recent meta-analysis of RCTs where a significant decrease in TPO-Ab titer was found at 6 and 12 months [86]. More important in the context of pregnancy is the reduction in thyroid inflammatory activity and the risk of postpartum thyroid disease found in an RCT of Se supplementation in TPO-Ab-positive women in Italy [94]. During pregnancy and the postpartum period, 151 TPO-Ab -positive women were randomized to Se (200 μg/day as selenomethionine) or placebo. TPO-Abs fell significantly during gestation but the reduction was significantly greater in the Se-supplemented group (P = 0.01) and remained so in the post-partum period (P = 0.01) (see Fig. 30.2). Importantly, there was a significant reduction in the incidence of post-partum thyroid disease and hypothyroidism in the Se-supplemented group (28.6 % vs. 48.6 %, P < 0.01 and 11.7 % vs. 20.3 %, P < 0.01, respectively) [94].
Thyroid peroxidase antibody (TPO-Ab ) titers in 151 TPO-Ab-positive Italian women randomized to Se (200 μg/day as selenomethionine) or placebo during pregnancy and the postpartum period. Values significantly different between groups at delivery (280 days) and in the postpartum period (modified from Negro et al. 2007 [99])
The only other RCT that investigated the effect of Se supplementation on autoimmune thyroid disease in pregnancy was a secondary analysis of samples and data from the SPRINT pilot RCT where 230 women at 12 weeks of gestation were randomized to receive 60 μg/day Se or placebo until delivery [95]. No difference was found in the magnitude of decrease between Se and placebo groups (54.2 % vs. 65.6 %, P = 0.785). The difference in results from those of the earlier study [94] can probably be explained by three factors: i) there were only 25, as opposed to 151, TPO-Ab-positive women, thus the trial lacked power; ii) the median baseline TPO-Ab concentration in the women was much lower: 110 kIU/L vs. 600 kIU/L (higher concentration appears to respond better to treatment [93]); and iii) the Se dose given was much lower, i.e., 60 μg/day vs. 200 μg/day. There is clearly a need for another adequately powered RCT in TPO-Ab-positive pregnant women to see if the results of Negro et al. [94] can be replicated.
5.1 How May Se Affect the Risk of Autoimmune Thyroid Disease in Pregnancy?
In pregnancy, a woman has to increase her production of T4 by 50 % to maintain maternal euthyroidism and to transfer thyroid hormone to the fetus in the first trimester before its own thyroid starts to function [96]. The increased synthesis of thyroid hormones triggers a rise in the production of hydrogen peroxide that is used by TPO in the synthesis of T4 from iodide and thyroglobulin [93]. As hydrogen peroxide is damaging, any excess must be removed for the protection of the thyroid, largely by GPx3, which is highly expressed in thyrocytes [93]. Thus, the requirement of the thyroid for Se in pregnancy probably increases above the non-pregnant level.
TPO-Ab s tend to correlate with lymphocytic inflammation of the thyroid. Hence, apart from the specific role of Se in GPx3, the anti-inflammatory effects of the selenoenzymes might play a role in down-regulating TPO-Abs during gestation as previously outlined [30, 40–43, 46–49, 83–85].
6 Insulin Resistance
Concern has been expressed in recent years that Se may increase the risk of type-2 diabetes though there are few studies investigating this potential effect in pregnancy. An adverse effect of Se, or at least of a selenoprotein was suggested by a study in pregnant women without gestational diabetes (GDM ), where the activity of GPx1, in erythrocytes increased during gestation and was positively associated with fasting plasma glucose, plasma insulin, C-peptide and the homoeostasis model of assessment for insulin resistance (HOMA-IR) index [97]. By contrast, the literature also shows that pregnant women with impaired glucose tolerance or GDM have much lower serum Se concentrations than women with normal pregnancies [98–101] and that there is an inverse relationship between serum Se and blood-glucose concentration [100, 101]. Furthermore, in a small group of pregnant women, the increase in plasma glucose following an oral glucose tolerance test administered at 12 weeks of gestation was inversely correlated with plasma Se concentration [102]. Recently, an RCT of Se (200 μg/d) in 70 women who had developed GDM found a significant reduction in fasting plasma glucose, serum insulin and HOMA-IR in those on Se [103].
There has been only one RCT of the effect of Se supplementation on the risk of GDM or insulin resistance in normal pregnant women. Stored plasma samples from the SPRINT RCT of Se supplementation in pregnancy [6] were used to test the effect of Se supplementation on a marker of insulin resistance pregnant women in the UK [104]. Plasma adiponectin concentration, a recognized marker of insulin resistance [105] and a strong independent predictor of the risk of GDM and type-2 diabetes [106, 107] that can be used in non-fasted samples was measured at 12 and 35 weeks [104]. There was no significant difference between the two treatment groups in the change in adiponectin from 12 to 35 weeks (P = 0.938), nor when the analysis was restricted to the bottom or top quartiles of baseline whole-blood Se (P = 0.515 and 0.858, respectively) [104]. The results of this RCT, though probably underpowered, help to allay fears that a small dose of Se will increase insulin resistance in pregnant women of modest Se status.
7 Concluding Remarks
Despite the positive evidence cited above, the role of Se/selenoproteins in the etiology of adverse conditions of pregnancy has still not been clearly established. There are few RCTs, which alone are capable of establishing causation, and those that there are, are largely underpowered, though we do have an excellent study in autoimmune thyroid disease and a meta-analysis with a significant result in the case of pre-eclampsia. In case-control studies of Se in pregnancy, which constitute the majority of the evidence, it is vital to match controls to cases on age, gestational age and parity, all of which can affect Se status. Only one of the cited studies has been matched on those three parameters [25]. Many also lack important information such as the Se status of the groups, and adequate detail of analytical methodology. There are few large prospective studies [75] though in any case they cannot establish causality.
We need more RCTs, properly powered, and these should be run in populations with relatively low Se status, e.g., plasma Se ≤90 μg/L. We already have an excellent RCT in autoimmune thyroid disease that requires replication and a strong rationale for a very early intervention with Se to reduce the risk of pre-eclampsia.
References
CW Redman, IL Sargent 2005 Science 308:1592
TH Hung et al 2010 Reprod Sci 17:401
AM Smith, MF Picciano 1986 J Nutr 116:1068
JA Butler et al 1982 Am J Clin Nutr 36:15.
BA Zachara et al 1993 Gynecol Obstet Invest 35:12
MP Rayman et al 2014 Br J Nutr 112:99
JW Kasik, EJ Rice 1995 Placenta 16:67
RF Burk et al 2013 FASEB J 27:3249
L Duley 2009 Semin Perinatol 33:130
EA Steegers et al 2010 Lancet 376:631
N Sattar, IA Greer 2002 BMJ 325:157
GJ Burton, E Jauniaux 2004 J Soc Gynecol Investig 11:342
CA Hubel 1999 Proc Soc Exp Biol Med 222:222
J Vanderlelie et al 2005 Placenta 26:53
GJ Burton et al 2009 Placenta 30:S43
RJ Levine et al 2004 N Engl J Med 350:672
AP Cockell 1997 Br J Obstet Gynaecol 104:235
JM Roberts 1989 Am J Obstet Gynecol 161:1200
JJ Vanderlelie 2011 Pregnancy Hypertens 1:213
M Xu et al 2015 Biol Trace Elem Res doi:10.1007/s12011-015-0545-7
MM Haque et al 2016 J Trace Elem Med Biol 33:21
VM Chamy et al 2006 Biol Res 39:229
HD Mistry et al 2008 Hypertension 52:881
SW Walsh, Y Wang 1993 Am J Obstet Gynecol 169:1456
MP Rayman et al 2003 Am J Obstet Gynecol 189:1343
MP Rayman et al 2015 Br J Nutr 113:249
L Han, S Zhou 1994 Chinese Med J 107:870
F Tara et al 2010 Taiwan J Obstet Gynecol 49:181
A Khera et al 2013 Placenta 34:594
R Brigelius-Flohé et al 2003 Antioxid Redox Signal 5:205
VA Shchedrina et al 2010 Antioxid Redox Signal 12:839
MH Lewin et al 2002 Biochim Biophys Acta 1593:85
S Miller et al 2001 Clin Sci (Lond) 100:543
JP Thomas et al 1993 J Lipid Res 34:479
X Lu et al 1994 Cardiovasc Res 28:345
GE Arteel et al 1999 FEBS Lett 445:226
H Traulsen et al 2004 Free Radic Res 38:123
LM Sordillo et al 2005 Prostaglandins Other Lipid Mediat 76:19
YZ Cao et al 2000 Free Radic Biol Med 28:381
H Vunta et al 2007 J Biol Chem 282:17964
H Vunta et al 2008 Mol Nutr Food Res 52:1316
RM Touyz, EL Schiffrin 2006 Vascul Pharmacol 45:19
SA Bainbridge, GN Smith 2005 Free Radic Biol Med 38:979
A Ahmed et al 2000 Mol Med 6:391
M Cudmore et al 2007 Circulation 115:1789
WL Trigona et al 2006 Biochem J 394:207
K Ejima et al 2002 Antioxid Redox Signal 4:569
TS Lee et al 2003 J Biol Chem 278:19325
G Krönke et al 2007 Arterioscler Thromb Vasc Biol 27:1276
M Stoedter et al 2010 Biochem J 429:43
JE Curran et al 2005 Nat Genet 37:1234
EK Moses et al 2008 Am J Obstet Gynecol 198:336.e1-5
JL Allison, DJ Schust 2009 Curr Opin Endocrinol Diabetes Obes 16:446
OB Christiansen et al 2006 Semin Fetal Neonatal Med 11:302
C Nichol et al 1998 Clin Chem 44:1764
K Hesse-Bähr et al 2000 Biofactors 11:83
JW Barrington et al 1996 Br J Obs Gynaecol 103:130
JW Barrington et al 1997 J Obs Gyn 17:199
R Abdulah et al 2013 Biol Trace Elem Res 154:1
KS Kumar et al 2002 J Obstet Gynaecol 22:181
AS Al-Kunani et al 2001 BJOG 108:1094
BA Zachara et al 2001 BJOG 108:244
AE Nicoll et al 1999 BJOG 106:1188
VV Thomas et al 2013 BMC Womens Health 13:40
CW Redman, IL Sargent 2010 Am J Reprod Immunol 63:534
A Leber et al 2011 Methods Mol Biol 677:397
RL Goldenberg et al 2008 Lancet 371:75
S Saigal, LW Doyle 2008 Lancet 371:261
DC Wilson et al 1991 Early Hum Devel 26:223
G Mask, HW Lane 1993 Nutr Res 13:901
W Wasowicz et al 1993 Biol Trace Elem Res 38:205
R Iranpour et al 2009 Zhongguo Dang Dai Er Ke Za Zhi 11:513
W Dobrzynski et al 1998 Analyst 123:93
G Gathwala et al 2003 Indian J Public Health 47:45
MP Rayman et al 2011 CMAJ 183:549
F Tara et al 2010 J Obstet Gynaecol 30:30
PA van den Brandt et al 1993 Cancer Epidemiol Biomarkers Prev 2:107
R Romero et al 2006 Semin Fetal Neonatal Med 11:317
J Cleary-Goldman et al 2008 Obstet Gynecol 112:85
S Parry, JF Strauss 3rd 1998 N Engl J Med 338:663
MP Rayman 2012 Lancet 379:1256
D Holst, Y Garnier 2008 Eur J Obstet Gynecol Reprod Biol 141:3
M Ricote et al 1998 Nature 391:79
KA Kirkby, CA Adin 2006 Am J Physiol Renal Physiol 290:F563
Y Gao et al 2006 Cytokine 33:246
Y Fan et al 2014 Int J Endocrinol 2014:904573
GE Krassas et al 2010 Endocr Rev 31:702
M Abbassi-Ghanavati et al 2010 Obstet Gynecol 116:381
PP Smyth et al 2005 Thyroid 15:474
MF Prummel, WM Wiersinga 2004 Eur J Endocrinol 150:751
T Männistö et al 2009 J Clin Endocrinol Metab 94:772
JE Haddow et al 2010 Obstet Gynecol 116:58
Köhrle J, Gartner R 2009 Best Pract Res Clin Endocrinol Metab 23:815
R Negro et al 2007 J Clin Endocrinol Metab 92:1263
J Mao et al 2014 Eur J Nutr doi:10.1007/s00394-014-0822-9
MB Zimmermann 2009 Endocr Rev 30:376
X Chen et al 2003 J Clin Endocrinol Metab 88:5963
M Tan et al 2001 Biol Trace Elem Res 83:231
E Al-Saleh et al 2004 J Matern Fetal Neonatal Med 16:15
M Kilinc et al 2008 Biol Trace Elem Res 123:35
S Bo et al 2005 Nutrition 21:186
Hawkes WC et al 2004 Biol Trace Elem Res 100:19
Z Asemi et al 2015 Nutrition 31:1235
J Mao et al 2016 Br J Nutr 115:32
K Kishida et al 2012 Immune Disord Drug Targets 12:118
K Hotta et al 2000 Arterioscler Thromb Vasc Biol 20:1595
S Li et al 2009 JAMA 302:179
Acknowledgements
I gratefully acknowledge financial support from the Wellcome Trust.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Rayman, M.P. (2016). Is Adequate Selenium Important for Healthy Human Pregnancy?. In: Hatfield, D., Schweizer, U., Tsuji, P., Gladyshev, V. (eds) Selenium. Springer, Cham. https://doi.org/10.1007/978-3-319-41283-2_30
Download citation
DOI: https://doi.org/10.1007/978-3-319-41283-2_30
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-41281-8
Online ISBN: 978-3-319-41283-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)