Abstract
Bacterial infection is found to be the cause of death throughout the world. Nuclear medicine imaging with the help of radiopharmaceuticals has great potential for treating infections. In the present work, clindamycin, a lincosamide antibiotic, was labeled with technetium-99 m (~380 MBq). Clindamycin has been proven to be efficient for treating serious infections caused by bacteria such as Staphylococcus aureus. Quality control, characterization, biodistribution, and scintigraphy of radiolabeled clindamycin were done, and labeling efficiency was determined by ascending paper chromatography. More than 95 % labeling efficiency with technetium-99 m (99mTc) was achieved at pH 6–7 while using 2.5–3 μg SnCl2 · H2O as a reducing agent and 100 μg of ligand at room temperature. The characterization of the compound was performed by using electrophoresis, HPLC and shake flask assay. Electrophoresis indicates the neutral behavior of 99mTc-clindamycin. HPLC analysis confirms the single specie of the labeled compound, while shake flask assay confirms high lipophilicity. The biodistribution studies of 99mTc-clindamycin were performed Sprague Dawley rats bearing bacterial infection. Scintigraphy and biodistribution studies showed a high uptake of 99mTc-clindamycin in the liver, heart, lung, and stomach as well as at S. aureus-infected sites in rabbits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infection and Inflammation are posing a high impact on clinical practices as localization and diagnosis of infection or inflammation sites is a significant clinical issue. Inflammation is the reaction of body tissues to an external injury or the result of infectious agents (bacteria, fungi, viruses, and parasites). Inflammation results in the activation of inflammatory mediators of immune system causing increased vascular permeability resulting in the accumulation of granulocytes in case of acute inflammation and lymphocytes and microphages in case of a chronic type of inflammation. Infection is invasion of the body or part of the body by any infectious agent causing an injurious effect resulting in symptoms of redness, heat, or swelling. Infection/inflammation diagnosis at very early stages is a major task for medical practitioners these days. Different medical imaging techniques in use are X-rays, computed tomography (CT), ultrasonography, and magnetic resonance imaging (MRI), but these emphasize on morphologic abnormalities and nonspecific for infection diagnosis. Also, these are incapable to identify the microorganisms causing the infection. The identification and localization of infection locus is very crucial for early diagnosis and medical treatment of the patients under clinical trials. Nuclear medicines are found to be a very powerful tool for the diagnosis and therapy of infectious and inflammatory diseases by whole body imaging. Radiopharmaceuticals can aid in the diagnosis of deep-seated lesions or infections in the body, providing the information at a molecular and cellular level, evaluating the pathophysiological and biochemical processes in the patients. A large number of radiopharmaceuticals have been developed that act specifically or nonspecifically at the infection site, and some of them can precisely differentiate between infection and inflammation. Radiotracers such as 67gallium-citrate, antigranulocyte monoclonal antibodies, and autologous leucocytes have been used for detection of infection or inflammation by scintigraphic imaging, but they are nonspecific in action. An ideal radiotracer locates the infection locus by rapid very specific uptake at infection site, low accumulation in normal tissues, rapid clearance, and absence of immune response of the body. Technetium-99 m (99mTc) is the most suitable radionuclide since it has found all these ideal properties. Technetium-99 m is commonly eluted from commercially available 99Mo/99mTc generator system and is available at all nuclear medical centers. Due to its favorable characteristics of convenient half-life (6 h), there was almost no radiation burden for patients, and 140 keV gamma ray emission was best for imaging. 99mTc-labeled antibiotics have been recently introduced as infection-seeking tracers. Several 99mTc-labeled compounds such as 99mTc-erythromycin [1],99mTc-ceflizoxime [2], 99mTc-enrofloxacin [3], 99mTc-ciprofloxacin [4–8], 99mTc-lomefloxacin and 99mTc-ofloxacin complexes [9], 99mTc-pefloxacin [10], 99mTc-kanamycin [11], 99mTc-ethambutol [12], 99mTc-fluconazole [13], 99mTc-vancomycin [14], 99mTc-dextran [15], 99mTc-tetrofosmin [16], 99mTc-cefuroxime [17], 99mTc-piroxicam [18], and 99mTc-infecton [19] have been developed for imaging purposes, and some of them are routinely employed in diagnostic nuclear medicine [20]. The use of radiolabeled antibiotics presents a promising approach for the precise diagnostic and detection of infectious lesions, because they may specifically bind to the bacterial components, making it possible to discriminate between bacterial infection and sterile inflammation [21–25]. Clindamycin is a bactericidal antibiotic of lincosamide family that fights against bacteria in the body. Clindamycin is used for treatment of various bacterial infections which include respiratory tract, dental, skin, soft tissue, acne, vaginosis, peritonitis, and toxic shock syndrome [26]. It is also used to treat bone and joint infections, particularly useful against some methicillin-resistant Staphylococcus aureus (MRSA) infections [27].
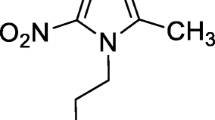
In the present work, the direct labeling of clindamycin (Fig. 1) with 99mTc was evaluated. Labeling efficiency, quality control, bacteria binding assay, stability, biodistribution, and scintigraphic imaging were performed.
Experimental
Materials and Methods
Clindamycin for intravenous injection was obtained from Ameer Medical and Superstores, Islamabad, Pakistan. Na99mTcO4 was eluted from a locally produced fission-based PAKGEN 99Mo/99mTc generator, with 0.9 % saline. All other reagents used were of analytical grade and purchased from E. Merck, Germany. S. aureus [American Type Culture Collection (ATCC 25923)] was obtained from National Institute of Health (NIH), Islamabad. All animal experiments followed the principles of laboratory animal care and were approved by the Institutional Animal Ethics committee. The animals were kept under standard conditions with free access to food and water. Tissue and organ radioactivity was measured with a gamma counter (Ludlum model 261). Gamma scintillation camera was used for imaging of rabbits.
Preparation of 99mTc-Clindamycin
For the radiolabeling of 99mTc-clindamycin, the optimum conditions were determined. The varying amounts of clindamycin (ligand) and SnCl2 · 2H2O (reducing agent) were used. The pH of the solution was adjusted by using 0.5 M NaOH. Ascorbic acid (3 mg) was used as a stabilizer in the reaction mixture. After adding all reagents, the mixture was stirred for few minutes and freshly eluted ~380 MBq 99mTcO4 − in isotonic saline was injected into the vial and left to react at room temperature. The volume of reaction mixture was ~1.5 mL.
Quality Control of 99mTc-Clindamycin
Instant thin-layer chromatography (ITLC) was used to access the radiochemical purity of 99mTc-clindamycin. In ITLC, the sample of 99mTc-clindamycin (1 μL) was spotted on silica gel plates (Gelman Laboratories) and was developed using 0.5 M NaOH as the mobile phase. In this system, 99mTc-clindamycin and free pertechnetate migrated with the solvent front of the mobile phase and the colloid was found at the origin of the strip. To determine the 99mTcO4 − content of the preparations, a strip of Whatman Paper No. 3 was developed using acetone as the mobile phase. In this system, 99mTcO4 − migrated with the solvent front of the mobile phase (R f = 1.0) while labeled/reduced hydrolyzed 99mTc remained at origin. The distribution of labeled, free and hydrolyzed chromatographic strips was measured using a 2π Scanner (Berthold, Germany). Otherwise, the strips were cut into segments of 1 cm and counted using a gamma counter.
HPLC of 99mTc-Clindamycin
The analysis of 99mTc-clindamycin was performed by D-200 Elite HPLC system using the analytical column of C-18 (Alltech) as a stationary phase. The mixture of acetonitrile and 0.02 M sodium dihydrogen phosphate (pH adjusted up to 2–3 by using 0.5 M NaOH) was used as a mobile phase in the ratio 850:150 % (v/v). The flow rate of the mobile phase was adjusted up to 1 mL per min. UV detector was used for detection purpose, and work was performed at a wavelength of 215 nm. Radiation detector was used for monitoring of 99mTc activity.
Electrophoresis and Lipophilicity Test of 99mTc-Clindamycin
Electrophoretic experiments of the 99mTc-clindamycin were performed by using deluxe electrophoresis chamber (Gelman) system. Whatman No. 1 paper strip of 30 cm and phosphate buffer (pH 6.8) were used in this experiment. A drop of 99mTc-clindamycin was placed at the midpoint of the strip, and a voltage of 300 V was applied for 30–60 min at room temperature. After completion of electrophoresis, the strip was dried and scanned using a 2π scanner for the charge on 99mTc-clindamycin.
Shake flask method was used for determination of lipophilicity. The partition coefficient was determined by mixing the complexes with an equal volume of 1-octanol and phosphate buffer (0.025 M, pH 7.0 and 7.4) in a centrifuge tube. The mixture was vortexed at room temperature for 1 min and then centrifuged at 5,000 rpm for 5 min. From each phase, 0.1 mL of the aliquot was pipetted and counted in a well gamma counter. The measurement was repeated three times. The partition coefficient (p) was calculated using the following equation: \( p=\frac{\mathrm{cpm}\ \mathrm{in}\ \mathrm{octanol}-\mathrm{cpm}\ \mathrm{in}\ \mathrm{background}}{\mathrm{cpm}\ \mathrm{in}\ \mathrm{buffer}-\mathrm{cpm}\ \mathrm{in}\ \mathrm{background}}. \)
In Vitro Stability Test
To test the serum stability of the 99mTc-clindamycin complex, we added 1.8 mL of normal human serum with 0.2 mL of 99mTc-clindamycin which was incubated in 37 °C for different time intervals up to 24 h; 0.2 mL aliquots were withdrawn and analyzed by instant thin-layer chromatography for determination of 99mTc-clindamycin, reduced/hydrolyzed 99mTc, and free 99mTcO4 −.
Culturing of S. aureus
Labeled 99mTc-clindamycin can be used for infection diagnosis caused by S. aureus (ATCC 25923). S. aureus ATCC 25923 was obtained from the American Type Culture Collection. Overnight cultures of S. aureus bacteria were prepared in brain heart infusion (BHI) broth (Oxoid) in a shaking water bath at 37 °C. Aliquots of suspensions containing viable stationary phase bacteria were snap frozen in liquid nitrogen and stored at −70 °C. Just before use, an aliquot of this suspension was rapidly thawed in a water bath at 37 °C and diluted in sodium phosphate buffer (Na-PB).
In Vitro Cell Binding Studies
Binding of 99mTc-clindamycin to S. aureus bacteria was assessed using the method described elsewhere [21]. Briefly, 0.1 mL of Na-PB containing ~5 MBq of 99mTc-clindamycin was transferred to a sterilized test tube; 0.8 mL of 50 % (v/v) of 0.01 M acetic acid in Na-PB containing about 1 × 108 viable bacteria was added. The mixture was incubated for 1 h at 4 °C and then centrifuged for 10 min at 2,000 g at 4 °C. The supernatant was removed, and the bacterial pallet was suspended again in 1 mL of ice-cooled Na-PB. The supernatant was removed, and the radioactivity in the bacterial pallet was determined using a gamma counter. The supernatant were also counted. The radioactivity related to bacteria was expressed in a percent of the added 99mTc activity bound to viable bacteria in regard to total 99mTc activity. For comparison purposes, in vitro binding study of 99mTc-clindamycin with S. aureus and 99mTc-ascorbic acid was also performed.
Labeling Ascorbic Acid with Tc-99 m
One milligram ascorbic acid was dissolved in 1 mL pure water, the pH adjusted to 5 with 0.1 M NH4OH solution, and then 0.2 mL of SnCl2 · H2O (1 mg/1 mL 0.1 M HCl) and 0.5 mL of Na99mTcO4 (100 MBq) in saline were added to the vial. The reaction vial was left at 25 °C for 20 min. The radiochemical purity of the labeled compound was checked with TLC [22].
Induction of Infectious Foci
A single clinical isolation of S. aureus from biological samples was used to produce focal infection. Individual colonies were diluted in order to obtain turbid suspension containing 2 × 108 colony-forming units (cfu) of S. aureus in 0.2 mL of saline intramuscularly injected into the left thigh of rats [23, 24]. Then, the rats were left for 24 h to get a visible swelling in the infected thigh. Three rats were used for one set of experiment.
Induction of Noninfected Inflammation with Heat-Killed S. aureus
Sterile inflammation was induced by injecting 0.2 mL of heat-killed S. aureus intramuscularly in the left thigh muscle of the rats. Two days later, swelling appeared. The S. aureus suspension was given with a temperature of 100 °C for 2 h for heat killing.
Induction of Noninfected Inflammation
Sterile inflammation was induced by injecting 0.2 mL of turpentine oil [25] in the left thigh muscle of the rats, intramuscularly. After 2 days, the swelling appeared.
Biodistribution
The study was approved and was in accordance with the guidelines set out by animal ethics committee. The animals were intravenously injected with 0.2 mL of 99mTc-clindamycin (~38 MBq) via the tail vein. After a definite time, the rats were sacrificed at 1, 4, and 24-h post-injection after ether anesthesia. Samples of the different organs were removed and counted for activity distribution in a well-type gamma counter. The average percent values of the administrated dose/organ were calculated. By cardiac puncture, 1 mL blood was taken and weighed. Activity in total blood was calculated by assuming a blood volume of 6.34 % of body weight.
Bioevaluation by Scintigraphy
The evaluation of 99mTc-clindamycin as a potential imaging agent was done by acquisition study in rabbit models by single-headed Siemens Integrated Orbiter Gamma Camera System interfaced with a high-resolution parallel-hole collimator. The infection was introduced by injecting 0.4 mL of S. aureus containing 2 × 108 cfu in saline intramuscularly in the left thigh muscle of rabbit. After ethical approval, anesthetized animal was placed on a flat hard surface with both hind legs spread out and all legs fixed with surgical tape. After injecting diazepam (5 mg) into the right thigh muscle, saline (0.2 mL) containing 38 MBq of 99mTc-clindamycin was injected intravenously into the marginal ear vein. Immediately after injection, dynamic acquisition with both thighs in focus was done for 120 min.
Results and Discussion
Labeling and Radiochemical Purity
Figures 2 and 3 depict the R f of labeled reduced/hydrolyzed and free 99mTc. At low pH (3–5), the labeling efficiency was minimum (80 %), while at pH 6–7, labeling efficiency of 99mTc-clindamycin was >95 % (Fig. 4). In basic media at pH 9, the labeling efficiency decreased to 68 %. The amount of reducing agent, SnCl2 · 2H2O with the highest labeling efficiency, was 2.5–3 μg, and a value of 2.8 μg of SnCl2 · 2H2O was chosen (Fig. 5). The amount of ligand having the highest labeling efficiency was 100 μg as shown in Fig. 6. The maximum complexation of 99mTc with clindamycin is achieved after 30 min and maintained for up to 12 h (Fig. 7). The radiochemical purity was assessed by ascending paper chromatography and instant thin-layer chromatography on silica gel. In paper chromatography, acetone was used as the solvent for free 99mTcO4 −, while in ITLC-SG chromatography, 0.5 M NaOH was used as the solvent for 99mTc-clindamycin and reduced/hydrolyzed 99mTc. In current study, clindamycin was labeled with 99mTc with high radiochemical yields. During the labeling of clindamycin, <2 % colloid and <2 % free pertechnetate were observed. The results obtained using this method were in excellent agreement with 99mTc-cefuroxime in which 95 % stability was seen in a labeled kit [28].
Stability Test
99mTc-clindamycin was fully stable in human serum during incubation as determined by ITLC. At 37 °C, up to 92 % labeling was found at 24 h of incubation and there was almost no increase in reduced/hydrolyzed 99mTc while very little increase was observed in free 99mTcO4 −. The total impurities were <5 % (Table 1).
Electrophoresis and HPLC
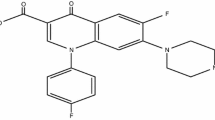
The electrophoresis results illustrate the neutral nature of ligand and the movement of free pertechnetate towards an anode after 1 h (Fig. 8). The lipophilicity test indicates that 99mTc-clindamycin is >99 % in organic layer and <1 % in aqueous layer, hence proving the lipophilic nature of 99mTc-clindamycin. Clindamycin contains a basic pyrrolidine ring attached to a sugar group through an amide bond. The replacement of the hydroxyl group in lincomycin to a chloride atom increases the lipophilicity, and therefore, clindamycin shows better absorption and penetration into bacterial cells. The radiochromatogram of 99mTc-clindamycin is given in Fig. 9 which shows a very sharp peak at 8.5 min of retention. This signal at 8.5 min represents the 99mTc-clindamycin labeling efficiency greater than 95 %. The HPLC analysis of inactive ligand by UV detector shows a percent purity of clindamycin (Fig. 10).
In Vitro Binding Studies
In vitro binding of 99mTc-clindamycin to bacteria was compared to 99mTc-ascorbic acid. Binding of 99mTc-clindamycin was in the range of 95–98 % (Table 2), while binding of 99mTc-ascorbic acid was <5 % (Table 3). Different amounts of 99mTc-clindamycin (10–100 μg) showed similar binding efficiency with bacteria. In vitro studies and animal experiments have shown that 99mTc-clindamycin localizes in bacteria-infected sites significantly. Due to the ease of 99mTc-clindamycin preparation and infection uptake, it may provide an alternative to 99mTc-ciprofloxacin in a variety of patients referred for infection evaluation [26, 27].
99mTc-Clindamycin Biodistribution and Scintigraphic Images
The biodistribution results (% injected activity/g) of 99mTc-clindamycin in different organs of the animals infected with living, heat-killed S. aureus and turpentine oil induced at 1, 4, and 24 h after intravenous administration are shown in Table 4. The results show that the 99mTc-clindamycin accumulates significantly high at the infected thigh muscle as compared to heat-killed S. aureus and turpentine oil-infected group of animals. Our studies in rats with intramuscular infection indicated that the uptake in the infected tissue is attributed to specific binding to living bacteria. Thus, in this study, we can establish the basis for the potential of 99mTc-clindamycin to distinguish bacterial from nonbacterial infection. As shown in Table 4, rats with infectious lesions injected with 99mTc-clindamycin showed a mean target-to-nontarget (T/NT) ratio equal to 3.1 ± 0.3 after 1 h post-injection, 2.56 ± 0.2 at 2 h post-injection, and 2.37 ± 0.5 at 24 h post-injection. 99mTc-clindamycin shows higher T/NT in the infected muscle (live S. aureus) at all-time intervals than that of sterile inflamed muscle (heat-killed S. aureus and turpentine). This 99mTc-clindamycin showed a slightly lower uptake in infected tissue than 99mTc-ciprofloxacin (T/NT = 3.8 ± 0.8) [29–31]. The mean abscess-to-muscle (T/NT) ratio for 99mTc-clindamycin was higher than that of other recently published 99mTc-labeled antibiotics such N-sulfanilamide (T/NT = 2.9 ± 0.1) [32] and streptomycin (T/NT = 2.4 ± 0.1) [33]. Our studies in rats with intramuscular infection indicated that the uptake in the infected tissue is attributed to specific binding to living bacteria. Thus, in this study, we can establish the basis for the potential of 99mTc-clindamycin to distinguish bacterial from nonbacterial infection. The infection is clearly visible at 3 h post-administration. The uptake of radioactivity in infected thigh muscle (target) at intervals of 1, 4, and 24 h post-injection was 1.94 ± 0.3, 2.38 ± 0.2, and 1.99 ± 1.2, respectively, and that of normal (nontarget) was 0.61 ± 0.3, 0.93 ± 0.2, and 0.84 ± 0.2, respectively, indicating a higher binding affinity to the S. aureus-induced infection (Table 4). Rats with infectious lesions injected with 99mTc-clindamycin showed a good target-to-nontarget ratio, which are in accordance with the results obtained from the in vitro binding assay. Whole body images of infected rabbit at 1, 4, and 24 h after 99mTc-clindamycin administration are presented in Fig. 11a–c, respectively. S. aureus infection was induced in the rabbit’s left thigh, and the area was seen with increased tracer accumulation after injection of labeled clindamycin as shown in Fig. 12. The rapid uptake seen on images at 1, 4, and 24 h most likely is due to the physiologic changes at the site of infection.
Conclusion
Due to high labeling efficiency and high uptake in infected muscle, 99mTc-clindamycin may be an important radiotracer for the diagnosis of deep-seated infections. Radiochemical purity was monitored by ITLC and paper chromatography which was greater than 95 %. The 99mTc-clindamycin complex is quite stable, and labeling of ≥92 % was maintained for up to 24 h. No post-labeling purification was required. HPLC, lipophilicity test, in vitro binding in human serum and in vivo study by checking biodistribution, and scintigraphy of 99mTc-clindamycin were very appropriate, making it a potential infection imaging agent.
References
Ercan, M. T., Aras, T., & Unsal, I. S. (1992). Nuclear Medicine and Biology, 19, 803–806.
Gomes, B. V., Rabiller, G., Iglesias, F., Soroa, V., Tubau, F., Roca, M., & Martin-Comin, J. (2005). Revista Española de Medicina Nuclear, 24, 312–318.
Siaens, R. H., Rennen, H. J., Boerman, O. C., Dierckx, R., & Slegers, G. (2004). Journal of Nuclear Medicine, 45, 2088–2094.
Oh, S. J., Ryu, J. S., Shin, J. W., Yoon, E. J., Ha, H. J., Cheon, J. H., & Lee, H. K. (2002). Applied Radiation and Isotopes, 57, 193–200.
Sonmezoglu, K., Sonmezoglu, M., & Halac, M. (2001). Journal of Nuclear Medicine, 42, 567–574.
Larikka, M. J., Ahonen, A. K., & Niemela, O. (2002). Nuclear Medicine Communications, 23, 167–170.
Sarda, L., Crémieux, A. C., & Lebellec, Y. (2003). Journal of Nuclear Medicine, 44, 920–926.
Appelboom, T., Emery, P., Tant, L., Dumarey, N., & Schoutens, A. (2003). Rheumatology, 42, 1179–1182.
Motaleb, M. A. (2007). Journal of Radioanalytical and Nuclear Chemistry, 272, 95–99.
El Ghany, E. A., El Kolaly, M. T., Amine, A. M., El Sayed, A. S., & Abdel-Gelil, F. (2005). Journal of Radioanalytical and Nuclear Chemistry, 266, 131–139.
Roohi, S., Mushtaq, A., Jehangir, M., & Salman, A. M. (2006). Journal of Radioanalytical and Nuclear Chemistry, 267, 561–566.
Verma, J., Singh, A. K., & Bhatnagar, A. (2005). World Journal of Nuclear Medicine, 4, 35–46.
Lupetti, A., Welling, M. M., Mazzi, U., Nibbering, P. H., & Pauwels, E. K. (2002). European Journal of Nuclear Medicine, 29, 674–679.
Roohi, S., Mushtaq, A., & Salman, A. M. (2005). Radiochimica Acta, 93, 415–418.
Bhatnagar, A., Singh, A. K., Singh, T., & Shankar, L. R. (1995). Nuclear Medicine Communications, 16, 1058.
Degirmenci, B., Kilini, O., Cirak, K. A., Capa, G., & Akpinar, O. (1996). Journal of Nuclear Medicine, 37, 233.
Lumbrecht, F. Y., Yilmaz, O., Unak, P., Seytigolu, B., Durkan, K., & Baskan, H. (2008). Journal of Radioanalytical and Nuclear Chemistry, 277, 491–494.
El Ghany, E. A., El Kolaly, M. T., Amine, A. M., El Sayed, A. S., & Abdel-Gelil, F. (2005). Journal of Radioanalytical and Nuclear Chemistry, 266, 125–130.
Hal, A. V., Solanki, K. K., Vinjamuri, S., Britton, K. E., & Das, S. S. (1998). Journal of Clinical Pathology, 51, 215–219.
Seyedeh, F. M., Mostafa, E., Seyed, E., Mohammad, H. T., & Farhad, H. H. (2010). Iranian Journal of Nuclear Medicine, 18, 45–5121.
Britton, K. E., Vinjamuri, S., Hall, A. V., Solanki, K., Siraj, Q. H., & Bomanji, J. (1997). European Journal Nuclear Medicine, 24, 553–556.
Ugur, S. Y., Fatma, Y. L., Perihan, Ü., Fazilet, Z. B., Emin, I. M., & Berkan, C. (2006). Preparation of 99mTc labeled vitamin C (ascorbic acid) and biodistribution in rats. Chemical and Pharmaceutical Bulletin, 54, 1–3.
Laken, V., Boerman, C. J., Oyen, O. C., van de Ven, W. J. G., Meer, J. W. M., & Corstens, F. H. M. (2000). Journal of Nuclear Medicine, 41, 463–469.
Oyen, W. J. G., Boerman, O. C., & Corstens, F. H. M. (2001). Journal of Microbiological Methods, 47, 151–157.
Asikoglu, M., Yurt, F., Cagliyan, O., Unak, P., & Ozkilic, H. (2000). Applied Radiations and Isotopes, 53, 411–413.
Winter, D. F., Van, D., Dumont, F., Van, J., Solanki, K., Britton, K., Slegers, G., Dierckx, R. A., & Thierens, H. (2001). European Journal Nuclear Medicine, 28, 570–574.
Das, S. S., & Britton, K. E. (2003). World Journal of Nuclear Medicine, 2, 173–179.
Chattopadhyay, S., Ghosh, M., Sett, S., Das, M. K., Chandra, S., Kakali, D., Mishra, M., Sinha, S., Sarkar, B. R., & Ganguly, S. (2012). Applied Radiation and Isotopes, 70, 2384–2387.
Ibrahim, T., El-Tawoosy, M., & Talat, H. M. (2011). International Scholarly Research Network Pharmaceutica, 5, 42.
Kleisner, I., Komarek, P., Komarkova, I., & Konopokova, M. (2002). Nuklearmedizin, 22, 441.
Rien, H. S., Huub, J. R., Otto, C. B., Rudid, D., & Guido, S. (2004). Journal of Nuclear Medicine, 45, 2088.
Imen, E., Wafa, G., Nadia, M. S., & Mouldi, S. (2010). Journal of Nuclear Medicine and Biology, 37, 821–829.
Meral, T., Erean, T., & Isil, S. U. (1992). Journal of Nuclear Medicine and Biology, 19, 802–806.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hina, S., Rajoka, M.I., Roohi, S. et al. Preparation, Biodistribution, and Scintigraphic Evaluation of 99mTc-Clindamycin: an Infection Imaging Agent. Appl Biochem Biotechnol 174, 1420–1433 (2014). https://doi.org/10.1007/s12010-014-1075-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12010-014-1075-z