Abstract
Background
Surgical treatment of knee dislocations is intended to correct the anatomic injury and restore knee stability and patient function. Several studies have shown successful results with surgical treatment of knee dislocations with up to 10 years of followup, but longer-term studies are uncommon.
Questions/purposes
We evaluated patients treated surgically for knee dislocations at 10-year followup to assess (1) knee stability; (2) return to preinjury level of function; (3) development of arthrosis; and (4) range of motion (ROM) loss.
Methods
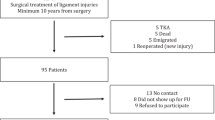
This study was a retrospective review of 127 combined PCL, ACL, and medial and/or lateral side reconstructions performed by a single surgeon (GCF) between 1990 and 2008. Of these, 44 were available for clinical and functional evaluation (35%) at a minimum 5-year followup. Inclusion criteria were combined PCL/ACL plus medial and/or lateral side reconstruction. Evaluation methods included arthrometer measurements, stress radiography, knee ligament rating and activity scales (Lysholm and Tegner), plain radiographs with osteoarthritic assessment, and physical examination.
Results
Of the 44 patients, there were nine ACL/PCL medial, 22 ACL/PCL lateral, and 13 ACL/PCL mediolateral reconstructions. Followup was at a minimum of 5 years (mean, 10 years; range, 5–22 years). The mean age at the time of injury was 31 years with a range of 13 to 65 years. The mean arthrometer-measured side-to-side differences were as follows: PCL screen, 1.9 mm; corrected posterior, 2.4 mm; corrected anterior, 0.8 mm; and anterior displacement at 30° of knee flexion, 1.7 mm. Stress radiographic measurements at 90° of knee flexion revealed a mean side-to-side difference of 1.9 mm. Mean Lysholm, and Tegner scores were 84 of 100 and 4.1 of 9, respectively. Ninety-three percent (41 of 44) of patients returned to their preinjury level of activity or one Tegner grade lower. Ten of the 44 knees (23%) developed degenerative joint disease. The mean flexion loss was 12.5°, and flexion contractures were not seen in any of the patients.
Conclusions
We found that a high proportion of patients treated for these severe injuries achieved static and functional stability, allowing the return to physically demanding work and recreational activities, but that nearly one-fourth of them will develop arthritis at a mean of 10 years. We cannot extrapolate our results to an elite athlete population, but our results probably apply well to working class populations.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee dislocations are rare injuries [2], but the impact to the patient can be tremendous. Although patients may not fully return to their preinjury level of function, the surgical treatment of knee dislocations is intended to correct the anatomic injury and restore knee stability and patient function. There is now a general consensus that surgical treatment of these injuries provides better results than nonsurgical treatment [4, 10, 11, 13, 15–18, 21–26, 29, 30, 32]. Although some progress has been made, a review of the literature still contains numerous accounts of surgical techniques and small patient cohorts [26]. Furthermore, there is a paucity of data related to clinical and functional outcomes for the surgical treatment of knee dislocation injuries [19]. Few studies have shown successful results with up to 10 years of followup [1, 5, 9, 12, 27, 28]. Even fewer studies include a substantial numbers of patients whose followup is into the second decade and beyond [12]. Of these studies, there is no consensus for the optimal evaluation methods in long-term followup. This retrospective review provides clinical and function outcomes that focus the long-term evaluation of knee dislocation injuries on four major issues: (1) Was knee stability achieved? (2) What percentage of patients returned to their preinjury level of function? (3) What percentage of patients developed arthrosis? (4) Was there a clinically relevant range of motion (ROM) loss after knee dislocation and surgical reconstruction?
Patients and Methods
Patient Cohort
This was a retrospective study of the long-term functional and clinical outcomes for surgically treated knee dislocations. Between 1990 and 2008, 176 total combined PCL, ACL, medial and/or lateral side reconstructions were performed by a single surgeon (GCF). Of these 127 patients, 44 were available for clinical and functional evaluation (35%). Minimum followup was 5 years (mean, 10 years; range, 5–22 years). All 44 patients (44 knees) had complete data sets for each of the four outcome categories: knee stability, return to level of function, development of arthrosis, and ROM loss.
The largest subset of these patients had ACL/PCL plus lateral side injuries (22 knees [50%]); the other patterns were ACL/PCL/medial (nine knees [20%]), and ACL/PCL medial/lateral (global laxity; 13 knees [30%]). Acute was defined as surgery less than 6 weeks postinjury, and chronic was defined as surgery greater than 6 weeks postinjury. Ten knees were acute (23%) and 34 knees were chronic (78%). The mean patient age at the time of surgery was 31 years (range, 13–65 years). There were 17 right knees (39%) and 27 left knees (61%). Patient occupations included 31 who were engaged in manual labor (70%), 11 whose occupations were more sedentary (25%), and two professional athletes (5%, one patient each who raced bicycle motocross and motocross). Mechanisms of injury included 26 motor vehicle-related (59%), nine sports injuries (20%), six industrial/farming (14%), and three pedestrian versus automobile accidents (7%).
Treatment Protocol
The same surgical techniques were used in all patients. The surgical techniques included an arthroscopically assisted transtibial tunnel PCL reconstruction using an Achilles tendon allograft for the anterolateral bundle and a tibialis anterior allograft for the posteromedial bundle when applicable. The ACL reconstruction was an arthroscopic transtibial femoral tunnel technique using an Achilles tendon allograft. Posterolateral reconstruction was performed using a fibular head-based reconstruction combined with a primary repair or posterolateral shift procedure. Posteromedial surgery consisted of primary repair plus allograft reconstruction, posteromedial capsular shift, or posteromedial capsular shift combined with allograft reconstruction [6, 7 ]. Tunnels were positioned so the grafts approximated the anatomic insertion sites of the ligaments being reconstructed. Surgical techniques for ACL, PCL, medial and lateral-sided reconstruction have been described previously by the senior author (GCF) [7].
The same postoperative rehabilitation program was used in all patients. Postoperative treatment included immobilization in extension and nonweightbearing with crutches for the first 5 postoperative weeks. This was followed by progressive weightbearing, ROM, strength, and proprioceptive skills training. Return to sports, heavy labor, and unrestricted activity occurred between 9 and 12 months postsurgery in a functional brace when strength, ROM, and proprioceptive skills were achieved. Functional bracing was discontinued after postoperative month number 18.
Knee Stability
Three major parameters were used to evaluate stability: KT1000™ arthrometer (MEDmetric Corp, San Diego, CA, USA) measurements, stress radiography using a Telos Stress Device (Austin & Associates, Inc, Baltimore, MD, USA), and physical examination. The techniques of KT1000™ measurements and stress radiography measurements have been described elsewhere [3]. Static stability end points using the KT1000™ and stress radiography were defined as 5 mm or less side-to-side difference comparing the surgical knee with the uninvolved, normal knee. Stress radiographic measurements were taken at 90° of knee flexion. KT1000™, stress radiographs, knee ligament rating scales, and physical examinations were performed by an independent examiner who was not the operating surgeon.
Return to Preinjury Level of Function
Two subjective outcome scores assessed the return of preinjury level of activity and the patient’s overall knee function: the Tegner activity scale [31] and the Lysholm scoring scale, respectively [20]. Use of the Lysholm and Tegner scales has been applied previously to the long-term assessment of the patient with knee dislocation [1, 5, 12, 27, 28].
Development of Arthrosis
Arthritis was assessed by AP and lateral nonweightbearing radiographs that were read by a radiologist. Arthritis was rated as either present or absent based on joint space narrowing and/or the presence of osteophytes. This methodology is similar to that used in the Kellgren and Lawerence (KL) grading system [14]. Patients without evidence of osteoarthritis would be considered KL Grade 0 to 1, whereas patients with radiographic evidence of osteoarthritis would be considered KL Grade 2 to 4.
Range of Motion Loss
ROM was assessed at clinical followup by the surgical team. A goniometer was used in all assessments.
Results
Knee Stability
Using the primary endpoints described in the methods, many of the patients achieved static stability. Five millimeters or less side-to-side difference comparing the surgical knee with the uninvolved normal knee was used for both KT1000™ and stress radiography assessment. Furthermore, 84% (37 of 44) of patients had a 0 to 5 mm side-to-side difference on static stability measurements.
The mean KT1000™ arthrometer side-to-side differences were as follows: PCL screen, 1.9 mm (range, 0–6 mm); corrected posterior, 2.4 mm (range, 0–6 mm); corrected anterior, 0.8 mm (range, −3 to 7 mm); and anterior displacement at 30° of knee flexion, 1.7 mm (range, −6 to 6 mm). The combined mean side-to-side difference measurement for all parameters was 1.7 mm.
Stress radiographic measurements at 90° of knee flexion with a posterior displacement force applied to the proximal tibia to evaluate the PCL reconstruction revealed a mean side-to-side difference of 1.9 mm (range, −8.6 to 12.7 mm). Eighty-four percent (37 of 44) of knees had side-to-side differences in the range of 0 to 5 mm.
Static stability was assessed by symmetrical physical examination of the involved surgical knee compared with the uninvolved normal knee. Functional stability was determined by the patient’s ability to return to his or her preinjury level of function.
Postreconstruction physical examination for the PCL revealed that 43 of 44 knees (98%) had symmetrical or less than Grade 1 posterior drawer. After ACL reconstruction, 39 knees (87%) had symmetrical Lachman test and 40 knees (91%) had symmetrical (negative) pivot shift. Symmetrical varus was present in 41 knees (93%), and symmetrical valgus was present in 43 knees (98%). Axial rotation was symmetrical to the normal knee in 38 knees (86%) and tighter than the normal knee in six (14%).
Return to Preinjury Level of Function
Sixty-six percent of patients (29 of 44) returned to their preinjury level of activity, and 93% (41 of 44) returned to their preinjury level of activity or one Tegner grade lower level of function. Mean Tegner score was 4.1 of 9 (range, 0–6). Mean Lysholm knee ligament score was 84 of 100 (range, 44–88).
Development of Arthrosis
Ten of the 44 knees (23%) developed radiographic evidence of degenerative joint disease. Three of the 44 patients (7%) underwent subsequent total knee arthroplasty (TKA).
Range of Motion Loss
There was no loss of terminal extension in any of the knees (no flexion contractures); however, the mean flexion loss was 12.5° (range, 0°–43°) compared with the normal contralateral knee.
Discussion
Clinical data on knee dislocations are sparse in the literature [19]. Furthermore, most studies are small retrospective cohorts that contain considerable variability in terms of surgical treatment, injury patterns, and mechanism of injury [26]. A review of the literature for long-term outcomes returned only five peer-reviewed articles documenting average outcomes greater than 5 years postoperatively [1, 5, 12, 27, 28]. With few studies focused on long-term followup, it was the purpose of this study to characterize the long-term recovery of the surgically treated patient with knee dislocation by focusing on four key issues: knee stability, return to preinjury level of function, development of radiographic signs of arthrosis, and ROM loss.
This study had a number of limitations, which include followup rate, how ROM was measured, how arthritis was assessed, and the heterogeneity of the patient population. Loss to followup may be the most important limitation. Our followup rate was 35% (44 of 126), which is low. The results presented in this article with respect to stability, return to function, development of arthritis, and motion loss should therefore be considered a best-case scenario. Patients lost to followup may or may not be doing as well as those who attend followup. Measurement of ROM is associated with some imprecision, and likewise the categorization of arthritis as either present or absent is a relatively crude metric. However, our finding that 7% of the patients (three of 44) had already undergone TKA certainly is a reasonably firm endpoint. As previously noted, because of loss to followup, our results probably underestimate the actual proportion of patients who have undergone TKA. The heterogeneity of our patient population is also a limitation of this study. The majority of patients are high-energy trauma victims who are working class people, not elite athletes. We therefore cannot extrapolate our results to an elite athlete population; however, our results may be very helpful in physicians caring for a working class population. Also, we have a mix of acute and chronic patients in this group. Despite the added heterogeneity, other studies have shown that there is no difference in outcomes between acute and chronic injury patterns both objectively and subjectively [8, 9]. We also have a mix of double-bundle and single-bundle PCL reconstructions, but likewise we have shown that there is no difference in outcomes between single- and double-bundle PCL reconstructions with respect to static and functional stability [8].
Knee Stability
The results of the stability assessment were excellent. KT1000™ and stress radiographic analysis showed the large majority of patients achieved clinically significant stability, less than 5-mm side-to-side differences, and absolute anterior or posterior values translation less than 5 mm. There are a variety of stability measures reported in the literature; however, KT1000™ arthrometry is standardized and commonly used in the evaluation of knee dislocations. KT1000™ was used assess stability in four of the five long-term case series of which we are aware (Table 1). Our results were comparable to other long-term studies with the exception of Hirschmann et al. [12]. This cohort of 68 knee dislocations documented clinical stability in nearly 99% of their patients. However, 20% of their patients were not able to achieve full extension.
Because the great majority of surgically treated patients achieved clinical stability, there are a few implications for the management of knee dislocations. Surgical technique and postoperative rehabilitation protocols described in this study were adequate to achieve objective stability in the long term. Therefore, further advances in treatment protocols should focus on improving other outcomes such as the development of osteoarthritis without sacrificing stability. Richter et al. [28] documented a significant correlation between osteoarthritic change and the level of knee stability. Our study as well as that of Hirschmann et al. [12] noted higher levels of stability and lower levels of osteoarthritis compared with the other long-term series (Table 1). However, even high levels of stability do not prevent the development of arthritis; nearly one-fourth of our patients developed degenerative joint disease; moreover, with a majority of our patients lost to followup, the proportion of patients observed with arthritis in our series almost certainly is higher than estimated by our results.
Return to Preinjury Level of Function
Postoperatively, many of our patients were able to achieve preinjury levels of activity as well as “good” overall knee function. Half of the patients reach a Lysholm score > 84, a commonly used threshold for “good” results [20]. In addition, our results are in line with function outcomes from other long-term studies (Table 1). One study reported lower Lysholm scores in their cohort, a mean of 75 [28]. However, this study included both patients treated operatively and nonoperatively. Although most patients are able to achieve knee stability, recovery is never complete. Pain is one confounding variables that can explain near, but not complete, recovery after knee dislocation. Development of painful osteoarthritis would limit both return to activity and reduce Lysholm outcome scores. Richter et al. [28] showed a significant correlation between osteoarthritic changes and both Lysholm as well as Tegner outcome scores.
Development of Arthrosis
Osteoarthritis continues to be a limitation in the recovery after knee dislocation injuries. Over 20% of our patients were diagnosed with radiographic signs of arthrosis in this study, and three patients subsequently underwent TKA. In comparison with other studies, our results were mild. Engebretsen et al. [5] and Richter et al. [28] presented over 80% of their knee dislocation patients with significant radiographic arthritis (Table 1). It should be noted that each of these studies used different classification systems for evaluating arthritic changes; however, all classification systems for evaluating osteoarthritis of the knee are based on similar radiographic findings. Although advances in surgical management and rehabilitation have provided excellent results for knee stability and ROM, many of the patients with knee dislocation will still develop arthritis.
Range of Motion Loss
Most patients achieved a functional ROM (0º–120º) with minimal loss of flexion. These results were comparable to other long-term studies. Our group did, however, have fewer flexion contractures (Table 1). Three studies reported over 15% of their patients with an extension deficit greater than 5° [1, 12, 28]. Bin and Nam [1] casted the leg in 40° of flexion for the first 3 to 4 weeks postoperatively. Hirschmann et al. [12] used a splint for up to 6 weeks postoperatively with 10° of extension deficit. In comparison, our rehabilitation protocol maintained patients in full extension for 5 weeks postoperatively. There are additional differences in patient demographics, patterns of injury, incidence of concomitant injuries, and surgical treatment that may account for these extension deficits. However, it is beyond the scope of this article to speculate.
In summary, we found that a high proportion of patients treated for these severe injuries achieved static and functional stability, allowing the return to physically demanding work and recreational activities. However, nearly one-fourth of surgically treated patients with knee dislocation will develop arthritis at a mean of 10 years. Some loss of ROM in terminal flexion will most likely occur; however, this does not appear to limit knee function or level of activity. We cannot extrapolate our results to an elite athlete population, but these findings may apply well to working class populations.
References
Bin SI, Nam TS. Surgical Outcome of 2-Stage management of multiple knee ligament injuries after knee dislocation. Arthroscopy. 2007;23:1066–1072.
Brautigan B, Johnson DL. The epidemiology of knee dislocation. Clin Sport Med. 2000;19:387–397.
Daniel DM, Akeson W, O’Conner J, eds. Knee Ligaments: Structure, Function, Injury, and Repair. New York, NY, USA: Raven; 1990:421–447.
Dwyer T, Marx RG, Whelan D. Outcomes of treatment of multiple ligament knee injuries. J Knee Surg. 2012;25:317–326.
Engebretsen L, Risberg MA, Robertson B, Ludvigsen TC, Johansen S. Outcome after knee dislocation: a 2 to 9 year followup of 85 consecutive patients. Knee Surg Sports Traumatol Arthrosc. 2009;17:1013–1026.
Fanelli GC. Surgical treatment of lateral posterolateral instability of the knee using biceps femoris tendon procedures. Sports Med Arthrosc Rev. 2006;14:37–43.
Fanelli GC. Surgical treatment of combined PCL ACL medial and lateral side injuries (global laxity): acute and chronic. In: Fanelli GC, ed. The Multiple Ligament Injured Knee. A Practical Guide to Management. 2nd ed. New York, NY, USA: Springer-Verlag; 2013:281–301.
Fanelli GC, Beck JD, Edson CJ. Single compared to double bundle PCL reconstruction using allograft tissue. J Knee Surg. 2012;25:59–64.
Fanelli GC, Edson CJ. Arthroscopically assisted combined ACL/PCL reconstruction: 2–10 year followup. Arthroscopy. 2002;18:703–714.
Fanelli GC, Stannard JP, Stuart MJ, MacDonald PB, Marx RG, Whelan DB, Boyd JL, Levy BA. Management of complex knee ligament injuries. J Bone Joint Surg Am. 2010;92:2235–2246.
Fanelli GC, Stannard JP, Stuart MJ, MacDonald PB, Marx RG, Whelan DB, Boyd JL, Levy BA. Management of complex knee ligament injuries. Instr Course Lect. 2011;60:523–535.
Hirschmann MT, Zimmermann N, Rychen T, Candrian C, Hudetz D, Lorez LG, Amsler F, Muller W, Friederich NF. Clinical and radiological outcomes after management of traumatic knee dislocation by open single stage complete reconstruction repair. BMC Musculoskelet Dis. 2010;11:102.
Ibrahim SA. Primary repair of the cruciate and collateral ligaments after traumatic dislocation of the knee. J Bone Joint Surg Br. 1999;81:987–990.
Kellgren JH, Lawerence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502.
Kennedy JC. Complete dislocation of the knee joint. J Bone Joint Surg Am. 1963;45:889–904.
Kremchek TE, Welling RE, Kremchek EJ. Traumatic dislocation of the knee. Orthop Rev. 1989;18:1051–1057.
Levy B, Dajani KA, Whalen DB, Stannard JP, Fanelli GC, Stuart MJ, Boyd JL, MacDonald PA, Marx RG. Decision making in the multiple ligament injured knee: an evidence based systematic review. Arthroscopy. 2009;25:430–438.
Levy B, Fanelli GC, Whalen D, Stannard J, MacDonald P, Boyd J, Marx R, Stuart M. Modern perspectives for the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg. 2009;17:197–206.
Levy BA, Marx RG. Outcome after knee dislocation. Knee Surg Sports Traumatol Arthrosc. 2009;17:1011–1012.
Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–154.
Meyers MH, Harvey JP. Traumatic dislocation of the knee joint: a study of eighteen cases. J Bone Joint Surg Am. 1971;53:16–29.
Meyers MH, Moore TM, Harvey JP. Followup notes on articles previously published in the journal: traumatic dislocation of the knee joint. J Bone Joint Surg Am. 1975;57:430–433.
Montgomery JB. Dislocation of the knee. Orthop Clin North Am. 1987;18:149–156.
O’Donoghue DH. An analysis of end results of surgical treatment of major injuries to the ligaments of the knee. J Bone Joint Surg Am. 1955;37:1–13.
Peskun CJ, Levy BA, Fanelli GC, Stannard JP, Stuart MJ, MacDonald PB, Marx RG, Boyd JL, Whelan DB. Diagnosis and management of knee dislocations. Phys Sports Med. 2010;38:101–111.
Peskun CJ, Whelan DB. Outcomes of operative and nonoperative treatment of multiligament knee injuries: an evidence based review. Sports Med Arthrosc Rev. 2011;19:167–173.
Plancher KD, Siliski J. Long-term functional results and complications in patient with knee dislocation. J Knee Surg. 2008;21:261–268.
Richter M, Bosch U, Wippermann B, Hofmann A, Krettek C. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med. 2002;30:718–727.
Roman PD, Hopson CN, Zenni EJ. Traumatic dislocation of the knee: a report of thirty cases and literature review. Orthop Rev. 1987;16:917–924.
Sisto DJ, Warren RF. Complete knee dislocation: a followup study of operative treatment. Clin Orthop Relat Res. 1985;198:94–101.
Tegner Y, Lysholm J. Rating system in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49.
Walker DN, Hardison RR, Schenck RC. A baker’s dozen of knee dislocations. Am J Knee Surg. 1994;7:117–124.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Fanelli, G.C., Sousa, P.L. & Edson, C.J. Long-term Followup of Surgically Treated Knee Dislocations: Stability Restored, but Arthritis Is Common. Clin Orthop Relat Res 472, 2712–2717 (2014). https://doi.org/10.1007/s11999-014-3707-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3707-6



