Abstract
Introduction
At present, limited knowledge regarding clinical, functional, and patient-reported outcomes at mid- and long-terms after surgical treatment of traumatic knee dislocations is available. This study aimed to investigate the mid-term recovery regarding clinical, functional, and patient-reported outcomes in patients following knee dislocation with associated multi-ligament injuries.
Materials and methods
The study design was a cross-sectional cohort study. Data were collected by retrospective chart review, clinical examination, and interview of patients. All patients treated surgically following a knee dislocation between January 2000 and December 2011 were included. The surgical technique was up to the decision of the individual surgeon. The main outcome was the Lysholm knee score. Secondary outcomes consist of clinical knee examination, functional performance test, pain, and patient-reported outcome across several domains in function, sport, pain, and quality of life.
Results
Seventy-five patients (66.3%) accepted the invitation to participate. The mean age at the time of knee dislocation was 33.5 years, with a range of 16–65 years of age. The mean follow-up time was 78 months (R: 17–147). 75% of patient a Schenck’s type 1 lesion and 23% a type 3. The median Lysholm knee score was 83 (R: 18–100). The mean KOOS for the five subscales were pain 84.5 (95% CI 80.5–88.5), symptoms 75.1 (95% CI 70.7–79.4), ADL 87.0 (95% CI 83.1–90.9), sport 59.9 (95% CI 53.3–66.4), and QOL 71.3 (95% CI 67.0–75.6). The mean Tegner activity level was 5.1 (95% CI 4.5–5.7). The median single assessment numeric evaluation (SANE) was 93 (R: 0–100). The pain intensity score for pain (VAS) during activity was reported with a mean of 2.7 (95% CI 2.1–3.3). The objective IKDC examination showed 76% of patients grouped by Grade A (normal knee function) or Grade B (nearly normal).
Conclusion
With a mean follow-up of 6.5 years, combined repair and reconstruction surgery following a knee dislocation shows good to excellent patient-reported outcome and more than 75% of patients experiencing normal knee functioned evaluated by the IKDC score.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic dislocation of the knee joint is an uncommon injury representing about 0.02% of all orthopaedic injuries [1]. The true frequency of traumatic knee dislocation is difficult to clarify as spontaneous knee joint reduction occurs in most cases [2]. A traumatic knee dislocation is commonly a consequence of traffic accidents but can also be caused by sport or work-related injuries and by minor trauma in obese patients [3].
Traumatic knee dislocation is a severe injury to the knee joint with multi-ligament lesions and associated injuries to soft tissues intraarticular and extraarticular to the knee joint [4]. The severity of traumatic knee dislocations has been reported in several studies [4,5,6]. The prevalence of peroneal nerve injury is reported to be 25–40% [6, 7]; vascular injuries are reported with a risk of 18% [7], and the rate of amputation following knee dislocation has been reported to be around 10% [5, 7].
The management of traumatic knee dislocation is challenging and widely discussed [2, 8, 9]. Multiple surgical techniques and protocols have been described; however, with advancements in arthroscopic techniques in recent decades, operative reconstruction has become more favourable. Furthermore, increasing evidence favours operative management over conservative treatment across several clinical and functional domains [9, 10].
The outcome of patients with traumatic knee dislocation has been investigated in few studies, in which most studies include a low number of patients and high variability between study methods and patient characteristics [11]. At present, limited knowledge regarding clinical, functional, and patient-reported outcomes at mid- and long-terms after surgical treatment of traumatic knee dislocations is available [8, 11,12,13,14,15,16].
This study aimed to investigate the mid-term recovery regarding clinical, functional, and patient-reported outcomes in patients following knee dislocation with associated multi-ligament injuries. Secondarily, the aim was to compare outcomes between patients treated surgically prior to or after 14 days of injury.
Materials and methods
This study was designed as a cross-sectional cohort study. Data were collected by retrospective chart review, clinical examination, and interview of patients.
The main outcome was predefined as the patient-reported Lysholm knee score [17].
Secondary outcomes consist of clinical knee examination, functional performance test, pain, and patient-reported outcome across several domains in function, sport, pain, and quality of life.
The study group was divided into 2 groups. The early group was defined as surgery prior to or on the 14th day following injury and the late group as patients treated after 14 days.
Recruitment of patients
All patients who were treated surgically following a knee dislocation with multi-ligament reconstruction at Capio Artro Clinic, Stockholm, Sweden, between 1 January 2000 and 31 December 2011 were identified.
Included were patients with multi-ligament injuries following X-ray verified knee dislocation defined as 2 or more ligaments of the knee injured including either ACL, PCL, MCL, LCL, or PLC. Conservatively treated patients were excluded. Patients treated with a tibial osteotomy and total knee replacement (TKR) before the time of follow-up were excluded. Patients younger than 18 years of age at the time of follow-up were also excluded.
The patients were contacted by mail and invited to participate. If the patient did not reply, a second request was sent by mail or telephone call. Written consent was obtained from all the included patients.
The Swedish Data Protection Agency and the Committee for Science Ethics of Sweden approved the study, which was performed according to the principles of the Declaration of Helsinki. The reporting of the study complies with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [18].
Surgical treatment
Surgical treatment was based on the preoperative clinical examination, X-rays/MRI, examination under anaesthesia, and arthroscopic findings. Conservative or surgical treatment and time of surgery was decided by the surgeon and patient on an individual basis. The surgical technique was up to the decision of the individual surgeon. A total of 4 senior surgeon performed the procedures.
The patient was positioned supine on the operating table. Tourniquet was used rarely. A lateral post was positioned near the level of the tourniquet, and a bump was placed distally so that when the foot was placed on it, the knee was flexed to ninety degrees.
The cruciate ligaments were always reconstructed arthroscopically, and a posterior-medial portal was used in the case of PCL reconstruction. A lateral or a medial approach was used to expose the anatomic structures of the lateral or the medial side, respectively. An oblique or longitudinal incision over the Pes Anserine was performed to harvest hamstring tendon. The quadriceps tendon and the patella tendon were harvested by a midline longitudinal approach. Contralateral auto-grafts were used based on surgeons’ preferences.
The cruciate ligaments
Acute bony avulsed cruciate ligaments were anatomically repaired using smart nails or sutures. ACL tears were reconstructed. Only auto-grafts were used. In case of injury to only one of the cruciate ligaments, the hamstrings tendon was used while for simultaneous rupture of both cruciate ligaments, bone-patellar tendon-bone (BPTB) autograft was used for ACL, and PCL was reconstructed with either hamstrings or quadriceps tendon.
Femoral fixation: for the PCL fixation, the hamstring/quadriceps graft was fixed in the femoral tunnel with Endobutton (Smith & Nephew)/RCI screw (Smith & Nephew), respectively. For fixation of the ACL BPTB graft in the femoral tunnel, a standard interference screw (Soft Silk, Smith, & Nephew) was used, and Endobutton (Smith & Nephew) was used if hamstrings were used. Fixation of the ACL and PCL grafts in their respective tibial tunnels was delayed until the repair of any medial or lateral injuries was complete. Tibial fixation: first, the PCL was fixed with the knee joint at approximately 90° of flexion. The normal tibia step off was restored by comparing to the non-injured knee, in neutral rotation with an interference screw (RCI, Smith & Nephew) if quadriceps was used, and with biocortical screw with a washer if hamstring was used providing suspensory fixation. The ACL was fixed with a biocortical screw with a washer on the tibia with the knee close to full extension after 20 flexion–extension movements had been carried out.
The medial structures
The repair of the medial ligament structures was performed in layers and with anatomical precision. The surgical procedure started from the menisco-femoral and menisco-tibial ligaments and continued to the more superficial layers. The ruptures or avulsions of the capsule and the posteromedial anatomical structures (posterior oblique ligament, semimembranosus) were repaired using sutures or anchors, while the mid-substance tears of the MCL were sutured using non-absorbable sutures. The sequence of the surgery was to reconstruct the cruciate ligaments first and then repair the MCL.
The lateral structures
Repair of acute injuries of the lateral side was attempted if possible. Lesions of the postero-lateral capsule and ligament structures were primarily sutured or reattached using suture anchors. Mid-substance tears of the LCL were treated by suturing the ligament and augmentation using gracilis tendon. Reattachment of the ligament abruptions from the fibular head was also performed with anchors or sutures through transosseous drill holes. Reconstruction of the popliteus tendon was performed in acute mid-substance tears or in chronic cases. For its reconstruction, the Larson technique was used in some and the LaPrade technique in others, depending on the treating surgeon. (RCI, Smith & Nephew) was used when fixating the graft.
Combined injuries to ACL, PCL, and Postero Lateral Corner (PLC), surgery began with the reconstruction of the ACL and PCL. Following fixation of the femoral side, attention was turned towards the lateral sided injuries.
Other lesions
The peripheral meniscal tears in the red–red zone were sutured. Other types of meniscal tears or tears in chronic cases were either conservatively treated or treated by partial meniscectomy. Articular cartilage lesions were treated by debridement. Patella tendon avulsions from the tuberosity were reattached using wire and/or large PDS sutures. Mid-substance ruptures of the tendon were sutured.
Postoperative regime and rehabilitation
In cases with PLC/PCl: immediately postoperatively, patients were placed into a knee brace, locked in full extension. During their hospital stay, passive motion was obtained with passive extension in a prone position without a brace. Passive knee flexion was not performed in the first 2 weeks. The patients were kept in an Albrecht PCL-Jack brace for 12 weeks to allow the PCL to begin healing without being stretched. The brace was locked the first 2 weeks, 0–30° during weeks three and four, 0–60° during weeks five and six, and 0–90° during the rest of the time. After 8 weeks, the patient was allowed strength training without the brace, observed by the physical therapist. During the first 6 weeks, patients were allowed partial weight-bearing with the assistance of crutches. Patients also performed isometric quadriceps exercises, straight leg raise exercises from the beginning, and more dynamic exercises when the range of motion in the knee increased. No change in the regime was suggested regardless of the presence of meniscus repair.
The patients progressed from partial weight-bearing to full weight-bearing, and strengthening exercises for quadriceps, hamstrings, and calf muscles were introduced. At 12 weeks, the brace was discontinued, and full active range of motion exercises was continued. Patients were allowed to return to full activity when they achieved a minimum of 90% quadriceps muscle strength compared to the uninjured limb and full knee range of motion, usually occurring between 9 and 12 months after surgery.
In cases where no PLC/PCL injury while only MCL and ACL were injured, a postoperative knee brace was used locked in 0–30 in the first 2 weeks, followed by 0–60 in the next 2 weeks, and 0–90 from week 4 to 6. Full weight-bearing was allowed, and strengthening exercises were introduced for the quadriceps and hamstrings muscles.
Follow-up procedure
Baseline characteristics
Patient charts were retrospectively reviewed to obtain baseline characteristics. Age, sex, date of injury, side of injury, mode of injury, type of injury, surgical procedures, treatment, and complications were obtained.
Schenck’s classification system was used to classify knee dislocation based on the pattern of multi-ligament injuries. Five subscales were used: I: ACL or PCL and MCL or LCL; II: ACL and PCL; III: ACL, PCL and either LCL or MCL; IV: ACL, PCL, LCL and MCL’ V: multi-ligament injury with a periarticular fracture [19].
Patient-reported outcomes
The Lysholm knee score is a patient-reported instrument developed to evaluate knee problems following knee injuries [17]. The Lysholm scale consists of eight items that measure pain, instability, locking, swelling, limp, stair climbing, squatting, and need for support. The total score is the sum of each response to the eight domains, and scores have a possible range from 0 to 100. Higher scores indicate a better outcome with fewer symptoms or less disability [17].Interpretations of the scores is considered: 95–100 point = excellent, 84–94 = good, 65–83 = fair, and 64 or less = poor.
The Knee Injury and Osteoarthritis Outcome Score (KOOS) [20] is a standardised and validated instrument to evaluate knee and associated knee problems. The questionnaire includes 5 subscales: pain, Activity of Daily Living (ADL), symptoms, sport, and quality of life (QOL). A total score of 100 indicates no symptoms, and 0 indicates major symptoms [21]. KOOS reference data from a general population-based sample in southern Sweden are published for 840 subjects [22].
The Tegner activity level is a patient-administered activity rating system for patients with various knee disorders [23]. The Tegner activity level is a one-item score that graded activity based on work and sports activities on a scale of 0 to 10. Zero represents serious disability due to knee problems, and 10 represents a national or international level in sport [23].
The Single Assessment Numeric Evaluation (SANE) is a patient rating from 0 to 100. Patients are asked to rate their current illness score (%) in relation to their pre-injury baseline [24].
The pain intensity at the injured knee at rest and in activity was measured on a 10 cm visual analogue scale (VAS) with the endpoints of ‘no pain’ and ‘maximal pain’.
Clinical examination
The IKDC objective examination form includes 7 domains (effusion, range of knee motion, ligament examination, compartment findings, harvest site pathology, X-rays, and functional test) 26]. Based on the clinical examination, patients were grouped as Grade A (normal knee function), B (nearly normal), C (abnormal), and D (severely abnormal) [25]. The objective examination was conducted by a specialised senior knee surgeon (SS).
The bilateral range of knee motion was measured with the standard goniometric technique with the patient in the supine position [26].
Tibial translation in the anterior direction was measured with the KT-1000 arthrometer (MED metric, San Diego, California) ensuring no residual posterior sag prior to measuring the translation. The difference in displacement between the two knees, expressed in millimetres, was used as a measurement of knee laxity [27].
Functional performance
One leg hop test: patients were asked to stand on one leg and jump as far forward as possible. This procedure was repeated three times for each leg. The longest distance of the three trials for each leg was used for analysis [28, 29].
Side hop test: patients were asked to stand on one leg and jump as many times as possible during a period of 30 s. from side to side between two parallel strips of tape, placed 40 cm apart on the floor. The number of successful jumps performed without touching the tape was recorded [28, 29].
Square hop test: patients were asked to stand on one leg outside a 40 × 40 cm square marked with tape on the floor and jump in and out of the square as many times as possible during a period of 30 s. The number of successful jumps performed without touching the tape was recorded [28, 29].
Functional performance was evaluated on both knees, and a percentage ratio was calculated to express the function of the operated knee.
Statistical analysis
All variables were summarised using standard descriptive statistics. Mean and 95% confidence intervals (CI)/standard deviation (SD) was used for normal distributed data. Median and range are reported for skewed data. Differences between legs in the functional performance were analysed with Student’s t test for dependent variables.
Differences between the time groups were analysed with Student’s t test and, if the distribution was severely skewed, the Mann–Whitney test for independent samples was used.
The significance level in all analyses was 0.05 (two-tailed). The statistical analysis was performed by SPSS for MAC (PASWStatistics 27.0).
Results
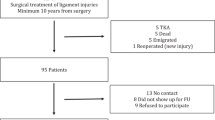
A total of 113 patients were admitted with a knee dislocation and treated with multi-ligament reconstruction during the study period. Of those, 38 patients were excluded due to the predefined exclusion criteria. Seventy-five patients (66.3%) accept the invitation to participate in this follow-up study. Fifty-five patients complete the full follow-up procedure at the hospital, and 20 patients participate solely by interview/questionnaire due to geographical conditions. The details of the recruitment process are shown in Fig. 1.
The mean age at the time of knee dislocation was 33.5 years, with a range of 16–65 years of age. Twenty-three (31%) patients were female, and 52 (69%) were males. The mean follow-up time was 78 months (R: 17–147). Baseline characteristics of all patients are presented in Table 1.
A total of 61 patients were treated with an acute repair of the medial or lateral side of the knee.
At time of follow-up, 2 patient had experienced revision surgery due to ligament stability of the knee joint, and 5 patients had developed arthrofibrosis.
Primary outcome (N = 75)
At the time of follow-up, the median Lysholm knee score was 83 (R: 18–100), indicating a high degree of function with the injured knee [17].
Secondary outcomes (N = 75)
The mean KOOS for the five subscales were pain 84.5 (95% CI 80.5–88.5), symptoms 75.1 (95% CI 70.7–79.4), ADL 87.0 (95% CI 83.1–90.9), sport 59.9 (95% CI 53.3–66.4), and QOL 71.3 (95% CI 67.0–75.6) (Fig. 2).
The mean Tegner activity level was 5.1 (95% CI 4.5–5.7), and the median Single Assessment Numeric Evaluation (SANE) was 93 (R: 0–100).
The pain intensity score for pain during activity (VAS) was reported with a mean of 2.7 (95% CI 2.1–3.3). The pain score for resting pain was reported with a mean of 1.1 (95% CI 0.6–1.5).
Clinical examination and functional performance (N = 55)
The objective IKDC examination is presented in Table 2, indicating a generally high degree of knee function, with 76% of patients grouped by Grade A (normal knee function) or Grade B (nearly normal).
The anterior/posterior translation difference between the injured and non-injured knee measured by KT-1000 was 3.4 mm (95% CI 2.4–4.4) (p < 0.001).
The range of motion examination showed comparable knee extension between the injured and non-injured knee. The examination of maximal knee flexion showed a mean of 6 degrees (95% CI 3.7–8.3) decrease/loss of flexion in the injured knee compared to the non-injured knee.
The tests of functional performance expressed as the ratio of knee function between the injured and non-injured knee (Limb Symmetry Index) (LSI)) were 95% one leg hop, 92% side hop, and 94% square test. (5 patients refused to participate, one because of hip pain and the rest because of surgery or injury in the contra-lateral knee). Eight patients who participated in the knee function test have conditions involving their contra-lateral knee. One has arthritis; one was operated on for ACL reconstruction and one for cartilage damage. The other five had diverse injuries.
Outcomes comparing early and late reconstruction surgery
The early group consisted of 37 patients and the late group of 38 patients. Comparing early (mean 9 days to surgery (R: 4–13 days)) and late knee surgery (mean 22 days to surgery (R: 14–184)) investigating the primary outcome, Lysholm score analyses showed no significant difference between the two groups (P = 0.26). Moreover, no significant difference in the patient-reported scores (KOOS, SANE, Tegner, pain) was observed (P < 0.49). The two groups’ functional assessment was also comparable (P < 0.26) (Fig. 2/Table 3).
Discussion
Key results
This retrospective cohort study assessed the results of 75 patients presenting with a traumatic knee dislocation with a follow-up between 2 and 10 years. The main findings are that 81% of patients showed ‘fair’ to ‘excellent’ patient-reported results, and the objective results of the knee function were examined ‘normal’ and ‘nearly normal’ in 76% of patients. The study’s findings suggest that with a mean follow-up of 6.5 years, combined repair and reconstruction surgery show satisfactory clinical and functional results, although some limitations in the knee function should be expected.
Primary outcome
The present study uses the Lysholm knee score as the main outcome to measure symptoms and function at mid-term follow-up in patients with traumatic knee dislocation. Results show ‘excellent’ to ‘fair’ results in 81% of patients. The Lysholm score was reported with a median of 83 points. Lysholm scores < 84 indicate knee problems in activities of daily living; 84 to 94 indicate problems during sporting activities, and ≥ 95 indicate no knee problems [30]. Comparable findings are reported by Fanelli et al. [31] using an arthroscopic assisted treatment protocol and reported a Lysholm score of 91 at mid-term follow-up. Furthermore, Fanelli et al. Hirschmann et al. [14], reporting on 68 patients with a mean follow-up of 12 years using an open single-stage procedure for surgical treatment, reported a Lysholm score of 83 which is slightly lower but still comparable. Other authors report similar results. However, comparison between studies is highly difficult due to differences in populations, sport activity, age, gender and treatment protocols, and a generally low number of available studies reporting on mid- to long-term follow-up [12, 15, 16, 32,33,34].
Patient-reported knee function and pain
This study reported a Tegner score of 5.1, indicating that patients following surgical treatment of a traumatic knee dislocation could participate in heavy labour work, cycling, cross-country skiing, recreational sports, and jogging on uneven ground at least twice weekly. Low pain scores in the study cohort supported these findings, both at resting (VAS 1.1) and at activity/sporting (VAS 2.7). The Single Assessment Numeric Evaluation (SANE) was 93, indicating that patients were very satisfied with the outcome of the surgical treatment. A high activity level, low pain scores, and a high degree of patient satisfaction align with previous studies reporting outcomes at mid- to long-term following surgical treatment of a traumatic knee dislocation [12, 15, 16, 32,33,34].
The KOOS score was included to evaluate knee-related pain, ADL, symptoms, sport, and QOL by a patient-reported questionary. The KOOS score was reported in the upper scale for all five subscales. The reported KOOS outcome of the present study is comparable with Ishibashi et al. [32] reporting on 31 patients with traumatic knee dislocation or multi-ligament knee injury at 5-year follow-up. Comparison of KOOS results with the established KOOS reference population of southern Sweden [22, 35], the study population showed statistically worse KOOS outcomes for the KOOS subgroups Symptoms, Sport, and QOL, due to non-overlapping 95% CI, indicating that some limitations in the knee function should be expected at mid-term following a traumatic knee dislocation. Moreover, this result indicates that KOOS may be more sensitive to subtle changes in the knee function and knee-related quality of life than the Lysholm score in patients with traumatic knee dislocations. However, more research is needed.
Objective knee function
The clinical examination of the knee function showed a ‘normal’ or ‘nearly normal’ objective IKDC score in 76% of patients, and only 2 patients demonstrated severely abnormal knee function. Several other studies reported comparable results, including some variability between studies, which may be due to a high difference in study populations [12, 15, 16, 32,33,34]. The anterior and posterior laxity measurements with the KT-1000 arthrometer demonstrated a high degree of static stability expressed by 3.4 mm (95% CI 2.4–4.4). Performance-based measures of knee function examined the dynamic stability of the knee joint. The ratio of knee function between the injured and non-injured knee was above 90%, indicating a high degree of dynamic knee stability at the mid-term follow-up. The examination of knee stability following multi-ligament reconstruction surgery has been reported in several studies. Results of the present study are in line with previous findings after surgical treatment of a traumatic knee dislocation [11, 14, 31, 34].
Timing of surgery
The initial decision regarding acute surgery following a traumatic knee dislocation is based on the vascular status of the injured leg, open injury, and the combination of ligament injuries [36]. The timing of surgery in patients presenting with multi-ligament injuries but injuries not requiring acute surgery is frequently discussed [9, 36]. This study explores outcomes of the patients in two groups divided by surgery prior to or after 14 days of the injury, and no significant difference in Lysholm, SANE, Tegner and pain scores were observed between the two groups. However, results should be interpreted with caution as the sample size was small, and analysis may lack power. Furthermore, the range in time to surgery in the late group treated after 14 days from injury was high (14–184 days). A metanalysis by Vicenti et al. [9] suggests that early treatment resulted in an increased Lysholm score and a higher percentage of excellent/good IKDC score, and a better range of motion. Existing literature currently lacks randomised clinical trials investigating acute vs late surgery for knee dislocation, including different subgroups of patients divided by injury patterns. Nevertheless, performing a high-quality randomised trial including an adequate sample size is difficult due to the low incidence of patients presenting with a knee dislocation.
Limitations
The main limitation to the present study is the retrospective, observational design and the low number of patients included, implying limited conclusions. Furthermore, the follow-up period with a mean of 6.5 years is a limitation. Furthermore 75% of patients were Schenck’s type 1, which implies a high number of less serious injuries. Long-term outcomes are needed to investigate the lifelong severity of a traumatic knee dislocation. Such information is rare in the literature but highly important as the majority of patients presenting with a knee dislocation are young. Moreover, the rehabilitation protocol of the present study was restrictive compared to other studies suggesting a more active rehabilitation protocol [8]. Another limitation to the present study is the lack of data investigating posttraumatic osteoarthritis. The risk of development of posttraumatic osteoarthritis following a knee dislocation is reported to increase about sixfold compared to an uninjured knee population at long-term follow-up [37].
A selection bias to the study may be present as 75 patients (66%) accepted the invitation to participate in this follow-up study. Fifty-five patients completed the entire follow-up procedure at the hospital, and 20 patients participated solely by interview/questionnaire.
Conclusion
With a mean follow-up of 6.5 years, combined repair and reconstruction surgery following a knee dislocation shows good to excellent patient-reported outcome and more than 75% of patients experiencing normal knee functioned evaluated by the IKDC score.
References
Levy BA, Dajani KA, Whelan DB et al (2009) Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthrosc J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 25:430–438. https://doi.org/10.1016/j.arthro.2009.01.008
Wascher DC, Dvirnak PC, DeCoster TA (1997) Knee dislocation: initial assessment and implications for treatment. J Orthop Trauma 11:525–529. https://doi.org/10.1097/00005131-199710000-00011
Brautigan B, Johnson DL (2000) The epidemiology of knee dislocations. Clin Sports Med 19:387–397. https://doi.org/10.1016/s0278-5919(05)70213-1
Kim SH, Park Y-B, Kim B-S et al (2021) Incidence of associated lesions of multiligament knee injuries: a systematic review and meta-analysis. Orthop J Sports Med 9:23259671211010410. https://doi.org/10.1177/23259671211010409
Stayner LR, Coen MJ (2000) Historic perspectives of treatment algorithms in knee dislocation. Clin Sports Med 19:399–413. https://doi.org/10.1016/s0278-5919(05)70214-3
Niall DM, Nutton RW, Keating JF (2005) Palsy of the common peroneal nerve after traumatic dislocation of the knee. J Bone Jt Surg Br 87:664–667. https://doi.org/10.1302/0301-620X.87B5.15607
Medina O, Arom GA, Yeranosian MG et al (2014) Vascular and nerve injury after knee dislocation: a systematic review. Clin Orthop Relat Res 472:2621–2629. https://doi.org/10.1007/s11999-014-3511-3
Frosch K-H, Preiss A, Heider S et al (2013) Primary ligament sutures as a treatment option of knee dislocations: a meta-analysis. Knee Surg, Sports Traumatol Arthrosc: Off J ESSKA 21:1502–1509. https://doi.org/10.1007/s00167-012-2154-8
Vicenti G, Solarino G, Carrozzo M et al (2019) Major concern in the multiligament-injured knee treatment: a systematic review. Injury 50:S89–S94. https://doi.org/10.1016/j.injury.2019.01.052
Peskun CJ, Whelan DB (2011) Outcomes of operative and nonoperative treatment of multiligament knee injuries: an evidence-based review. Sports Med Arthrosc Rev 19:167–173. https://doi.org/10.1097/JSA.0b013e3182107d5f
Fanelli GC, Sousa PL, Edson CJ (2014) Long-term followup of surgically treated knee dislocations: stability restored, but arthritis is common. Clin Orthop Relat Res 472:2712–2717. https://doi.org/10.1007/s11999-014-3707-6
Hirschmann MT, Iranpour F, Müller W, Friederich NF (2010) Surgical treatment of complex bicruciate knee ligament injuries in elite athletes. Am J Sports Med 38:1103–1109. https://doi.org/10.1177/0363546509356978
Eranki V, Begg C, Wallace B (2010) Outcomes of operatively treated acute knee dislocations. Open Orthop J 4:22–30. https://doi.org/10.2174/1874325001004010022
Hirschmann MT, Zimmermann N, Rychen T et al (2010) Clinical and radiological outcomes after management of traumatic knee dislocation by open single stage complete reconstruction/repair. BMC Musculoskelet Disord 11:102. https://doi.org/10.1186/1471-2474-11-102
Schenck RC, Richter DL, Wascher DC (2014) Knee dislocations. Orthop J Sports Med 2:232596711453438. https://doi.org/10.1177/2325967114534387
Harner CD, Waltrip RL, Bennett CH et al (2004) Surgical management of knee dislocations. J Bone Jt Surg Am 86:262–273. https://doi.org/10.2106/00004623-200402000-00008
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10:150–154. https://doi.org/10.1177/036354658201000306
von Elm E, Altman DG, Egger M et al (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg (London, England) 12:1495–1499. https://doi.org/10.1016/j.ijsu.2014.07.013
Schenck R (2003) Classification of knee dislocations. Oper Tech Sports Med 11:193–198. https://doi.org/10.1053/otsm.2003.35918
KOOS questionnary [KOOS web site]. Available at: http:/www.koos.nu. Accessed 12 June 2011
Roos EM, Roos HP, Ekdahl C, Lohmander LS (1998) Knee injury and osteoarthritis outcome score (KOOS)–validation of a Swedish version. Scand J Med Sci Sports 8:439–448. https://doi.org/10.1111/j.1600-0838.1998.tb00465.x
Paradowski PT, Bergman S, Sunden-Lundius A et al (2006) Knee complaints vary with age and gender in the adult population. Population-based reference data for the Knee injury and osteoarthritis outcome score (KOOS). BMC Musculoskelet Disord 7:38. https://doi.org/10.1186/1471-2474-7-38
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clinical Orthop Relat Res 198:43–49
Williams GN, Taylor DC, Gangel TJ et al (2000) Comparison of the single assessment numeric evaluation method and the Lysholm score. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-200004000-00022
Irrgang JJ, Anderson AF, Boland AL et al (2017) Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 29:600–613. https://doi.org/10.1177/03635465010290051301
Gogia PP, Braatz JH, Rose SJ, Norton BJ (1987) Reliability and validity of goniometric measurements at the knee. Phys Ther 67:192–195. https://doi.org/10.1093/ptj/67.2.192
Pugh L, Mascarenhas R, Arneja S et al (2009) Current concepts in instrumented knee-laxity testing. Am J Sports Med 37:199–210. https://doi.org/10.1177/0363546508323746
Gustavsson A, Neeter C, Thomeé P et al (2006) A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc: Off J ESSKA 14:778–788. https://doi.org/10.1007/s00167-006-0045-6
Itoh H, Kurosaka M, Yoshiya S et al (1998) Evaluation of functional deficits determined by four different hop tests in patients with anterior cruciate ligament deficiency. Knee Surg, Sports Traumatol, Arthrosc: Off J ESSKA 6:241–245. https://doi.org/10.1007/s001670050106
Kostogiannis I, Ageberg E, Neuman P et al (2007) Activity level and subjective knee function 15 years after anterior cruciate ligament injury. Am J Sports Med 35:1135–1143. https://doi.org/10.1177/0363546507299238
Fanelli GC, Edson CJ (2002) Arthroscopically assisted combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Arthrosc J Arthrosc Relat Surg 18:703–714. https://doi.org/10.1053/jars.2002.35142
Ishibashi Y, Kimura Y, Sasaki E et al (2020) Acute primary repair of extraarticular ligaments and staged surgery in multiple ligament knee injuries. J Orthop Traumatol: Off J Ital Soc Orthop Traumatol 21:18. https://doi.org/10.1186/s10195-020-00557-5
Owens BD, Neault M, Benson E, Busconi BD (2007) Primary repair of knee dislocations: results in 25 patients (28 knees) at a mean follow-up of four years. J Orthop Trauma 21:92–96. https://doi.org/10.1097/BOT.0b013e3180321318
Li T, Xiong Y, Zhang Z et al (2021) Results of multiple ligament reconstruction after knee dislocation–a prospective study with 95 patients and minimum 2-year follow up. BMC Musculoskelet Disord 22:904. https://doi.org/10.1186/s12891-021-04596-9
Larsen P, Lund H, Laessoe U et al (2014) Restrictions in quality of life after intramedullary nailing of tibial shaft fracture: a retrospective follow-up study of 223 cases. J Orthop Trauma 28:507–512. https://doi.org/10.1097/BOT.0000000000000031
Fanelli GC (2020) Timing of repair or reconstruction after knee dislocation. J Knee Surg 33:335–338. https://doi.org/10.1055/s-0039-1700573
Snoeker B, Turkiewicz A, Magnusson K et al (2020) Risk of knee osteoarthritis after different types of knee injuries in young adults: a population-based cohort study. Br J Sports Med 54:725–730. https://doi.org/10.1136/bjsports-2019-100959
Funding
The author(s) received no financial or material support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to report. The authors did not receive benefits or grants in any form from a commercial party related directly or indirectly to the subject of this article. The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare that are relevant to the content of this article. All the authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Ethical approval
The local Research Ethics Committee has approved the study.
Informed consent
Written informed consent was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Said, S.M., Elsoe, R., Mikkelsen, C. et al. Clinical, functional, and patient-reported outcome of traumatic knee dislocations: a retrospective cohort study of 75 patients with 6.5-year follow-up. Arch Orthop Trauma Surg 143, 2589–2597 (2023). https://doi.org/10.1007/s00402-022-04578-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04578-z





