Abstract
Recent studies report mid- and long-term oncologic control with thermal ablation for small renal tumors to be equivalent to surgery. Comparisons of cryoablation, radiofrequency ablation (RFA), and laparoscopic approaches to percutaneous approaches report equivalent results. Studies report little or no decrease in renal function after ablation of renal tumors. These studies support the use of percutaneous thermal ablation for treatment of small renal malignancies. Studies also report that percutaneous ablation is a safe and durable treatment of the primary tumor in stage IV patients, ultrasound guidance for percutaneous ablation can be effective, and chyluria is relatively common after RFA. Results were disappointing for newer ablation techniques, including microwave, irreversible electroporation, and high-intensity focused ultrasound. These techniques require improvements before their use in place of RFA and cryoablation. The rates of diagnostic and subtype-specific renal tumor biopsies can be improved by using both aspirate and core techniques.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over the past decade, interest in and use of thermal ablation (TA) for treatment of renal tumors has increased substantially. However, questions have remained regarding oncologic efficacy and risk of complications. In addition, competing technologies, such as radiofrequency ablation (RFA) and cryoablation, continue to be studied to determine optimal techniques for oncologic control of renal cell carcinomas (RCCs). This article reviews recent studies evaluating RFA, cryoablation, and other newer modalities for ablation of RCCs. Some important developments to be discussed include oncologic outcomes, comparison of surgical versus percutaneous ablation techniques, renal function preservation using TA, cost effectiveness of TA, new applications of TA for treatment of RCC, various guidance systems, complications, and evaluation of new ablation techniques such as microwave ablation, irreversible electroporation (IRE), and high-intensity focused ultrasound (HIFU). Recent results on techniques and utility of renal tumor biopsy before treatment also will be discussed.
Oncologic Control
Since the development of TA techniques for treatment of RCCs, questions have arisen regarding the oncologic efficacy of these techniques. Because there can be no pathologic assessment of ablation margins and RCCs typically show modest growth, long-term data is required to confirm oncologic efficacy of TA techniques. An important recent study looked at greater than 5-year follow-up in patients with biopsy-proven RCCs treated with RFA [1••]. All treatments were done percutaneously with computed tomography (CT) guidance. In this series, 24 patients with 30 RCCs survived with a median follow-up of 61 months. There were several significant findings from this study looking at long-term disease-free survival rates for patients with RCC treated with percutaneous RFA. There were no recurrences when RCCs smaller than 4 cm were treated with RFA. No patients in the long-term survival group had metastatic RCC. One patient with an RCC larger than 4 cm did develop a late recurrence at 68 months, which was successfully treated with repeat RFA. The long-term recurrence-free survival rate was 88% after RFA, with only one patient requiring re-ablation. In this study, 12% of patients did have recurrent/residual tumor after a single RFA session. None of the tumors with recurrence were smaller than 4 cm and the median size of the tumors with recurrence was 5.2 cm. This suggests that RFA is substantially less effective for tumors larger than 4 cm, but is highly effective for smaller tumors. These long-term outcomes support the use of percutaneous RFA in patients with small RCCs who are not optimal surgical candidates, and raise the possibility of applying this technology to a larger subset of patients without significant comorbidities.
A second study with nearly identical results involved percutaneous CT–guided RFA of 31 patients with 39 renal tumors, none biopsy-proven [2]. The average follow-up of these patients was 61.2 months with a range of 36 to 84 months. The overall 3- and 5-year tumor control rates were 92% and 89%, respectively. Tumor recurrence was seen in four tumors, and the major risk factor for recurrence was tumors larger than 4 cm, a finding identical to the previously described long-term follow-up study.
A third renal RFA study used a combination of intraoperative and percutaneous image-guided RFA to assess long-term oncologic outcomes [3]. In this study, 79% of tumors were confirmed to be RCC. This study reported 5-year actuarial metastasis-free and cancer-specific survival rates of 95% and 99%, respectively. The mean follow-up period was 27 months. Good intermediate-term data were yielded from 53 of the biopsy-proven RCCs that were followed for greater than 3 years.
A fourth study examined the intermediate-term results for laparoscopic RFA of 90 biopsy-proven RCCs and found a disease-free survival rate of 97.8%, as well as cancer-specific and overall survival rates of 100% [4].
One additional recent paper looked at intermediate-term results for surgical cryoablation of 21 RCCs in 19 patients; all lesions were smaller than 4 cm [5]. Mean follow-up period was 41.6 months, with a range of 7 to 84 months. Recurrences occurred in four patients, with one cancer-specific death in this group. The 4-year recurrence-free survival rate was 83.6% and the overall survival rate was 94.1% for patients treated with surgical cryoablation. While the recurrence rate is slightly higher in this study than the previously described RFA studies, the small size of this series calls into question its statistical significance.
These five recently published studies all appear to confirm excellent oncologic efficacy of TA techniques for treatment of small RCCs. Follow-up data exceeding 5 years strongly support the durable oncologic efficacy of RFA for treatment of RCC [1••]. While these techniques are largely reserved for patients with significant comorbidities, consideration of applying percutaneous TA techniques to a larger population of patients with small RCCs seems warranted. In addition, these studies indicate that tumors larger than 4 cm have a substantially higher likelihood of residual/recurrent disease after ablation techniques. Close follow-up of these patients is recommended. Additional ablation cycles or surgical techniques may be required for complete tumor eradication. Finally, because late recurrences are reported in these studies, long-term imaging follow-up of at least 5-years duration after TA is recommended to exclude recurrence.
Surgical Versus Percutaneous Ablation Techniques
Three recent studies compared percutaneous with surgical ablation techniques [6, 7••, 8]. Two of these studies focused on percutaneous versus laparoscopic cryoablation of small renal masses [6, 8]. One study, a mixed retrospective and prospective study, compared 90 patients who underwent percutaneous cryoablation and 81 patients who underwent laparoscopic cryoablation [7••]. There was a slightly higher rate of primary treatment failure in the percutaneous group than in the laparoscopic group, albeit not statistically significant. After primary treatment failure, the residual tumors were successfully retreated with percutaneous cryoablation. There was a slightly higher complication rate in the laparoscopic group, but again, this was not statistically significant. This study did find that patients undergoing percutaneous cryoablation had a reduced hospital stay and lower surgical complication rate compared to surgical cryoablation. Renal function was maintained in both groups.
A group from Fox Chase Cancer Center and Temple University did a cumulative review and analysis of literature comparing percutaneous cryoablation and surgical cryoablation of small renal tumors [6]. Their data also found that there was no statistically significant difference in oncologic control between surgical and percutaneous cryoablation procedures.
Finally, one study compared patients who underwent percutaneous RFA with patients who underwent radical nephrectomy and/or partial nephrectomy for stage T1a RCCs. In this study, 51 patients underwent RFA, 54 patients had radical nephrectomy, and 10 patients had partial nephrectomy. At 5-year follow-up, the disease-free survival rate after RFA was 98%, comparable to radical nephrectomy, which had a rate of 95%; partial nephrectomy had a 3-year disease-free survival rate of 75%. This difference was not statistically significant. As expected, renal function decline was substantially worse for radical nephrectomy than for the RFA and partial nephrectomy cohorts.
These three studies support the use of percutaneous TA instead of surgical TA techniques. The data indicate no significant difference in oncologic outcomes for percutaneous ablation compared to laparoscopic or open surgical techniques. There are also major advantages of percutaneous techniques, including shorter hospital stay and fewer complications. Based on these findings, it appears that laparoscopic TA should be reserved for the small subgroup of patients with small renal masses that cannot be treated safely using percutaneous RFA or cryoablation. While surgical extirpation of small renal masses remains the most widely accepted curative technique, these recent results suggest that oncologic control with percutaneous TA techniques are similar, if not identical, to those achieved with resection.
Cryoablation Versus Radiofrequency Ablation
A recently reported study compared 41 percutaneous RFAs and 70 percutaneous cryoablations for treatment of small renal masses [9••]. The study investigators found that there was no significant difference between recurrence rates using these two techniques. There were no major procedural complications in either group of treated patients. Tumors treated in this study ranged from 0.8 to 4.8 cm in diameter, with a mean of 2.2 cm. These data further confirm that the oncologic efficacies of percutaneous cryoablation and percutaneous RFA are equivalent for small renal tumor ablation.
Preservation of Renal Function
Four recent studies examined the impact of TA techniques on renal function [7••, 10–12•]. One study, which also addressed the oncologic efficacy of cryoablation, evaluated 90 patients with 99 tumors who were treated with percutaneous or laparoscopic cryoablation [7••]. Analysis of these patients showed that renal function did not significantly change in these patients after cryoablation. A second study evaluated the effect on renal function for 29 patients who underwent percutaneous cryoablation and for 36 patients who underwent RFA for treatment of renal tumors in solitary kidneys [10]. There was no significant decrease in renal function after percutaneous ablation in either group of patients.
Two additional studies involved only patients undergoing percutaneous RFA [11, 12•]. One evaluated 62 patients who underwent RFA for treatment of renal tumors [12•]. In this study group, there was no mean difference in estimated glomerular filtration rate (eGFR) values from baseline to 1 month or 1 year after percutaneous RFA for treatment of a single renal mass. The second study focused on patients with Von Hippel–Lindau disease (VHL) who underwent percutaneous RFA [11]. All patients in this study had previously undergone renal surgery. In this group of VHL patients, serum creatinine increased 6.4% and the mean eGFR rate decreased by 12.8% after the last ablation.
These four studies confirm earlier observations indicating that TA techniques, either percutaneous or laparoscopic (including both RFA and cryoablation), result in excellent renal function preservation [7••, 10–12•]. Three of these four studies showed no significant decrease in renal function after ablation [7••, 10, 12•] while the fourth study showed a mild decrease in renal function after percutaneous RFA [11]. When preservation of renal function is a high priority in patients with small renal tumors, TA appears to be an excellent option.
Cost-Effectiveness of Various Nephron-Sparing Options in the Management of Small Renal Masses
An interesting recent analysis utilized an analytic Markov model to evaluate treatment options and health outcomes for a theoretical healthy 65-year-old patient found to have an asymptomatic unilateral small renal tumor [13••]. This theoretical model compared open and laparoscopic partial nephrectomy as well as laparoscopic and percutaneous ablation, active surveillance with possible delayed intervention, and nonsurgical management utilizing observation. All options compared were considered nephron-sparing approaches. This study found that laparoscopic partial nephrectomy is the preferred nephron-sparing option for healthy patients younger than 74 years. An effective alternative option is surveillance with possible delayed percutaneous ablation for patients with advanced age or for those with significant comorbidities.
This cost-effectiveness analysis supports the idea of utilizing percutaneous TA techniques in patients with active small renal masses who have significant comorbidities or are of advanced age. In addition, the results also seem to support utilization of percutaneous TA for other patients in whom surgical nephron-sparing approaches are not feasible.
Trends in Use of Various Treatments for Localized Kidney Cancer
A recent large study has examined the Surveillance, Epidemiology, and End Results (SEER) database to discern trends in utilization of treatment techniques for localized renal cancers, focusing on stage I RCC [14]. Over 15,000 patients underwent a procedure for RCCs that were organ-confined and less than 7 cm in diameter. While over 14,000 of these procedures were surgical, with a greater than 2:1 ratio of radical nephrectomy to partial nephrectomy, the use of TA for stage I RCC was increasing over a relatively short period near the end of the time evaluated in this study. As expected, TA was more commonly used in patients of more advanced age with smaller tumors. Use of both partial nephrectomy and TA were increasing when compared to radical nephrectomy rates.
This data analysis indicates that use of TA is increasing, particularly for patients with advanced age who have small renal tumors. Based on the growing body of data supporting TA techniques, it is expected that this trend will continue, especially among patients with serious comorbidities or for those in whom partial nephrectomy is not feasible.
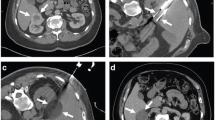
Collecting System Complications with Central Cryoablation
One recent study evaluated the complication rates of percutaneous cryoablation when the resultant ice ball involved a portion of the renal collecting system [15••]. In 67 patients, the ice ball involved the renal sinus to some degree. However, there were no collecting system injuries identified after cryoablation of the renal sinus. One patient did develop hemorrhage that required intervention. This study indicates that cryoablation of the peripheral portions of the renal sinus is relatively safe without significant risk of collecting system injury. While this study does provide evidence of the safety of utilizing percutaneous cryoablation for centrally located lesions, techniques such as ureteral perfusion should be used when either cryoablation or RFA is utilized in proximity to a vulnerable portion of the pelvocalyceal system such as the ureteropelvic junction or upper ureter.
Radiofrequency Ablation of the Primary Tumor in Patients with Stage IV Renal Cell Carcinoma Undergoing Systemic Therapy
The efficacy of cytoreductive nephrectomy in some patients with stage IV disease who are undergoing immunotherapy has been established. One recent novel study evaluated the feasibility and safety of utilizing RFA for treatment of the primary RCC in patients with metastatic disease undergoing systemic immunotherapy instead of resection [16]. In this retrospective study, 15 patients were treated with percutaneous RFA. The authors found that percutaneous RFA was safe and resulted in durable local control of the primary RCC. This technique, which avoids the morbidity associated with nephrectomy, supports the idea of using percutaneous TA techniques for cytoreductive treatment when systemic immunotherapy is used for patients with metastatic RCC.
Comparison of Ultrasound and Computed Tomography Guidance for Percutaneous Radiofrequency Ablation
While previous studies have almost exclusively used CT guidance for percutaneous TA, one study evaluated the possibility of replacing CT guidance with ultrasound guidance for RFA treatment of small renal tumors [17]. In this study, 36 renal tumors in 32 patients were treated with percutaneous RFA exclusively utilizing ultrasound guidance. Primary treatment effectiveness was 86.1% and the rate of major complications was 8.3%, both comparable to studies using CT guidance. This study concluded that ultrasound-guided RFA is an effective treatment of small renal tumors with results comparable to those published for CT-guided RFA studies. Most authors utilize CT guidance to avoid injury to adjacent vulnerable structures that may be difficult to visualize with ultrasound, such as ureter, colon, and pancreatic tail. However, this study supports the use of ultrasound guidance for RFA treatment, particularly when the tumor is known to be distant from adjacent vulnerable organs. Other limitations exist for ultrasound guidance when using cryoablation, particularly inability to visualize the depth of the ice ball due to shadowing from the near edge.
Chyluria After Radiofrequency Ablation of Renal Tumors
While it has been recognized for some time that chyluria occurs after percutaneous RFA for treatment of renal tumors, a recent study evaluated the significance and incidence of this abnormality [18]. This study found that chyluria occurred in 41% of patients who had renal tumors treated with percutaneous RFA. It is speculated that chyluria occurs due to fistulization with lymphatics in the zone of ablation. It was also found that the chyluria was asymptomatic in these patients, but did persist for a prolonged period of time. Therefore, chyluria is a common finding after RFA of renal tumors. It also can be seen after renal surgery or renal trauma. It appears to be of no clinical significance, but it is useful to be aware of this finding so that it is not confused with a significant complication or other abnormality.
Other Ablation Techniques: Microwave, Irreversible, Electroporation, and High-Intensity Focused Ultrasound
There have been several recent studies assessing the safety and efficacy of emerging ablation techniques for treatment of small renal tumors. Castle et al. [19] reviewed their experience in 10 patients using a microwave ablation device. The results of this study were disappointing and substantially worse than would be expected for cryoablation or RFA. In this study, where the mean tumor size was 3.65 cm, there was a 38% recurrence rate and the complication rate was 40%. While theoretically microwave ablation has some advantages, this early study indicates that it should not be utilized routinely for ablation of renal tumors when other techniques, such as RFA and cryoablation, are available. Improvements in microwave ablation technique and technology will be needed before advocating its use for treatment of small renal tumors.
Irreversible electroporation (IRE) is a nonthermal ablative technique utilizing direct electrical pulses to induce apoptosis and ultimately cell death in the exposed area. Preliminary results have suggested that IRE preserves extracellular matrix and may result in less collateral damage than TA techniques. Three recent studies with preliminary results suggest that IRE deserves further evaluation for the treatment of renal tumors [20–22]. Deodhar et al. [20] evaluated 29 ablations in porcine kidneys. This showed effective necrosis without intervening live cells. While there was urothelial sloughing, the renal pelvic extracellular matrix was intact after IRE, suggesting that urothelial regeneration could occur. This study did not evaluate ablation size or effectiveness in treating renal tumors. A second study looked at the safety of IRE in humans including seven RCCs smaller than 1.3 cm [22]. Once synchronized electrocardiogram (EKG) gating was utilized, IRE was found to be safe for use in humans. However, treatment results were disappointing for these small RCCs. Of the seven treated RCCs, two developed progressive disease and one developed a ureteral stricture. While this study suggests that EKG gating can overcome arrhythmia problems experienced with IRE, more data on efficacy of IRE for treatment of small renal tumors will be required before this can be endorsed as a treatment modality comparable to RFA or cryoablation.
Additionally, a phase 1 clinical study involved six patients who were undergoing curative resection of RCC and underwent IRE in the operating room before resection [21]. This study did not examine the efficacy of IRE in ablating renal tumors, but evaluated the safety of applying IRE to humans with renal tumors. Close monitoring of cardiac rhythm and hemodynamic variables in these patients showed no significant perturbation during IRE application. The authors concluded that IRE is feasible and hemodynamically safe for use in patients with renal tumors. As with the other IRE studies, further clinical data will be required before accepting this technique as an alternative to other ablation techniques.
A recent review article evaluated the utility of high-intensity focused ultrasound (HIFU) for treatment of renal tumors [23]. This article highlights the difficulties in using HIFU for treatment of even small renal tumors. Two human studies reviewed in this paper showed that HIFU was unreliable in inducing even minimal histologic damage in small renal tumors. In one of the studies, histologic necrosis could be detected in only 9 of 14 treated tumors. Additionally, in those that did demonstrate some histologic necrosis, the necrotic area encompassed a maximum of 35% of the targeted tumor tissue. In a second study, where HIFU was applied as palliative treatment in 13 cases of advanced RCC, treatment was considered to be inadequate in 10 of those patients. While there have been no serious side effects from HIFU, it appears to be inadequate, in its current state, for treatment of RCC.
Improved Biopsy Techniques for Sampling of Renal Neoplasms
One recent study performed at Wake Forest Baptist Medical Center examined the results from 351 consecutive patients who underwent biopsy before percutaneous TA of renal tumors [24••]. Both fine-needle aspiration and 20-gauge core biopsies were performed in most cases. When pathologic reports were either diagnostic, suspicious, or included atypical findings, 89.3% of biopsies were diagnostic of neoplasm. In this study, fine-needle aspiration biopsy was found to have greater sensitivity and utility than core biopsies, but the role of the two techniques was complementary. Core biopsy was particularly useful for specific classification of histologic types of RCC and for additional studies when classifying some problematic histologic types of tumors. Based on this study, it is recommended that both fine-needle aspiration and core biopsies be obtained to maximize diagnostic yield when biopsying small renal tumors.
Conclusions
Recent publications have demonstrated a trend of increasing use of TA for treatment of small renal tumors. Based on the recently published studies described in this paper and the authors' experience, this trend is likely to accelerate. This acceleration will be due to the results reported here, including long-term follow-up data indicating excellent oncologic outcomes after both RFA and cryoablation of small RCCs. The results for treatment of RCCs smaller than 4 cm are comparable to those of surgical extirpation. Comparison studies indicate that RFA and cryoablation have equivalent rates for eradication of small RCCs. Reported complication rates remain low. Recent studies also support the advantages of percutaneous TA over surgical ablative techniques. The data show no oncologic advantage of laparoscopic RFA or cryoablation when compared to percutaneous application of these techniques. For these reasons, when TA is indicated for treatment of a small renal tumor, percutaneous techniques should be preferred. Because there are growing data that the results of percutaneous TA are comparable to surgical resection, consideration may be given to expanding the pool of candidates for percutaneous TA beyond those of advanced age with serious comorbidities.
Studies noted in this article reinforce the fact that TA techniques result in minimal, if any, significant decrease in renal function. For this reason, ablation has substantial benefits over radical nephrectomy for treatment of small RCCs. Percutaneous ablation should be considered when even a healthy patient cannot undergo partial nephrectomy for tumor treatment. In addition, recent studies have shown that ultrasound, as an alternative to CT, may be used as an effective guidance technique for percutaneous treatment of small renal tumors. Ideally, ultrasound can be used for tumors that are known to be well away from adjacent vulnerable structures such as bowel and ureter. Also, RFA or cryoablation can be considered for cytoreductive treatment of the primary RCC in some patients with metastatic RCC who are undergoing systemic immunotherapy. Results utilizing ablation instead of nephrectomy appear to be comparable, but without the morbidity of surgery.
If biopsy of a renal tumor is to be performed before treatment, then a large series quoted in this article indicates that a combination of both fine-needle aspiration and core biopsy is beneficial for diagnosis and subtyping of renal tumors.
Finally, new techniques that are emerging include microwave ablation, IRE, and HIFU. Preliminary studies indicate that while these appear to be reasonably safe, the results are not comparable to the more mature techniques, RFA and cryoablation. Further study of these newer techniques will be required before they can be advocated for clinical use in treatment of small renal tumors.
Based on the oncologic outcome study, it is imperative that long-term follow-up imaging surveillance of patients who have undergone TA techniques be performed. Late recurrences have been reported and, while these can safely be treated with repeat ablation, detection of these late recurrences is imperative to avoid the undetected development of advanced stage disease.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Zagoria RJ, Pettus JA, Rogers M, et al. Long-term outcomes after percutaneous radiofrequency ablation for renal cell carcinoma. Urology. 2011;77(6):1393–7. This study provides greater than 5-year follow-up in patients with biopsy-proven RCC. For tumors smaller than 4 cm, there was no disease recurrence after RFA.
Ferakis N, Bouropoulus C, Granitsas T, et al. Long-term results after computed-tomography-guided percutaneous radiofrequency ablation for small renal tumors. J Endourol. 2010;24(12):1909–13.
Tracy CR, Raman JD, Donnally C, et al. Durable oncologic outcomes after radiofrequency ablation: experience from treating 243 small renal masses over 7.5 years. Cancer. 2010;116(13):3135–42.
Ji C, Li X, Zhang S, et al. Laparoscopic radiofrequency ablation of renal tumors: 32-month mean follow-up results of 106 patients. Urology. 2011;77(4):798–802.
Chalasani V, Martinez CH, Lim D, et al. Surgical cryoablation as an option for small renal masses in patients who are not ideal partial nephrectomy candidates: intermediate-term outcomes. Can Urol Assoc J. 2010;4(6):399–402.
Long CJ, Kutikov A, Canter DJ, et al. Percutaneous vs surgical cryoablation of the small renal mass: is efficacy compromised? BJU Int. 2011;107(9):1376–80.
•• Mues AC, Okhunov Z, Haramis G, et al. Comparison of percutaneous and laparoscopic renal cryoablation for small (<3.0 cm) renal masses. J Endourol. 2010;24(7):1097–100. The authors noted no significant difference in oncologic efficacy between percutaneous and laparoscopic cryoablation techniques. The percutaneous approach had the added benefits of reduced hospital stay and lower complication rate.
Takaki H, Yamakado K, Soga N, et al. Midterm results of radiofrequency ablation versus nephrectomy for T1a renal cell carcinoma. Jpn J Radiol. 2010;28(6):460–8.
•• Pirasteh A, Snyder L, Boncher N, et al. Cryoablation vs. radiofrequency ablation for small renal masses. Acad Radiol. 2011;18(1):97–100. In a head-to-head comparison, these thermal ablative techniques were found to have identical oncologic efficacies for the treatment of small renal masses.
Altunrende F et al. Image guided percutaneous probe ablation for renal tumors in 65 solitary kidneys: functional and oncological outcomes. J Urol. 2011;186(1):35–41.
Park SY, Park BK, Kim CK, et al. Percutaneous radiofrequency ablation of renal cell carcinomas in patients with von Hippel Lindau disease previously undergoing a radical nephrectomy or repeated nephron-sparing surgery. Acta Radiol. 2011;52(6):680–5.
• Pettus JA, Werle DM, Saunders W, et al. Percutaneous radiofrequency ablation does not affect glomerular filtration rate. J Endourol. 2010;24(10):1687–91. This article describes excellent renal function preservation following radiofrequency ablation.
•• Chang SL, Cipriano LE, Harshman LC, et al. Cost-effectiveness analysis of nephron sparing options for the management of small renal masses. J Urol. 2011;185(5):1591–7. This is a novel cost-effectiveness study utilizing an analytic model to evaluate treatment options and outcomes in a theoretical 65-year-old patient with a small asymptomatic renal tumor.
Choueiri TK, Schultz FA, Hevelone ND, et al. Thermal ablation vs surgery for localized kidney cancer: a surveillance, epidemiology, and end results (SEER) database analysis. Urology. 2011;78(1):93–8.
•• Rosenberg MD, Kim CY, Tsivian M, et al. Percutaneous cryoablation of renal lesions with radiographic ice ball involvement of the renal sinus: analysis of hemorrhagic and collecting system complications. AJR Am J Roentgenol. 2011;196(4):935–9. This study demonstrated that percutaneous cryoablation of tumors with endophytic components can be successfully undertaken without major collecting system complications.
Karam JA, Ahrar K, Wood CG, et al. Radio frequency ablation of renal tumors in patients with metastatic renal cell carcinoma. J Urol. 2010;184(5):1882–7.
Davis K, Kielar A, Jafari K. Effectiveness of ultrasound-guided radiofrequency ablation in the treatment of 36 renal cell carcinoma tumours compared with published results of using computed tomography guidance. In: Can Assoc Radiol J 2010, Published by Elsevier Inc.
Kaur H, Matin SF, Javadi S, et al. Chyluria after radiofrequency ablation of renal tumors. J Vasc Interv Radiol. 2011;22(7):924–7.
Castle SM, Salas N, Leveillee RJ. Initial experience using microwave ablation therapy for renal tumor treatment: 18-month follow-up. Urology. 2011;77(4):792–7.
Deodhar A, Monette S, Single GW, et al. Renal tissue ablation with irreversible electroporation: preliminary results in a porcine model. Urology. 2011;77(4):754–60.
Pech M, Janitzky A, Wendler JJ, et al. Irreversible electroporation of renal cell carcinoma: a first-in-man phase I clinical study. Cardiovasc Intervent Radiol. 2011;34(1):132–8.
Thomson KR, Cheung W, Ellis SJ, et al. Investigation of the safety of irreversible electroporation in humans. J Vasc Interv Radiol. 2011;22(5):611–21.
Nabi G, Goodman C, Melzer A. High intensity focused ultrasound treatment of small renal masses: clinical effectiveness and technological advances. Indian J Urol. 2010;26(3):331–7.
•• Parks GE, Perkins LA, Zagoria RJ, et al. Benefits of a combined approach to sampling of renal neoplasms as demonstrated in a series of 351 cases. Am J Surg Pathol. 2011;35(6):827–35. This study demonstrated a high diagnostic yield for percutaneous renal mass biopsy and underscored the importance of utilizing both fine-needle aspirate and core biopsy techniques.
Disclosures
R. Zagoria: none. Dr. David D. Childs has served as a consultant for Galil Medical.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zagoria, R.J., Childs, D.D. Update on Thermal Ablation of Renal Cell Carcinoma: Oncologic Control, Technique Comparison, Renal Function Preservation, and New Modalities. Curr Urol Rep 13, 63–69 (2012). https://doi.org/10.1007/s11934-011-0224-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-011-0224-y