Abstract
MR imaging and musculoskeletal ultrasound are expanding their utility in the assessment of patients with chronic inflammatory arthritis. These imaging techniques, by providing additional and more sensitive information over clinical examination and conventional radiographs, are promising tools for the diagnosis, prognosis and assessment of treatment efficacy in patients with juvenile idiopathic arthritis (JIA). Owing to the peculiarities of the growing skeleton, knowledge of imaging in healthy children is of high priority. A sound understanding of growth-related changes is of foremost value in establishing whether the apparent changes on joint surface reflect real damage or are actually part of normal development. This review explores current evidence and suggests a new workflow for imaging in JIA, in which conventional and modern imaging modalities can be integrated for optimal management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Juvenile idiopathic arthritis (JIA) is the most common chronic rheumatic disease in childhood with a prevalence that varies between 16 and 150 per 100,000 children [1]. JIA is not a single disease entity but an exclusion diagnosis which includes all forms of chronic arthritis that begin before the age of 16 years, persist for more than 6 weeks, and are of unknown origin. Indeed, JIA encompasses several disease categories, each with its own distinct clinical features and, in some cases, genetic background [2, 3]. Despite the heterogeneity, all forms are characterized by synovial inflammation, which if not adequately controlled may ultimately lead to cartilage loss and bone damage and consequent permanent disability [4]. Of note, JIA is one of the main causes of acquired disability in childhood [5].
Over the past decade, the management of JIA has dramatically changed, owing to the shift towards early aggressive interventions and the development of effective structure-modifying drugs, such as biological agents, that have considerably decreased the risk of permanent damage to joint structures [6–10]. As a consequence, it has become essential to identify patients who are more likely to develop unremitting illness carrying significant risk of joint destruction and who are suitable for aggressive treatment early in the disease course [11–13].
Imaging has a considerable role in the diagnosis of JIA, in assessing its severity and prognosis and in monitoring treatment efficacy. Conventional radiography (CR) is regarded as the mainstay of imaging evaluation of joint structural damage in children with JIA. However, the trend towards the early introduction of effective disease-modifying treatments has generated the need for alternative imaging modalities that are more sensitive in detecting pre-erosive inflammatory changes, in order to stratify patients for treatment and to monitor therapeutic efficacy more effectively. CR is inadequate in this setting, as it reveals late and largely irreversible consequences of synovial inflammation. Magnetic resonance imaging (MRI) and musculoskeletal ultrasound (MSUS) are therefore playing an expanding role in the assessment of arthritic joints. Despite the large amount of evidence that has accumulated on the value of these modern imaging modalities in predicting and monitoring treatment efficacy in adults with rheumatoid arthritis (RA) [14–20], this field has remained almost unexplored in JIA.
Unlike adults, imaging in children represents a real challenge because growing joints change anatomically over time. During childhood, skeletal maturation is marked by an orderly sequence of recognizable changes in the appearance of the skeleton. Such changes include timing and sequence of appearance of ossification centres, specific alterations in bone contours, and timing of the ultimate closure of the growth plates. All these growth-related physiological changes may be altered by chronic joint inflammation, resulting in radiographic changes, such as advancement of maturation and epiphyseal overgrowth secondary to hyperemia, or retardation of maturation due to damage, which are peculiar to JIA.
The present review aims to provide current evidence to support the use of MRI and MSUS for the assessment of patients with JIA, both in clinical and research settings. Furthermore, the specific aspects relevant to the evaluation of the growing skeleton will be discussed.
Magnetic Resonance Imaging
MR imaging, by providing multiplanar tomographic imaging with unparallel soft tissue contrast, allows the assessment of all joint structures involved in inflammatory arthritis. A thorough knowledge of the advantages and limitations of this imaging modality (Table 1) is crucial for identifying the clinical context in which MRI is most likely to be recommended. To diagnose JIA properly, a wide range of differential diagnoses needs to be excluded, many of which have recognizable features on imaging. CR is the first-step imaging modality in order to exclude other causes of joint pain and swelling in children, such as trauma, osteochondroses, osteoid tumors, or skeletal dysplasias [21–23]. In selected cases, however, MRI may be indicated to rule out other intra-articular disorders that mimic inflammatory arthritis such as hemangioma or pigmented villonodular synovitis [24–26]. In patients with known JIA, MRI is well suited to depict the involvement of particular joints that are not easy to assess clinically, such as the temporo-mandibular, hip, and sacroiliac joints [27–33]. Finally, MRI appears suitable for identifying odontoid lesions and assessing functional instability of the cervical spine [34].
Over the last decade, however, along with breakthroughs in therapeutics, new expectations of MRI have emerged. By directly imaging synovitis, contrast-enhanced MRI has an intuitive advantage in assessing response to treatment over clinical surrogate measurements of inflammation (Fig. 1). Standardized and validated methods of evaluating MRI findings in JIA have progressed and validated pediatric scales are now available [35–38]. In a recent study comparing MRI and clinical criteria in 40 JIA patients who were starting a second-line therapy, the Rheumatoid Arthritis MRI synovitis score has proven to be a promising imaging biomarker for measuring therapeutic response [39•]. Notably, only the highest levels of clinical response were associated with significant decrease in synovitis and the halting of structural damage. These findings support the need to move towards more strict definitions of clinical response when assessing drug efficacy in JIA, and suggest the potential for MRI as a primary efficacy outcome in clinical studies. In this field of outcome assessment, prospective quantitative measurements of synovitis appear particular promising in evaluating treatment efficacy. Due to advances in imaging technologies, the rate and magnitude of synovial enhancement that reflect local tissue vascularity and capillary permeability can be reliably quantified using dynamic contrast-enhanced MRI (DCE-MRI). This technique has permitted the differentiation of active, hypervascular synovial membrane from the inactive, fibrotic pannus and provides a reliable assessment of disease activity in patients with JIA [40]. Furthermore, the use of pharmacokinetic modeling to quantify DCE-MRI, has provided an objective follow-up measure of therapeutic efficacy in JIA pilot studies [41, 42]. In addition, computerized measurements of wrist synovial volumes (Fig. 2), obtained using an automated segmentation program in a cohort of 56 JIA patients, were found to be more sensitive in detecting treatment efficacy and predicting progressive joint destruction compared to a semi-quantitative approach [43]. Quantitative methods are not typically part of standard daily practice, since they require post-processing analysis and dedicated software. Owing to their high sensitivity in detecting even the smallest treatment-related changes, they appear particularly promising in a clinical trial setting.
Wrist MRI in a 12-year-old girl with juvenile idiopathic arthritis. Contrast-enhanced coronal 3D Fast Field Echo T1-weighted MRI with fat saturation shows active synovitis in the radioulnar, radiocarpal and intercarpal joint recesses and diffuse bone marrow oedema involving several carpal bones and the metacarpal bases (a). Marked reduction of synovitis and bone marrow oedema after treatment with anti-tumour necrosis factor α (b)
Therapeutic advances have increased the expectations of treatment benefits with disease remission now becoming a realistic goal [44, 45]. Sustained synovitis detected by MRI was recently documented in a sizable proportion of JIA patients who satisfied clinically-defined remission criteria [39•, 43, 46]. However, no longitudinal studies have thus far investigated whether subclinical inflammation may end up in further joint damage and functional disability, as reported in adults with RA [47]. Overall, although MRI appears a promising outcome measure for the assessment of treatment efficacy and remission, further studies are required to establish whether targeting therapy to the measures obtained from imaging provides better outcomes compared to treating by using only clinical targets.
Early detection of patients who will develop erosive damage and consequent aggressive control of the disease is a highly desirable goal to reduce the chance of further disability. MRI is the only imaging modality able to visualize bone marrow edema (BMO), a key predictor of erosive joint damage and functional impairment in adults with RA [48–50]. Recent studies comparing MRI appearances with bone histology in patients with RA have revealed that BMO regions contain a vascularized, cell-rich inflammatory tissue in close apposition to activated osteoclasts, as revealed by extensive expression of RANKL [51]. These findings have suggested a new pathway for the development of bone erosions, which starts from an inflammatory process within BM leading to RANKL-induced osteoclastogenesis and bone resorption. Caution is, however, needed before considering BMO as a prognostic indicator in JIA, since longitudinal studies investigating whether the presence of BMO predates the development of bone erosions are still lacking. Furthermore, signal changes resembling BMO have recently been detected in a high percentage of carpal bones in healthy children of different ages [52••, 53]. Notably, the same phenomenon was not reported in similar studies including healthy adults [54, 55], thus highlighting the peculiarities of the growing skeleton and the need to include age-matched healthy subjects in MRI studies on JIA.
The availability of normative data is also pivotal for an accurate assessment of bone erosions. In line with studies in RA [56, 57], the higher sensitivity of MRI in detecting early erosive damage over the others imaging modalities has been demonstrated also in JIA [27, 28, 58]. However, a certain concern that the increased sensitivity of MRI may be at the cost of a reduced specificity has been raised after a MRI study on 88 healthy children in which bony depressions, mimicking erosive changes, were found in the carpal bones of all subjects [52••]. A sound knowledge of growth-related bony changes is of foremost value to establish whether the apparent changes on bone surface are pathological or part of normal development [59]. Unexpectedly, Malattia et al. did not find a clear advantage in the use of wrist MRI compared to CR when evaluating structural damage progression over 1 year [39•]. The fact that cartilage loss, whose evaluation is included in the radiographic scale but not in the MRI scoring system, is the most common form of damage throughout the disease course [60] might explain the higher sensitivity of CR in detecting structural changes. Additionally, in younger children, the radiographic changes in carpal bones are frequently observed and scored as deformity in shape rather than as discrete erosions [60]. This phenomenon is distinctive of JIA and is likely attributable to a combination of growth abnormalities, ossification of previous injured cartilage, and true bone erosions [61, 62]. Owing to the unique features of the growing skeleton, the MRI definition of damage developed for RA patients may not necessarily be applicable to pediatric patients. A more comprehensive MRI scale incorporating measurements of cartilage damage and bone deformity may increase the sensitivity of this imaging technique for testing the disease-modifying potential of antirheumatic drugs.
As previously mentioned, articular cartilage is a major target of the erosive process in chronic inflammatory arthritis, and the assessment of its integrity should constitute a key goal for any imaging modality used in children with JIA. MRI allows discrimination between different types of cartilage (articular, epiphyseal, and physeal) and the direct visualization of signs of cartilaginous damage such as thinning and erosions (Fig. 3) [63]. Of note, it is also possible, through the use of apposite MR techniques and software, to investigate biophysical properties and molecular changes in the composition of extracellular cartilage matrix that occur before morphologic changes can be detected by conventional imaging and when cartilage damage is potentially reversible [64–67].
Musculoskeletal Ultrasound
The use of MSUS is rapidly undergoing expansion into daily clinical practice for the diagnosis, monitoring, and managing of patients with JIA. MSUS is even more appealing for pediatric rheumatologists than other imaging modalities, as it does not entail sedation and ionizing radiation, allows a safe and multiplane assessment of several joints at one time, and is well accepted (Table 2) [68•]. The evolution of ultrasound equipment by manufacturers, with miniaturization and the availability of useful higher frequency transducers, have made joint evaluation considerably easier in the joints of children that are difficult to reach owing to their small size [69•]. Furthermore, the advent of Doppler modalities, as applied in the MSUS assessment, has allowed the identification of intra-synovial vascular signals, which can consistently help to differentiate active synovitis from inactive disease. Nevertheless, the current major limitation of the technique lies in its strong operator dependency and in the equipment used. Additionally, MSUS is not yet a properly validated tool for the assessment of synovitis in children with JIA [70•], as no definitions of common ultrasound abnormalities and standard reference values have been developed thus far.
The potential of MSUS to visualize most of the anatomical structures involved throughout JIA course is of considerable help in the successful management of disease. The integrity of cartilage can be appropriately detected by MSUS. Damage usually appears as cartilage loss with thinning or blurring of its anechoic structure. Recent studies have reported an acceptable inter- and intra-observer reliability [71] and a good agreement between MSUS and MRI for the measurement of cartilage thickness [72] in all the joints considered, except for the wrist. Furthermore, age- and sex-related normal standards for cartilage thickness for several joints have been established [73]. Recently, the same investigators described a decrease in cartilage thickness in JIA patients, when matched with similar joints of healthy subjects, with the loss being greatest in the knee of systemic and polyarticular JIA patients, which are commonly known to be the most clinically aggressive subtypes. Of interest, a decrease in joint cartilage thickness was also found in joints without previous arthritis involvement [74]. Overall, these findings highlight the potential of MSUS in the assessment of cartilage integrity, either in clinically active or in subclinical disease, and they may change the future approach in caring for patients with JIA by guiding very early and tailored treatment aimed at preventing the establishment of osteocartilaginous injury.
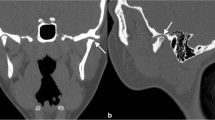
Indeed, structural damage is often a direct result of a chronic and uncontrolled synovitis and the occurrence of an early bone erosion has been associated with a poor long-term outcome in children with JIA [11]. The assessment of erosive changes in a growing skeleton is challenging, as some physiological bone irregularities in recently ossified bones can be misinterpreted as cortical erosions [69•]. Owing to the lack of studies on normal sonographic bone anatomy for all age groups, the use of MSUS may potentially lead both to an over- or under-estimation of structural damage in children with JIA, and this is the major current limitation for the application of the technique for such evaluation. In addition, MSUS performs at its best for assessing bone erosions only where accessibility is optimal and allows a perpendicular positioning of the probe over the examined bone structure. In this context, the anatomical areas which cannot be reached with a comprehensive 360° assessment, such as intercarpal and intertarsal bones and hip, are more complex to evaluate.
MSUS has proven to be more accurate than clinical evaluation in the assessment of joint inflammation [75–77]. As the current ILAR classification for JIA is based on the number of affected joints, the issue of MSUS detectable subclinical synovitis may be particular relevant in JIA. The detection of subclinical inflammation by MSUS may potentially lead to both reclassifying patients and shifting to a more aggressive treatment. Joint effusion and synovial hypertrophy are the most common abnormalities detected by gray-scale MSUS (Fig. 4), but they may not reflect ongoing active disease [47]. Color and power Doppler modalities are of particular benefit in the assessment of active joint inflammation in comparison with gray-scale alone (Fig. 5). However, the interpretation of juxta-articular Doppler signal is challenging in children, as it can be a sign of the increased synovial vascularization indicating inflammation, or expression of the physiologically enhanced blood flow of the well-vascularized epiphyseal cartilage [77]. Unlike adults with RA [78], the prognostic meaning of MSUS findings in JIA is still being debated, as abnormalities, including Doppler signal, have been documented not to predict a flare of disease [79••]. This shortcoming further highlights the need to define the normal sonographic anatomy throughout pediatric age groups before addressing the role of MSUS in children with JIA.
Tendons are another anatomical compartment frequently involved throughout JIA course, and isolated tenosynovitis may be responsible for joint swelling and pain (Fig. 6). It is common knowledge that prominent adipose tissue and the small size of the joints create difficulties in interpretation even for the well-trained physician who attempts to identify clinically tenosynovitis in younger children. Recently, attention was centered around the assessment of joint and tendon disease using MSUS compared to clinical evaluation in patients with JIA and ankle involvement [80]. The poor agreement reported by the investigators suggests that clinical assessment of the ankle region is inadequate and supports the use of MSUS in identifying the real site of inflammation for joints with anatomical complexity and numerous adjacent tendons. Furthermore, MSUS may also help in the clinical setting to perform guided injections into joint recesses and peri-tendinous areas [81], enhancing both the efficacy of the procedure and minimizing the rate of side effects.
In childhood, a clinical diagnosis of enthesitis, which is a common feature of the enthesitis-related arthritis (ERA) category of JIA, may be somewhat difficult to make, due to the soft tissue swelling around the bone anatomical landmarks at the enthesis insertion sites. MSUS coupled with PD has been used for detecting enthesis inflammation in children with JIA [82]. In that study, although clinical enthesitis was often associated with PD-MSUS enthesitis, PD signal without any clinical evidence of enthesitis was also documented. These findings raise the question of whether the presence of a PD signal may be an early sign of enthesis involvement in clinically-silent enthesitis. Of interest, in a recent study, MSUS has proven to be superior to a standardized dolorimeter examination in detecting enthesitis in children with ERA [83], further supporting the use of MSUS as an alternative and more objective measure of entheseal inflammation, both at diagnosis and follow-up time.
Conclusions
The imaging approach to JIA has radically changed over the last decade, and modern imaging modalities such as MR and MSUS are increasingly overtaking CR for diagnosis of JIA, assessing its severity and prognosis, monitoring disease course and treatment efficacy. These imaging modalities are still in their infancy and further research focusing on the validation and standardization of these techniques is warranted before considering their use in clinical practice. Due to the peculiarities of the growing skeleton, studies aiming to establish normative data for healthy children are of high priority.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance ••Of major importance
Ravelli A, Martini A. Juvenile idiopathic arthritis. Lancet. 2007;369:767–78.
Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31:390–2.
Martini A. It is time to rethink juvenile idiopathic arthritis classification and nomenclature. Ann Rheum Dis. 2012;71:1437–9.
Oen K, Reed M, Malleson PN, Cabral DA, Petty RE, Rosenberg AM, et al. Radiologic outcome and its relationship to functional disability in juvenile rheumatoid arthritis. J Rheumatol. 2003;30:832–40.
Benjamin CM. Review of UK data on the rheumatic diseases–1. Juvenile chronic arthritis. Br J Rheumatol. 1990;29:231–3.
Lovell DJ, Giannini EH, Reiff A, Cawkwell GD, Silverman ED, Nocton JJ, et al. Etanercept in children with polyarticular juvenile rheumatoid arthritis. Pediatric Rheumatology Collaborative Study Group. N Engl J Med. 2000;342:763–9.
Lovell DJ, Ruperto N, Goodman S, Reiff A, Jung L, Jarosova K, et al. Adalimumab with or without methotrexate in juvenile rheumatoid arthritis. N Engl J Med. 2008;359:810–20.
Ruperto N, Lovell DJ, Quartier P, Paz E, Rubio-Pérez N, Silva CA, et al. Abatacept in children with juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled withdrawal trial. Lancet. 2008;372:383–91.
De Benedetti F, Brunner HI, Ruperto N, Kenwright A, Wright S, Calvo I, et al. Randomized trial of tocilizumab in systemic juvenile idiopathic arthritis. N Engl J Med. 2012;367:2385–95.
Ruperto N, Brunner HI, Quartier P, Constantin T, Wulffraat N, Horneff G, et al. Two randomized trials of canakinumab in systemic juvenile idiopathic arthritis. N Engl J Med. 2012;367:2396–406.
Ravelli A, Martini A. Early predictors of outcome in juvenile idiopathic arthritis. Clin Exp Rheumatol. 2003;21:S89–93.
Oen K. Long-term outcomes and predictors of outcomes for patients with juvenile idiopathic arthritis. Best Pract Res Clin Rheumatol. 2002;16:347–60.
Ravelli A. Toward an understanding of the long-term outcome of juvenile idiopathic arthritis. Clin Exp Rheumatol. 2004;22:271–5.
Suter LG, Fraenkel L, Braithwaite RS. Role of magnetic resonance imaging in the diagnosis and prognosis of rheumatoid arthritis. Arthritis Care Res. 2011;63:675–88.
McQueen FM, Ostergaard M. Imaging in rheumatology: new tools for use in clinical practice in 2012. Preface. Best Pract Res Clin Rheumatol. 2012;26:743–9.
Haavardsholm EA, Østergaard M, Hammer HB, Bøyesen P, Boonen A, van der Heijde D, et al. Monitoring anti-TNFalpha treatment in rheumatoid arthritis: responsiveness of magnetic resonance imaging and ultrasonography of the dominant wrist joint compared with conventional measures of disease activity and structural damage. Ann Rheum Dis. 2009;68:1572–9.
Colebatch AN, Edwards CJ, Østergaard M, van der Heijde D, Balint PV, D'Agostino MA, et al. EULAR recommendations for the use of imaging of the joints in the clinical management of rheumatoid arthritis. Ann Rheum Dis. 2013;72:804–14.
American College of Rheumatology Rheumatoid Arthritis Clinical Trials Task Force Imaging Group and Outcome Measures in Rheumatology Magnetic Resonance Imaging Inflammatory Arthritis Working Group. Review: the utility of magnetic resonance imaging for assessing structural damage in randomized controlled trials in rheumatoid arthritis. Arthritis Rheum. 2013;65:2513–23.
Naredo E, Möller I, Cruz A, Carmona L, Garrido J. Power Doppler ultrasonographic monitoring of response to anti-tumor necrosis factor therapy in patients with rheumatoid arthritis. Arthritis Rheum. 2008;58:2248–56.
Conaghan PG, Emery P, Østergaard M, Keystone EC, Genovese MC, Hsia EC, et al. Assessment by MRI of inflammation and damage in rheumatoid arthritis patients with methotrexate inadequate response receiving golimumab: results of the GO-FORWARD trial. Ann Rheum Dis. 2011;70:1968–74.
Babyn P, Doria AS. Radiologic investigation of rheumatic diseases. Rheum Dis Clin North Am. 2007;33:403–40.
Johnson K. Imaging of juvenile idiopathic arthritis. Pediatr Radiol. 2006;36:743–58.
Lamer S, Sebag GH. MRI and ultrasound in children with juvenile chronic arthritis. Eur J Radiol. 2000;33:85–93.
Jelinek JS, Kransdorf MJ, Utz JA, Berrey Jr BH, Thomson JD, Heekin RD, et al. Imaging of pigmented villonodular synovitis with emphasis on MR imaging. AJR Am J Roentgenol. 1989;152:337–42.
Kim HK, Zbojniewicz AM, Merrow AC, Cheon JE, Kim IO, Emery KH. MR findings of synovial disease in children and young adults: Part 1. Pediatr Radiol. 2011;41:495–511.
Buchmann RF, Jaramillo D. Imaging of articular disorders in children. Radiol Clin North Am. 2004;42:151–68.
Weiss PF, Arabshahi B, Johnson A, Bilaniuk LT, Zarnow D, Cahill AM, et al. High prevalence of temporomandibular joint arthritis at disease onset in children with juvenile idiopathic arthritis, as detected by magnetic resonance imaging but not by ultrasound. Arthritis Rheum. 2008;58:1189–96.
Müller L, Kellenberger CJ, Cannizzaro E, Ettlin D, Schraner T, Bolt IB, et al. Early diagnosis of temporomandibular joint involvement in juvenile idiopathic arthritis: a pilot study comparing clinical examination and ultrasound to magnetic resonance imaging. Rheumatology. 2009;48:680–5.
Meyers AB, Laor T. Magnetic resonance imaging of the temporomandibular joint in children with juvenile idiopathic arthritis. Pediatr Radiol. 2013;43:1632–41.
Cannizzaro E, Schroeder S, Müller LM, Kellenberger CJ, Saurenmann RK. Temporomandibular joint involvement in children with juvenile idiopathic arthritis. J Rheumatol. 2011;38:510–5.
Pedersen TK, Küseler A, Gelineck J, Herlin T. A prospective study of magnetic resonance and radiographic imaging in relation to symptoms and clinical findings of the temporomandibular joint in children with juvenile idiopathic arthritis. J Rheumatol. 2008;35:1668–75.
Argyropoulou MI, Fanis SL, Xenakis T, Efremidis SC, Siamopoulou A. The role of MRI in the evaluation of hip joint disease in clinical subtypes of juvenile idiopathic arthritis. Br J Radiol. 2002;75:229–33.
Nistala K, Babar J, Johnson K, Campbell-Stokes P, Foster K, Ryder C, et al. Clinical assessment and core outcome variables are poor predictors of hip arthritis diagnosed by MRI in juvenile idiopathic arthritis. Rheumatology. 2007;46:699–702.
Oren B, Oren H, Osma E, Cevik N. Juvenile rheumatoid arthritis: cervical spine involvement and MRI in early diagnosis. Turk J Pediatr. 1996;38:189–94.
Malattia C, Damasio MB, Pistorio A, Ioseliani M, Vilca I, Valle M, et al. Development and preliminary validation of a paediatric-targeted MRI scoring system for the assessment of disease activity and damage in juvenile idiopathic arthritis. Ann Rheum Dis. 2011;70:440–6.
Damasio MB, Malattia C. Tanturri de Horatio L, Mattiuz C, Pistorio A, Bracaglia C, et al. MRI of the wrist in juvenile idiopathic arthritis: proposal of a paediatric synovitis score by a consensus of an international working group. Results of a multicentre reliability study. Pediatr Radiol. 2012;42:1047–55.
Tanturri de Horatio L, Damasio MB, Barbuti D, Bracaglia C, Lambot-Juhan K, Boavida P, et al. MRI assessment of bone marrow in children with juvenile idiopathic arthritis: intra- and inter-observer variability. Pediatr Radiol. 2012;42:714–20.
Hemke R, van Rossum MA, van Veenendaal M, Terra MP, Deurloo EE, de Jonge MC, et al. Reliability and responsiveness of the Juvenile Arthritis MRI Scoring (JAMRIS) system for the knee. Eur Radiol. 2013;23:1075–83.
Malattia C, Consolaro A, Pederzoli S, Madeo A, Pistorio A, Mazzoni M, et al. MRI versus conventional measures of disease activity and structural damage in evaluating treatment efficacy in juvenile idiopathic arthritis. Ann Rheum Dis. 2013;72:363–8. This study is the first to show that MRI represents a promising imaging biomarker for measuring therapeutic response in JIA.
Malattia C, Damasio MB, Basso C, Verri A, Magnaguagno F, Viola S, et al. Dynamic contrast-enhanced magnetic resonance imaging in the assessment of disease activity in patients with juvenile idiopathic arthritis. Rheumatology. 2010;49:178–85.
Workie DW, Dardzinski BJ, Graham TB, Laor T, Bommer WA, O'Brien KJ. Quantification of dynamic contrast-enhanced MR imaging of the knee in children with juvenile rheumatoid arthritis based on pharmacokinetic modeling. Magn Reson Imaging. 2004;22:1201–10.
Workie DW, Graham TB, Laor T, Rajagopal A, O'Brien KJ, Bommer WA, et al. Quantitative MR characterization of disease activity in the knee in children with juvenile idiopathic arthritis: a longitudinal pilot study. Pediatr Radiol. 2007;37:535–43.
Malattia C, Damasio MB, Basso C, Santoro M, Verri A, Pederzoli S, et al. Novel automated system for magnetic resonance imaging quantification of the inflamed synovial membrane volume in patients with juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). 2012;64:1657–64.
Wallace CA, Ruperto N, Giannini E. Childhood Arthritis and Rheumatology Research Alliance; Pediatric Rheumatology International Trials Organization; Pediatric Rheumatology Collaborative Study Group. Preliminary criteria for clinical remission for select categories of juvenile idiopathic arthritis. J Rheumatol. 2004;31:2290–4.
Ruperto N, Giannini EH, Pistorio A, Brunner HI, Martini A, Lovell DJ. Is it time to move to active comparator trials in juvenile idiopathic arthritis?: a review of current study designs. Arthritis Rheum. 2010;62:3131–9.
Brown A, Hirsch R, Laor T, Hannon MJ, Levesque MC, Starz T, et al. Do patients with juvenile idiopathic arthritis in clinical remission have evidence of persistent inflammation on 3T magnetic resonance imaging? Arthritis Care Res (Hoboken). 2012;64:1846–54.
Brown AK, Quinn MA, Karim Z, Conaghan PG, Peterfy CG, Hensor E, et al. Presence of significant synovitis in rheumatoid arthritis patients with disease-modifying antirheumatic drug-induced clinical remission: evidence from an imaging study may explain structural progression. Arthritis Rheum. 2006;54:3761–73.
McQueen FM, Benton N, Perry D, Crabbe J, Robinson E, Yeoman S, et al. Bone edema scored on magnetic resonance imaging scans of the dominant carpus at presentation predicts radiographic joint damage of the hands and feet six years later in patients with rheumatoid arthritis. Arthritis Rheum. 2003;48:1814–27.
Benton N, Stewart N, Crabbe J, Robinson E, Yeoman S, McQueen FM. MRI of the wrist in early rheumatoid arthritis can be used to predict functional outcome at 6 years. Ann Rheum Dis. 2004;63:555–61.
Hetland ML, Ejbjerg B, Hørslev-Petersen K, Jacobsen S, Vestergaard A, Jurik AG, et al. MRI bone oedema is the strongest predictor of subsequent radiographic progression in early rheumatoid arthritis. Results from a 2-year randomised controlled trial (CIMESTRA). Ann Rheum Dis. 2009;68:384–90.
Dalbeth N, Smith T, Gray S, Doyle A, Antill P, Lobo M, et al. Cellular characterisation of magnetic resonance imaging bone oedema in rheumatoid arthritis; implications for pathogenesis of erosive disease. Ann Rheum Dis. 2009;68:279–82.
Müller LS, Avenarius D, Damasio B, Eldevik OP, Malattia C, Lambot-Juhan K, et al. The paediatric wrist revisited: redefining MR findings in healthy children. Ann Rheum Dis. 2011;70:605–10. The authors highlight the peculiarities of the growing skeleton and the need to include age-matched healthy subjects in imaging studies on JIA.
Shabshin N, Schweitzer ME. Age dependent T2 changes of bone marrow in pediatric wrist MRI. Skeletal Radiol. 2009;38:1163–8.
Ejbjerg B, Narvestad E, Rostrup E, Szkudlarek M, Jacobsen S, Thomsen HS, et al. Magnetic resonance imaging of wrist and finger joints in healthy subjects occasionally shows changes resembling erosions and synovitis as seen in rheumatoid arthritis. Arthritis Rheum. 2004;50:1097–106.
Olech E, Crues 3rd JV, Yocum DE, Merrill JT. Bone marrow edema is the most specific finding for rheumatoid arthritis (RA) on noncontrast magnetic resonance imaging of the hands and wrists: a comparison of patients with RA and healthy controls. J Rheumatol. 2010;3:265–74.
Hoving JL, Buchbinder R, Hall S, et al. A comparison of magnetic resonance imaging, sonography, and radiography of the hand in patients with early rheumatoid arthritis. J Rheumatol. 2004;31:663–75.
Østergaard M, Hansen M, Stoltenberg M, et al. New radiographic bone erosions in the wrists of patients with rheumatoid arthritis are detectable with magnetic resonance imaging a median of 2 years earlier. Arthritis Rheum. 2003;48:2128–31.
Malattia C, Damasio MB, Magnaguagno F, Pistorio A, Valle M, Martinoli C, et al. Magnetic resonance imaging, ultrasonography, and conventional radiography in the assessment of bone erosions in juvenile idiopathic arthritis. Arthritis Rheum. 2008;59:1764–72.
Ording Muller LS, Boavida P, Avenarius D, Damasio B, Eldevik OP, Malattia C, et al. MRI of the wrist in juvenile idiopathic arthritis: erosions or normal variants? A prospective case-control study. Pediatr Radiol. 2013;43:785–95.
Rossi F, Di Dia F, Galipo O, Pistorio A, Valle M, Magni-Manzoni S, et al. Use of the Sharp and Larsen scoring methods in the assessment of radiographic progression in juvenile idiopathic arthritis. Arthritis Rheum. 2006;55:717–23.
Reed MH, Wilmot DM. The radiology of juvenile rheumatoid arthritis: a review of the English language literature [review]. J Rheumatol Suppl. 1991;31:2–22.
Cohen PA, Job-Deslandre CH, Lalande G, Adamsbaum C. Overview of the radiology of juvenile idiopathic arthritis (JIA) [review]. Eur J Radiol. 2000;33:94–101.
Ho-Fung VM, Jaramillo D. Cartilage imaging in children: current indications, magnetic resonance imaging techniques, and imaging findings. Radiol Clin North Am. 2013;51:689–702.
Kight AC, Dardzinski BJ, Laor T, Graham TB. Magnetic resonance imaging evaluation of the effects of juvenile rheumatoid arthritis on distal femoral weight-bearing cartilage. Arthritis Rheum. 2004;50:901–5.
Daher RJ, Chahine NO, Greenberg AS, Sgaglione NA, Grande DA. New methods to diagnose and treat cartilage degeneration. Nat Rev Rheumatol. 2009;5:599–607.
Miese F, Buchbender C, Scherer A, Wittsack HJ, Specker C, Schneider M, et al. Molecular imaging of cartilage damage of finger joints in early rheumatoid arthritis with delayed gadolinium-enhanced magnetic resonance imaging. Arthritis Rheum. 2012;64:394–9.
Buchbender C, Scherer A, Kröpil P, Körbl B, Quentin M, Reichelt DC, et al. Cartilage quality in rheumatoid arthritis: comparison of T2* mapping, native T1 mapping, dGEMRIC, ΔR1 and value of pre-contrast imaging. Skeletal Radiol. 2012;41:685–92.
Magni-Manzoni S, Malattia C, Lanni S, Ravelli A. Advances and challenges in imaging in juvenile idiopathic arthritis. Nat Rev Rheumatol. 2012;8:329–36. This review provides a summary of the current information on conventional radiography, ultrasonography and MRI in JIA and highlights the advantages and limitations of each imaging modality.
Lanni S, Wood M, Ravelli A, Magni Manzoni S, Emery P, Wakefield RJ. Towards a role of ultrasound in children with juvenile idiopathic arthritis. Rheumatology (Oxford). 2013;52:413–20. This review considers the most important studies regarding the use of MSUS in JIA and points out the current major aspects to be developed in further studies.
Collado P, Jousse-Joulin S, Alcalde M, Naredo E, D'Agostino MA. Is ultrasound a validated imaging tool for the diagnosis and management of synovitis in juvenile idiopathic arthritis? A systematic literature review. Arthritis Care Res (Hoboken). 2012;64:1011–9. This systematic literature review shows the utility of MSUS for detecting synovitis in JIA and its superiority to clinical examination. However, the authors also highlight the need for further studies in order to demonstrate MSUS reliability and responsiveness in JIA and to validate the technique as an outcome tool in JIA.
Spannow AH, Pfeiffer-Jensen M, Andersen NT, Stenbøg E, Herlin T. Inter -and intraobserver variation of ultrasonographic cartilage thickness assessments in small and large joints in healthy children. Pediatr Rheumatol Online J. 2009;4:7–12.
Spannow AH, Stenboeg E, Pfeiffer-Jensen M, Fiirgaard B, Haislund M, Ostergaard M, et al. Ultrasound and MRI measurements of joint cartilage in healthy children: a validation study. Ultraschall Med. 2011;32 Suppl 1:S110–6.
Spannow AH, Pfeiffer-Jensen M, Andersen NT, Herlin T, Stenbøg E. Ultrasonographic measurements of joint cartilage thickness in healthy children: age- and sex-related standard reference values. J Rheumatol. 2010;37:2595–601.
Pradsgaard DØ, Spannow AH, Heuck C, Herlin T. Decreased cartilage thickness in juvenile idiopathic arthritis assessed by ultrasonography. J Rheumatol. 2013;40:1596–603.
Magni-Manzoni S, Epis O, Ravelli A, Klersy C, Veisconti C, Lanni S, et al. Comparison of clinical versus ultrasound-determined synovitis in juvenile idiopathic arthritis. Arthritis Rheum. 2009;61:1497–504.
Haslam KE, McCann LJ, Wyatt S, Wakefield RJ. The detection of subclinical synovitis by ultrasound in oligoarticular juvenile idiopathic arthritis: a pilot study. Rheumatology (Oxford). 2010;49:123–7.
Breton S, Jousse-Joulin S, Cangemi C, de Parscau L, Colin D, Bressolette L, et al. Comparison of clinical and ultrasonographic evaluations for peripheral synovitis in juvenile idiopathic arthritis. Semin Arthritis Rheum. 2011;41:272–8.
Scirè CA, Montecucco C, Codullo V, Epis O, Todoerti M, Caporali R. Ultrasonographic evaluation of joint involvement in early rheumatoid arthritis in clinical remission: power Doppler signal predicts short-term relapse. Rheumatology (Oxford). 2009;48:1092–7.
Magni-Manzoni S, Scirè CA, Ravelli A, Klersy C, Rossi S, Muratore V, et al. Ultrasound-detected synovial abnormalities are frequent in clinically inactive juvenile idiopathic arthritis, but do not predict a flare of synovitis. Ann Rheum Dis. 2013;72:223–8. This study shows that the presence of ultrasound pathology does not predict an early flare of synovitis in the affected joints of children with JIA, which is of interest as it contrasts with the observation in adults with RA.
Pascoli L, Wright S, McAllister C, Rooney M. Prospective evaluation of clinical and ultrasound findings in ankle disease in juvenile idiopathic arthritis: importance of ankle ultrasound. J Rheumatol. 2010;37:2409–14.
Laurell L, Court-Payen M, Nielsen S, Zak M, Boesen M, Fasth A. Ultrasonography and color Doppler in juvenile idiopathic arthritis: diagnosis and follow-up of ultrasound-guided steroid injection in the ankle region. A descriptive interventional study. Pediatr Rheumatol Online J. 2011;9:4.
Jousse-Joulin S, Breton S, Cangemi C, Fenoll B, Bressolette L, de Parscau L, et al. Ultrasonography for detecting enthesitis in juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). 2011;63:849–55.
Weiss PF, Chauvin NA, Klink AJ, Localio R, Feudtner C, Jaramillo D, et al. Detection of enthesitis in children with Enthesitis-related arthritis: Dolorimeter examination compared to ultrasonography. Arthritis Rheum. 2014;66:218–27.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
The GASLINI Hospital (the public hospital at which Alberto Martini works as a full-time employee) has received contributions to support the research activities of the network of PRINTO (www.printo.it) from Bristol-Myers Squibb, Centocor Research & Development, GlaxoSmithKline, Novartis, Pfizer, Roche, Sanofi Aventis, and Schwarz Biosciences GmbH.
Alberto Martini has served as a consultant for Abbott Laboratories, Boehringer, Italfarmaco, Bristol-Myers Squibb, MedImmune, Novartis, NovoNordisk, Sanofi Aventis, Roche, Servier, and Pfizer; has received grant support from Bristol-Myers Squibb, Centocor Research & Development, GlaxoSmithKline, Novartis, Pfizer, Roche, Sanofi Aventis, and Schwarz Biosciences GmbH; and has served on speakers bureaus and had travel/accommodations expenses covered/reimbursed by Abbott Laboratories, Bristol-Myers Squibb, Astellas, Boehringer, Italfarmaco, MedImmune, Novartis, NovoNordisk, Pfizer, Sanofi Aventis, Roche, and Servier.
Stefano Lanni and Clara Malattia declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Imaging
Rights and permissions
About this article
Cite this article
Lanni, S., Martini, A. & Malattia, C. Heading Toward a Modern Imaging Approach in Juvenile Idiopathic Arthritis. Curr Rheumatol Rep 16, 416 (2014). https://doi.org/10.1007/s11926-014-0416-9
Published:
DOI: https://doi.org/10.1007/s11926-014-0416-9