Abstract
Objectives
To assess the reliability and responsiveness of a new Juvenile Arthritis MRI Scoring (JAMRIS) system for evaluating disease activity of the knee.
Methods
Twenty-five juvenile idiopathic arthritis (JIA) patients with clinical knee involvement were studied using open-bore 1-T MRI. MRI features of synovial hypertrophy, bone marrow changes, cartilage lesions and bone erosions were independently scored by five readers using the JAMRIS system. In addition, the JAMRIS system was determined to be a follow-up parameter by two readers to evaluate the response to therapy in 15 consecutive JIA patients.
Results
Inter-reader (ICCs 0.86–0.95) and intra-reader reliability (ICCs 0.92–1.00) for the scoring of JAMRIS features was good. Reliability of the actual scores and changes in scores over time was good for all items: ICCs 0.89–1.00, 0.87–1.00, respectively. Concerning therapy response, the mean synovial hypertrophy scores decreased significantly (mean 1.1 point; P < 0.001, SRM = −0.65). No change was observed with respect to bone marrow change, cartilage lesion and bone erosion scores.
Conclusions
The JAMRIS proved to be a simple and highly reliable assessment score in the evaluation of JIA disease activity of the knee. The JAMRIS system may serve as an objective and accurate outcome measure in future research and clinical trials.
Key Points
• MRI is increasingly used to diagnose and assess juvenile idiopathic arthritis.
• A simple and reliable scoring method would help monitor progress and research.
• The Juvenile Arthritis MRI Scoring (JAMRIS) system provides reliable objective measures.
• JAMRIS evaluates synovial hypertrophy, bone marrow changes, cartilage lesions and bone erosions.
• The JAMRIS system can detect therapeutic response and should help future research.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Juvenile idiopathic arthritis (JIA) is the most common autoinflammatory musculoskeletal disease in childhood, with a prevalence that varies between 16 and 150 per 100,000 [1]. JIA is not a single disease, but a term that encompasses all forms of arthritis of unknown aetiology and pathophysiology that begin before the age of 16 years and persist for more than 6 weeks [2]. It is characterised by prolonged synovial inflammation that can lead to the destruction of joints, pain and loss of function [1].
As early therapeutic intervention improves long-term outcome, objective and accurate measures in the assessment of disease activity are needed for the evaluation of individual responses to therapy and the general efficacy of treatment in JIA [3, 4]. Physical examination, even by an experienced observer, has only limited reliability [5, 6]. Conventional radiography is insensitive in detecting soft tissue changes such as synovitis, which is one of the most critical hallmarks of disease activity in JIA as well as in detecting the earliest stages of persistent erosive changes [7]. Within the past 10 years, the use of magnetic resonance imaging (MRI) and advances in MRI techniques have substantially improved the evaluation of joint abnormalities in JIA patients [8, 9]. Currently, MRI is considered to be the most suitable imaging technique in this respect. Although MRI has been evaluated for the standardised evaluation of wrist involvement in both JIA and rheumatoid arthritis patients [10–12], standardised measures for data acquisition and interpretation are currently not available regarding the evaluation of the disease status of the knee, as the most commonly affected joint in JIA [9]. Hence, this technique is under-utilised in research and clinical trials. Part of the reason for the under-utilisation of MRI as an outcome measure in clinical trials in JIA relates to the lack of standardisation of protocols and scales for data acquisition and interpretation, respectively, in the literature. In addition, standardised knowledge of the normal joint of interest is required as the developmental growth process of joints in paediatric patients should be taken into account and not be mistaken for a joint abnormality [9, 13]. The development of an MRI outcome measure for the assessment of disease status in JIA is important and therefore of specific interest in the outcome measures in the rheumatology (OMERACT) group.
The utility of MRI in the assessment of JIA joint abnormalities is limited by the fact that there is no generally accepted, easy-to-use MRI scoring system for the assessment of the disease status in JIA. We set out to design a new scoring system. Because the evaluation and the weighing of certain pathological MRI features are lacking, we realised that the initial score should be broadly inclusive [14]. During the current study special attention was given to the refinement of the initial system in order to develop an easy-to-use scoring system with good inter- and intra-reader reliability. The aim of our study, therefore, is to assess the reliability and responsiveness of the newly developed Juvenile Arthritis MRI Scoring (JAMRIS) system for evaluating the disease activity of the most commonly affected joint in JIA (i.e. the knee).
Materials and methods
Patients and MRI protocol
A collaborative programme between two tertiary paediatric rheumatology centres was established in 2007, incorporating paediatric rheumatologists and radiologists who were experienced in the research field of imaging in JIA. Patients visited one of the outpatient clinics of these two centres. All patients fulfilled the International League of Associations for Rheumatology (ILAR) criteria for JIA [2]. The indication for MRI was evaluation of disease activity before initiation or a proposed change in treatment. Exclusion criteria were a history of intra-articular corticosteroid injection within the last 6 months, the need for anaesthesia during the MRI examination and general contraindications for MRI. The institutional review board waived informed consent for the current study because the cases were derived from retrospective review of existing MRI examinations in the JIA study database, in which written informed consent had been obtained from at least one parent of each child.
Prospectively collected MRI data sets from two substudies were integrated in this report. In substudy 1, the inter- and intra-observer reliabilities were assessed. MR images for the assessment of reliability were randomly selected from MRIs of clinically active knees performed between December 2008 and February 2011. In substudy 2, we evaluated the responsiveness of the JAMRIS system. MR image sets for both substudies were obtained using an open-bore 1.0-T magnet (Panorama HFO, Philips Medical Systems, Best, The Netherlands). No sedation was used and the children were placed in the supine position with the knee joint centrally in the magnetic field using a dedicated knee coil. MRI in paediatric JIA patients proved to be feasible using an open-bore system [14], and by using a dedicated knee coil an adequate signal-to-noise ratio was obtained. Contrast-enhanced MRI of the clinically most involved knee (target joint) was performed. If there were no differences in clinical activity between the knees, the right knee was considered to be the target joint. To provide an optimal discrimination between enhancing synovium and joint effusion, post-contrast images were obtained in the early phase (<5 min) after intravenous injection of Gd (0.1 mg per kilogram of body weight, gadopentetate dimeglumine, Schering, Berlin, Germany) [15]. See Table 1 for the acquired sequences.
Substudy 1: reliability
To evaluate the inter-observer reliability image sets of 25 JIA patients [68 % female, mean age 13.7 years (SD 2.8, range 8.2–16.9 years)] were scored independently by five readers, including one reader who was not affiliated with either of the two centres. Patients had a median disease duration of 3.2 years (IQR 1.1–7.2 years). Frequency of JIA subtypes was as follows: seven (28 %) persistent oligoarthritis, four (16 %) extended oligoarthritis, ten (40 %) polyarthritis, two (8 %) psoriatic arthritis and two (8 %) enthesitis-related arthritis. Readers comprised two musculoskeletal radiologists (17, and 10 years of experience), one paediatric radiologist (4 years of experience), one radiology musculoskeletal fellow (4 years of experience) and a radiology trainee (4 years of experience). All readers were blinded to clinical history, including the duration, extent and severity of the symptoms. MR images were scored in accordance with the scoring systems as described below (JAMRIS). To analyse the intra-reader reliability, data sets of these 25 patients were evaluated twice within an interval of 6 months by two readers. To assess the feasibility of JAMRIS the duration of the scoring sessions was timed.
Substudy 2: responsiveness
To evaluate the JAMRIS system as a follow-up parameter, two readers independently evaluated the MR images of 15 consecutive JIA patients [53 % female, mean age 12.4 years (SD 3.2, range 8.4–15.3 years)] with clinically active disease at baseline and who showed clinical improvement according to the American College of Rheumatology (ACR) Paediatric 50 criteria during follow-up [16]. The JIA patients selected for substudy 2 had a median disease duration of 1.9 years (IQR 0.5–5.0 years). Frequency of JIA subtypes was as follows: three (20 %) persistent oligoarthritis, two (13 %) extended oligoarthritis, seven (47 %) polyarthritis, one (7 %) psoriatic arthritis, one (7 %) enthesitis-related arthritis and one (7 %) undifferentiated JIA. For this longitudinal exercise, images were read blinded to chronological order.
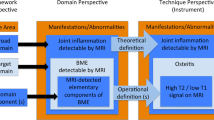
Juvenile arthritis MRI scoring system for the knee
The Juvenile Arthritis MRI Scoring (JAMRIS) system for the knee comprises four MRI features: one soft-tissue item (synovial hypertrophy), two bone items (bone marrow changes, bone erosions) and one cartilage item (cartilage lesions). The JAMRIS system therefore includes two features assessing early inflammatory changes (synovial hypertrophy, bone marrow changes) and two features focusing on late destructive changes (cartilage lesions, bone erosions). An extensive overview of the JAMRIS system is depicted in Fig. 1. An easy-to-use description of the scoring features and the anatomic delineation of the JAMRIS scoring regions are depicted in Supplementary file 1.
Synovial hypertrophy
Synovial hypertrophy was defined as enhancing thickened synovium (>2 mm). The inflamed synovial membrane is thickened, irregular and can have wavy outlines. The signal intensity of this hypertrophic synovial membrane is low to intermediate on T1-weighted images and high on T2-weighted images. Enhancement (signal intensity increase) was judged by comparison between T1-weighted images obtained before and after intravenous gadolinium contrast medium administration (adapted from Østergaard et al. [11]).
The presence of synovial hypertrophy was evaluated at six sites of the knee joint: patellofemoral, suprapatellar recesses, infrapatellar fat pad, adjacent to the cruciate ligaments (ACL and PCL), and adjacent to the medial and lateral posterior condyle. Synovial thickness was scored semi-quantitatively based on the maximal thickness of any slice at each site as follows: grade 0 if <2 mm, grade 1 if ≥2–4 mm and grade 2 if >4 mm, resulting in a minimum score of 0 and a maximum score of 12 (Fig. 2) (adapted from Guermazi et al. [17]).
Patellofemoral synovial hypertrophy. Axial fat-saturated contrast-enhanced T1-weighted images obtained in (a) a 13-year-old girl with a maximal synovial thickness of 0.9 mm resulting in a synovial hypertrophy score of 0 (<2 mm). b An 11-year-old boy with a maximal synovial thickness of 2.8 mm resulting in a synovial hypertrophy score of 1 (2–4 mm). c A 17-year-old girl with a maximal synovial thickness of 6.6 mm resulting in a synovial hypertrophy score of 2 (>4 mm)
Bone marrow changes suggestive of bone marrow oedema
Bone marrow changes suggestive of bone marrow oedema were defined as lesions within the trabecular bone, with ill-defined margins and high signal intensity on T2-weighted fat-saturated images and low signal intensity on T1-weighted images (adapted from Østergaard et al. [11]).
The presence of bone marrow changes was scored in eight anatomical regions. The patella was divided into two regions, the medial and lateral patella on the axial view. The femur was divided into four anatomical regions: the medial and lateral condyle, and the medial and lateral weight-bearing femur. The tibia was divided into two regions: the medial and lateral tibial plateau. Bone marrow changes suggestive of bone marrow oedema were scored semi-quantitatively based on the subjectively estimated percentage of involved bone volume at each site as follows: grade 0, none; grade 1, <10 % of the whole bone volume; grade 2, ≥10–25 % of the whole bone volume; grade 3, >25 % of the whole bone volume, resulting in a minimum score of 0 and a maximum score of 24 (Fig. 3) (adapted from Hunter et al. [18]).
Bone marrow changes suggestive of bone marrow oedema in the lateral condyle of the femur. Coronal fat-saturated T2-weighted images obtained in (a) a 15-year old girl with no bone marrow changes resulting in a bone marrow change score of 0. b A 12-year-old girl with bone marrow changes scored as grade 1 (<10 % of whole bone volume). c An 11-year-old boy with bone marrow changes suggestive of bone marrow oedema scored as grade 2 (10–25 % of the whole bone volume). d A 14-year-old boy with bone marrow changes scored as grade 3 (>25 % of whole bone volume)
Cartilage lesions
The cartilage was scored for the presence of lesions (superficial loss and/or thinning, or deep loss to the subchondral bone, adapted from Gylys-Morin et al. [19]) in the previously mentioned eight anatomical regions: the medial and lateral patella, the medial and lateral condyles, the medial and lateral weight-bearing femur, and the medial and lateral tibial plateau. The cartilage lesions were scored semi-quantitatively based on the subjectively estimated percentage of involved surface area at each site as follows: grade 0, none; grade 1, <10 % of the region of the cartilage surface area; grade 2, ≥10–25 % of the region of the cartilage surface area; grade 3, >25 % of the region of the cartilage surface area, resulting in a minimum score of 0 and a maximum score of 24 (adapted from Hunter et al. [18]).
Bone erosions
A bone erosion was defined as a sharply marginated bone lesion with correct juxta-articular localisation, typical signal characteristics and visible in two planes with a cortical break in at least one plane [11]. On T1-weighted images there is a loss of the normal low signal intensity of cortical bone and loss of the normal high signal intensity of trabecular bone (adapted from Østergaard et al. [11]).
The presence of bone erosions was scored in the eight anatomical regions: medial and lateral patella, medial and lateral condyles, medial and lateral weight-bearing femur, and medial and lateral tibial plateau. The bone erosions were scored semi-quantitatively based on the subjectively estimated percentage of involved bone volume at each site as follows: grade 0, none; grade 1, <10 % of the whole bone volume; grade 2, ≥10–25 % of the whole bone volume; grade 3, >25 % of the whole bone volume, resulting in a minimum score of 0 and a maximum score of 24 (adapted from Hunter et al. [18]).
Statistics
Descriptive statistics were reported in terms of percentages, means, ranges and standard deviations (SD). The Kruskal-Wallis test was used to analyse differences between groups/scores. The Wilcoxon signed ranks test was used to analyse differences within groups. Both tests assumed a two-tailed probability, and a P value of less than 0.05 indicated a significant difference. Because the sum of scores was considered to be continuous data, the single measure intraclass correlation coefficient (ICC) was used to analyse inter- and intra-reader reliability and was classified as follows: ICC <0.40 = poor, ≥0.40–0.60 = moderate, >0.60–0.80 = substantial and >0.80 = good reliability. To assess the responsiveness of the JAMRIS system, the differences between time point A and time point B were used for calculating the standardised response mean (SRM = mean change of the score/SD change of the score) and was classified as follows: SRM <0.40 = poor, ≥0.40–0.60 = moderate, >0.60–0.80 = substantial and >0.80 = good effect [20]. All data were analysed by using SPSS version 16.0 (SPSS, Chicago, IL, USA). Statistical analyses were performed in close collaboration with a clinical epidemiologist.
Results
Inter-reader reliability
When the scores of the five readers were compared, there were no significant differences for synovial hypertrophy (P = 0.930), bone marrow changes suggestive of bone marrow oedema (P = 0.782), cartilage lesion (P = 0.937) or bone erosion scores (P = 0.943) (Table 2). Consequently, inter-reader reliability was good for all features (ICC 0.86–0.95) (Table 2). ICCs for synovial hypertrophy 0.95 (95 % CI 0.91–0.97), bone marrow changes 0.86 (95 % CI 0.77–0.93), cartilage lesions 0.91 (95 % CI 0.85–0.96) and bone erosions 0.88 (95 % CI 0.80–0.94) were good.
Intra-reader reliability
Intra-reader reliability was good for all scored items. Single measure ICCs for both readers were as follows: synovial hypertrophy 0.99 (95 % CI 0.98–1.00) and 1.00 (95 % CI 0.99–1.00), bone marrow changes 0.96 (95 % CI 0.93–0.98) and 0.97 (95 % CI 0.93–0.99), cartilage lesions 0.99 (95 % CI 0.97–0.99) and 0.98 (95 % CI 0.96–0.99), and bone erosions 0.92 (95 % CI 0.83–0.96) and 1.00 (95 % CI 1.00–1.00), respectively.
Feasibility
The scoring took an acceptable median of 6.6 (SD 1.5) minutes per patient, indicating good feasibility of the JAMRIS system. The scoring duration ranged from 4.8 min per patient for reader 2 to 8.4 min per patients for reader 3.
Responsiveness
All JIA patients were treated for 12 months or longer with a disease-modifying antirheumatic drug (DMARD) and/or a TNF-α blocker. Actual scores were obtained at time point A and again at time point B after a median follow-up time of 1.4 years (IQR 1.2–1.7) (Table 3). A statistically significant decrease concerning synovial hypertrophy scores (mean 1.1) was observed between time points (P < 0.001). The responsiveness of the JAMRIS system showed a substantial effect regarding change in synovial hypertrophy scores (SRM = −0.65). No change was seen in bone marrow change (SRM = −0.15), cartilage lesion and bone erosion scores. Regarding the inter-reader reliability of the status scores (time points A and B), the ICCs were good for all items: 0.89–1.00 and 0.87–1.00, respectively. ICCs for the status scores (time points A and B) were as follows: synovial hypertrophy 0.96 (95 % CI 0.90–0.99), 0.92 (95 % CI 0.76–0.97); bone marrow changes 0.89 (95 % CI 0.66–0.96), 0.87 (95 % CI 0.60–0.96); cartilage lesions 1.00 (95 % CI 1.00–1.00), 1.00 (95 % CI 1.00–1.00); bone erosions 1.00 (95 % CI 1.00–1.00), 1.00 (95 % CI 1.00–1.00), respectively.
Discussion
This article describes the developmental process and the reliability of a standardised Juvenile Arthritis MRI Scoring (JAMRIS) system for the knee. Our study shows good reliability in terms of ICC for the different items scored, which supports the applicability of JAMRIS as an objective, simple and accurate outcome measure in future research and clinical trials in the evaluation of JIA disease status of the knee.
Since the development of highly effective therapies for rheumatic diseases, the main goal of treatment consists of complete suppression of joint inflammation to prevent destructive changes. Therefore, outcome measures in clinical trials should comprise sensitive and reliable measures of inflammation [9]. Contrast-enhanced MRI is the most suitable imaging technique to date for serving this purpose by accurately detecting synovial hypertrophy, one of the most critical hallmarks of disease activity in JIA. Furthermore, it is the only technique able to visualise bone marrow changes suggestive of bone marrow oedema [19]. In rheumatoid arthritis it has been shown that both synovial hypertrophy and bone marrow oedema are key predictors of early erosive joint damage. Currently, these are considered the most sensitive MRI features for monitoring disease activity [21–24]. Prolonged disease activity may ultimately lead to cartilage and bone damage, which are responsible for most disability in JIA [25, 26]. Apart from synovial hypertrophy and bone marrow oedema, cartilage lesions and bone erosions were also included in JAMRIS to monitor the presence and deterioration of damage to the knee.
The inter-reader reliability of the scored items was good for all MRI features (ICCs 0.86–0.95). This is a promising and strong characteristic of the JAMRIS system because readers had variable levels of experience (from 4 to 17 years of experience in musculoskeletal radiology) in the evaluation of MR images of JIA patients and the MRI data sets were scored completely separately. The reliability scores for the knee are comparable to values seen in reliability studies regarding JIA and rheumatoid arthritis MRI scores of the wrist [10, 27]. In the development of the JAMRIS system, we primarily focused on early stage JIA disease activity. The JAMRIS scale for bone marrow changes, cartilage lesions and bone erosions affecting <25 % of the surface area/bone volume is, therefore, more sensitive to change compared to the rough division used in current JIA and rheumatoid arthritis MRI scores of the wrist [10, 11]. Our data regarding the JAMRIS system as a follow-up parameter suggest that the scoring system is able to measure change in articular disease activity in longitudinal settings. High reliability and sensitivity to change were observed for synovial hypertrophy (ICC = 0.92; SRM = −0.65). However, it should be noted that—contrary to synovial hypertrophy—there was no such absolute change in bone marrow, cartilage lesion and bone erosion scores between time points. The presence of bone marrow changes is an important predictor of early erosive joint damage in rheumatoid arthritis [21, 22], though its prognostic value in JIA has never been assessed. The clinical relevance of the presence of bone marrow changes in paediatric JIA patients is therefore unclear and might be unrelated to JIA disease activity but part of the joint development or the patient’s mobility (sports) instead.
There is a degree of histopathological variation of the synovial membrane in knees of patients with active arthritis [28]. Further, it is common practice to evaluate not one but several regions of the joint in the most accepted scoring systems concerning the evaluation of joint abnormalities [11, 18, 29–31]. The knee was divided accordingly into six or eight easy-to-use regions for the evaluation of inflammation and damage. Although synovial volume has greater sensitivity than maximal synovial thickness in the assessment of clinical synovitis, synovial thickness is more practical to use because it can be easily measured, requires no post-processing and correlates well with synovial volume [19]. Therefore, the enhancing synovial membrane was scored semi-quantitatively based on the maximal thickness in millimetres in any slice at each site to ensure that the JAMRIS system would be a sensitive yet reader-friendly measurement tool.
Several advanced MRI techniques are available for the evaluation of inflammatory and destructive changes in JIA, including dynamic contrast-enhanced MRI (DCE-MRI), T2-mapping, diffusion-weighted MRI (DWI) and delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) [32, 33]. Currently, these imaging techniques are used particularly in the context of research and to a lesser extent in daily practice. Moreover, for the interpretation and post-processing of these images specialised knowledge is needed. At this moment, advanced imaging techniques are, therefore, not valuable for use in an easy-to-use scoring method such as the JAMRIS system.
Radiography of bilateral joints is considered to be of great importance in the assessment of damage and growth disturbances in both JIA and RA [26, 30]. MRI of both knees is feasible in paediatric JIA patients [14]. Current limiting factors in the MRI examination of bilateral joints include the reduction of resolution when both joints undergo imaging together or an increase in imaging time when joints undergo imaging separately. Moreover, only one joint can undergo imaging with contrast enhancement. Despite practical limitations, the JAMRIS system could provide more complete information when both knees are scored. The additional value of MRI of bilateral knees in the evaluation of disease status in JIA patients is being addressed in an ongoing study.
A limitation of our study is the lack of MR images of age-matched healthy controls. Because growing joints mature, it may be difficult to establish whether differences in the appearance of the knee joint are pathological or part of normal maturation. For instance, the prevalence of bony depressions and signal changes suggestive of bone marrow oedema in the wrists and knees of healthy children is high [13, 34].
In summary, the JAMRIS system was developed and validated for the evaluation of inflammatory and destructive changes in the knees of JIA patients. It proved to be an easy-to-use and reliable assessment score in the evaluation of JIA disease activity in terms of inflammation and damage, and may therefore be used as an objective outcome measure in future research and clinical trials. The use of JAMRIS as a follow-up parameter for synovial hypertrophy is promising. More follow-up data in JIA will be needed to assess the reliability concerning a change in bone marrow change, cartilage lesion and bone erosion scores over time.
References
Ravelli A, Martini A (2007) Juvenile idiopathic arthritis. Lancet 369:767–778
Petty RE, Southwood TR, Manners P et al (2004) International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol 31:390–392
Albers HM, Wessels JA, van der Straaten RJ et al (2009) Time to treatment as an important factor for the response to methotrexate in juvenile idiopathic arthritis. Arthritis Rheum 61:46–51
Vilca I, Munitis PG, Pistorio A et al (2010) Predictors of poor response to methotrexate in polyarticular-course juvenile idiopathic arthritis: analysis of the PRINTO methotrexate trial. Ann Rheum Dis 69:1479–1483
Nistala K, Babar J, Johnson K et al (2007) Clinical assessment and core outcome variables are poor predictors of hip arthritis diagnosed by MRI in juvenile idiopathic arthritis. Rheumatology (Oxford) 46:699–702
Guzman J, Burgos-Vargas R, Duarte-Salazar C, Gomez-Mora P (1995) Reliability of the articular examination in children with juvenile rheumatoid arthritis: interobserver agreement and sources of disagreement. J Rheumatol 22:2331–2336
Doria AS, Babyn PS, Feldman B (2006) A critical appraisal of radiographic scoring systems for assessment of juvenile idiopathic arthritis. Pediatr Radiol 36:759–772
Johnson K (2006) Imaging of juvenile idiopathic arthritis. Pediatr Radiol 36:743–758
Miller E, Uleryk E, Doria AS (2009) Evidence-based outcomes of studies addressing diagnostic accuracy of MRI of juvenile idiopathic arthritis. AJR Am J Roentgenol 192:1209–1218
Malattia C, Damasio MB, Pistorio A et al (2011) Development and preliminary validation of a paediatric-targeted MRI scoring system for the assessment of disease activity and damage in juvenile idiopathic arthritis. Ann Rheum Dis 70:440–446
Østergaard M, Peterfy C, Conaghan P et al (2003) OMERACT rheumatoid arthritis magnetic resonance imaging studies. Core set of MRI acquisitions, joint pathology definitions, and the OMERACT RA-MRI scoring system. J Rheumatol 30:1385–1386
Hodgson RJ, O’Connor P, Moots R (2008) MRI of rheumatoid arthritis image quantitation for the assessment of disease activity, progression and response to therapy. Rheumatology (Oxford) 47:13–21
Müller LS, Avenarius D, Damasio B et al (2011) The paediatric wrist revisited: redefining MR findings in healthy children. Ann Rheum Dis 70:605–610
Hemke R, van Veenendaal M, Kuijpers TW, van Rossum MA, Maas M (2012) Increasing feasibility and patient comfort of MRI in children with juvenile idiopathic arthritis. Pediatr Radiol 42:440–448
Østergaard M, Klarlund M (2001) Importance of timing of post-contrast MRI in rheumatoid arthritis: what happens during the first 60 minutes after IV gadolinium-DTPA? Ann Rheum Dis 60:1050–1054
Giannini EH, Ruperto N, Ravelli A, Lovell DJ, Felson DT, Martini A (1997) Preliminary definition of improvement in juvenile arthritis. Arthritis Rheum 40:1202–1209
Guermazi A, Roemer FW, Hayashi D et al (2011) Assessment of synovitis with contrast-enhanced MRI using a whole-joint semiquantitative scoring system in people with, or at high risk of, knee osteoarthritis: the MOST study. Ann Rheum Dis 70:805–811
Hunter DJ, Lo GH, Gale D, Grainger AJ, Guermazi A, Conaghan PG (2008) The reliability of a new scoring system for knee osteoarthritis MRI and the validity of bone marrow lesion assessment: BLOKS (Boston Leeds Osteoarthritis Knee Score). Ann Rheum Dis 67:206–211
Gylys-Morin VM, Graham TB, Blebea JS et al (2001) Knee in early juvenile rheumatoid arthritis: MR imaging findings. Radiology 220:696–706
Norman GR, Wyrwich KW, Patrick DL (2007) The mathematical relationship among different forms of responsiveness coefficients. Qual Life Res 16:815–822
Haavardsholm EA, Bøyesen P, Østergaard M, Schildvold A, Kvien TK (2008) Magnetic resonance imaging findings in 84 patients with early rheumatoid arthritis: bone marrow oedema predicts erosive progression. Ann Rheum Dis 67:794–800
Hetland ML, Ejbjerg B, Horslev-Petersen K et al (2009) MRI bone oedema is the strongest predictor of subsequent radiographic progression in early rheumatoid arthritis. Results from a 2-year randomised controlled trial (CIMESTRA). Ann Rheum Dis 68:384–390
Østergaard M, Hansen M, Stoltenberg M et al (1999) Magnetic resonance imaging-determined synovial membrane volume as a marker of disease activity and a predictor of progressive joint destruction in the wrists of patients with rheumatoid arthritis. Arthritis Rheum 42:918–929
Conaghan PG, O’Connor P, McGonagle D et al (2003) Elucidation of the relationship between synovitis and bone damage: a randomized magnetic resonance imaging study of individual joints in patients with early rheumatoid arthritis. Arthritis Rheum 48:64–71
Oen K, Reed M, Malleson PN et al (2003) Radiologic outcome and its relationship to functional disability in juvenile rheumatoid arthritis. J Rheumatol 30:832–840
van Rossum MA, Zwinderman AH, Boers M et al (2003) Radiologic features in juvenile idiopathic arthritis: a first step in the development of a standardized assessment method. Arthritis Rheum 48:507–515
McQueen F, Lassere M, Duer-Jensen A et al (2009) Testing an OMERACT MRI scoring system for peripheral psoriatic arthritis in cross-sectional and longitudinal settings. J Rheumatol 36:1811–1815
Youssef PP, Kraan M, Breedveld F et al (1998) Quantitative microscopic analysis of inflammation in rheumatoid arthritis synovial membrane samples selected at arthroscopy compared with samples obtained blindly by needle biopsy. Arthritis Rheum 41:663–669
Bøyesen P, Haavardsholm EA, Østergaard M, van der Heijde D, Sesseng S, Kvien TK (2011) MRI in early rheumatoid arthritis: synovitis and bone marrow oedema are independent predictors of subsequent radiographic progression. Ann Rheum Dis 70:428–433
van der Heijde D (1999) How to read radiographs according to the Sharp/van der Heijde method. J Rheumatol 26:743–745
McQueen F, Lassere M, Bird P et al (2007) Developing a magnetic resonance imaging scoring system for peripheral psoriatic arthritis. J Rheumatol 34:859–861
Shire NJ, Dardzinski BJ (2011) Picture-perfect: imaging techniques in juvenile idiopathic arthritis. Imaging Med 3:635–651
Malattia C, Damasio MB, Basso C et al (2010) Dynamic contrast-enhanced magnetic resonance imaging in the assessment of disease activity in patients with juvenile idiopathic arthritis. Rheumatology (Oxford) 49:178–185
Jans LB, Jaremko JL, Ditchfield M, Verstraete KL (2011) Evolution of femoral condylar ossification at MR imaging: frequency and patient age distribution. Radiology 258:880–888
Acknowledgments
A research grant was received from the Reumafonds, Dutch Arthritis Association (Amsterdam, The Netherlands). The Dutch Arthritis Association was not involved in designing and conducting this study, did not have access to the data, and was not involved in data analysis or preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 465 kb)
Rights and permissions
About this article
Cite this article
Hemke, R., van Rossum, M.A.J., van Veenendaal, M. et al. Reliability and responsiveness of the Juvenile Arthritis MRI Scoring (JAMRIS) system for the knee. Eur Radiol 23, 1075–1083 (2013). https://doi.org/10.1007/s00330-012-2684-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-012-2684-y