Abstract
Purpose of Review
Diabetes is associated with an increased risk for several types of cancer. Therefore, use of antihyperglycemic medications to lower blood glucose may modify cancer risk. Here we review available data on the link between the most common classes of antihyperglycemic agents and cancer risk among patients with diabetes.
Recent Findings
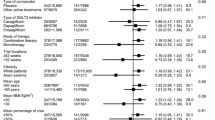
A database search was conducted between February 2022 and June 2022 on PubMed and Embase for systematic reviews and meta-analyses investigating the association between antihyperglycemic agents and risk of cancer. Use of biguanides such as metformin is associated with 20–30% lower risk for all cancer incidence, and somewhat greater benefit for cancer-related mortality. Alpha-glucosidase inhibitors, e.g., acarbose, have not been consistently associated with cancer. Similarly, no consistent effects have been reported for thiazolidinediones, but the relationship with cancer seems to depend on the type of drug, dose, and duration of treatment. Exposure to various types of incretin-based therapies (glucagon-like peptide-1 agonists and dipeptidyl peptidase-4 inhibitors) has not been found to significantly modify cancer risk. Inhibitors of sodium glucose cotransporter-2 may raise risk for bladder cancer and reduce risk for gastrointestinal cancer. Use of insulin and insulin analogs is associated with a significant increase in total cancer risk by almost 50% compared to other antihyperglycemic drugs. Likewise, insulin secretagogues like sulfonylureas have generally been linked to greater risk for cancer by ~ 20%, although these associations may be agent-specific and dose-dependent.
Summary
Current evidence suggests that the risk of cancer associated with the use of antihyperglycemic medications among patients with diabetes depends on the class of drug and type of agent, dosage, and duration of treatment. More research is needed to delineate the mechanisms by which these agents affect the process of carcinogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of overweight and obesity has increased rapidly over the past several decades [1, 2]. In 2016, it was estimated that 13% of the population was obese, reflecting a threefold increase in prevalence since 1975 [1,2,3]. This increase occurred among both men and women and in all geographical regions around the world [2]. Currently, about 1.9 billion adults have some degree of excess weight, and about 650 million of them are obese. Although obesity is a multifactorial disease, the common denominator is an imbalance between calorie intake and energy expenditure leading to chronic positive energy balance. Globally, more people are living a sedentary lifestyle, while food has become more energy-dense and portions have increased; the obesogenic environment where convenience is essential is undoubtedly a major contributor to the obesity epidemic [1, 3].
Obesity is associated with many cardiometabolic abnormalities—e.g., hyperglycemia, insulin resistance, dyslipidemia, hypertension, and inflammation—and thus increases the risk for developing many non-communicable diseases such as diabetes mellitus. A decrease of the insulin-inducible glucose transporter 4 and its membrane translocation is often observed in obesity, leading to a reduction in insulin-mediated glucose uptake and, eventually, the development of hyperglycemia [4]. Obesity is also linked with chronic subclinical inflammation, which leads to macrophage infiltration and release of proinflammatory cytokines such as tumor necrosis factor-α, interleukin-6 and interleukin-1β, and adipokines. Among other mechanisms, the inflammatory response induces nitric oxide synthase which leads to S-nitrosylation of the signaling proteins that are essential to insulin signaling and the development of insulin resistance [5]. Over time, insulin resistance becomes more severe, and the body responds with increased insulin secretion from the pancreatic beta cells. The beta cells can compensate for a period of time; however, eventually, the requirement for increased insulin leads to beta cell failure, and type 2 diabetes (T2D) develops [6]. In type 1 diabetes (T1D), immune-mediated destruction of the beta cells and subsequent complete lack of insulin availability is the primary driver of hyperglycemia.
Alongside the rise in the prevalence of overweight and obesity, the rate of diabetes has quadrupled since the 1980s [7]. In 1980, there were 108 million people with diabetes [8, 9] and this number rose to 537 million in 2021, with another 541 million having impaired glucose tolerance (prediabetes), which in many cases leads to diabetes. Furthermore, the International Diabetes Federation projects a 45% increase in diabetes around the world from 2021 to 2045; besides the medical consequences for the health of the individual and the population in general, the economic burden for managing the disease is also expected to rise considerably from the 966 billion USD in 2021 (which has more than tripled since 2006) [8]. Diabetes is therefore a serious public health problem. In 2021, there were 6.7 million deaths because of diabetes, which translates into 1 person dying from a diabetes complication every fifth second [8]. People with diabetes are at risk for developing multiple microvascular and macrovascular complications. Chronic hyperglycemia causes a number of physiological alterations in many organ systems and tissues (“glucotoxicity”)—it can induce oxidative stress, stimulate polyol and hexosamine pathways, activate protein kinase C, promote the formation of advanced glycation end-products, and alter gene expression, among others [10]—and can lead to diseases or vascular complications such as cardiovascular disease, nephropathy, neuropathy, retinopathy, periodontitis, and also cancer [11, 12].
Diabetes is associated with a greater risk for several types of cancer, e.g., liver, pancreas, and breast cancers. The main metabolic disturbances that are thought to underlie the increased risk of cancer among people with diabetes include hyperglycemia, hyperinsulinemia, and inflammation [13,14,15,16]. Nonetheless, it remains unclear if the association between diabetes and cancer is direct, due to these metabolic abnormalities, or indirect, through common risk factors such as obesity [17]. In any case, the need for treating diabetes, or at least for controlling hyperglycemia and maintaining a stable blood glucose concentration throughout the day, is critical to prevent or delay the medical complications of the disease. However, use of some antihyperglycemic agents has been linked with the development and progression of certain types of cancer, despite that all of them are, by definition, effective in lowering blood glucose [15]. The possibility that antihyperglycemic agents induce certain types of cancers raises concern that becomes greater when one takes into account the projected rise in the number of people with diabetes and, accordingly, in the use of antihyperglycemic medications in the foreseeable future.
There are currently more than 60 antihyperglycemic pharmaceuticals approved by the US Food and Drug Administration and nearly 100 more are being evaluated in clinical trials [18•, 19]. In this manuscript, we review the results from observational (cross-sectional and cohort) or randomized studies—focusing mainly on systematic reviews and meta-analyses—on the relationship between the use of antihyperglycemic agents and cancer risk among patients with diabetes (Table 1). We discuss the most commonly used antihyperglycemic medications, including biguanides (e.g., metformin), alpha-glucosidase inhibitors (AGIs, e.g., acarbose), thiazolidinediones (TZDs), glucagon-like peptide-1 (GLP-1) agonists, dipeptidyl peptidase-4 (DPP-4) inhibitors, sodium glucose cotransporter-2 (SGLT-2) inhibitors, insulin and insulin analogs, and secretagogues (e.g., sulfonylureas).
Biguanides
Metformin is one of the most popular antihyperglycemic medications used to manage diabetes, and has dominantly shown beneficial effects on overall cancer incidence [20•, 21•], although this is not always evident [21•, 22]. In 2005, Evans et al. conducted a case–control study and reported that use of metformin among 923 patients with newly diagnosed diabetes was associated with a 15–20% lower incidence of cancer [23]. Bowker et al. compared metformin against insulin or sulfonylureas in a population-based cohort study with ~ 5.5 years of follow-up, and found that exposure to metformin was associated with decreased risk of cancer mortality by 30–90% compared to exposure to insulin or sulfonylureas among 10,309 patients with diabetes [24]. In 2021, Zhang et al. [25••] conducted a systematic review and meta-analysis on metformin and risk of cancer among patients with T2D. A total of 67 studies met the inclusion criteria, resulting in 10,685,875 patients with T2D and 145,108 cancer cases. Overall, there was a significant decrease of cancer risk for ever-metformin users compared to never-metformin users by ~ 30% (odds ratio [OR] 0.70, confidence interval [CI] 0.65–0.76). The beneficial effect of metformin on cancer risk was evident also when compared to the use of other antihyperglycemic agents (OR 0.80, 95% CI 0.73–0.87). In a subgroup analysis for different types of cancer, it was found that risks of bladder cancer, colorectal cancer, esophageal cancer, liver cancer, head and neck cancer, lung cancer, pancreatic cancer, and prostate cancer were all significantly lower among ever-metformin users compared to non-users. These results were largely similar in cohort and case–control studies [25••].
Ng et al. [26••] recently performed a systematic review, meta-analysis, and meta-regression to investigate the effects of metformin use on the risk of colorectal cancer. They compared metformin vs. non-metformin users, metformin users vs. non-diabetics, and metformin users vs. diabetics treated only with diet. A total of 58 studies that reported on the incidence of colorectal adenoma and cancer were included and analyzed. Six studies compared metformin users vs. non-metformin users and showed a significant 23% reduction in adenoma formation among users of metformin (relative risk [RR] 0.77, CI 0.67–0.88, p < 0.001). In addition, four studies showed there was a 39% lower risk of advanced adenoma (RR 0.61, CI 0.42–0.88, p = 0.008). When it came to cancer, the analysis included a total of 946,292 metformin users and 773,506 non-metformin users and demonstrated that the former had a 24% lower colorectal cancer incidence compared to the latter (RR 0.76, CI 0.69–0.84, p < 0.001) [26••]. Farmer et al. [27] conducted a comprehensive bias evaluation in their systematic review on metformin and cancer in T2D. This analysis included 46 studies, 21 of which investigated the effect of metformin on all cancer types. Results indicated that no studies reported a harmful effect from metformin use and 12 out of the 21 studies reported a statistically significant protective effect associated with metformin use. A few years earlier, Franciosi et al. [28] evaluated the link between metformin therapy and risk of cancer in patients with T2D through yet another systematic review of observational studies. Overall, there was a significant association of exposure to metformin with lower risk of cancer death (6 studies, 24,410 patients, OR 0.65, CI 0.53–0.80), as well as total cancer incidence (18 studies, 561,836 patients, OR 0.73, CI 0.61–0.88) and incidence of cancers of the liver, colon and rectum, pancreas, stomach, and esophagus; but not with breast, lung, ovarian, uterus, prostate, bladder, and kidney cancers, and melanoma [28].
Although the precise mechanisms by which metformin protects against cancer are not fully understood, the increase in the intracellular ratio of AMP-to-ATP due to the depletion of ATP levels leads to the activation of the liver-kinase-B1 (LKB1)-AMP-activated-protein kinase (AMPK) signaling pathway, which then negatively regulates the mammalian target of rapamycin (mTOR) pathway; this has been proposed as a key event for the apparent anticancer properties of metformin [20•, 29,30,31,32].
Alpha-glucosidase Inhibitors
The association between the use of AGIs and cancer risk has not been consistently reported. A meta-analysis of 265 studies (44 cohort studies, 39 case–control studies, and 182 randomized trials) concluded that AGI use was associated with increased risk of cancer (RR 1.10, CI 1.05–1.15) [33], but this analysis included a mixture of observational studies and randomized trials, different cancer types, and small sample sizes [33]. Subsequent studies provided inconsistent results [34, 35]. More recently, Zhao et al. [36] conducted a systematic review and meta-analysis of both observational studies and randomized trials, which included a total of 25 studies (14 cohort, 7 case–control, 4 randomized) and more than 1.2 million participants [36]. Four studies found a decreased risk of cancer with AGI use [34, 37,38,39], one found a higher risk [40], and 20 reported no statistically significant association [35, 41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. When observational studies were analyzed separately, AGI use was associated with lower cancer incidence (OR 0.86, CI 0.78–0.96), but this was not the case in randomized trials (OR 0.83, CI 0.20–3.46) [36]. Furthermore, 17 studies (16 observational, 1 randomized) reported the risk of specific cancer types in AGI users vs. non-users. The beneficial effects of AGI use was particularly pronounced for lung cancer (OR 0.70, CI 0.52–0.93), colorectal cancer (OR 0.79, CI 0.54–1.15), liver cancer (OR 0.89, CI 0.75–1.05), gastric cancer (OR 0.69, CI 0.36–1.31), gastrointestinal cancer (OR 0.83, CI 0.71–0.97), and breast cancer (OR 0.74, CI 0.37–1.51), but most of these results were not statistically significant [36]. In addition, no significant associations were found for pancreatic, esophageal, and urothelial cancers [36]. These findings should be interpreted with caution, bearing in mind that the majority of participants were taking multiple antihyperglycemic medications simultaneously, including metformin, which has protective effects against cancer [60, 61], and thus possibly masking the actual effect on the risk associated with using AGIs alone.
Thiazolidinediones
In a recent meta-analysis of 10 observational studies, Liu et al. investigated antihyperglycemic medication use and risk of colorectal cancer among 2,470,768 patients with diabetes and 18,972 cancer cases [62]. Exposure to TZDs was associated with a 9% reduction of colorectal cancer risk (RR 0.91, CI 0.84–0.99, p = 0.03). An inverse relationship between TZDs and colorectal cancer, as well as liver cancer, had also been observed earlier by Bosetti et al. [63]. In that meta-analysis, however, TZD use was not associated with overall cancer risk among patients with T2D (RR 0.96, CI 0.91–1.01) [63]. Also, there was no association of TZD use with pancreatic, lung, breast, and prostate cancers, whereas in fact an excess risk of bladder cancer was found with pioglitazone (RR 1.20, CI 1.07–1.34, 6 studies) but not rosiglitazone (RR 1.08, CI 0.95–1.23, 3 studies) [63]. The pioglitazone-associated increase in risk was greater for higher dosages (RR 1.64 for cumulative doses > 28,000 mg) and for longer duration of use (RR 1.42 for > 2 years) [63]. A similar result was reported by Mamtani et al. [64], who investigated the association between the duration of antihyperglycemic therapy and risk of bladder cancer in a cohort study of patients with T2D mellitus treated with TZDs (n = 18,459) or sulfonylureas (n = 41,396). Although there was no difference in bladder cancer risk between the two cohorts in analyses that did not account for duration of exposure (TZD vs. sulfonylureas, hazard ratio (HR) 0.93, CI 0.68–1.29), the use of TZDs for a period ≥ 5 years was associated with an increased risk of bladder cancer compared with sulfonylureas (HR 3.25, CI 1.08–9.71). In that analysis, pioglitazone and rosiglitazone did not differ in their effects on cancer risk. With respect to lung cancer, and contrary to a null effect reported in the meta-analysis by Bosetti et al. [63], Wang et al. in the same year conducted a meta-analysis of 7 cohort studies and found that TZD use reduces the risk of lung cancer by ~ 20% in patients with T2D [22].
TZDs have been shown to suppress the growth of cancer cells in vitro and in vivo [20•, 65,66,67]. This has been observed with rosiglitazone through the inhibition of tumor growth in a human neuroblastoma xenograft, most likely mediated by its strong anti-angiogenic activity [66].
Glucagon-Like Peptide-1 Receptor Agonists
Cao et al. [68] investigated the risk of cancer in patients with T2D using GLP-1 receptor agonists. They focused on randomized trials that had treated patients with GLP-1 agonists for at least 52 weeks and were able to find 37 eligible studies. Pooled analysis demonstrated that the risk for any type of cancer was not significantly different with GLP-1 agonists than with various other comparators (OR 1.03, CI 0.95–1.12, p = 0.41). Usage of albiglutide was associated with a reduced risk for overall cancer (OR 0.76, CI 0.60–0.97, p = 0.03), whereas no GLP-1 agonist was found to increase cancer risk. This was also true for thyroid and pancreatic cancers [68]. Similar results were reported in two other meta-analyses [69, 70]. Likewise, in the meta-analysis by Piccoli et al. [71••], treatment with GLP-1 agonists was found to not affect the risk of breast cancer.
Guo et al. conducted a meta-analysis of 26 randomized trials including ~ 16,000 patients with T2D who were treated once weekly with GLP-1 receptor agonists [72]. Their analysis compared GLP-1 agonists to other antihyperglycemic agents and indicated no significant effects on the risk of tumors (RR 1.02, CI 0.74–1.41, p = 0.91). These results were the same regardless of the type of GLP-1 agonist, as well as for different treatment durations (less or more than 1 year). However, this study is limited by the fact that all types of tumors—benign, malignant, and unspecified neoplasms—were included. Furthermore, due to the lack of detailed description of the neoplasms in several primary studies, it was not entirely clear if the neoplasms appeared after treatment or were present even before treatment [72]. In 2019, Liu et al. addressed the question of whether GLP-1 agonists increase the risk of malignant neoplasia compared with placebo or other antihyperglycemic agents in patients with T2D [73]. These authors included data from randomized trials that had a duration of ≥ 24 weeks and identified 34 studies with ~ 50,000 patients. The analysis showed that regardless of the type of GLP-1 receptor agonists, there was no significant increase in the risk for malignant neoplasm formation—all GLP-1 agonists (OR 1.04, CI 0.94–1.15, p = 0.46); liraglutide (OR 1.08, CI 0.91–1.27); exenatide (OR 1.00, CI 0.86–1.16); semaglutide (OR 0.89, CI 0.35–2.22); and albiglutide (OR 1.07, 0.23–4.88) [73].
GLP-1 receptor agonists present pleiotropic physiological actions [74, 75] but the mechanisms that could potentially affect cancer risk remain elusive. Studies in rodent models have suggested that stimulation of thyroid C-cells by GLP-1 agonists triggers the release of calcitonin and leads to the upregulation of gene expression, resulting in C-cell hyperplasia and an increased risk of medullary adenomas and carcinomas [76]. In addition, long-term stimulation with GLP-1 agonists has been associated with increased levels of calcitonin mRNA, C-cell proliferation, and tumor formation in mice and rats [76, 77•]. Nonetheless, data from human studies do not support an increase in thyroid cancer risk with GLP-1 agonists [686970].
DPP-4 Inhibitors
Zhang et al. recently conducted a meta-analysis to evaluate how treatment with DPP-4 inhibitors (and GLP-1 agonists) affects the risk of pancreatitis and pancreatic cancer in patients with T2D [78•]. They included a total of 17 eligible studies with 102,257 participants and found that DPP-4 inhibitors were not associated with an increase in risk for pancreatic cancer (RR 0.79, CI 0.26–2.40). These results were robust in sensitivity and subgroup analyses [78•]. Similar results were reported in two other meta-analyses: one that included 6 placebo-controlled trials with 55,248 patients with T2D, which found that incretin-based therapies (DPP-4 inhibitors and GLP-1 receptor agonists; 3 studies each) do not affect pancreatic cancer risk [79]; and another that included 11 randomized trials (55,921 patients treated with GLP-1 agonists and 43,306 patients treated with DPP-4 inhibitors), which found the same [80•]. Likewise, in the meta-analysis of 157 randomized trials by Dicembrini et al. [81••], treatment with DPP-4 inhibitors was not associated with any significant change in the risk of total cancer (OR 0.93, CI 0.86–1.00, p = 0.07). The same was true for the incidence of all malignant neoplasms in the meta-analysis by Abd El Aziz et al. [80•]. Results were largely similar for the different types of DPP-4 inhibitors [81••]. However, in post hoc analysis limited to placebo-controlled trials, a significant association was found between use of DPP-4 inhibitors and reduced incidence of overall cancer (OR 0.90, CI 0.82–0.99, p = 0.03) and colorectal cancer (OR 0.70, CI 0.53–0.94, p = 0.02) [81••].
DPP-4 inhibitors inactivate the enzyme DPP-4 which naturally degrades the incretin hormones (GLP-1 and gastric inhibitory polypeptide) [82]. However, there has been some concern about the possible role of DPP-4 inhibitors in the development of invasive carcinomas, because of altered regulation of the activity of various biopeptides through proteolytic cleavage, including chemokines and cytokines [83]. DPP-4 inhibitors include the substrate C-X-C motif chemokine ligand 12 (CXCL12), which naturally binds to the receptor’s C-XC motif chemokine receptor 4 and C-XC motif chemokine receptor 7, and regulates tumor growth and tumor metastasis [84, 85•]. Thus, a higher level of CXCL12 due to DPP-4 inhibitors can be relevant for CXCR4-positive cancers (e.g., in kidney, lung, brain, prostate, breast, pancreas, and ovarian cancers, and melanomas) [86].
Sodium Glucose Cotransporter-2 Inhibitors
SGLT2 inhibitors act on kidneys and decrease renal glucose reabsorption, thus lowering blood glucose independently of insulin insufficiency or insulin resistance [87]. There have been mixed findings regarding the safety and efficacy of these drugs, mainly due to concerns about the use of dapagliflozin and increased risk for bladder and breast cancers [88, 89]. Other SGLT2 inhibitors have not been associated with an elevated risk of bladder or breast cancer in humans [87].
Tang et al. [90] performed a pair-wise meta-analysis of all data from randomized trials to analyze the risk for specific cancers associated with the use of SGLT2 inhibitors vs. placebo in individuals with T2D [90]. All trials had a duration of ≥ 24 weeks and reported cancer incidence as an outcome. The study included a total of 46 independent trials with 34,569 patients who were randomly assigned to an SGLT2 inhibitor (canagliflozin, dapagliflozin, or empagliflozin) or a comparator (placebo or a different type of antihyperglycemic medication) [90]. There was no significant difference between treatment with SGLT2 inhibitors and comparators for total cancer risk (OR 1.14, CI 0.96–1.36); however, among the participants with diabetes and obesity, exposure to SGLT2 inhibitors was linked to an increased total cancer risk (OR 1.23, CI 1.02–1.48). For site-specific cancers, SGLT2 inhibitors were significantly associated with an increased risk of bladder cancer (OR 3.87, CI 1.48–10.08) and this was particularly true for empagliflozin (OR 4.49, CI 1.21–16.73) [90]. Trials lasting for ≥ 1 year also showed an increased risk of bladder cancer with SGLT2 inhibitors, mainly empagliflozin (OR 4.80, CI 1.74–13.29) [90].
The use of SGLT2 inhibitors has been associated with higher rates of glycosuria and urinary tract infections, which may explain the higher risk of cancer at this site [87]. By contrast, canagliflozin has been associated with substantially lower risk of gastrointestinal cancers than comparator arms (OR 0.15, CI 0.04–0.60). Canagliflozin suppresses both SGLT2 and SGLT1, and the latter is key for cancer cell survival through mediating glucose uptake [91]. Thus, the beneficial effect of this SGLT2 inhibitor on the risk for gastrointestinal cancer may be due to its intestinal SGLT1-supressing ability [91]. It is important to note that the beneficial effect of SGLT2 inhibitors on body weight [90] may confound the risk for cancer indirectly, through reduced adiposity which is a known risk factor for bladder cancer [90]. SGLT2 inhibitors are also often prescribed together with metformin, which has been shown to decrease the risk of cancer [92]. This further highlights the challenges of identifying the mechanisms behind the elevated risk of bladder cancer associated with use of SGLT2 inhibitors.
Insulin and Insulin Analogs
Insulin, a key growth hormone regulating glucose homeostasis, remains the most important agent for managing diabetes [93]. Although a wide range of insulin types have been developed since the discovery of insulin in 1921 [93], the majority of individuals living with diabetes start off on a combination of neutral protamine Hagedorn (NPH) insulin, an intermediate-acting insulin, and a rapid-acting analog like aspart or lispro administered 2 to 3 times daily [94]. Current insulin therapies, such as subcutaneous insulin infusion, employ both glargine insulin (long-acting insulin) and rapid-acting analogs [94]. Insulin mainly targets the liver, skeletal muscle, and adipose tissue [95] and has important effects on a variety of physiological functions, including glucose and amino acid transport, lipid and glycogen metabolism, protein synthesis, and gene transcription [95].
Patients with diabetes who are on insulin therapy are typically exposed to high levels of exogenously administered insulin to achieve optimal glucose control [17]. Therefore, it is biologically plausible that treatment with insulin increases risk of cancer since insulin is a growth factor that can stimulate neoplastic growth [96, 97]. Earlier observational studies reported concerning results about the plausible link between insulin use and risk of cancer; however, many of these studies failed to take into account dose, duration, and timing of insulin exposure, so it was not possible to draw firm conclusions [98,99,100,101]. Information from randomized trials is scarce, partly because carcinogenesis is a long-term process, and those that have been completed so far are too small or too short to robustly quantify risk of specific cancers [102, 103].
Karlstad et al. [17] performed a systematic review and meta-analysis of observational studies that investigated the association between risk of cancer (any type) and exogenous human insulin or insulin analogs in patients with T1D and T2D [17]. These authors compared insulin use vs. no-insulin use; insulin vs. other antihyperglycemic drugs; and glargine insulin vs. non-glargine insulin. In total, 34 studies fulfilled the inclusion criteria for the pooled analysis. The results indicated that patients who use insulin have a significantly greater risk for pancreatic cancer (RR 2.58, CI 2.05–3.25), liver cancer (RR 1.84, CI 1.32–2.58), kidney cancer (RR 1.38, CI 1.06–1.79), cancers of the respiratory system (RR 1.30, CI 1.14–1.47), and stomach cancer (RR 1.65, CI 1.02–2.68), but significantly lower risk for prostate cancer (RR 0.80, CI 0.73–0.88) than those who do not use insulin (all p < 0.05) [17]. When comparing insulin to other antihyperglycemic drugs, a significant increase was observed for total cancer risk (RR 1.52, CI 1.16–2.00), pancreatic cancer risk (RR 3.83, CI 1.43–10.23), and colorectal cancer risk (RR 1.79, CI 1.36–2.36) (all p < 0.05) [17]. Furthermore, the use of insulin glargine was associated with lower risk for colon cancer (RR 0.71, CI 0.56–0.91) but higher risk for breast cancer (RR 1.14, CI 1.01–1.29) [17]. Nevertheless, these results must be interpreted with caution. The importance of insulin dose and duration of insulin exposure should be analyzed concurrently when assessing cancer risk; however, many investigators did not include such information in the primary studies [17]. In addition, the choice of covariates differed substantially in the included studies, which highlights the existing variability in confounders for each specific cancer [17]. Exposure duration may also have been too short to indicate causality regarding cancer. Some studies have observed exceptionally higher risk with shorter durations compared to longer durations of treatment [104,105,106,107].
Sulfonylureas
In 2015, Wu et al. conducted a meta-analysis that included 265 studies to investigate the association between pharmacologic therapy of diabetes and overall cancer risk and mortality. They identified 72 studies (18 case–control, 16 cohort, 38 randomized trials) which reported on sulfonylurea use and cancer incidence, and found that sulfonylureas were associated with an increased risk of cancer (RR 1.20, CI 1.13–1.27) [33]. In 2013, Thakkar et al. investigated both metformin and sulfonylureas in relation to cancer risk in patients with T2D. In their meta-analysis, they included 18 studies, and concluded that sulfonylureas were associated with an increased overall cancer risk, although not with cancer mortality. Moreover, a significant association with cancer incidence was found only among the 6 cohort studies (RR 1.55, CI 1.48–1.63) but not among the 10 case–control studies (RR 1.02, CI 0.93–1.13) and the 2 randomized trials (RR 1.17, CI 0.95–1.45) [108]. A recent meta-analysis by Mekuria et al. synthesized data from 8 cohort studies comparing monotherapy with metformin or sulfonylureas among patients with T2D, and reported significantly greater cancer risk by ~ 25% in those using sulfonylureas compared to those using metformin, whether before or after adjustment for confounders [109].
Contrary to these results, Yang et al. in 2010 found that use of both gliclazide and glibenclamide was associated with ~ 35% lower cancer risk, and in a dose-dependent manner, during ~ 5 years of follow-up of 6103 patients with T2D [59]. On the other hand, in a case–control study of patients with T2D with or without cancer, exposure to gliclazide for more than 36 months was associated with a significant reduction in the risk of cancer after adjusting for confounders (OR 0.40, CI 0.21–0.57, p = 0.004), whereas conversely, exposure to glibenclamide for at least 36 months was associated with increased cancer incidence (OR 2.62, CI 1.26–5.42, p = 0.009). Evidently, the use of sulfonylureas needs to be further investigated in relation to cancer risk, and the associations may be agent-specific and dose-dependent.
Conclusion
The protective effect of metformin on the overall development of cancer seems to be well-established. Accordingly, it may be relevant to include metformin in multidrug treatment regimens to mitigate increased cancer risk from other medications, e.g., insulin or sulfonylureas. Evidence for other classes of antihyperglycemic agents including alpha-glucosidase inhibitors, thiazolidinediones, and incretin-based therapies (GLP-1 agonists and DPP-4 inhibitors) is inconsistent so far and indicates either no association with cancer or some positive and negative associations with site-specific cancers, which can furthermore depend on the specific agent, dose, and duration of treatment. One major confounder in studies of this sort is that patients are often concurrently exposed to more than one medication for variable periods of time. More research is needed to dissect the associations between each class of antihyperglycemic agents and cancer risk in humans, and delineate the mechanisms by which these agents could potentially affect the process of carcinogenesis.
Data Availability
This article does not contain any primary data.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15:288–98. https://doi.org/10.1038/s41574-019-0176-8.
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10. https://doi.org/10.1016/j.metabol.2018.09.005.
World Health Organization. Obesity and overweight; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 23 Nov 2022.
Atawia RT, Bunch KL, Toque HA, Caldwell RB, Caldwell RW. Mechanisms of obesity-induced metabolic and vascular dysfunctions. Front Biosci. 2019;24:890–934. https://doi.org/10.2741/4758.
Martyn JA, Kaneki M, Yasuhara S. Obesity-induced insulin resistance and hyperglycemia: etiologic factors and molecular mechanisms. Anesthesiology. 2008;109:137–48. https://doi.org/10.1097/ALN.0b013e3181799d45.
Kasuga M. Insulin resistance and pancreatic beta cell failure. J Clin Invest. 2006;116:1756–60. https://doi.org/10.1172/jci29189.
World Health Organization. Obesity-complications; 2022. Available from: https://www.who.int/health-topics/obesity#tab=tab_2. Accessed 23 Nov 2022.
International Diabetes Federation. Diabetes atlas, 10 edn. Brussels: International Diabetes Federation; 2021. Available from: https://diabetesatlas.org/atlas/tenth-edition/. Accessed 23 Nov 2022.
World Health Organization. Diabetes; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/diabetes. Accessed 23 Nov 2022.
Giri B, Dey S, Das T, Sarkar M, Banerjee J, Dash SK. Chronic hyperglycemia mediated physiological alteration and metabolic distortion leads to organ dysfunction, infection, cancer progression and other pathophysiological consequences: an update on glucose toxicity. Biomed Pharmacother. 2018;107:306–28. https://doi.org/10.1016/j.biopha.2018.07.157.
Cade WT. Diabetes-related microvascular and macrovascular diseases in the physical therapy setting. Phys Ther. 2008;88:1322–35. https://doi.org/10.2522/ptj.20080008.
International Diabetes Federation. Diabetes complications; 2020. Available from: https://www.idf.org/aboutdiabetes/complications.html. Accessed 23 Nov 2022.
Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of hyperglycemia in type 2 diabetes, 2018 — a consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41:2669–701. https://doi.org/10.2337/dci18-0033.
Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, et al. Diabetes and cancer: a consensus report. Diabetes Care. 2010;33:1674–85. https://doi.org/10.2337/dc10-0666.
Wojciechowska J, Krajewski W, Bolanowski M, Kręcicki T, Zatoński T. Diabetes and cancer: a review of current knowledge. Exp Clin Endocrinol Diabetes. 2016;124:263–75. https://doi.org/10.1055/s-0042-100910.
Zelenko Z, Gallagher EJ. Diabetes and cancer. Endocrinol Metab Clin North Am. 2014;43:167–85. https://doi.org/10.1016/j.ecl.2013.09.008.
Karlstad O, Starup-Linde J, Vestergaard P, Hjellvik V, Bazelier MT, Schmidt MK, et al. Use of insulin and insulin analogs and risk of cancer — systematic review and meta-analysis of observational studies. Curr Drug Saf. 2013;8:333–48. https://doi.org/10.2174/15680266113136660067.
Dahlén AD, Dashi G, Maslov I, Attwood MM, Jonsson J, Trukhan V, et al. Trends in antidiabetic drug discovery: FDA approved drugs, new drugs in clinical trials and global sales. Front Pharmacol. 2021;12:807548. https://doi.org/10.3389/fphar.2021.807548 (An updated review of currently available antihyperglycemic pharmacotherapies and future developments.).
Haas B, Eckstein N, Pfeifer V, Mayer P, Hass MD. Efficacy, safety and regulatory status of SGLT2 inhibitors: focus on canagliflozin. Nutr Diabetes. 2014;4: e143. https://doi.org/10.1038/nutd.2014.40.
Srivastava SP, Goodwin JE. Cancer biology and prevention in diabetes. Cells. 2020;9(6):1380. https://doi.org/10.3390/cells9061380 (A review of our understanding of the mechanistic links between diabetes and cancer.).
Alsaggaf R, Pfeiffer RM, Wang Y, St George DMM, Zhan M, Wagner KR, et al. Diabetes, metformin and cancer risk in myotonic dystrophy type I. Int J Cancer. 2020;147:785–92. https://doi.org/10.1002/ijc.32801 (A case-control study in more than 13,000 people demonstrating that diabetes confers increased cancer risk in patients with myotonic dystrophy type I but this increase is abolished among those treated with metformin.).
Wang Z, Bao C, Su C, Xu W, Luo H, Chen L, et al. Association between diabetes or antidiabetic therapy and lung cancer: a meta-analysis. J Diabetes Investig. 2013;4:659–66. https://doi.org/10.1111/jdi.12112.
Evans JMM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD. Metformin and reduced risk of cancer in diabetic patients. BMJ. 2005;330:1304–5. https://doi.org/10.1136/bmj.38415.708634.F7.
Bowker SL, Majumdar SR, Veugelers P, Johnson JA. Increased cancer-related mortality for patients with type 2 diabetes who use sulfonylureas or insulin. Diabetes Care. 2006;29:254–8. https://doi.org/10.2337/diacare.29.02.06.dc05-1558.
Zhang K, Bai P, Dai H, Deng Z. Metformin and risk of cancer among patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Prim Care Diabetes. 2021;15:52–8. https://doi.org/10.1016/j.pcd.2020.06.001 (A recent systematic review with meta-analysis of 67 studies with more than 10 million patients with diabetes, demonstrating that (i) those who have ever used metformin have 30% lower risk than those who have never used metofrmin, and (ii) metformin is associated with 20% lower risk compared with other antidiabetic medications.).
Ng CW, Jiang AA, Toh EMS, Ng CH, Ong ZH, Peng S, et al. Metformin and colorectal cancer: a systematic review, meta-analysis and meta-regression. Int J Colorectal Dis. 2020;35:1501–12. https://doi.org/10.1007/s00384-020-03676-x (A recent systematic review with meta-analysis of 58 studies in about 1.8 million patients with type 2 diabetes showing that metformin use is associated with reduced incidence of, and improved survival from, colorectal cancer.).
Farmer RE, Ford D, Forbes HJ, Chaturvedi N, Kaplan R, Smeeth L, et al. Metformin and cancer in type 2 diabetes: a systematic review and comprehensive bias evaluation. Int J Epidemiol. 2017;46:728–44. https://doi.org/10.1093/ije/dyw275.
Franciosi M, Lucisano G, Lapice E, Strippoli GF, Pellegrini F, Nicolucci A. Metformin therapy and risk of cancer in patients with type 2 diabetes: systematic review. PLoS ONE. 2013;8:e71583. https://doi.org/10.1371/journal.pone.0071583.
Dowling RJO, Zakikhani M, Fantus IG, Pollak M, Sonenberg N. Metformin inhibits mammalian target of rapamycin–dependent translation initiation in breast cancer cells. Cancer Res. 2007;67:10804–12. https://doi.org/10.1158/0008-5472.Can-07-2310.
Shaw RJ, Lamia KA, Vasquez D, Koo S-H, Bardeesy N, DePinho RA, et al. The kinase LKB1 mediates glucose homeostasis in liver and therapeutic effects of metformin. Science. 2005;310:1642–6. https://doi.org/10.1126/science.1120781.
Shackelford DB, Shaw RJ. The LKB1–AMPK pathway: metabolism and growth control in tumour suppression. Nat Rev Cancer. 2009;9:563–75. https://doi.org/10.1038/nrc2676.
Rena G, Hardie DG, Pearson ER. The mechanisms of action of metformin. Diabetologia. 2017;60:1577–85. https://doi.org/10.1007/s00125-017-4342-z.
Wu L, Zhu J, Prokop LJ, Murad MH. Pharmacologic therapy of diabetes and overall cancer risk and mortality: a meta-analysis of 265 studies. Sci Rep. 2015;5:10147. https://doi.org/10.1038/srep10147.
Tseng YH, Tsan YT, Chan WC, Sheu WH, Chen PC. Use of an alpha-glucosidase inhibitor and the risk of colorectal cancer in patients with diabetes: a nationwide, population-based cohort study. Diabetes Care. 2015;38:2068–74. https://doi.org/10.2337/dc15-0563.
Valent F. Diabetes mellitus and cancer of the digestive organs: an Italian population-based cohort study. J Diabetes Complicat. 2015;29:1056–61. https://doi.org/10.1016/j.jdiacomp.2015.07.017.
Zhao Y, Wang Y, Lou H, Shan L. Alpha-glucosidase inhibitors and risk of cancer in patients with diabetes mellitus: a systematic review and meta-analysis. Oncotarget. 2017;8:81027–39. https://doi.org/10.18632/oncotarget.17515.
Chen YL, Cheng KC, Lai SW, Tsai IJ, Lin CC, Sung FC, et al. Diabetes and risk of subsequent gastric cancer: a population-based cohort study in Taiwan. Gastric Cancer. 2013;16:389–96. https://doi.org/10.1007/s10120-012-0197-7.
Lai SW, Liao KF, Chen PC, Tsai PY, Hsieh DP, Chen CC. Antidiabetes drugs correlate with decreased risk of lung cancer: a population-based observation in Taiwan. Clin Lung Cancer. 2012;13:143–8. https://doi.org/10.1016/j.cllc.2011.10.002.
Lin CM, Huang HL, Chu FY, Fan HC, Chen HA, Chu DM, et al. Association between gastroenterological malignancy and diabetes mellitus and anti-diabetic therapy: a nationwide, population-based cohort study. PLoS ONE. 2015;10: e0125421. https://doi.org/10.1371/journal.pone.0125421.
Chang CH, Lin JW, Wu LC, Lai MS, Chuang LM, Chan KA. Association of thiazolidinediones with liver cancer and colorectal cancer in type 2 diabetes mellitus. Hepatology. 2012;55:1462–72. https://doi.org/10.1002/hep.25509.
Bosco JL, Antonsen S, Sorensen HT, Pedersen L, Lash TL. Metformin and incident breast cancer among diabetic women: a population-based case-control study in Denmark. Cancer Epidemiol Biomark Prev. 2011;20:101–11. https://doi.org/10.1158/1055-9965.EPI-10-08170.
Chen YC, Kok VC, Chien CH, Horng JT, Tsai JJ. Cancer risk in patients aged 30 years and above with type 2 diabetes receiving antidiabetic monotherapy: a cohort study using metformin as the comparator. Ther Clin Risk Manag. 2015;11:1315–23. https://doi.org/10.2147/TCRM.S91513.
Chiu CC, Huang CC, Chen YC, Chen TJ, Liang Y, Lin SJ, et al. Increased risk of gastrointestinal malignancy in patients with diabetes mellitus and correlations with anti-diabetes drugs: a nationwide population-based study in Taiwan. Intern Med. 2013;52:939–46. https://doi.org/10.2169/internalmedicine.52.8276.
Dabrowski M, Szymanska-Garbacz E, Miszczyszyn Z, Derezinski T, Czupryniak L. Risk factors for cancer development in type 2 diabetes: a retrospective case-control study. BMC Cancer. 2016;16:785. https://doi.org/10.1186/s12885-016-2836-6.
Kawaguchi T, Taniguchi E, Morita Y, Shirachi M, Tateishi I, Nagata E, et al. Association of exogenous insulin or sulphonylurea treatment with an increased incidence of hepatoma in patients with hepatitis C virus infection. Liver Int. 2010;30:479–86. https://doi.org/10.1111/j.1478-3231.2009.02191.x.
Kawamori R, Inagaki N, Araki E, Watada H, Hayashi N, Horie Y, et al. Linagliptin monotherapy provides superior glycaemic control versus placebo or voglibose with comparable safety in Japanese patients with type 2 diabetes: a randomized, placebo and active comparator-controlled, double-blind study. Diabetes Obes Metab. 2012;14:348–57. https://doi.org/10.1111/j.1463-1326.2011.01545.x.
Lai SW, Chen PC, Liao KF, Muo CH, Lin CC, Sung FC. Risk of hepatocellular carcinoma in diabetic patients and risk reduction associated with anti-diabetic therapy: a population-based cohort study. Am J Gastroenterol. 2012;107:46–52. https://doi.org/10.1038/ajg.2011.384.
Liao KF, Lai SW, Li CI, Chen WC. Diabetes mellitus correlates with increased risk of pancreatic cancer: a population-based cohort study in Taiwan. J Gastroenterol Hepatol. 2012;27:709–13. https://doi.org/10.1111/j.1440-1746.2011.06938.x.
Monami M, Colombi C, Balzi D, Dicembrini I, Giannini S, Melani C, et al. Metformin and cancer occurrence in insulin-treated type 2 diabetic patients. Diabetes Care. 2011;34:129–31. https://doi.org/10.2337/dc10-1287.
Nakamura T, Matsuda T, Kawagoe Y, Ogawa H, Takahashi Y, Sekizuka K, et al. Effect of pioglitazone on carotid intima-media thickness and arterial stiffness in type 2 diabetic nephropathy patients. Metabolism. 2004;53:1382–6. https://doi.org/10.1016/j.metabol.2004.05.013.
Origasa H, Lee SH, Nakagawa H, Kumagai N, Fuse H, Tobe K. Pioglitazone use and bladder cancer — hospital-based results from a nested case-control study in Japan. Jpn Pharmacol Ther. 2013;41:663–7.
Pan C, Yang W, Barona JP, Wang Y, Niggli M, Mohideen P, et al. Comparison of vildagliptin and acarbose monotherapy in patients with type 2 diabetes: a 24-week, double-blind, randomized trial. Diabet Med. 2008;25:435–41. https://doi.org/10.1111/j.1464-5491.2008.02391.x.
Simo R, Plana-Ripoll O, Puente D, Morros R, Mundet X, Vilca LM, et al. Impact of glucose-lowering agents on the risk of cancer in type 2 diabetic patients The Barcelona case-control study. PLoS One. 2013;8:e79968. https://doi.org/10.1371/journal.pone.0079968.
Son JW, Lee IK, Woo JT, Baik SH, Jang HC, Lee KW, et al. A prospective, randomized, multicenter trial comparing the efficacy and safety of the concurrent use of long-acting insulin with mitiglinide or voglibose in patients with type 2 diabetes. Endocr J. 2015;62:1049–57. https://doi.org/10.1507/endocrj.EJ15-0325.
Tseng CH. Diabetes and risk of prostate cancer: a study using the National Health Insurance. Diabetes Care. 2011;34:616–21. https://doi.org/10.2337/dc10-1640.
Tseng CH. Diabetes and risk of bladder cancer: a study using the National Health Insurance database in Taiwan. Diabetologia. 2011;54:2009–15. https://doi.org/10.1007/s00125-011-2171-z.
Tseng CH. Thyroid cancer risk is not increased in diabetic patients. PLoS ONE. 2012;7:e53096. https://doi.org/10.1371/journal.pone.0053096.
Tseng CH. Use of metformin and risk of kidney cancer in patients with type 2 diabetes. Eur J Cancer. 2016;52:19–25. https://doi.org/10.1016/j.ejca.2015.09.027.
Yang X, So WY, Ma RC, Yu LW, Ko GT, Kong AP, et al. Use of sulphonylurea and cancer in type 2 diabetes—the Hong Kong Diabetes Registry. Diabetes Res Clin Pract. 2010;90:343–51. https://doi.org/10.1016/j.diabres.2010.08.022.
Coyle C, Cafferty FH, Vale C, Langley RE. Metformin as an adjuvant treatment for cancer: a systematic review and meta-analysis. Ann Oncol. 2016;27:2184–95. https://doi.org/10.1093/annonc/mdw410.
Daugan M, Dufay Wojcicki A, d’Hayer B, Boudy V. Metformin: an anti-diabetic drug to fight cancer. Pharmacol Res. 2016;113:675–85. https://doi.org/10.1016/j.phrs.2016.10.006.
Liu Y, Jin PP, Sun XC, Hu TT. Thiazolidinediones and risk of colorectal cancer in patients with diabetes mellitus: a meta-analysis. Saudi J Gastroenterol. 2018;24:75–81. https://doi.org/10.4103/sjg.SJG_295_17.
Bosetti C, Rosato V, Buniato D, Zambon A, La Vecchia C, Corrao G. Cancer risk for patients using thiazolidinediones for type 2 diabetes: a meta-analysis. Oncologist. 2013;18:148–56. https://doi.org/10.1634/theoncologist.2012-0302.
Mamtani R, Haynes K, Bilker WB, Vaughn DJ, Strom BL, Glanz K, et al. Association between longer therapy with thiazolidinediones and risk of bladder cancer: a cohort study. J Natl Cancer Inst. 2012;104:1411–21. https://doi.org/10.1093/jnci/djs328.
Nagamine M, Okumura T, Tanno S, Sawamukai M, Motomura W, Takahashi N, et al. PPAR gamma ligand-induced apoptosis through a p53-dependent mechanism in human gastric cancer cells. Cancer Sci. 2003;94:338–43. https://doi.org/10.1111/j.1349-7006.2003.tb01443.x.
Cellai I, Petrangolini G, Tortoreto M, Pratesi G, Luciani P, Deledda C, et al. In vivo effects of rosiglitazone in a human neuroblastoma xenograft. Br J Cancer. 2010;102:685–92. https://doi.org/10.1038/sj.bjc.6605506.
Luconi M, Mangoni M, Gelmini S, Poli G, Nesi G, Francalanci M, et al. Rosiglitazone impairs proliferation of human adrenocortical cancer: preclinical study in a xenograft mouse model. Endocr Relat Cancer. 2010;17:169–77. https://doi.org/10.1677/erc-09-0170.
Cao C, Yang S, Zhou Z. GLP-1 receptor agonists and risk of cancer in type 2 diabetes: an updated meta-analysis of randomized controlled trials. Endocrine. 2019;66:157–65. https://doi.org/10.1007/s12020-019-02055-z.
Bethel MA, Patel RA, Merrill P, Lokhnygina Y, Buse JB, Mentz RJ, et al. Cardiovascular outcomes with glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes: a meta-analysis. Lancet Diabetes Endocrinol. 2018;6:105–13. https://doi.org/10.1016/s2213-8587(17)30412-6.
Monami M, Nreu B, Scatena A, Cresci B, Andreozzi F, Sesti G, et al. Safety issues with glucagon-like peptide-1 receptor agonists (pancreatitis, pancreatic cancer and cholelithiasis): data from randomized controlled trials. Diabetes Obes Metab. 2017;19:1233–41. https://doi.org/10.1111/dom.12926.
Piccoli GF, Mesquita LA, Stein C, Aziz M, Zoldan M, Degobi NAH, et al. Do GLP-1 receptor agonists increase the risk of breast cancer? A systematic review and meta-analysis. J Clin Endocrinol Metab. 2021;106:912–21. https://doi.org/10.1210/clinem/dgaa891 (A meta-analysis of 52 randomized controlled trials in patients with type 2 diabetes and/or obesity, who were treated with GLP-1 receptor agonists for at least 6 months. Results indicated that treatment did not increase the risk of breast neoplasms.).
Guo X, Yang Q, Dong J, Liao L, Zhang W, Liu F. Tumour risk with once-weekly glucagon-like peptide-1 receptor agonists in type 2 diabetes mellitus patients: a systematic review. Clin Drug Investig. 2016;36:433–41. https://doi.org/10.1007/s40261-016-0389-8.
Liu Y, Zhang X, Chai S, Zhao X, Ji L. Risk of malignant neoplasia with glucagon-like peptide-1 receptor agonist treatment in patients with type 2 diabetes: a meta-analysis. J Diabetes Res. 2019;2019:1534365. https://doi.org/10.1155/2019/1534365.
Shaefer CF Jr, Kushner P, Aguilar R. User’s guide to mechanism of action and clinical use of GLP-1 receptor agonists. Postgrad Med. 2015;127:818–26. https://doi.org/10.1080/00325481.2015.1090295.
Drucker DJ. Mechanisms of action and therapeutic application of glucagon-like peptide-1. Cell Metab. 2018;27:740–56. https://doi.org/10.1016/j.cmet.2018.03.001.
Bjerre Knudsen L, Madsen LW, Andersen S, Almholt K, de Boer AS, Drucker DJ, et al. Glucagon-like peptide-1 receptor agonists activate rodent thyroid C-cells causing calcitonin release and C-cell proliferation. Endocrinology. 2010;151:1473–86. https://doi.org/10.1210/en.2009-1272.
Smits MM, Van Raalte DH. Safety of semaglutide. Front Endocrinol. 2021;12:645563. https://doi.org/10.3389/fendo.2021.645563 (An overview of the safety aspects of the most popular and effective (at present) GLP-1 receoptor agonist, concluding there is overall low risk for severe adverse events, including pancreatic and thyroid cancers.).
Zhang X, Wang M, Wang X, Zhu Z, Zhang W, Zhou Z, et al. Comparison of new glucose-lowering drugs on the risk of pancreatitis in type 2 diabetes: a network meta-analysis. Endocr Pract. 2022;28:333–41. https://doi.org/10.1016/j.eprac.2021.12.007 (A meta-analysis of 17 studies with more than 100,000 patients with type 2 diabetes demonstrating that GLP-1 agonists and DPP-4 inhibitors do not increase the risk for pancreatic cancer.).
Zhang Z, Chen X, Lu P, Zhang J, Xu Y, He W, et al. Incretin-based agents in type 2 diabetic patients at cardiovascular risk: compare the effect of GLP-1 agonists and DPP-4 inhibitors on cardiovascular and pancreatic outcomes. Cardiovasc Diabetol. 2017;16:31. https://doi.org/10.1186/s12933-017-0512-z.
Abd El Aziz M, Cahyadi O, Meier JJ, Schmidt WE, Nauck MA. Incretin-based glucose-lowering medications and the risk of acute pancreatitis and malignancies: a meta-analysis based on cardiovascular outcomes trials. Diabetes Obes Metab. 2020;22:699–704. https://doi.org/10.1111/dom.13924 (A meta-analysis of 11 randomized, placebo-controlled, prospective cardiovascular outcomes studies with GLP-1 receptor agonists and DPP-4 inhibitors that found no increase in the risk for pancreatic cancer.).
Dicembrini I, Nreu B, Montereggi C, Mannucci E, Monami M. Risk of cancer in patients treated with dipeptidyl peptidase-4 inhibitors: an extensive meta-analysis of randomized controlled trials. Acta Diabetol. 2020;57:689–96. https://doi.org/10.1007/s00592-020-01479-8 (A meta-analysis of 157 placebo-controlled trials with more than 60,000 patients with type 2 diabetes per arm, demonstrating that use of DPP-4 inhibitors is not associated with the risk for overall cancer, and may in fact have beneficial effect on colorectal cancer risk (30% reduction).).
Thornberry NA, Gallwitz B. Mechanism of action of inhibitors of dipeptidyl-peptidase-4 (DPP-4). Best Pract Res Clin Endocrinol Metab. 2009;23:479–86. https://doi.org/10.1016/j.beem.2009.03.004.
Metzemaekers M, Van Damme J, Mortier A, Proost P. Regulation of chemokine activity — a focus on the role of dipeptidyl peptidase IV/CD26. Front Immunol. 2016;7:483. https://doi.org/10.3389/fimmu.2016.00483.
Yang F, Takagaki Y, Yoshitomi Y, Ikeda T, Li J, Kitada M, et al. Inhibition of dipeptidyl peptidase-4 accelerates epithelial-mesenchymal transition and breast cancer metastasis via the CXCL12/CXCR4/mTOR axis. Cancer Res. 2019;79:735–46. https://doi.org/10.1158/0008-5472.Can-18-0620.
Li S, Fan Y, Kumagai A, Kawakita E, Kitada M, Kanasaki K, et al. Deficiency in dipeptidyl peptidase-4 promotes chemoresistance through the CXCL12/CXCR4/mTOR/TGFβ signaling pathway in breast cancer cells. Int J Mol Sci. 2020;21:805. https://doi.org/10.3390/ijms21030805 (A cell culture and animal model study showing that DPP-4 inhibitors potentiate chemotherapy resistance via the induction of ABC transporters by the CXCL12/CXCR4/mTOR/TGFβ signaling pathway in breast cancer cells.).
Mortier A, Gouwy M, Van Damme J, Proost P, Struyf S. CD26/dipeptidylpeptidase IV-chemokine interactions: double-edged regulation of inflammation and tumor biology. J Leukoc Biol. 2016;99:955–69. https://doi.org/10.1189/jlb.3MR0915-401R.
Lin HW, Tseng CH. A review on the relationship between SGLT2 inhibitors and cancer. Int J Endocrinol. 2014;2014: 719578. https://doi.org/10.1155/2014/719578.
Burki TK. FDA rejects novel diabetes drug over safety fears. Lancet. 2012;379:507. https://doi.org/10.1016/s0140-6736(12)60216-5.
US Department of Health and Human Services. FDA briefing document — NDA 202293: dapagliflozin tablets, 5 and 10mg; 2011. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2014/202293Orig1s000ltr.pdf. Accessed 23 Nov 2022.
Tang H, Dai Q, Shi W, Zhai S, Song Y, Han J. SGLT2 inhibitors and risk of cancer in type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. Diabetologia. 2017;60:1862–72. https://doi.org/10.1007/s00125-017-4370-8.
Scafoglio C, Hirayama BA, Kepe V, Liu J, Ghezzi C, Satyamurthy N, et al. Functional expression of sodium-glucose transporters in cancer. Proc Natl Acad Sci U S A. 2015;112:E4111–9. https://doi.org/10.1073/pnas.1511698112.
Lutz SZ, Staiger H, Fritsche A, Haring HU. Antihyperglycaemic therapies and cancer risk. Diab Vasc Dis Res. 2014;11:371–89. https://doi.org/10.1177/1479164114549553.
Greco DS, Broussard JD, Peterson ME. Insulin therapy. Vet Clin North Am Small Anim Pract. 1995;25:677–89. https://doi.org/10.1016/s0195-5616(95)50062-2.
Haller MJ, Atkinson MA, Schatz D. Type 1 diabetes mellitus: etiology, presentation, and management. Pediatr Clin North Am. 2005;52:1553–78. https://doi.org/10.1016/j.pcl.2005.07.006.
Baron V, Van Obberghen E. Mechanism of insulin action. C R Seances Soc Biol Fil. 1995;189:25–41.
Home P. Insulin therapy and cancer. Diabetes Care. 2013;36(Suppl 2):S240–4. https://doi.org/10.2337/dcS13-2002.
Pollak M, Russell-Jones D. Insulin analogues and cancer risk: cause for concern or cause celebre? Int J Clin Pract. 2010;64:628–36. https://doi.org/10.1111/j.1742-1241.2010.02354.x.
Hernandez-Diaz S, Adami HO. Diabetes therapy and cancer risk: causal effects and other plausible explanations. Diabetologia. 2010;53:802–8. https://doi.org/10.1007/s00125-010-1675-2.
Pocock SJ, Smeeth L. Insulin glargine and malignancy: an unwarranted alarm. Lancet. 2009;374:511–3. https://doi.org/10.1016/S0140-6736(09)61307-6.
Renehan AG. Insulin analogues and cancer risk: the emergence of second-generation studies. Diabetologia. 2012;55:7–9. https://doi.org/10.1007/s00125-011-2352-9.
Suissa S, Azoulay L. Metformin and the risk of cancer: time-related biases in observational studies. Diabetes Care. 2012;35:2665–73. https://doi.org/10.2337/dc12-0788.
Dejgaard A, Lynggaard H, Rastam J, Krogsgaard TM. No evidence of increased risk of malignancies in patients with diabetes treated with insulin detemir: a meta-analysis. Diabetologia. 2009;52:2507–12. https://doi.org/10.1007/s00125-009-1568-4.
Investigators OT, Gerstein HC, Bosch J, Dagenais GR, Diaz R, Jung H, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med. 2012;367:319–28. https://doi.org/10.1056/NEJMoa1203858.
Carstensen B, Witte DR, Friis S. Cancer occurrence in Danish diabetic patients: duration and insulin effects. Diabetologia. 2012;55:948–58. https://doi.org/10.1007/s00125-011-2381-4.
Li D, Tang H, Hassan MM, Holly EA, Bracci PM, Silverman DT. Diabetes and risk of pancreatic cancer: a pooled analysis of three large case-control studies. Cancer Causes Control. 2011;22:189–97. https://doi.org/10.1007/s10552-010-9686-3.
Li D, Yeung SC, Hassan MM, Konopleva M, Abbruzzese JL. Antidiabetic therapies affect risk of pancreatic cancer. Gastroenterology. 2009;137:482–8. https://doi.org/10.1053/j.gastro.2009.04.013.
Mizuno S, Nakai Y, Isayama H, Yanai A, Takahara N, Miyabayashi K, et al. Risk factors and early signs of pancreatic cancer in diabetes: screening strategy based on diabetes onset age. J Gastroenterol. 2013;48:238–46. https://doi.org/10.1007/s00535-012-0622-z.
Thakkar B, Aronis KN, Vamvini MT, Shields K, Mantzoros CS. Metformin and sulfonylureas in relation to cancer risk in type II diabetes patients: a meta-analysis using primary data of published studies. Metabolism. 2013;62:922–34. https://doi.org/10.1016/j.metabol.2013.01.014.
Mekuria AN, Ayele Y, Tola A, Mishore KM. Monotherapy with metformin versus sulfonylureas and risk of cancer in type 2 diabetic patients: a systematic review and meta-analysis. J Diabetes Res. 2019;2019:7676909. https://doi.org/10.1155/2019/7676909.
Author information
Authors and Affiliations
Contributions
C.S.S. and P.N.E. were involved in study conceptualization, data extraction, analysis, methodology, visualization, and writing the original draft. M.D. was involved in reviewing and editing the manuscript. F.M. was involved in study conceptualization, data extraction, methodology, supervision, visualization, and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have any potential conflicts of interest to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Søndergaard, C.S., Esquivel, P.N., Dalamaga, M. et al. Use of Antihyperglycemic Drugs and Risk of Cancer in Patients with Diabetes. Curr Oncol Rep 25, 29–40 (2023). https://doi.org/10.1007/s11912-022-01344-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-022-01344-7