Abstract
Purpose of Review
This review summarizes the current FDA practice in developing risk- and evidence-based product-specific bioequivalence guidances for antiepileptic drugs (AEDs).
Recent Findings
FDA’s product-specific guidance (PSG) for AEDs takes into account the therapeutic index of each AED product. Several PSGs for AEDs recommend fully replicated studies and a reference-scaled average bioequivalence (RS-ABE) approach that permit the simultaneous equivalence comparison of the mean and within-subject variability of the test and reference products.
Summary
The PSGs for AEDs published by FDA reflect the agency’s current thinking on the bioequivalence studies and approval standards for generics of AEDs. Bioequivalence between brand and generic AED products demonstrated in controlled studies with epilepsy patients provides strong scientific support for the soundness of FDA bioequivalence standards.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy is a neurological condition characterized as an enduring predisposition to generate epileptic seizures [1]. The number of people having epilepsy is estimated to be about 65 million worldwide [2], making it one of the most common neurological diseases. Epilepsy is more common in children younger than 2 years old and adults’ age of 65 years and older [3]. Epilepsy-related conditions such as cognitive problems, depression, and anxiety can be chronic and disabling. Although genetic factors, brain conditions, infectious diseases, and developmental disorders may play a role in the etiology of epilepsy disorders, cause of epilepsy remains unknown in many patients.
Current treatment options for epilepsy include medications, surgery, implantable devices, and dietary therapies. While surgery and medical devices are effective in some epilepsy patients, antiepileptic drug (AED) therapy is the current mainstay of epilepsy treatment. The American Academy of Neurology (AAN), the American Epilepsy Society (AES), and other professional organizations have issued evidence-based guidelines for the management of epilepsy [4]. Current clinical evidence indicates that most patients with newly diagnosed epilepsy respond to the first one or two AEDs and their seizure conditions can be completely controlled with a maintenance dose of AEDs [5]. Surgical procedures and medical devices are alternative options for the remaining patients whose seizures cannot be effectively controlled by AEDs.
Over 20 new FDA-approved new drug substances have entered the AED market over the past few decades [6••]. The availability of these AEDs has translated into good control of epileptic seizures in patients. For many patients, epilepsy is a life-long condition requiring chronic AEDs to achieve and maintain seizure control. AED medication compliance is a particular concern for breakthrough seizures. With more generics of AEDs becoming available for patients, AED medications are becoming more affordable and patient compliance is likely to be facilitated [7].
Before any generic AED can enter the US market, it must meet FDA’s high standards for approval. In general, a generic manufacturer submits an Abbreviated New Drug Application (ANDA) to the FDA for review and approval. ANDAs rely on the previously established safety and efficacy of the brand name product, or reference listed drug (RLD) it copies. To ensure that generics are therapeutically equivalent to the RLD, they must show pharmaceutical equivalence together with bioequivalence to the RLD. Bioequivalence is defined as the absence of a significant difference in the rate and extent to which the active ingredient or active moiety in pharmaceutical equivalents or pharmaceutical alternatives becomes available at the site of drug action when administered at the same molar dose under similar conditions in an appropriately designed study [8]. In 2013, FDA issued the revised draft guidance, Bioequivalence Studies with Pharmacokinetic Endpoints for Drugs Submitted under an ANDA, that provides FDA’s general and current thinking on bioequivalence study designs and bioequivalence standards [9]. FDA also published the guidance Statistical Approaches to Establishing Bioequivalence in 2001 [10].
The issue of AED generic substitution and possible impact on therapeutic effect has been debated for many years. FDA continuously monitors and reviews this issue and has found insufficient evidence to indicate that the use of generic AEDs may lead to therapeutic failure or increased risk of adverse events or that the use of FDA-approved generic anticonvulsants results in an increased frequency of seizures [11, 12•]. Additionally, there has been some general misunderstanding of FDA’s criteria for demonstrating bioequivalence. To establish bioequivalence, the calculated 90% confidence interval (CI) for geometric mean ratios for AUC (area under the concentration-time curve) and C max (peak serum/plasma concentration) values between the generic product and the RLD generally should fall entirely within an 80.00 to 125.00% acceptance interval. Because the entire 90% CI has to fall within the 80.00–125.00% range, the actual mean pharmacokinetic values of the generic drug must be very close to the mean pharmacokinetic value of the RLD. In a review of 12 years of bioequivalence data submitted to FDA, the average differences in C max and AUC value between approved generic products and respective RLD were observed to be 4.35 and 3.56%, respectively [13].
As the type of studies and evidence required to establish bioequivalence can be different for each AED product, FDA routinely conducts internal research and develops product-specific guidances (PSGs). PSGs describe the agency’s current thinking and recommendations on the bioequivalence studies for individual generic products. FDA has issued PSGs for most AED products through the FDA webpage [14]. Table 1 summarizes the PSGs for AED products that include oral tablets, capsules, disintegrating tablets, suspensions and syrups, and some intravenous solutions.
This review focuses on the FDA-recommended in vivo studies for bioequivalence testing of AED products. Consistent with the widely used classification of AEDs based on their respective approval dates, generic bioequivalence is described the in the context of first, second, and newer generation AEDs.
First-Generation AEDs
First-generation AEDs are those that initially entered the market before the 1990s and include phenytoin, trimethadione, primidone, methsuximide, ethotoin, ethosuximide, acetazolamide, diazepam, carbamazepine, clonazepam, valproic acid, valproate sodium, and divalproex. While phenobarbital is considered a first-generation AED, it is not in this review because it is currently marketed as an unapproved drug product [15].
FDA considers four of these first-generation AEDs, phenytoin, carbamazepine, valproic acid, and divalproex, narrow therapeutic index (NTI) drugs [14]. These four AEDs have little separation between therapeutical and toxic concentrations with an estimated therapeutic index of around 2. For instance, phenytoin has a therapeutic concentration range of 10–20 mcg/mL, with serious dose-related adverse events observed more frequently at plasma concentrations above 20 mcg/mL [16, 17]. The therapeutic serum concentration range for carbamazepine is considered to be 4–12 mcg/mL [18]. The serum carbamazepine concentration at the first occurrence of the typical adverse event could be as low as 10 mcg/mL [19], while concentrations above 20 mcg/mL are considered comatose-fatal [20]. Valproic acid has a therapeutic concentration range of 50–100 mcg/mL and the toxic concentration is about 100 mcg/mL [21]. In addition, due to the steep exposure-response relationship for efficacy (i.e., seizure control), patients with sub-therapeutic concentrations may have a higher risk of therapeutic failure. As a result, phenytoin, carbamazepine, valproic acid, and divalproex are subject to routine therapeutic drug monitoring based on serum/plasma drug concentrations. Doses for these four drugs are often adjusted in very small increments (< 20%). These four products have within-subject variability of less than 30% in drug exposure. NTI drugs generally have low within-subject variability because with a combination of a steep exposure-response relationship and high variation in drug exposure, patients would be at risk of serious lack of efficacy or adverse events due to normal variations in drug exposure.
To ensure therapeutic equivalence of generic NTI AEDs to the RLD they copy, FDA recommends a four-way, fully replicated, crossover study design for in vivo testing and reference-scaled average bioequivalence (RS-ABE) approach for data analysis [12•, 22•]. Since 2014, FDA has revised the PSGs for the first-generation AED products that demonstrate characteristics of NTI drugs to incorporate these recommendations (Table 1). In the RS-ABE approach, the bioequivalence limits are scaled based on the within-subject standard deviation of reference product from a fully replicated, crossover study (Table 2). In addition, comparison of the within-subject standard deviation of test and reference products ensures equivalent therapeutic performance. As an example, details of the statistical analysis using the RS-ABE approach can be found in the PSG for warfarin sodium oral tablet, an anticoagulant NTI drug product [23].
For the other first-generation AED products that are not considered NTI drugs, the average bioequivalence approach is used for bioequivalence assessment of pharmacokinetic data obtained from two-way crossover studies in healthy adult subjects. The 90% CI for the test-to-reference ratio of geometric means should fall within the bioequivalence limits of 80.00–125.00% for C max and AUC [10].
Second-Generation AEDs
The pharmaceutical industry successfully developed and introduced 13 new drug substances to the US market between 1990 and 2010. These drugs are felbamate, gabapentin, lamotrigine, fosphenytoin, topiramate, tiagabine, levetiracetam, oxcarbazepine, zonisamide, pregabalin, rufinamide, lacosamide, and vigabatrin. Based on literature reports [24], many of these drugs greatly improve the treatment of epilepsy because of a more favorable pharmacokinetic property and/or a better safety and efficacy profile due to less adverse effects and fewer drug interactions. Many second-generation brand name AEDs have recently or will soon lose patent and exclusivity protection, creating a significant opportunity for the development and approval of generic versions of these AEDs. To date, FDA has developed 23 PSGs (Table 1) for these second-generation AED products.
For the most part, FDA does not consider second-generation AED products to be NTI drugs. For instance, the therapeutic index of lamotrigine is estimated to vary largely among patients, up to 20 in a recent systematic review of available literature data [25]. Since the available evidence does not indicate that lamotrigine is an NTI drug, therapeutic drug monitoring is not routinely implemented [26].
Immediate-release products containing tiagabine, levetiracetam, pregabalin, and lacosamide are highly permeable and soluble and are considered to be Biopharmaceutics Classification System (BCS) class I drugs [27]. As a result, generic manufactures of these immediate-release solid oral products may request a waiver of in vivo testing, provided that the drug product is rapidly dissolving and excipients in the product do not affect the rate or extent of absorption of the drug. Although a waiver of in vivo bioequivalence testing is an option, many of the FDA-approved IR solid oral dosage forms of tiagabine, levetiracetam, and lacosamide have been tested for bioequivalence using in vivo studies under fed and fasting conditions. A few pregabalin oral capsule generics have a “tentative approval” status, meaning that they have met FDA’s scientific standards for approval, but cannot be approved until unexpired patents or exclusivity issues are resolved.
While most in vivo bioequivalence studies for AED products use healthy subjects, FDA recommends epilepsy patients when evaluating bioequivalence of felbamate and vigabatrin products due to risks associated with these products. Felbamate products have a boxed warning based on the risk of aplastic anemia and acute hepatic failure [28]. Therefore, the safety concerns from life-threatening adverse events of aplastic anemia and acute hepatic failure may preclude enrolling health subjects for the bioequivalence evaluation. Bioequivalence testing for this product should only be conducted in epilepsy patients already established on felbamate monotherapy or adjunctive therapy. Similarly, vigabatrin products have a boxed warning regarding the serious risk of permanent bilateral concentric visual field constriction and vision loss [29]. Therefore, FDA recommends bioequivalence studies in adult patients with refractory complex partial seizures who are already on established vigabatrin adjunctive therapy. When conducting bioequivalence study in patients, attainment of steady state should be confirmed with at least three consecutive measurements of plasma drug concentrations prior to dosing. Peak drug concentrations during a dosing interval at a steady state (C maxSS) and AUC over a dosing interval at a steady state (AUC0-tau) should be assessed [9]. In addition, other pharmacokinetic metrics such as concentration at the end of a dosing interval (C minSS), average concentration during a dosing interval (C avSS), degree of fluctuation [(C max − C min)/C avSS], swing [(C maxSS − C minSS)/C avSS], and time to peak concentration (T max) should be reported as supportive information [9].
Newer AEDs
Over the past few years, FDA has approved five new drugs for the management of epilepsy. Clobazam is a member of the benzodiazepine class that includes first-generation AEDs such as diazepam and clonazepam. While it has been clinically used worldwide for about 40 years, clobazam oral formulations were approved by FDA as an adjunctive treatment of seizures associated with Lennox-Gastaut syndrome in 2011 [30•]. Eslicarbazepine, a third-generation dibenzazepine AED, is indicated for the treatment of partial-onset seizures as monotherapy or adjunctive therapy [31]. Brivaracetam, a levetiracetam analog, was approved by FDA as adjunctive therapy in the treatment of partial-onset seizures in 2016 [32]. Ezogabine and perampanel are two novel AEDs unique in the chemical structure and mechanism of action. There are no approved generics for newer generation AEDs due to patents and exclusivity [6••]. Nevertheless, FDA has reviewed product information, clinical pharmacokinetic, and safety data from their original new drug applications and issued PSGs for all except brivaracetam which was approved in 2016. FDA does not considered any of these products to be NTI drugs. Therefore, the PSGs for these products recommend a single-dose, two-way crossover study design for bioequivalence studies in healthy subjects under fasting and fed conditions. For perampanel, adequate washout period between treatments should be considered given that it has a long terminal half-life (about 105 h) [33]. Alternatively, a single-dose, parallel study design can be considered where a separate group of healthy subjects with similar demographics is enrolled [9]. C max and an AUC truncated at 72 h (AUC0–72 h) can be used to characterize peak and drug exposure for the purpose of bioequivalence assessment [14].
Lamotrigine Bioequivalence Studies Funded by FDA: a Case Example
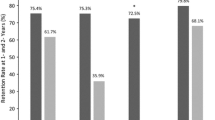
Lamotrigine is one of the most commonly prescribed AEDs due to its broad-spectrum efficacy, good tolerability, and availability in generic forms [34]. To date, FDA has approved lamotrigine generics in all four oral dosage forms: immediate-release (IR) tablet, extended-release (ER) tablet, chewable tablet, and orally disintegrating tablet (ODT). For each oral dosage form, there are multiple generics available on the US market (Fig. 1). Over the last decade, neurologists have raised concerns about the risk of switching to a generic from a brand lamotrigine product or another generic in epilepsy patients [35, 36]. To address neurologists’ concerns, FDA has funded a series of postmarket studies on lamotrigine products since 2010. Specifically, a Bioequivalence in Epilepsy Patients (BEEP) study (ClinicalTrials.gov identifier NCT01995825) was to evaluate the pharmacokinetic performance of the brand name lamotrigine IR product, LAMICTAL® (manufactured by GlaxoSmithKline), against a generic lamotrigine IR product in epilepsy patients which was reported to have a potential problem with generic switching [37••]. The BEEP study was conducted using a randomized, single-center, double-blinded, multiple-dose, steady-state, fully replicated, crossover study design. The study results demonstrated that the generic and brand lamotrigine IR products are bioequivalent in epilepsy patients, validating FDA’s recommendation of in vivo testing in healthy subject and approval standards for generic lamotrigine IR products (i.e., the conventional 80.00–125.00% acceptance limit). This study also demonstrated similar seizure control and tolerability in the vast majority of epilepsy patients. Another study, Equivalence among Generic AEDs (EQUIGEN, ClinicalTrials.gov identifier NCT01713777), evaluated whether generic lamotrigine IR products from different manufacturers are bioequivalent in epilepsy patients receiving concomitant AEDs [38••]. This multiple-dose study was conducted using a randomized, double-blinded, fully replicated, crossover design. Similar to the results from the BEEP study, the EQUIGEN study demonstrated that two generic lamotrigine IR products are bioequivalent in epilepsy patients and loss of seizure control or unanticipated adverse events are not evident. Of note, the two generics were the most disparate to each other (but in the allowable range of difference from the brand) in terms of their bioequivalence measures and inactive ingredients in the formulation in their FDA application. Because a multiple-dose study may be less sensitive than a single-dose study in detecting formulation differences between the drug products, a bioequivalence study of LAMICTAL® and these two disparate generic lamotrigine IR products was conducted using a single-dose, three-sequence, six-period replicate study design. The study results demonstrated brand to generic as well as generic to generic equivalence in patients with epilepsy (NCT01733394) [39]. Additionally, the within-subject variability of LAMICTAL® and two generics is similar and relatively low (i.e., < 15%) in epilepsy patients. This EQUIGEN study specifically addressed neurologists’ concerns regarding switches among multiple generic AEDs which may have variable differences from the RLD.
Overall, the BEEP and EQUIGEN studies conducted in patients with epilepsy confirm that the current FDA bioequivalence standards are appropriate for lamotrigine IR formulations. Based on these study results, the AES issued a statement acknowledging that drug formulation substitution with FDA-approved generic AEDs does not compromise efficacy in January 2016 [40••]. Of note, a recent case-crossover study using the Medicaid Analytic eXtract and a US commercial health insurance database concluded that switching between different manufacturers of the same generic AED appears to be safe [41•].
Generic modified-release (MR) product may have different control release mechanism and formulation design from those of the brand AED [42•]. A neurologist has some remaining concerns regarding substitutability of generic MR AEDs [43•]. To ensure therapeutic equivalence for lamotrigine MR products, FDA has established a risk-analysis platform which integrates knowledge in formulation design, clinical studies, modeling and simulation, and postmarket surveillance [44]. Besides statistic assessment on C max and AUC, we routinely evaluate T max differences in the clinical context for generic MR products. FDA also sponsored additional studies on generic MR AED products, e.g., a recent study (NCT02821338) of a generic lamotrigine ER and LAMICTAL® XR tablet products in healthy subjects under fed conditions will help confirm product bioequivalence and provide insights on brand-to-generic AED MR product switching.
Multiple-Dose Versus Single-Dose Bioequivalence Studies
Some AEDs have nonlinear pharmacokinetic properties. For instance, phenytoin can saturate its own metabolism after repeated dose administration. Carbamazepine is an inducer of certain CYP enzymes, so it can auto-induce its own clearance. Therefore, its clearance following repeated oral administration is greater than that following a single-dose administration. Based on these drug metabolism findings, Tothfalusi et al. raised a concern that AED products with established bioequivalence in single-dose bioequivalence studies in healthy subjects may not be bioequivalent in epilepsy patients [45]. To address this concern, a population physiological-based pharmacokinetic (PBPK) model and clinical trial simulations of bioequivalence studies were conducted [46]. The study demonstrated that the FDA’s recommended fully replicated single-dose bioequivalence studies with the RS-ABE approach in healthy subjects can ensure bioequivalence in patients following chronic treatment. Therefore, the FDA-recommended single-dose bioequivalence study for carbamazepine is sensitive in detecting both changes in the extent of bioavailability and changes in in vitro drug release profiles associated with formulation changes. Similarly, results from phenytoin modeling work showed that the RS-ABE approach based on the currently recommended single-dose fully replicated bioequivalence studies is appropriate and ensures BE following chronic dosing.
Concluding Remarks
Bioequivalence for generic AEDs is critical for epilepsy management. FDA routinely conducts research to develop risk- and evidence-based bioequivalence recommendations for AEDs. In the case of AEDs that demonstrated characteristics of NTI drugs, FDA recommends a specific bioequivalence approach which permits the simultaneous equivalence comparison of the mean and within-subject variability of the test and reference products. For felbamate and vigabatrin products, safety concerns preclude the use of healthy subjects and FDA recommends bioequivalence testing in epilepsy patients stable on these AEDs. For IR solid oral dosage forms of high solubility and high permeability drug substance, a waiver of in vivo bioequivalence testing can be considered. Moreover, several FDA-funded clinical studies not only demonstrate therapeutic equivalence of lamotrigine products in epilepsy patients but also support current FDA approval standards and bioequivalence criteria. These clinical findings further provide assurance on the safety and efficacy of generic substitution.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fisher RS, van Emde Boas W, Blume W, Elger C, Genton P, Lee P, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005;46(4):470–2. https://doi.org/10.1111/j.0013-9580.2005.66104.x.
Institute of Medicine (US) Committee on the Public Health Dimensions of the Epilepsies. Epilepsy across the Spectrum: promoting health and understanding. Washington (DC): National Academic Press (US); 2012.
Epilepsy, One of the Nation’s Most Common Neurological Conditions at a Glance 2016. https://www.cdc.gov/chronicdisease/resources/publications/AAG/epilepsy.htm.
Practice Guidelines for Epilepsy. https://www.aan.com/Guidelines/Home/ByTopic?topicId=23.
Brodie MJ, Barry SJ, Bamagous GA, Norrie JD, Kwan P. Patterns of treatment response in newly diagnosed epilepsy. Neurology. 2012;78(20):1548–54. https://doi.org/10.1212/WNL.0b013e3182563b19.
•• Orange Book: approved drug products with therapeutic equivalence evaluations. 2017. https://www.accessdata.fda.gov/scripts/cder/ob/default.cfm. The Orange Book identifies brand and generic drug products approved on the basis of safety and effectiveness by the FDA.
Paschal AM, Rush SE, Sadler T. Factors associated with medication adherence in patients with epilepsy and recommendations for improvement. Epilepsy Behav. 2014;31:346–50. https://doi.org/10.1016/j.yebeh.2013.10.002.
Title 21, Code of Federal Regulations, Section 314.3. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=314.3.
Draft guidance for industry: bioequivalence studies with pharmacokinetic endpoints for drugs submitted under an Abbreviated New Drug Application. 2013. https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM377465.pdf.
Guidance for industry: statistical approaches to establishing bioequivalence. 2001. https://www.fda.gov/downloads/drugs/guidances/ucm070244.pdf.
FDA policy on generic anticonvulsants. SCRIP. 1989;1469:28–9.
• LX Y, Jiang W, Zhang X, Lionberger R, Makhlouf F, Schuirmann DJ, et al. Novel bioequivalence approach for narrow therapeutic index drugs. Clin Pharmacol Ther. 2015;97(3):286–91. https://doi.org/10.1002/cpt.28. Summary of FDA-proposed bioequivalence study design and related data analysis for NTI drugs.
Davit BM, Nwakama PE, Buehler GJ, Conner DP, Haidar SH, Patel DT, et al. Comparing generic and innovator drugs: a review of 12 years of bioequivalence data from the United States Food and Drug Administration. Ann Pharmacother. 2009;43(10):1583–97. https://doi.org/10.1345/aph.1M141.
Product-specific guidances for generic drug development. https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm075207.htm.
Yasiry Z, Shorvon SD. How phenobarbital revolutionized epilepsy therapy: the story of phenobarbital therapy in epilepsy in the last 100 years. Epilepsia. 2012;53(Suppl 8):26–39. https://doi.org/10.1111/epi.12026.
Product label of phenytoin chewable tablets. 2015. http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/084427Orig1s032lbl.pdf.
Product label of phenytoin oral suspension. 2016. http://www.accessdata.fda.gov/drugsatfda_docs/label/2016/008762s057s058lbl.pdf.
Product label of carbamazepine extended-release tablets. 2015. http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/016608s097,018281s045,018927s038,020234s026lbl.pdf. Accessed Aug 2015.
Specht U, May TW, Rohde M, Wagner V, Schmidt RC, Schutz M, et al. Cerebellar atrophy decreases the threshold of carbamazepine toxicity in patients with chronic focal epilepsy. Arch Neurol. 1997;54(4):427–31.
Spiller HA, Krenzelok EP, Cookson E. Carbamazepine overdose: a prospective study of serum levels and toxicity. J Toxicol Clin Toxicol. 1990;28(4):445–58.
Product label of valproic acid capsules. Mar 2017. http://www.accessdata.fda.gov/drugsatfda_docs/label/2017/018081s066,018082s049lbl.pdf.
• Jiang W, Makhlouf F, Schuirmann DJ, Zhang X, Zheng N, Conner D, et al. A bioequivalence approach for generic narrow therapeutic index drugs: evaluation of the reference-scaled approach and variability comparison criterion. AAPS J. 2015;17(4):891–901. https://doi.org/10.1208/s12248-015-9753-5. Evaluation of different bioequivalence approaches for NTI drugs using modeling and simulation.
Draft guidance on warfarin sodium oral tablets. https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM201283.pdf.
French JA, Gazzola DM. New generation antiepileptic drugs: what do they offer in terms of improved tolerability and safety? Ther Adv Drug Saf. 2011;2(4):141–58. https://doi.org/10.1177/2042098611411127.
Privitera M, Welty T, Gidal B, Carlson C, Pollard J, Berg M. How do clinicians adjust lamotrigine doses and use lamotrigine blood levels?—a Q-PULSE survey. Epilepsy Curr. 2014;14(4):218–23. https://doi.org/10.5698/1535-7597-14.4.218.
Cai W, Ting T, Polli J, Berg M, Privitera M, Jiang W. Lamotrigine, a narrow therapeutic index drug or not? Am Acad Neurol Ann Meet Philadelphia Abstract. 2014;P4:267.
Draft guidance for industry: waiver of in vivo bioavailability and bioequivalence studies for immediate-release solid oral dosage forms based on a biopharmaceutics classification system. 2015. https://www.fda.gov/downloads/Drugs/Guidances/ucm070246.pdf.
Product label of felbamate tablets and oral suspension. Jul 2011. http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/020189s023lbl.pdf.
Product label of vigabatrin tablet and oral solution. Jun 2016. http://www.accessdata.fda.gov/drugsatfda_docs/label/2016/020427Orig1s014,022006Orig1s015bl.pdf.
• Gauthier AC, Mattson RH. Clobazam: a safe, efficacious, and newly rediscovered therapeutic for epilepsy. CNS Neurosci Ther. 2015;21(7):543–8. https://doi.org/10.1111/cns.12399. A review of clobazam safety and efficacy.
Product label of eslicarbazepine acetate oral tablets. 2015. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/022416s001lbl.pdf.
Rogawski MA. Brivaracetam: a rational drug discovery success story. Br J Pharmacol. 2008;154(8):1555–7. https://doi.org/10.1038/bjp.2008.221.
Product label of perampanel oral tablets and oral suspension. 2016. http://www.accessdata.fda.gov/drugsatfda_docs/label/2016/208277s000lbl.pdf.
Werz MA. Pharmacotherapeutics of epilepsy: use of lamotrigine and expectations for lamotrigine extended release. Ther Clin Risk Manag. 2008;4(5):1035–46.
LeLorier J, Duh MS, Paradis PE, Lefebvre P, Weiner J, Manjunath R, et al. Clinical consequences of generic substitution of lamotrigine for patients with epilepsy. Neurology. 2008;70(22 Pt 2):2179–86. https://doi.org/10.1212/01.wnl.0000313154.55518.25.
Andermann F, Duh MS, Gosselin A, Paradis PE. Compulsory generic switching of antiepileptic drugs: high switchback rates to branded compounds compared with other drug classes. Epilepsia. 2007;48(3):464–9. https://doi.org/10.1111/j.1528-1167.2007.01007.x.
•• Ting TY, Jiang W, Lionberger R, Wong J, Jones JW, Kane MA, et al. Generic lamotrigine versus brand-name Lamictal bioequivalence in patients with epilepsy: a field test of the FDA bioequivalence standard. Epilepsia. 2015;56(9):1415–24. https://doi.org/10.1111/epi.13095. Bioequivalence testing of generic lamotrigine and Lamictal in patients who are potentially sensitive to problems with generic switching.
•• Privitera MD, Welty TE, Gidal BE, Diaz FJ, Krebill R, Szaflarski JP, et al. Generic-to-generic lamotrigine switches in people with epilepsy: the randomised controlled EQUIGEN trial. Lancet Neurol. 2016;15(4):365–72. https://doi.org/10.1016/S1474-4422(16)00014-4. Bioequivalence testing of two disparate generic lamotrigine products in patients with epilepsy.
Berg M, Privitera M, Diaz F, Dworetzky B, Elder E, Gidal B, et al. Equivalence among generic AEDs (EQUIGEN): single-dose study. Am Epilepsy Soc Ann Meet Philadelphia Abstract. 2015;2:267.
•• Vossler DG, Anderson GD, Bainbridge JAES. Position statement on generic substitution of antiepileptic drugs. Epilepsy Curr. 2016;16(3):209–11. https://doi.org/10.5698/1535-7511-16.3.209. AES acknowledges that drug formulation substitution with FDA-approved generic products reduces cost without compromising efficacy.
• Kesselheim AS, Bykov K, Gagne JJ, Wang SV, Choudhry NK. Switching generic antiepileptic drug manufacturer not linked to seizures: a case-crossover study. Neurology. 2016;87(17):1796–801. https://doi.org/10.1212/WNL.0000000000003259. Estimation the risk of seizure-related events associated with switching generic AED manufacturers.
• Johnson EL, Chang YT, Davit B, Gidal BE, Krauss GL. Assessing bioequivalence of generic modified-release antiepileptic drugs. Neurology. 2016;86(17):1597–604. https://doi.org/10.1212/WNL.0000000000002607. A review of bioequivalence studies of approved generic modified-release AEDs.
• Krauss GL. Potential influence of FDA-sponsored studies of antiepilepsy drugs on generic and brand-name formulation prescribing. JAMA Neurol. 2017; https://doi.org/10.1001/jamaneurol.2017.0492. A summary of clinical impact of FDA-sponsored lamotrigine bioequivalence studies and clinicians’ concerns remaining to be addressed.
Jiang W. Therapeutic equivalence of generic modified release AED products. American Epilepsy Society Annual Meeting; Houston; 2016.
Tothfalusi L, Endrenyi L. Approvable generic carbamazepine formulations may not be bioequivalent in target patient populations. Int J Clin Pharmacol Ther. 2013;51(6):525–8. https://doi.org/10.5414/CP201845.
Fang L. Bioequivalence study designs for anti-epileptic drugs (AED). American Epilepsy Society Annual Meeting; Houston; 2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Zhichuan Li, Lanyan Fang, Wenlei Jiang, Myong-Jin Kim, and Liang Zhao declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Epilepsy
This article reflects the views of the authors and should not be construed to represent the views or policies of the US Food and Drug Administration (FDA).
Rights and permissions
About this article
Cite this article
Li, Z., Fang, L., Jiang, W. et al. Risk-Based Bioequivalence Recommendations for Antiepileptic Drugs. Curr Neurol Neurosci Rep 17, 82 (2017). https://doi.org/10.1007/s11910-017-0795-1
Published:
DOI: https://doi.org/10.1007/s11910-017-0795-1