Abstract
A new appreciation of the microbiome is changing the way we perceive human health and disease. The holobiontic nature of humans is even etched into our DNA in the form of viral symbionts. Empirical evidence for the presence of endogenous retroviruses (ERVs) in the human genome and their activity in homeostatic and pathologic states has accumulated; however, no causal relationship with human disease has been established to date. In this review, we will focus on the role of endogenous retrovirus-K in neurologic disease. Specifically, we will attempt to reconcile the pathologic contribution of ERVK in disparate neurologic diseases by providing evidence as to inter-individual differences in ERVK genotypes, addressing the molecular regulation of ERVK, and provide detailed examples of ERVK-mediated processes in nervous system diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
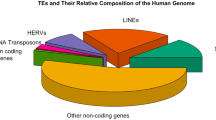
The DNA provirus hypothesis—where viral DNA integrates into a host genome—was proposed by Nobel laureate Howard M. Temin in the 1960s [1]. Indeed, over 8 % of human DNA is the result of retrovirus integrations scattered throughout the genome. Among the 31 lineages of endogenous retroviruses (ERVs) within the human genome, (which are spread among several Retroviridae subfamilies), the betaretrovirus ERVK (alias human endogenous retrovirus-K, HERV-K) is the most recently endogenated ERV. The ERVK (HML-2) clade is estimated to have been active as recently as 250,000 years ago [2••], and is considered the most transcriptionally active ERV. Several insertions in the human genome are relatively intact, permitting the expression of viral RNA and proteins. Full-length ERVK elements retain a classical retroviral genome structure, with core genes gag (group-specific antigen), pr (protease), pol (polymerase), and env (envelope) flanked by long terminal repeats (LTRs) [3]. Regulatory proteins within ERVK have also been described [4, 5]. There is even evidence of ERVK virion production in HIV infection [6] and lymphoma [7]. Unlike canonical retroviruses, Dube et al have recently proposed that ERVK virions can contain either infectious viral RNA or viral DNA genomes [8], thus changing how ERVK expression and replication should be viewed in the context of health and disease pathology.
Genotypic Interindividual Differences in ERVK
There are approximately 1000 ERVK (HML-2) integrations in humans, based on the human reference genome. Of these, all are considered replication-defective, with only 24 fixed loci retaining the capacity to encode viral proteins from at least 1 of their genes [3, 9]. However, evidence suggests that this is a fraction of the entire ERVK presence within individual human genomes [2••, 10, 11•].
Polymorphic ERVK insertions (unfixed proviruses) have been identified in several cohort studies [2••, 3, 9, 12, 13], with considerable variation between ethnic groups, as well as distinct inter-individual profiles. These studies indicate that people carry a distinctive ERVK signature based on individual genotypes. For a given locus, ERV polymorphism can occur as integration of a full-length ERV (with varying degrees of coding capacity), a solitary LTR, or an unoccupied pre-integration site [3, 9, 14]. Recently, Belshaw’s group has performed Next Generation Sequencing on individual human genomes revealing that several unfixed ERVK (HML-2) loci are absent from the human reference genome annotation [2••]. Moreover, the frequency of unfixed ERVK (HML-2) loci varied dramatically in the populations tested [2••], further supporting the idea that specific ERVK signatures may be associated with inter-individual differences in ERVK expression, pathology and disease states.
Sequence variation, resulting in ERV alleles, may also alter the function of viral proteins. For example, the ERVK-18 envelope protein is a superantigen that is encoded by 3 distinct alleles, which can alter the amino acid sequence of the protein [15], with predicted but uncharacterized biological effects. Among these 3 ERVK-18 env alleles, the K18.3 form is the minor allele with a frequency of 10.8 % within the Caucasian population [15]. The ERVK-18 env polymorphism has been shown to be a risk factor for Multiple Sclerosis (MS); homozygous carriers of the K18.3 allele had a significantly increased risk of this disease, suggesting that ERVK-18 may influence the genetic susceptibility to MS [16, 17]. ERVK-18 has also been associated with enhanced risk of Type 2 diabetes (T2D) in individuals with schizophrenia (SCZ) [18], with a risk haplotype comprised of 2 single nucleotide polymorphisms (SNPs) in the env region (rs558648 and rs1090799). These results remain controversial, as several cohort studies disagree over whether ERVK-18 polymorphisms are risk factors in T2D and SCZ [18, 19].
Phenotypic Variation in the Expression of ERVK
Current research indicates that not all ERVs remain silent passengers within our genomes; re-activation of ERVK is associated with many inflammatory diseases, such as cancers [7], HIV infection [4], rheumatoid arthritis [20], systemic lupus erythematosus [20] as well as neurologic conditions including multiple sclerosis (MS) [21], schizophrenia (SCZ) [22], bipolar disorder (BD) [22], amyotrophic lateral sclerosis (ALS) [23•], and Creutzfeldt-Jakob disease (CJD) [24]. While there is ubiquitous ERV expression in many tissues, regardless of health or disease, it has been shown that individuals largely exhibit distinct ERV expression signatures [22]. A difficulty in understanding these individual profiles and their association with disease states is a lack of appreciation for the biological control of ERVs.
At the molecular level, there is limited experimental evidence to indicate the cellular state or signals that are required to control the expression of ERVK. Accumulating evidence points to the importance of epigenetic mechanisms in the control of transposable elements including ERVs, and has been reviewed elsewhere [25]. The transcription of ERVK is under the control of viral promoters called long terminal repeats (LTRs), which flank either side of the provirus. To date, only transcription factors Sp1 [26], Sp3 [26], YY1 [27], MITF-M [28], and steroid hormone receptors [29, 30] have been experimentally shown to induce ERVK activity in human cells. Our group has recently focused on examining the role of proinflammatory transcription factors in the induction of ERVK expression. Using bioinformatics, we have revealed that the ERVK promoter contains multiple conserved putative binding sites for proinflammatory transcription factors, including nuclear factor kappa B (NF-κB) and interferon response factors (IRFs) [31••]. Specifically, the viral promoter harbors 2 conserved Interferon Stimulated Response Elements (ISREs) (Fig. 1); thus, inflammatory stimuli may modulate ERVK transcription. We have also generated substantial experimental evidence using human neuron and astrocyte in vitro models to support this claim (unpublished results). Thus, ERVK can exploit anti-viral immune responses and perhaps certain disease backgrounds, as select transcription factors can promote ERVK expression.
Proinflammatory signaling cascades and the associated transcription factors that may stimulate ERVK gene expression in multiple neurodegenerative diseases. TNFα, IFNγ and IFNα signaling leads to the phosphorylation (P) and activation of NF-κB (isoforms p50 and p65), IRF1, and IRF9, respectively. These proinflammatory transcription factors then translocate to the nucleus, where they bind their respective sites in the target promoters. The ERVK promoter (5′ LTR) contains multiple conserved putative NF-κB binding sites, as well as 2 interferon stimulated response elements (ISREs) that bind IRFs including IRF1 and IRF9 [31••]. Binding of nuclear NF-κB, IRF1, and/or IRF9 to the ERVK promoter may induce the expression of downstream proviral genes. Env envelope, Gag group specific antigen, Pol polymerase, Pr protease
Additional evidence supports the importance of innate immune signaling in ERVK re-activation, as select antiviral and proinflammatory cytokines can enhance ERVK expression. Cytokines, notably Tumor Necrosis Factor α (TNFα) and Interferon γ (IFNγ), play critical roles in the pathology of many neurodegenerative diseases including ALS [32, 33], SCZ [34], MS [35], and CJD [36]. TNFα and IFNγ are potent activators of NF-κB and IRF1, respectively, and may, thus, enhance ERVK transcription in these neuroinflammatory diseases (Fig. 1). We have recently generated evidence in human neuron and astrocyte in vitro models to support this claim (unpublished results). TNFα has previously been demonstrated to augment ERVK expression in rheumatoid arthritis—another inflammatory disease [37]. TNFα-mediated induction of ERVW env expression, following the binding of NF-κB with the ERVW promoter, has also been documented [35]. In addition, ERVK-18 expression can be enhanced upon IFNα treatment of peripheral blood lymphocytes [15]. Exogenous IFNα drives IRF9 activation and its translocation to the nucleus where it binds to ISREs in target promoters (Fig. 1). These results are consistent with our observation that ISREs in the ERVK LTR serve as key promoter elements. The ERVK env may also confer a self-regulating capacity, as an immunosuppressive domain in the transmembrane (TM) protein alters cytokine release through its immunomodulatory effects [38•]. Although recombinant ERVK transmembrane protein and ERVK virions induced substantial IL-10 secretion in peripheral blood mononuclear cells (PBMCs), reproducible inter-individual differences in the IL-10 response were observed [38•]. Moreover, notable enhancement of proinflammatory cytokine expression and impairment of genes involved in innate immunity [38•], further suggests that the ERVK TM protein will alter the regulation of ERVK, as well as host genes. Additionally, ERVK encoded dUTPase can activate NF-κB and promote proinflammatory cytokine secretion [39]. Additional ERV proteins are suspected to influence protein-protein interactions in humans [40]. Considering that signaling pathways are finely tuned based on the activity of interacting proteins, the genetic background of the host will play a significant role in ERVK expression and immunomodulation. These findings suggest that ongoing signaling cascades in neuroinflammatory disease may trigger ERVK re-activation, thus, promoting the expression of viral RNA and proteins, which may further modulate the pathologic status.
Putative Protective and Pathologic Roles of ERVK in Neurologic Disease
Amyotrophic Lateral Sclerosis (ALS)
Retroviruses, such as human immunodeficiency virus (HIV) and human T-cell leukemia virus (HTLV), have been associated with an increased incidence of ALS-like syndromes [41, 42]. Currently, a single study has demonstrated a direct association between ERVK and ALS [23•], despite evidence for retroviral pathology stemming from the repeated measurement of reverse transcriptase (RT: the retroviral enzyme that transcribes viral RNA into DNA) activity in this disease [43–45]. Elevated levels of ERVK pol transcripts (derived from select HML-2 and HML-3 loci) are detectable in postmortem brain tissues of patients with ALS, compared with tissues from Parkinson’s disease, systemic disease, and accidental death [23•]. Not only was ERVK RNA expressed in ALS, immunohistological analysis revealed the presence of RT protein in the cortical neurons of patients with ALS [23•]. Clusters of neurons in the prefrontal and motor cortex of patients with ALS exhibited the strongest RT expression, coinciding with the affected brain areas in this disease. An earlier report demonstrated that over half of ALS patients examined showed serum IgG reactivity against ERVK (HML-2) gag protein [46]. Patients with reactive anti-HML-2 gag antibodies exhibited a 10-fold reduction of viral RNA in PBMCs, suggesting an effective and ongoing immune response against ERVK in these patients with ALS [46]. As discussed by Alfahad and Nath [47], these studies open new avenues of investigation into the treatment of ALS.
Schizophrenia (SCZ) and Bipolar Disorder (BD)
Several studies have documented aberrant expression of ERVs in patients with schizophrenia [22, 48–53], and to a lesser extent, in patients with bipolar disorder [22, 48]. ERVW gene expression has been discovered in blood samples [49–51], in cerebrospinal fluid (CSF) [52], and in postmortem brain tissue [52, 53] of patients with SCZ, and has been reviewed extensively elsewhere [54]. Specifically, only ERVK10 (HML-2) RNA was significantly overexpressed in both SCZ and BD compared with healthy postmortem brain tissue [22]. The ERVK HML-7 clade is also significantly overrepresented in SCZ compared with BD samples (but not in SCZ compared with healthy controls), and under-represented in samples from patients with BD compared with healthy-brain samples [22]. A study by Diem et al further demonstrated that ERVK transcription was not affected by treatment with valproic acid (VPA; a medication used to treat SCZ) or any of the other medications tested, indicating that previous findings of an association between ERVK transcription and SCZ cannot be explained by patient treatment with any of the 4 medications analyzed in this study [55•]. To date, this represents limited and loci-specific alterations in ERVK expression in these neuropsychiatric diseases.
It has been postulated that it may not be mutations in genes associated with SCZ that result in a disease state, but rather mutations in the regulatory regions of these genes [56]. ERV LTRs are known to have promoter, enhancer, and regulatory functions [57]. Approximately 50 % of all human-specific ERVK (hsERVK–HML-2) elements show promoter activity in human tissues [58]. Epigenetic silencing of ERVs by DNA methylation is a known phenomenon and is thought to be a part of the antiretroviral defense system [25]. Therefore, the silencing or downregulation of genes with ERV sequences in their regulatory regions may be the consequence of the host’s attempts to stop the expression of these endogenous viruses.
Recently, a full-length almost intact ERVK (HML-2) sequence that displays strong enhancer activity, was identified near the PRODH gene [59•]. Mutations in PRODH, which encodes a mitochondrial enzyme, have been found to be associated with neuropsychiatric disorders, including SCZ [60]. Given this link between PRODH and schizophrenia, Suntsova et al attempted to characterize this ERVK locus (referred to as hsERV PRODH ) and its potential enhancer activity for PRODH [59•]. They showed that the enhancer activity of hsERV PRODH is regulated by methylation, and it acts synergistically with the PRODH internal CpG island to activate the PRODH promoter. Transcriptional analysis showed that PRODH displays the highest expression level in the hippocampus, where hsERV PRODH is hypo-methylated [59•]. The hippocampus is known to be one of the structures of the brain that is most affected in SCZ [61]; if hyper-methylation of hsERV PRODH occurred, aberrant expression of PRODH in the hippocampus would likely result.
Similarly, an ERVW LTR is located in the regulatory region of the GABA receptor B1 gene (GABBR1) [56], a gene located in region associated with risk for SCZ [62]. It is speculated that hyper-methylation of this ERVW LTR may downregulate GABBR1 in brains of patients with SCZ [56], thus, accounting for its altered expression pattern [63, 64]. As a result, Hegyi et al propose that the overexpression of ERVs at the onset of disease leads to their subsequent silencing by hypermethylation, which may pathologically contribute to diseases such as SCZ [56]. This hypothesis also offers an explanation as to why ERVW transcripts are readily found in the CSF of patients with recent-onset SCZ, but rarely in chronic patients [49, 52, 65]. It could be that the activation of ERVs occurs early in the etiopathology of schizophrenia or during highly symptomatic periods of disease, resulting in the upregulation of some genes for which ERV elements act as promoters or enhancers. This may be followed by hypermethylation of ERV sequences as a defense mechanism, leading to downregulation of ERV-regulated genes.
Multiple Sclerosis (MS)
Among ERVs associated with MS, ERVW has been the most extensively studied. Many studies have reported significant upregulation of ERVW RNA in brain samples from MS patients [35, 66]. ERVW env protein is highly expressed within astrocytes and microglia in MS plaques, and correlates with the extent of inflammation and active demyelination [35, 66]. Augmented ERVW expression has also been observed in the CSF and blood of MS patients [67, 68]. A recent study has also shown enhanced ERVW DNA copy number in the PBMCs of women with MS; this phenomenon correlated with disease severity scores [68]. In contrast, other studies depict a lack of association between enhanced ERVW expression and MS. Using high-throughput amplicon sequencing, Schmitt et al reported a lack of significant difference in ERVW transcripts between MS and control brain tissue samples, despite clear evidence of inter-individual variability [69]. Similarly, enhanced ERVW expression in the CSF and blood of MS patients could not be detected in several studies [70, 71]. Thus, a definitive association between ERVW activation and MS neuropathology remains to be established.
Nonetheless, other human endogenous retroviruses, including ERVK, have been reported to be upregulated in MS. Elevated levels of ERVK RNA have been found in the brain tissue from MS patients [72]. As mentioned above, the ERVK-18.3 env allele has been determined to be a risk factor for MS. Interestingly, ERVK-18 env superantigen can be transactivated by Epstein Barr Virus (EBV) latent membrane protein LMP-2A [73, 74], and EBV infection is considered to be one of the major risk factors for MS [75]. Similarly, ERVW env protein also displays superantigenic properties, and can be transactivated by EBV infection of astrocytes in vitro [76]. Together, these superantigens may promote the nonspecific activation of T lymphocytes in the CNS, leading to extensive demyelination and neuronal injury [77]. Thus, ERV-derived superantigens may contribute to MS immunopathogenesis, particularly in the context of EBV infection.
Activation of the host immune system has been implicated as the ultimate effector in MS pathogenesis. Re-activation of human endogenous retroviruses in the CNS may play an important role in this process, as the immune system may mount an antiviral response against ERV elements in order to eliminate ERV-expressing cells. Antiretroviral defense mechanisms can be mediated by a variety of innate immune sensors including Pattern Recognition Receptors (PRRs) that detect retroviral RNA and proteins. PRRs, including Tripartite motif containing 5 (TRIM5) and Toll like receptor 4 (TLR4), are known to recognize retroviral capsid and envelope proteins, respectively; engagement of these sensors with their viral ligands activates signaling cascades that stimulate innate immunity [78•, 79]. The role of TRIM5 in detection of gag proteins encoded by MS-associated ERVs has not yet been studied. Nonetheless, single nucleotide polymorphisms (SNPs) in TRIM5 gene (as well as SNPs in other viral restriction factors) have been associated with the risk of MS [80]. However, the functional outcomes of these SNPs remain unclear.
Another mechanism by which ERV proteins may trigger MS immunopathology is through molecular mimicry. Recently, ERVW env proteins were predicted to share several T and B cell epitope regions with myelin oligodendrocyte glycoprotein (MOG) and myelin basic protein (MBP) [81]. This suggests that ERVW env overexpression in the CNS may break tolerance toward host MOG and MBP, generating an autoimmune response against these myelin proteins, which can explain extensive demyelination typically observed in MS. However, the cross-reactivity between ERVW env and myelin protein epitopes, and the resulting autoimmune reaction, needs to be validated experimentally. In addition, whether antigen mimicry is also employed by other MS-associated ERVs, such as ERVK, remains to be explored.
HIV Infection
ERVK activity is well-documented in HIV infection [6, 82] (reviewed in [4]), including the nervous system (Douville and Nath, unpublished) [83••]. Recently, Bhat et al have provided evidence that enhanced ERVK (HML-2) env protein expression in the brains of HIV infected individuals may confer neuroprotective effects [83••]. This is based on the observation that neuroblastoma cells transfected with an ERVK env expressing construct were protected from injury by staurosporine and the HIV-1 Vpr protein, compared with the control vector alone. Moreover, the protection from HIV-1 Vpr toxicity was recapitulated in vpr/RAG1−/− mice which were adoptively transferred with neural stem cells expressing ERV-K env into the striatum; these animals exhibited a significant reduction in TNFα expression compared with controls. Exaptation of ERVK env may provide neurons a degree of protection in the context of chronic neurodegenerative diseases.
As well, cellular cytotoxic responses and antibodies produced against ERVK can prove to be detrimental to HIV-infected cells [84, 85•]. During HIV infection, ERVK env peptides can be a target for cytotoxic T cells [84]. NK cells may also destroy HIV-infected cells via an antibody-dependent cytotoxic mechanism, based on in vitro assays [85•]. Additionally, it was observed that either the HIV strain or the host were important factors in determining the extent of ERVK env induction in HIV-infected cells [85•, 86], and thus, may alter the degree of CNS tissue injury in HIV-associated neurocognitive disorder (HAND).
In addition, other ERVK proteins may promote changes in dendritic spine morphology in pyramidal neurons. The ERVK regulatory protein Rec has been shown to interact with the mRNA binding protein Staufen-1, causing its accumulation in the nucleus [5]. This interaction may alter Staufen-1-mediated mRNA trafficking and turnover, functions that are essential for regulation of neuronal synapses during long-term plasticity in learning and memory [87]. The interaction with Staufen-1 also favored Rec-dependent viral RNA transport [5], and thus may enhance ERVK protein expression. Moreover, ERVK and HIV gag proteins can both independently interact with Staufen-1 to enhance their respective production of virions [5, 88], as well as ERVK env expression within HIV-1 virions [89]. Together, these studies suggest that ERVK expression in the CNS may have both protective and pathologic consequences.
Prion Disease
Prion diseases, such as Creutzfeldt-Jakob disease (CJD) in humans, are a group of rare but fatal neurodegenerative disorders. The causative agent of these diseases is believed to be an infectious misfolded cellular protein called a prion protein (PrPSC), which is resistant to proteinase degradation and accumulates inside neurons, leading to neuronal toxicity and death [24, 90]. The disease propagates upon transmission of PrPSC to new cells, which further catalyzes the conversion of the normal cellular prion protein (PrpC) into its abnormal form; however, the mechanisms behind this conversion have not been clearly elucidated.
Recently, augmented expression of several ERVs has been observed in the CSF of CJD patients [24]. Although the frequency of ERVK transcripts was higher in CJD CSF samples compared with the controls, this result did not reach statistical significance. Nonetheless, the increased expression of ERVs in CJD suggests that endogenous retroviruses may contribute to the pathogenesis of this prion disease. For instance, ERV viral RNA molecules may elicit the transformation of PrPC to PrPSC [90]. In support of this hypothesis, small highly structured RNAs have been shown to interact with human recombinant PrPC and stimulate its conversion to a proteinase resistant isoform [91]. Interestingly, RNA molecules derived from ERVK elements have extremely conserved complex secondary structures resembling that of the small highly structured RNAs used in these studies [91] (Carr and Douville, unpublished). Highly structured RNAs derived from HIV-1 have also been shown to interact with the human recombinant PrPC and impart proteinase resistance to it in vitro [92]. Thus, increased levels of ERVK RNA in the CSF of CJD patients have the potential to drive the transformation of the normal human prion protein to its infectious misfolded isoform.
In addition, ERVs may facilitate the spread of pathologic prion agents intercellularly by recruiting prion proteins to virions as ERVs replicate. In fact, it was recently demonstrated that murine PrPSC associates with gag and env proteins on Moloney Murine Leukemia Virus (MMLV) particles, and infection with MMLV strongly enhances the extracellular release of murine PrPSC, thus, augmenting the infectivity of this prion protein [90, 93]. Similarly, human PrPSC has also been shown to be recruited by HIV-1 virions [93]. Human endogenous retroviruses, ERVW and ERVK, which are capable of producing virions [7, 21], may also be able to recruit PrPSC either through interactions with surface gag and env proteins or with viral RNA, thereby transmitting prion proteins to new cells and facilitating the progression of human prion diseases.
Moreover, CJD is neuroinflammatory and marked by augmented levels of proinflammatory cytokines, including TNFα [36, 94]. Mice models of CJD also exhibit increased TNFα, as well as NF-κB activity [95]. Recently, the toxic domain of human prion protein has been shown to activate NF-κB and lead to TNFα production in a macrophage cell line [96]. Based on our prediction of NF-κB responsive elements in the ERVK promoter [31••] (Fig. 1), it is possible that PrPSC-induced TNFα production and NF-κB activation may enhance ERVK transcription in CJD brains. This may culminate in a positive feedback loop favoring further neuroinflammation, ERVK re-activation, and prion infection.
Conclusions
Although ERVK has not been shown to be a causative agent of nervous system disease, its expression can clearly influence both protective and pathologic aspects of motor neuron, neuropsychiatric, and neurodegenerative diseases (Table 1). A common thread among ERVK-associated disease appears to be the presence of inflammatory signals; but how this retrovirus fits into the complex interplay between infection, immunity, autoimmunity, and environmental exposures is yet to be fully elucidated. Activation of multiple ERVs may cooperatively stimulate a multitude of host antiretroviral immune responses against ERV-expressing cells; and, ERVs may exploit this response, culminating in a positive feedback loop favoring further viral gene expression, excessive neuroinflammation, and subsequent neuronal injury and loss. Moreover, it is important to consider that specific ERVK loci can confer select pathologic contributions. Bulk measurement of ERVs (without consideration of the individual integrations and their genomic context) may be an insufficient methodology to address their role in distinct neurologic diseases. Examining an individual’s unique complement of ERVs may prove to be a better predictor of disease risk, once further inroads are made in understanding the protective and pathologic roles of each integrated provirus. It will be important for future studies to expand how we measure ERVK activity in the CNS; improved screening for ERVK expression in specific cell types, CNS regions and disease stages, as well as an expansion toward single-loci ERVK measurements will broaden our current knowledge in this area. Current studies are limited by the availability of commercial ERV-specific reagents for molecular biology and the expense of high-throughput screening techniques – a possible solution for our field would be the development of an ERV resource bank, as has been accomplished with the NIH AIDS Reagent Program.
Another benefit of ERV research in the context of nervous system disease is the possibility of improved therapeutics. For example, patients with schizophrenia and bipolar disorder are treated with a range of chemotherapeutics including antipsychotics and lithium. Lithium is protective against HIV neurotoxicity, and HIV patients treated with this medication show cognitive improvements [97]. Clozapine is an antipsychotic drug, which actually inhibits HIV replication in vitro [98]. Since both of these drugs interact with exogenous retroviruses, it is possible that they may have some effect on ERVs as well. In support of this notion, there is epidemiologic evidence that incidence of ALS is extremely rare among individuals with SCZ (much lower than predicted for the general population) [99]. Common medications for SCZ may convey prophylactic neuroprotection, inhibiting the development of ALS [99]. There is some evidence that medications routinely prescribed to schizophrenics may stop inflammation and support neuronal survival [100]. Abating inflammation may also decrease the expression of ERVK, which is upregulated by inflammatory transcription factors [31••]. With improved biomarkers for neurologic disease risk, the use of currently vetted SCZ medications may be repurposed for the prevention or delay of ERVK-associated nervous system diseases.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Weiss RA. The discovery of endogenous retroviruses. Retrovirology. 2006;3:67.
Marchi E, Kanapin A, Magiorkinis G, Belshaw R. Unfixed endogenous retroviral insertions in the human population. J Virol. 2014;88(17):9529–37. This study highlights the inter-individual variability of ERVK polymorphisms, and reveals novel ERVK insertions, which are not annotated in the human reference genome. Marchi et al also predict that ERVK has been active in the human germline as recently as 250,000 years ago.
Shin W, Lee J, Son SY, et al. Human-specific HERV-K insertion causes genomic variations in the human genome. PLoS One. 2013;8:e60605.
van der Kuyl AC. HIV infection and HERV expression: a review. Retrovirology. 2012;9:6.
Hanke K, Hohn O, Liedgens L, et al. Staufen-1 interacts with the human endogenous retrovirus family HERV-K(HML-2) rec and gag proteins and increases virion production. J Virol. 2013;87:11019–30.
Contreras-Galindo R, Kaplan MH, Contreras-Galindo AC, et al. Characterization of human endogenous retroviral elements in the blood of HIV-1-infected individuals. J Virol. 2012;86:262–76.
Contreras-Galindo R, Kaplan MH, Leissner P, et al. Human endogenous retrovirus K (HML-2) elements in the plasma of people with lymphoma and breast cancer. J Virol. 2008;82:9329–36.
Dube D, Contreras-Galindo R, He S, et al. Genomic flexibility of human endogenous retrovirus type K. J Virol. 2014;88(17):9673–82.
Subramanian RP, Wildschutte JH, Russo C, Coffin JM. Identification, characterization, and comparative genomic distribution of the HERV-K (HML-2) group of human endogenous retroviruses. Retrovirology. 2011;8:90.
Belshaw R, Dawson AL, Woolven-Allen J, et al. Genomewide screening reveals high levels of insertional polymorphism in the human endogenous retrovirus family HERV-K(HML2): implications for present-day activity. J Virol. 2005;79:12507–14.
Contreras-Galindo R, Kaplan MH, He S, et al. HIV infection reveals widespread expansion of novel centromeric human endogenous retroviruses. Genome Res. 2013;23:1505–13. Here, expression of a novel ERVK (HML-2) provirus termed K11 is identified in HIV-1 infection. Multiple K11 copies are found in centromeric regions of human chromosomes and not yet annotated in the human genome assembly.
Moyes DL, Martin A, Sawcer S, et al. The distribution of the endogenous retroviruses HERV-K113 and HERV-K115 in health and disease. Genomics. 2005;86:337–41.
Turner G, Barbulescu M, Su M, et al. Insertional polymorphisms of full-length endogenous retroviruses in humans. Curr Biol. 2001;11:1531–5.
Hughes JF, Coffin JM. Human endogenous retrovirus K solo-LTR formation and insertional polymorphisms: implications for human and viral evolution. Proc Natl Acad Sci U S A. 2004;101:1668–72.
Stauffer Y, Marguerat S, Meylan F, et al. Interferon-alpha-induced endogenous superantigen. a model linking environment and autoimmunity. Immunity. 2001;15:591–601.
Tai AK, O’Reilly EJ, Alroy KA, et al. Human endogenous retrovirus-K18 Env as a risk factor in multiple sclerosis. Mult Scler. 2008;14:1175–80.
de la Hera B, Varade J, Garcia-Montojo M, et al. Role of the human endogenous retrovirus HERV-K18 in autoimmune disease susceptibility: study in the Spanish population and meta-analysis. PLoS One. 2013;8:e62090.
Dickerson F, Rubalcaba E, Viscidi R, et al. Polymorphisms in human endogenous retrovirus K-18 and risk of type 2 diabetes in individuals with schizophrenia. Schizophr Res. 2008;104:121–6.
Nyegaard M, Demontis D, Thestrup BB, et al. No association of polymorphisms in human endogenous retrovirus K18 and CD48 with schizophrenia. Psychiatr Genet. 2012;22:146–8.
Balada E, Ordi-Ros J, Vilardell-Tarres M. Molecular mechanisms mediated by human endogenous retroviruses (HERVs) in autoimmunity. Rev Med Virol. 2009;19:273–86.
Perron H, Lang A. The human endogenous retrovirus link between genes and environment in multiple sclerosis and in multifactorial diseases associating neuroinflammation. Clin Rev Allergy Immunol. 2010;39:51–61.
Frank O, Giehl M, Zheng C, et al. Human endogenous retrovirus expression profiles in samples from brains of patients with schizophrenia and bipolar disorders. J Virol. 2005;79:10890–901.
Douville R, Liu J, Rothstein J, Nath A. Identification of active loci of a human endogenous retrovirus in neurons of patients with amyotrophic lateral sclerosis. Ann Neurol. 2011;69:141–51. This article describes the expression of ERVK RNA from specific loci in the cortical brain tissue of patients with ALS. Immunohistologic staining revealed that ERVK reverse transcriptase protein expression was localized in prefrontal and motor cortical neurons in ALS-affected individuals.
Jeong BH, Lee YJ, Carp RI, Kim YS. The prevalence of human endogenous retroviruses in cerebrospinal fluids from patients with sporadic Creutzfeldt-Jakob disease. J Clin Virol. 2010;47:136–42.
Maksakova IA, Mager DL, Reiss D. Keeping active endogenous retroviral-like elements in check: the epigenetic perspective. Cell Mol Life Sci. 2008;65:3329–47.
Fuchs NV, Kraft M, Tondera C, et al. Expression of the human endogenous retrovirus (HERV) group HML-2/HERV-K does not depend on canonical promoter elements but is regulated by transcription factors Sp1 and Sp3. J Virol. 2011;85:3436–8.
Knossl M, Lower R, Lower J. Expression of the human endogenous retrovirus HTDV/HERV-K is enhanced by cellular transcription factor YY1. J Virol. 1999;73:1254–61.
Katoh I, Mirova A, Kurata S, et al. Activation of the long terminal repeat of human endogenous retrovirus K by melanoma-specific transcription factor MITF-M. Neoplasia. 2011;13:1081–92.
Ono M, Kawakami M, Ushikubo H. Stimulation of expression of the human endogenous retrovirus genome by female steroid hormones in human breast cancer cell line T47D. J Virol. 1987;61:2059–62.
Goering W, Ribarska T, Schulz WA. Selective changes of retro element expression in human prostate cancer. Carcinogenesis. 2011;32:1484–92.
Manghera M, Douville RN. Endogenous retrovirus-K promoter: a landing strip for inflammatory transcription factors? Retrovirology. 2013;10:16. Using a bioinformatics approach, this paper predicts that prototypical ERVK promoters contain multiple conserved binding sites for proinflammatory transcription factors, particularly Nuclear Factor-kappa B (NF-κB) and Interferon Response Factors (IRFs). An interesting feature of the ERVK promoter is the presence of 2 conserved Interferon Stimulated Response Elements (ISREs), which are known to bind IRFs. These findings suggest that augmented levels of proinflammatory transcription factors, such as NF-κB and IRF1, during neuroinflammation may be responsible for enhanced ERVK transcription in a variety of neurodegenerative conditions.
Tateishi T, Yamasaki R, Tanaka M, et al. CSF chemokine alterations related to the clinical course of amyotrophic lateral sclerosis. J Neuroimmunol. 2010;222:76–81.
Aebischer J, Moumen A, Sazdovitch V, et al. Elevated levels of IFNgamma and LIGHT in the spinal cord of patients with sporadic amyotrophic lateral sclerosis. Eur J Neurol. 2012;19(752–9):e745–56.
Monji A, Kato T, Kanba S. Cytokines and schizophrenia: microglia hypothesis of schizophrenia. Psychiatry Clin Neurosci. 2009;63:257–65.
Mameli G, Astone V, Arru G, et al. Brains and peripheral blood mononuclear cells of multiple sclerosis (MS) patients hyperexpress MS-associated retrovirus/HERV-W endogenous retrovirus, but not Human herpes virus 6. J Gen Virol. 2007;88:264–74.
Shi Q, Xie WL, Zhang B, et al. Brain microglia were activated in sporadic CJD but almost unchanged in fatal familial insomnia and G114V genetic CJD. Virol J. 2013;10:216.
Freimanis G, Hooley P, Ejtehadi HD, et al. A role for human endogenous retrovirus-K (HML-2) in rheumatoid arthritis: investigating mechanisms of pathogenesis. Clin Exp Immunol. 2010;160:340–7.
Morozov VA, Dao Thi VL, Denner J. The transmembrane protein of the human endogenous retrovirus—K (HERV-K) modulates cytokine release and gene expression. PLoS One. 2013;8:e70399. This paper demonstrates that ERVK virions and recombinant ERVK TM protein can inhibit the proliferation of human immune cells. The recombinant TM protein as well as ERVK virions also stimulated the expression and secretion of several cytokines, including the soluble TNF receptor II (sTNFRII) and Interleukin 10 (IL-10). An immunosuppressive state induced by the antiproliferative and anti-inflammatory effects of ERVK TM protein may allow tumor cells to escape immune detection. Thus, enhanced expression of ERVK env in multiple cancers may be responsible for promoting tumor proliferation.
Ariza ME, Williams MV. A human endogenous retrovirus K dUTPase triggers a TH1, TH17 cytokine response: does it have a role in psoriasis? J Invest Dermatol. 2011;131:2419–27.
Rachita HR, Nagarajaram HA. Viral proteins that bridge unconnected proteins and components in the human PPI network. Mol Biosyst. 2014;10(9):2448–58.
Matsuzaki T, Nakagawa M, Nagai M, et al. HTLV-I-associated myelopathy (HAM)/tropical spastic paraparesis (TSP) with amyotrophic lateral sclerosis-like manifestations. J Neurovirol. 2000;6:544–8.
Verma A, Berger JR. ALS syndrome in patients with HIV-1 infection. J Neurol Sci. 2006;240:59–64.
MacGowan DJ, Scelsa SN, Imperato TE, et al. A controlled study of reverse transcriptase in serum and CSF of HIV-negative patients with ALS. Neurology. 2007;68:1944–6.
McCormick AL, Brown Jr RH, Cudkowicz ME, Al-Chalabi A, Garson JA. Quantification of reverse transcriptase in ALS and elimination of a novel retroviral candidate. Neurology. 2008;70:278–83.
Steele AJ, Al-Chalabi A, Ferrante K, et al. Detection of serum reverse transcriptase activity in patients with ALS and unaffected blood relatives. Neurology. 2005;64:454–8.
Hadlock KG, Miller RG, Jin X, et al. Elevated rates of antibody reactivity to HML-2/HERV-K but not other endogenous retroviruses in ALS. Amyotroph Lateral Scler Motor Neuron Disord. 2004;5:63.
Alfahad T, Nath A. Retroviruses and amyotrophic lateral sclerosis. Antivir Res. 2013;99:180–7.
Weis S, Llenos IC, Sabunciyan S, et al. Reduced expression of human endogenous retrovirus (HERV)-W GAG protein in the cingulate gyrus and hippocampus in schizophrenia, bipolar disorder, and depression. J Neural Transm. 2007;114:645–55.
Huang W, Li S, Hu Y, et al. Implication of the env gene of the human endogenous retrovirus W family in the expression of BDNF and DRD3 and development of recent-onset schizophrenia. Schizophr Bull. 2011;37:988–1000.
Yao Y, Schroder J, Nellaker C, et al. Elevated levels of human endogenous retrovirus-W transcripts in blood cells from patients with first episode schizophrenia. Genes Brain Behav. 2008;7:103–12.
Perron H, Mekaoui L, Bernard C, et al. Endogenous retrovirus type W GAG and envelope protein antigenemia in serum of schizophrenic patients. Biol Psychiatry. 2008;64:1019–23.
Karlsson H, Bachmann S, Schroder J, et al. Retroviral RNA identified in the cerebrospinal fluids and brains of individuals with schizophrenia. Proc Natl Acad Sci U S A. 2001;98:4634–9.
Yolken RH, Karlsson H, Yee F, Johnston-Wilson NL, Torrey EF. Endogenous retroviruses and schizophrenia. Brain Res Rev. 2000;31:193–9.
Leboyer M, Tamouza R, Charron D, Faucard R, Perron H. Human endogenous retrovirus type W (HERV-W) in schizophrenia: a new avenue of research at the gene-environment interface. World J Biol Psychiatry. 2013;14:80–90.
Diem O, Schaffner M, Seifarth W, Leib-Mosch C. Influence of antipsychotic drugs on human endogenous retrovirus (HERV) transcription in brain cells. PLoS One. 2012;7:e30054. Schizophrenia patients analyzed in previous studies (which often showed elevated levels of ERVs), were almost all taking medications such as antipsychotics. Since some neuroleptics and antidepressants are known to influence gene expression, in this study they attempted to determine if medications commonly prescribed to schizophrenics influence the expression of ERVs. Overall, they found that some cell types and postmortem brain tissue show upregulation of several types of HERVs with valproic acid treatment, but these did not include ERVK (HML2). Their results suggest that antipsychotic medication may contribute to increased expression of select ERV groups in patients with neuropsychiatric diseases.
Hegyi H. GABBR1 has a HERV-W LTR in its regulatory region—a possible implication for schizophrenia. Biol Direct. 2013;8:5.
Cohen CJ, Lock WM, Mager DL. Endogenous retroviral LTRs as promoters for human genes: a critical assessment. Gene. 2009;448:105–14.
Buzdin A, Kovalskaya-Alexandrova E, Gogvadze E, Sverdlov E. At least 50 % of human-specific HERV-K (HML-2) long terminal repeats serve in vivo as active promoters for host nonrepetitive DNA transcription. J Virol. 2006;80:10752–62.
Suntsova M, Gogvadze EV, Salozhin S, et al. Human-specific endogenous retroviral insert serves as an enhancer for the schizophrenia-linked gene PRODH. Proc Natl Acad Sci U S A. 2013;110:19472–7. A human specific (hs) ERV belonging to the ERVK (HML-2) group is involved in the transcriptional regulation of a schizophrenia-related gene, PRODH. PRODH regulates proline catabolism, and is integral in normal functioning of the CNS; several mutations in this gene are associated with neuropsychiatric disorders, including schizophrenia. In cells expressing PRODH, hsERV PRODH is hypomethylated. Using bioinformatics they predicted that the hsERV PRODH LTR contains transcription factor binding sites for SOX2 and NF-κB1, when these genes were overexpressed in vitro, only over-expression of SOX2 resulted in a strong enhancer effect of hsERV PRODH .
Kempf L, Nicodemus KK, Kolachana B, et al. Functional polymorphisms in PRODH are associated with risk and protection for schizophrenia and fronto-striatal structure and function. PLoS Genet. 2008;4:e1000252.
Grace AA. Dopamine system dysregulation by the hippocampus: implications for the pathophysiology and treatment of schizophrenia. Neuropharmacology. 2012;62:1342–8.
Shi J, Levinson DF, Duan J, et al. Common variants on chromosome 6p22.1 are associated with schizophrenia. Nature. 2009;460:753–7.
Fatemi SH, Folsom TD, Rooney J, Thuras PD. Expression of GABAA alpha2-, beta1- and epsilon-receptors are altered significantly in the lateral cerebellum of subjects with schizophrenia, major depression and bipolar disorder. Translation. Psychiatry. 2013;3:e303.
Fatemi SH, Folsom TD, Thuras PD. Deficits in GABA(B) receptor system in schizophrenia and mood disorders: a postmortem study. Schizophr Res. 2011;128:37–43.
Karlsson H, Schroder J, Bachmann S, Bottmer C, Yolken RH. HERV-W-related RNA detected in plasma from individuals with recent-onset schizophrenia or schizoaffective disorder. Mol Psychiatry. 2004;9:12–3.
Perron H, Germi R, Bernard C, et al. Human endogenous retrovirus type W envelope expression in blood and brain cells provides new insights into multiple sclerosis disease. Mult Scler. 2012;18:1721–36.
Brudek T, Christensen T, Aagaard L, et al. B cells and monocytes from patients with active multiple sclerosis exhibit increased surface expression of both HERV-H Env and HERV-W Env, accompanied by increased seroreactivity. Retrovirology. 2009;6:104.
Garcia-Montojo M, Dominguez-Mozo M, Arias-Leal A, et al. The DNA copy number of human endogenous retrovirus-W (MSRV-type) is increased in multiple sclerosis patients and is influenced by gender and disease severity. PLoS One. 2013;8:e53623.
Schmitt K, Richter C, Backes C, et al. Comprehensive analysis of human endogenous retrovirus group HERV-W locus transcription in multiple sclerosis brain lesions by high-throughput amplicon sequencing. J Virol. 2013;87:13837–52.
Alvarez-Lafuente R, Garcia-Montojo M, De Las Heras V, et al. Herpes viruses and human endogenous retroviral sequences in the cerebrospinal fluid of multiple sclerosis patients. Mult Scler. 2008;14:595–601.
Laufer G, Mayer J, Mueller BF, Mueller-Lantzsch N, Ruprecht K. Analysis of transcribed human endogenous retrovirus W env loci clarifies the origin of multiple sclerosis-associated retrovirus env sequences. Retrovirology. 2009;6:37.
Johnston JB, Silva C, Holden J, et al. Monocyte activation and differentiation augment human endogenous retrovirus expression: implications for inflammatory brain diseases. Ann Neurol. 2001;50:434–42.
Hsiao FC, Tai AK, Deglon A, et al. EBV LMP-2A employs a novel mechanism to transactivate the HERV-K18 superantigen through its ITAM. Virology. 2009;385:261–6.
Sutkowski N, Chen G, Calderon G, Huber BT. Epstein-Barr virus latent membrane protein LMP-2A is sufficient for transactivation of the human endogenous retrovirus HERV-K18 superantigen. J Virol. 2004;78:7852–60.
Serafini B, Rosicarelli B, Franciotta D, et al. Dysregulated Epstein-Barr virus infection in the multiple sclerosis brain. J Exp Med. 2007;204:2899–912.
Mameli G, Poddighe L, Mei A, et al. Expression and activation by Epstein Barr virus of human endogenous retroviruses-W in blood cells and astrocytes: inference for multiple sclerosis. PLoS One. 2012;7:e44991.
Mameli G, Madeddu G, Mei A, et al. Activation of MSRV-type endogenous retroviruses during infectious mononucleosis and Epstein-Barr virus latency: the missing link with multiple sclerosis? PLoS One. 2013;8:e78474.
Pertel T, Hausmann S, Morger D, et al. TRIM5 is an innate immune sensor for the retrovirus capsid lattice. Nature. 2011;472:361–5. This paper demonstrates that TRIM5 acts as a typical pattern recognition receptor, capable of detecting the retroviral capsid lattice. The engagement of TRIM5 with the retroviral capsid proteins stimulates inflammatory innate immune signaling mediated by AP-1 and NF-κB transcription factors, which is crucial for restricting retroviral replication.
Rolland A, Jouvin-Marche E, Viret C, et al. The envelope protein of a human endogenous retrovirus-W family activates innate Immunity. through CD14/TLR4 and promotes Th1-like responses. J Immunol. 2006;176:7636–44.
Nexo BA, Hansen B, Nissen KK, et al. Restriction genes for retroviruses influence the risk of multiple sclerosis. PLoS One. 2013;8:e74063.
do Olival GS, Faria TS, Nali LH, et al. Genomic analysis of ERVWE2 locus in patients with multiple sclerosis: absence of genetic association but potential role of human endogenous retrovirus type W elements in molecular mimicry with myelin antigen. Front Microbiol. 2013;4:172.
Gonzalez-Hernandez MJ, Cavalcoli JD, Sartor MA, et al. Regulation of the HERV-K (HML-2) transcriptome by the HIV-1 Tat protein. J Virol. 2014;88(16):8924–35.
Bhat RK, Rudnick W, Antony JM, et al. Human endogenous retrovirus-K(II) envelope induction protects neurons during HIV/AIDS. PLoS One. 2014;9:e97984. Bhat et al describe the neuronal expression of ERVK (HML-2) envelope protein in brain tissue from HIV-infected and uninfected individuals. In vitro and murine models suggest that the ERVK (HML-2) transmembrane protein is protective against HIV-1 Vpr-mediated toxicity. Thus, exaptation of ERVK env may be a neuroprotective mechanism under pathologic conditions.
Garrison KE, Jones RB, Meiklejohn DA, et al. T cell responses to human endogenous retroviruses in HIV-1 infection. PLoS Pathog. 2007;3:e165.
Michaud HA, SenGupta D, de Mulder M, et al. Cutting edge: an antibody recognizing ancestral endogenous virus glycoproteins mediates antibody-dependent cellular cytotoxicity on HIV-1-infected cells. J Immunol. 2014;193(4):1544–8. This study examines how an antibody targeting the ERVK transmembrane protein facilitates NK killing of HIV-1 infected cells. The humoral response against ERVK in HIV-infected individuals may play a role in antibody-dependent cellular cytotoxicity, and could be used in novel immunomodulatory or neuroprotective strategies.
Michaud HA, de Mulder M, SenGupta D, et al. Trans-activation, post-transcriptional maturation, and induction of antibodies to HERV-K (HML-2) envelope transmembrane protein in HIV-1 infection. Retrovirology. 2014;11:10.
Lebeau G, DesGroseillers L, Sossin W, Lacaille JC. mRNA binding protein staufen 1-dependent regulation of pyramidal cell spine morphology via NMDA receptor-mediated synaptic plasticity. Mol Brain. 2011;4:22.
Chatel-Chaix L, Boulay K, Mouland AJ, Desgroseillers L. The host protein Staufen1 interacts with the Pr55Gag zinc fingers and regulates HIV-1 assembly via its N-terminus. Retrovirology. 2008;5:41.
Brinzevich D, Young GR, Sebra R, et al. HIV-1 interacts with human endogenous retrovirus K (HML-2) envelopes derived from human primary lymphocytes. J Virol. 2014;88:6213–23.
Lee Y-J, Jeong B-H, Choi E-K, Kim Y-S. Involvement of endogenous retroviruses in prion diseases. Pathogens. 2013;2:533–43.
Adler V, Zeiler B, Kryukov V, et al. Small, highly structured RNAs participate in the conversion of human recombinant PrP(Sen) to PrP(Res) in vitro. J Mol Biol. 2003;332:47–57.
Leblanc P, Baas D, Darlix JL. Analysis of the interactions between HIV-1 and the cellular prion protein in a human cell line. J Mol Biol. 2004;337:1035–51.
Leblanc P, Alais S, Porto-Carreiro I, et al. Retrovirus infection strongly enhances scrapie infectivity release in cell culture. EMBO J. 2006;25:2674–85.
Veerhuis R, Hoozemans JJ, Janssen I, et al. Adult human microglia secrete cytokines when exposed to neurotoxic prion protein peptide: no intermediary role for prostaglandin E2. Brain Res. 2002;925:195–203.
Kim JI, Ju WK, Choi JH, et al. Expression of cytokine genes and increased nuclear factor-kappa B activity in the brains of scrapie-infected mice. Brain Res Mol Brain Res. 1999;73:17–27.
Lu Y, Liu A, Zhou X, et al. Prion peptide PrP106-126 induces inducible nitric oxide synthase and proinflammatory cytokine gene expression through the activation of NF-kappaB in macrophage cells. DNA Cell Biol. 2012;31:833–8.
Letendre SL, Woods SP, Ellis RJ, et al. Lithium improves HIV-associated neurocognitive impairment. AID. 2006;20:1885–8.
Jones-Brando LV, Buthod JL, Holland LE, Yolken RH, Torrey EF. Metabolites of the antipsychotic agent clozapine inhibit the replication of human immunodeficiency virus type 1. Schizophr Res. 1997;25:63–70.
Stommel EW, Graber D, Montanye J, Cohen JA, Harris BT. Does treating schizophrenia reduce the chances of developing amyotrophic lateral sclerosis? Med Hypotheses. 2007;69:1021–8.
Moots RJ, Al-Saffar Z, Hutchinson D, et al. Old drug, new tricks: haloperidol inhibits secretion of proinflammatory cytokines. Ann Rheum Dis. 1999;58:585–7.
Compliance with Ethics Guidelines
Conflict of Interest
Mamneet Manghera and Jennifer Ferguson declare that they have no conflict of interest. Renée Douville has received establishment and operating grants from the Manitoba Health Research Council, an operating grant from the Manitoba Medical Services Foundation, a starter grant from the ALS Association, and major and discretionary awards from the University of Winnipeg.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Infection
Rights and permissions
About this article
Cite this article
Manghera, M., Ferguson, J. & Douville, R. Endogenous Retrovirus-K and Nervous System Diseases. Curr Neurol Neurosci Rep 14, 488 (2014). https://doi.org/10.1007/s11910-014-0488-y
Published:
DOI: https://doi.org/10.1007/s11910-014-0488-y