Abstract
Primary central nervous system lymphoma (PCNSL) is a rare form of non-Hodgkin lymphoma, but in recent years the incidence in the immunocompetent population has been increasing. Elderly patients, or those over the age of 60 years, represent an important subgroup and account for over half of PCNSL patients. Treatment of older patients poses a number of challenges, and the optimum approach is yet to be defined. Chemotherapy, particularly with high-dose methotrexate as a single agent or in combination, is the mainstay of treatment of PCNSL. However, chemotherapy is associated with systemic toxicities, such as myelosuppression, to which the older patient is more vulnerable. Radiotherapy is also effective but is limited by significant delayed neurotoxicity, especially in older patients. Most studies support the use of chemotherapy-only treatments for elderly patients given the high risks of neurotoxicity associated with radiotherapy. Nevertheless, the prognosis remains poor regardless of the chemotherapy chosen. This article reviews the principles guiding the treatment of PCNSL in the elderly, identifies the limitations of current studies, and critically reports on the available literature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system lymphoma (PCNSL) is an extranodal form of non-Hodgkin lymphoma (NHL) that affects the brain, leptomeninges, spinal cord, and eyes. It is rare and accounts for only 3-4 % of all primary central nervous system tumors and 1-2 % of all lymphomas [1, 2]. Up to 95 % of PCNSLs are histologically identical to diffuse large B-cell lymphoma but invariably have a lower cure rate than their systemic counterpart. Approximately half of patients affected are older than 60 years, and the highest incidence has been reported in those older than 75 years [1]. The incidence of PCNSL has risen over the past 30 years in immunocompetent patients in all age groups and this cannot be explained by changes in medical practice, improvements in imaging, or increased disease awareness [3–6]. Notably, more recent studies indicate that the incidence is continuing to rise only in older patients whereas it has plateaued in younger age groups. This, along with an increasing aging population, emphasizes the relevance of an improved understanding of the treatment of PCNSL in the elderly [7].
This article will review the literature available on PCNSL in the elderly patient population, focusing on prognostic factors, treatments, and their limitations in this group of patients.
Age as a Prognostic Factor
The median survival of patients with PCNSL treated solely with supportive care has been reported as 1.9–3.3 months [8, 9]. With radiotherapy, it increases to 11–18 months [10–13], and with radiotherapy combined with chemotherapies such as methotrexate (MTX) and cytarabine (ara-C), it increases to 33–44.5 months [14–18]. The use of chemotherapy alone has also shown comparable results, with a median survival of 30-36 months [19–23]. These studies, however, have largely included younger patients with a high Karnofsky performance status and do not accurately predict survival in patients older than 60 years.
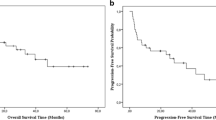
Older age significantly influences prognosis and treatment decisions (Fig. 1). PCNSL in older patients is associated with lower response rates, higher rates of relapse, and increased acute and delayed toxicities [24, 25, 26••, 27–30]. Age is the most significant predictor of the administration of any treatment, whether radiotherapy or chemotherapy, such that with increasing age, the rate of treatment decreases [31]. Data from the Surveillance Epidemiology and End Results (SEER) cancer registry linked with Medicare claims from 1994–2002 demonstrated an overall median survival of only 7 months in patients older than 65 years with a new diagnosis of PCNSL. Only 80 % of patients received treatment, and radiotherapy was the most frequently used treatment modality (36 %) as compared with combined modality treatment (26 %) or chemotherapy alone (17 %). Furthermore, treatment patterns were profoundly affected by age—only 66 % of patients older than 85 years were treated, and of those, 48 % were treated with radiotherapy alone [31.] In contrast, a retrospective study of PCNSL patients older than 65 years treated with chemotherapy at a tertiary care center at initial diagnosis demonstrated both treatment tolerability and a median overall survival of 25 months [32]. These findings suggest this group of patients may benefit from more aggressive approaches, and suboptimal treatment secondary to age, often administered outside tertiary care centers, may be partly responsible for worse outcomes.
Treatment algorithm for primary central nervous system lymphoma (PCNSL) in the elderly patient. PCNSL primary CNS lymphoma, rdWBRT reduced dose whole brain radiation, HD-AraC high-dose cytarabine, MTX methotrexate, HDCT high-dose chemotherapy, ASCT autologous stem-cell transplant. *Algorithm appropriate for any patient ≥ age 60 and should be considered for patients ≥ age 50
Even when treatment is identical, older patients often fare worse. Age has been identified as a prognostic factor in almost every clinical trial reported to date. It is also a critical component of each of the two major prognostic scoring systems described for PCNSL. In the Memorial Sloan-Kettering Cancer Center scoring system, age above 50 years confers a worse prognosis, whereas in the International Extranodal Lymphoma Study Group system, it is age above 60 years that is associated with worse outcome. In fact, age is a continuous variable, with each additional year associated with a worse chance of disease control and increased risk of toxicity [24, 25].
How to Define the “Elderly” Population
The de-escalation of care and underrepresentation of the elderly in clinical trials have prompted further exploration in an attempt to identify barriers and optimize treatment and quality of life [33–35]. Inconsistencies and bias in the definition of the “elderly” complicate the interpretation of many studies, which have included patients from 54-90 years of age [19, 20, 22, 36–41].
In reality, there is great heterogeneity even among patients of the same age within these broad groups. Older age is associated with an accumulation of physiologic deficits that alter the pharmacokinetics and pharmacodynamics of therapy and may increase the risk of toxicities such as nephrotoxicity and myelosuppression. Comorbid conditions and subsequent polypharmacy also play a significant role. Chronologic age, however, does not always correlate well with the degree of physiologic or physical decline in older patients, and functional status serves as an independent factor in predicting overall survival and drug toxicity [24, 25, 42, 43]. The Karnofsky performance status and Eastern Cooperative Oncology Group (ECOG) performance status are the most commonly applied performance measures. Unfortunately, these tools may not be adequate predictors in the elderly [44–46]. A more comprehensive predictive model that includes geriatric assessment tools and physiologic markers, such as hemoglobin level and creatinine clearance, may be necessary to evaluate geriatric vulnerability and treatment-related toxicity more effectively, but they have not been applied prospectively to older PCNSL patients [42, 47]. Nonetheless, in making a decision for treatment, one must consider age, comorbidities, and functional status both at the time of and prior to diagnosis.
Previous Treatments and Their Limitations in the Elderly Population
Treatment of PCNSL has changed significantly over the past few decades. Whole-brain radiotherapy (WBRT) induced a complete or partial response in most patients, increasing the median survival to 11-18 months [10–12, 48]. The results, however, were short-lived and 61 % of patients developed local recurrence, as demonstrated in Radiation Therapy Oncology Group (RTOG) study 8315. Outcomes were notably worse in patients older than 60 years, with a median survival of only 7.6 months [10].
This prompted further investigation into combined modality therapy (Table 1). Standard NHL regimens with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) failed to show improved survival compared with WBRT alone, partially owing to poor permeability of an intact blood–brain barrier for these agents [49, 50]. The use of MTX at doses greater than 1 g/m2 with leucovorin rescue helped to overcome this problem, and when combined with WBRT (45 Gy) resulted in a median survival of 30-40 months [14, 51–53]. Thus, MTX-based chemotherapy became the standard therapy for PCNSL. With the addition of other chemotherapeutic agents, such as procarbazine, ara-C, vincristine, and carmustine, to MTX-based chemotherapy and radiotherapy, further improvements in overall survival were achieved, but an increased frequency of grade 3 or grade 4 hematologic toxicity was observed as compared with use of single-agent MTX with WBRT [17, 18, 20, 54, 55]. Although patients older than 60 years in these studies had worse outcomes, they still had significant benefit, with median overall survival of 22-33 months, superior to that with WBRT alone [18, 20].
Radiation and Neurotoxicity
Prolonged survival, however, was accompanied by significant delayed treatment-related neurotoxicity observed more frequently in the elderly, which resulted in severe cognitive dysfunction, ataxia, and urinary incontinence. Neurotoxicity occurred in 19-83 % of patients older than 60 years who received WBRT following MTX-based chemotherapy at an average of 3-52 months after completing treatment [18, 20, 28, 52, 56•]. In a retrospective review of delayed neurotoxicity in 185 patients with PCNSL treated with high-dose MTX and WBRT, neurotoxicity increased over time and was often severe. Furthermore, it tended to occur earlier with advancing age at the time of treatment and was appreciated only with effective regimens that produced long-term remission. In addition, subtle cognitive changes were likely underestimated as no prospective neuropsychological tests or quality of life measures were incorporated. However, more than twice as many patients died of disease progression than neurotoxicity, suggesting that treatment vigorous enough to cause severe leukoencephalopathy was still not curative [28]. Although neurotoxicity is not limited to the elderly, it occurs more severely and rapidly in older patients, making this group a sensitive indicator of the neurotoxic potential of a given regimen in any group of patients.
In an attempt to reduce neurotoxicity without impairing outcomes, several studies have investigated reduced-dose WBRT or focused radiotherapy [18, 57–59]. In a subset analysis in the multicenter prospective study by the RTOG, a hyperfractionated schedule of WBRT with a reduced dose of 3,600 cGy was compared with standard 4,500-cGy WBRT. The reduced dose of radiotherapy did not compromise disease control and delayed, but did not prevent, neurotoxicity [18, 57]. The study was limited, however, as it did not assess efficacy specifically in older patients, who are at greatest risk of toxicity, and measured cognition with the mini-mental status examination, which likely underestimated the degree of neurocognitive impairment [60]. A preliminary report of 19 patients (seven older than 60 years) treated with reduced-dose WBRT (23.4 Gy) after achieving a complete response to MTX-based chemotherapy demonstrated promising efficacy and no cognitive decline in the 12 patients who completed a comprehensive neurocognitive assessment 2 years after treatment [59, 61]. However, a mild increase in treatment-related white matter changes, albeit less pronounced than with standard WBRT, was observed in nine patients following completion of treatment (6 or 12 months); four of those patients were older than 60 years. There was no significant correlation between treatment-related white matter changes and cognitive performance [61]. Although promising, these data need confirmation in a larger number of patients, particularly older patients, and longer follow-up to better assess relapse risk and cognitive function.
Current Treatment Approaches
The limitations of radiotherapy in the elderly have prompted exploration of chemotherapy-only treatment regimens for this cohort of patients (Table 2). The moderate efficacy of MTX-based regimens has been demonstrated in multiple phase II trials with doses ranging from 3 to 8 g/m2, achieving complete response rates of 30-79 % and median overall survival of 14-50 months [26••, 62–65]. Unfortunately, there was great variability in the patient characteristics and treatment regimens used in these studies, making it difficult to infer benefit for older patients. Salvage therapy with radiotherapy or other chemotherapeutic agents was frequently used in some studies and could account for prolonged overall survival even with short progression-free survival, but salvage treatment may also contribute to neurotoxicity.
High-Dose Methotrexate Monotherapy
MTX remains the single most important agent in all patients with PCNSL regardless of age group. Although the use of high-dose MTX in the elderly has been thought to require frequent dose adjustments because of reduced creatinine clearance and limited bone marrow reserve, there is good evidence that supports its tolerability. Mostly grade 1 and grade 2 nonhematologic and grade 1-3 hematologic toxicities were reported in 110 patients older than 60 years who received high-dose MTX (4 g/m2) for treatment of PCNSL. Less than 10 % grade 4 toxicity was reported. Specifically for hematologic toxicities, there was no significant difference in the severity and frequency of anemia, leukopenia, thrombopenia, or infections following treatment when compared with patients younger than 60 years. Dose reductions, however, were required more frequently in patients older than 60 years because of reduced creatinine clearance; efficacy of treatment was not assessed [40]. In two small retrospective studies of patients primarily older than 70 years treated with single-agent MTX at doses of 8 g/m2 adjusted for creatinine clearance, 60 % of patients had a complete response, median progression-free survival was 7.1-18 months, and median overall survival was 36-37 months [22, 41]. Dose reductions were required in as many as 87 % of patients; however, all patients received MTX doses of at least 4 g/m2 [41]. This suggests that patients older than 60 years may benefit from doses of 3-4 g/m2, which can be administered despite reduced creatinine clearance.
Methotrexate-Based Multidrug Regimens
The need for dose reductions of MTX in patients older than 60 years increases the relevance of other chemotherapeutic agents that can be used in conjunction with an MTX-based regimen. A randomized phase II trial strongly supported an added benefit of combination therapy, in this case MTX and ara-C compared with MTX alone [54]. Furthermore, with the increasing use of prophylactic colony-stimulating factors, myelotoxicity associated with combined chemotherapy can be reduced.
A nonrandomized study of combined chemotherapy alone demonstrated survival identical to that for the same chemotherapeutic regimen followed by WBRT in patients older than 60 years. MTX (3.5 g/m2) combined with vincristine and procarbazine yielded response rates as high as 90 %, and preliminary results in patients older than 60 years showed a median overall survival of 33 months compared with 32 months in those who received WBRT [20]. Long-term follow-up of these patients confirmed no significant difference in overall survival (29 months) between patients older than 60 years who received WBRT and patients older than 60 years who did not receive WBRT. Median progression-free survival, however, was 7 months in the group that deferred radiotherapy but had not yet been reached in the chemotherapy and radiotherapy group. There was a 25 % relapse rate with chemotherapy and radiotherapy as opposed to 58 % with chemotherapy alone, and neurotoxicity was reported in 75 % of patients who received radiotherapy. Thus, WBRT improved disease control and reduced relapse, but its attendant neurotoxicity resulted in death at the same rate as for patients treated with chemotherapy alone [21].
Similarly, the European Organisation for Research and Treatment of Cancer (EORTC) Brain Tumor Group conducted a multicenter phase II study of chemotherapy alone with 50 patients older than 60 years. Treatment consisted of MTX (1 g/m2), lomustine, procarbazine, methylprednisolone, intrathecally administered MTX, and intrathecally administered ara-C. A complete response was observed in 42 % of patients and a partial response was observed in 6 %. Median overall survival was 14.3 months. Delayed treatment-related neurotoxicity was reported in 12 % of patients. Although these results were not as favorable as in previous studies, survival was still twice as long as that 7 months after WBRT alone [37].
Comparable results have been reported with a number of different MTX-based chemotherapy regimens for patients older than 60 years, with differing degrees of toxicity dependent on the agents used [19, 23, 36–38]. In the most elderly patients, those aged 80 years and older, treatment with an MTX-based regimen, usually in combination with vincristine and procarbazine, resulted in an objective response in 62.5 % of patients and a median overall survival of 7.9 months; eight of the 28 patients survived 2 years or longer [66•]. Thus, MTX-based regimens can be well tolerated and produce prolonged disease control even in the oldest PCNSL patients. However, even with these regimens, recurrence is common, and improved therapies are needed.
Neurotoxicity also remains a concern with chemotherapy alone, especially in older patients. In a German phase III study, clinically determined neurotoxicity was seen in 26 % of long-term survivors in the chemotherapy alone arm, which was less than the 49 % incidence seen in patients who received chemotherapy and WBRT [26••]. Others have also noted both clinical and radiographic evidence of neurotoxicity in patients treated with chemotherapy [20, 21, 23, 37, 39, 56•, 65]. Thus, omitting WBRT substantially reduces but does not eliminate the risk of treatment-related cognitive impairment following successful treatment of PCNSL.
Novel Therapeutic Approaches
Novel approaches to treatment have focused on alternative chemotherapeutic agents and targeted drugs. The successful use of rituximab, a chimeric monoclonal antibody against the CD20 antigen, in diffuse large B-cell lymphoma prompted investigation of this agent for treatment of PCNSL, which is CD20 positive in at least 95 % of patients. Although rituximab penetrates the blood–brain barrier poorly, several studies have shown modest efficacy in the treatment of PCNSL [67–69]. This may be partly due to disruption of the blood–brain barrier in contrast-enhanced tumor. Clinical experience with rituximab in PCNSL is limited; several studies have demonstrated favorable response rates when combing rituximab with a high-dose MTX regimen both for induction therapy and salvage therapy, but it is unclear if rituximab enhances the response rate above that seen with the identical regimen without rituximab [59, 70–75]. Rituximab in combination with high-dose MTX (3 g/m2), procarbazine, and lomustine in 28 patients with PCNSL older than 65 years yielded a high response rate, with 64 % achieving a complete response following three 43-day cycles, and 18 % achieving a partial response. Three-year overall survival and progression-free survival were each 31 %; median progression-free survival was 16 months and median overall survival was 17.5 months. Patients older than 80 years, however, did not respond as well and had a median overall survival of 4.3 months, and grade 3 and grade 4 neutropenias were observed [71]. Intrathecal administration of rituximab has also been investigated and has demonstrated some benefit [59, 68].
A few studies have explored less toxic agents such as temozolomide. Twenty-three patients aged 60-79 years received induction chemotherapy with MTX (3.5 g/m2) and temozolomide (100 mg/m2), and patients who achieved a partial or complete response proceeded to maintenance therapy with MTX and temozolomide monthly for a maximum of five cycles; 33 % achieved a complete response, 55 % a partial response following induction, and 30 % received salvage WBRT. The median progression-free survival was 8 months, and the median overall survival was 35 months. No neurotoxicity was observed, but most patients received WBRT late in the course of the disease and died because of disease progression [36]. Although this regimen is well tolerated, efficacy greater than that of MTX alone has not yet been demonstrated.
The Role of Consolidation Therapy
In patients who have achieved a complete response after high-dose MTX-based induction therapy, it is unclear whether consolidation treatment improves disease control or survival. For older patients, however, consolidation with WBRT has a deleterious effect and compromises survival because of neurotoxic effects. A retrospective analysis of 122 patients who achieved complete response with MTX-based induction therapy assessed the impact of consolidation with WBRT, ara-C, or both on overall survival and failure-free survival. Intensive consolidation with WBRT and ara-C resulted in a longer median failure-free survival of 42 months compared with 15 months without consolidation, 18 months with ara-C alone, and 22 months with WBRT alone. There was no significant difference in overall survival, but a trend toward prolonged median overall survival with WBRT with or without high-dose ara-C compared with no consolidation was observed. This may be explained in part by the more favorable age and functional characteristics of those who received WBRT with ara-C; radiotherapy was also associated with higher rates of neurotoxicity [76]. Thus, intensive consolidation may provide better disease control without a clear impact on survival. This has been demonstrated in other studies as well [77, 78]. Particularly for elderly patients, who are at higher risk of neurotoxicity, radiation-sparing consolidation regimens such as high-dose ara-C may be a more reasonable option. However, consolidation treatment with chemotherapy has not been well studied and warrants further investigation.
Maintenance Therapy as Consolidation
Attempts have been made to use maintenance therapy to reduce relapse risk with mixed results. The North Central Cancer Treatment Group conducted a large trial using maintenance methylprednisolone therapy in patients older than 70 years following WBRT. A 6-month survival of only 33 % was reported, and the trial closed prematurely. Of note, the induction treatment regimen consisted of CHOP, which is ineffective, followed by WBRT [79]. MTX monthly following a complete response to single-agent MTX induction therapy resulted in a progression-free survival of only 12.8 months [63]. Maintenance rituximab therapy (more than 50 mg/m2 monthly) after complete response to induction or salvage therapy was studied in nine patients. Administration was well tolerated, with grade 2 neutropenia reported in only one patient and grade 3 hypogammaglobulinemia requiring immunoglobulin infusion in another patient. This study, however, included patients with recurrent PCNSL as well as those with systemic NHL with central nervous system involvement, and many had had multiple relapses. The treatment used before rituximab to achieve a complete response was quite variable, but progression-free survival ranged from 18.9 to 54.9 months, which is substantially longer than expected in patients with multiple relapses [80]. This may be reasonable in elderly patients who have achieved a complete response to induction or salvage chemotherapy and in whom radiotherapy can have deleterious consequences.
High-Dose Chemotherapy with Autologous Stem Cell Transplantation
In the younger patient population, high-dose chemotherapy followed by autologous stem cell rescue is a promising consolidation or salvage strategy [81–90]. Treatment-related mortality has been reported as high as 14 %, largely due to the hematologic toxicity of these regimens. This is an impractical approach for elderly patients and is usually not an option for the older population.
Treatment of Refractory and Recurrent Disease
Chemotherapy only with a high-dose MTX-based regimen can be efficacious but is associated with higher rates of relapse and shorter progression-free intervals, and many patients require salvage therapy. WBRT remains one of the most effective salvage treatments and has been used frequently, but it is still associated with neurotoxicity, particularly if given to older patients within 6 months of treatment with MTX [21, 64, 65, 91]. Reduced-dose WBRT is not an option as it would be inadequate treatment for bulky recurrent disease; it may be a consideration as consolidation after reinduction and response to chemotherapy [61].
Other studies have looked at optimal chemotherapy salvage regimens. Retreatment with high-dose MTX for patients who had an initial response to MTX gave an overall response rate of 91 % and an overall median survival of 61.9 months from the time of relapse. The median age of this cohort was 58 years, and nearly 41 % of patients were older than 60 years. All patients, however, had achieved a complete response to initial induction therapy [92].
Other chemotherapeutic agents have also been investigated with encouraging results [93, 94]. The combination of rituximab and temozolomide gave a median overall survival of 14 months and median progression-free survival of 7.7 months from relapse in patients with recurrent or refractory PCNSL [73]. A recent phase II study using a similar treatment regimen was less encouraging, with a median progression-free survival of 7 weeks, and was closed following an interim analysis [74]. These agents warrant further investigation as both are relatively well tolerated and may be beneficial in patients who are unable to receive aggressive chemotherapy because of potential toxicity.
To date, the best results have been obtained using induction chemotherapy with ara-C and etoposide followed by thiotepa, busulfan, and cyclophosphamide with stem cell rescue. Progression-free survival was 41.1 months in patients who had received transplants and overall survival was 58.6 months, but this treatment was used primarily in younger patients [89]. Toxicity was very high, and this transplant is not typically available to older patients.
Future Treatments: The Enrollment of Elderly Patients in Clinical Trials
There are a number of active clinical trials, some of which are designed specifically for older patients. Those most relevant to the elderly include an RTOG phase II randomized study examining the role of low-dose WBRT in patients treated with rituximab, MTX, procarbazine, and vincristine; neurotoxicity and quality of life are being evaluated prospectively in this trial [95]. Also in progress is a phase II study of MTX and temozolomide compared with MTX, procarbazine, and vincristine for patients older than 60 years [96]. Alternative agents and treatment strategies are also being explored, such as blood–brain barrier disruption, radiolabelled antibodies, and antiangiogenic agents such as pomalidomide [97–99]. These studies may offer effective treatment for patients who are at high risk of myelotoxicity and neurotoxicity. The elderly, however, are clearly underrepresented in most clinical trials, and future studies will need to focus on this specific population to improve outcomes and overall quality of life for this group of patients.
Conclusions
In spite of major advances in the treatment of PCNSL with MTX-based regimens, optimal treatment of the elderly remains challenging and uncertain. This is partly due to the vague definition of the elderly. Although in studies of PCNSL those older than 60 years are considered old, chronologic age may not be the best marker of tolerability of treatment and treatment-related toxicity because of great variability in functional status and comorbidities within this group of patients. High-dose MTX remains the single most important chemotherapeutic agent in treating PCNSL, even in the elderly, many of whom tolerate it without difficulty. Radiotherapy continues to play an important role; however, there is a clear predisposition to debilitating neurotoxicity following WBRT in patients older than 60 years and even in some younger patients. As demonstrated in a recent retrospective study, response to treatment is one of the most important predictors of survival in elderly patients [66•]. Thus, future trials may need to focus on stratification of patients older than 60 years with the goal of achieving and maintaining remission, increasing tolerability, and minimizing delayed treatment effects that can greatly compromise quality of life. Treatment in younger patients is with curative intent, but in the older population a more individualized approach needs to be taken. For the most elderly patients, the goals of treatment may need to be more palliative in nature and efforts should be steered toward minimizing toxicity and improving function. Fortunately, an increased understanding of the natural history of PCNSL, the limitations of treatment, and the vulnerability of older patients with PCNSL have brought greater attention to the need for more individualized care and will, hopefully, result in improved outcomes in the future.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Dolecek TA, Propp JM, Stroup NE, Kruchko C. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2005-2009. Neuro Oncol. 2012;14(Suppl 5):v1–49.
US Cancer Statistics Working Group. United States cancer statistics 1999-2004 Incidence and mortality Web-based report. Atlanta: US Department of Health and Human Services Center for Disease Control and Prevention and National Institute of Health; 2007–2008.
Olson JE, Janney CA, Rao RD, et al. The continuing increase in the incidence of primary central nervous system non-Hodgkin lymphoma: a surveillance, epidemiology, and end results analysis. Cancer. 2002;95:1504–10.
Werner MH, Phuphanich S, Lyman GH. The increasing incidence of malignant gliomas and primary central nervous system lymphoma in the elderly. Cancer. 1995;76:1634–42.
Eby NL, Grufferman S, Flannelly CM, et al. Increasing incidence of primary brain lymphoma in the US. Cancer. 1988;62:2461–5.
Cote TR, Manns A, Hardy CR, et al. Epidemiology of brain lymphoma among people with or without acquired immunodeficiency syndrome. AIDS/Cancer Study Group. J Natl Cancer Inst. 1996;88:675–9.
United States Census Bureau. Age and sex compositions: 2010. 2010 census briefs. Washington: United States Census Bureau; 2011.
Jellinger K, Radaskiewicz TH, Slowik F. Primary malignant lymphomas of the central nervous system in man. Acta Neuropathol Suppl. 1975;6:95–102.
Henry JM, Heffner Jr RR, Dillard SH, et al. Primary malignant lymphomas of the central nervous system. Cancer. 1974;34:1293–302.
Nelson DF, Martz KL, Bonner H, et al. Non-Hodgkin's lymphoma of the brain: can high dose, large volume radiation therapy improve survival? Report on a prospective trial by the Radiation Therapy Oncology Group (RTOG): RTOG 8315. Int J Radiat Oncol Biol Phys. 1992;23:9–17.
Gonzalez DG, Schuster-Uitterhoeve AL. Primary non-Hodgkin's lymphoma of the central nervous system. Results of radiotherapy in 15 cases. Cancer. 1983;51:2048–52.
Laperriere NJ, Cerezo L, Milosevic MF, et al. Primary lymphoma of brain: results of management of a modern cohort with radiation therapy. Radiother Oncol. 1997;43:247–52.
Berry MP, Simpson WJ. Radiation therapy in the management of primary malignant lymphoma of the brain. Int J Radiat Oncol Biol Phys. 1981;7:55–9.
Glass J, Gruber ML, Cher L, Hochberg FH. Preirradiation methotrexate chemotherapy of primary central nervous system lymphoma: long-term outcome. J Neurosurg. 1994;81:188–95.
Bessell EM, Graus F, Punt JA, et al. Primary non-Hodgkin's lymphoma of the CNS treated with BVAM or CHOD/BVAM chemotherapy before radiotherapy. J Clin Oncol. 1996;14:945–54.
Pollack IF, Lunsford LD, Flickinger JC, Dameshek HL. Prognostic factors in the diagnosis and treatment of primary central nervous system lymphoma. Cancer. 1989;63:939–47.
Blay JY, Bouhour D, Carrie C, et al. The C5R protocol: a regimen of high-dose chemotherapy and radiotherapy in primary cerebral non-Hodgkin's lymphoma of patients with no known cause of immunosuppression. Blood. 1995;86:2922–9.
DeAngelis LM, Seiferheld W, Schold SC, et al. Combination chemotherapy and radiotherapy for primary central nervous system lymphoma: Radiation Therapy Oncology Group study 93-10. J Clin Oncol. 2002;20:4643–8.
Freilich RJ, Delattre JY, Monjour A, DeAngelis LM. Chemotherapy without radiation therapy as initial treatment for primary CNS lymphoma in older patients. Neurology. 1996;46:435–9.
Abrey LE, Yahalom J, DeAngelis LM. Treatment for primary CNS lymphoma: the next step. J Clin Oncol. 2000;18:3144–50.
Gavrilovic IT, Hormigo A, Yahalom J, et al. Long-term follow-up of high-dose methotrexate-based therapy with and without whole brain irradiation for newly diagnosed primary CNS lymphoma. J Clin Oncol. 2006;24:4570–4.
Ng S, Rosenthal MA, Ashley D, Cher L. High-dose methotrexate for primary CNS lymphoma in the elderly. Neuro Oncol. 2000;2:40–4.
Pels H, Schmidt-Wolf IG, Glasmacher A, et al. Primary central nervous system lymphoma: results of a pilot and phase II study of systemic and intraventricular chemotherapy with deferred radiotherapy. J Clin Oncol. 2003;21:4489–95.
Ferreri AJ, Blay JY, Reni M, et al. Prognostic scoring system for primary CNS lymphomas: the International Extranodal Lymphoma Study Group experience. J Clin Oncol. 2003;21:266–72.
Abrey LE, Ben-Porat L, Panageas KS, et al. Primary central nervous system lymphoma: the Memorial Sloan-Kettering Cancer Center prognostic model. J Clin Oncol. 2006;24:5711–5.
•• Thiel E, Korfel A, Martus P, et al. High-dose methotrexate with or without whole brain radiotherapy for primary CNS lymphoma (G-PCNSL-SG-1): a phase 3, randomised, non-inferiority trial. Lancet Oncol. 2010;11:1036–47. This was the first phase III, noninferiority trial of high-dose MTX-based chemotherapy with or without WBRT. A total of 551 patients were enrolled, but because of high drop-out rates, 318 were analyzed. Although the trial did not meet its primary end point, WBRT increased progression free but not overall survival. Neurotoxicity in long-term survivors was less in the chemotherapy alone group compared with the chemotherapy and WBRT treatment arm.
Panageas KS, Elkin EB, DeAngelis LM, et al. Trends in survival from primary central nervous system lymphoma, 1975-1999: a population-based analysis. Cancer. 2005;104:2466–72.
Omuro AM, Ben-Porat LS, Panageas KS, et al. Delayed neurotoxicity in primary central nervous system lymphoma. Arch Neurol. 2005;62:1595–600.
Corry J, Smith JG, Wirth A, et al. Primary central nervous system lymphoma: age and performance status are more important than treatment modality. Int J Radiat Oncol Biol Phys. 1998;41:615–20.
Roth P, Martus P, Kiewe P, et al. Outcome of elderly patients with primary CNS lymphoma in the G-PCNSL-SG-1 trial. Neurology. 2012;79:890–6.
Panageas KS, Elkin EB, Ben-Porat L, et al. Patterns of treatment in older adults with primary central nervous system lymphoma. Cancer. 2007;110:1338–44.
Ney DE, Reiner AS, Panageas KS, et al. Characteristics and outcomes of elderly patients with primary central nervous system lymphoma: the Memorial Sloan-Kettering Cancer Center experience. Cancer. 2010;116:4605–12.
Townsley CA, Chan KK, Pond GR, et al. Understanding the attitudes of the elderly towards enrolment into cancer clinical trials. BMC Cancer. 2006;6:34.
Townsley CA, Naidoo K, Pond GR, et al. Are older cancer patients being referred to oncologists? A mail questionnaire of Ontario primary care practitioners to evaluate their referral patterns. J Clin Oncol. 2003;21:4627–35.
Monfardini S. What do we know on variables influencing clinical decision-making in elderly cancer patients? Eur J Cancer. 1996;32A:12–4.
Omuro AM, Taillandier L, Chinot O, et al. Temozolomide and methotrexate for primary central nervous system lymphoma in the elderly. J Neurooncol. 2007;85:207–11.
Hoang-Xuan K, Taillandier L, Chinot O, et al. Chemotherapy alone as initial treatment for primary CNS lymphoma in patients older than 60 years: a multicenter phase II study (26952) of the European Organization for Research and Treatment of Cancer Brain Tumor Group. J Clin Oncol. 2003;21:2726–31.
Taoka K, Okoshi Y, Sakamoto N, et al. A nonradiation-containing, intermediate-dose methotrexate regimen for elderly patients with primary central nervous system lymphoma. Int J Hematol. 2010;92:617–23.
Illerhaus G, Marks R, Muller F, et al. High-dose methotrexate combined with procarbazine and CCNU for primary CNS lymphoma in the elderly: results of a prospective pilot and phase II study. Ann Oncol. 2009;20:319–25.
Jahnke K, Korfel A, Martus P, et al. High-dose methotrexate toxicity in elderly patients with primary central nervous system lymphoma. Ann Oncol. 2005;16:445–9.
Zhu JJ, Gerstner ER, Engler DA, et al. High-dose methotrexate for elderly patients with primary CNS lymphoma. Neuro Oncol. 2009;11:211–5.
Hurria A, Togawa K, Mohile SG, et al. Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. J Clin Oncol. 2011;29:3457–65.
Schuurmans M, Bromberg JE, Doorduijn J, et al. Primary central nervous system lymphoma in the elderly: a multicentre retrospective analysis. Br J Haematol. 2010;151:179–84.
Terret C, Albrand G, Moncenix G, Droz JP. Karnofsky Performance Scale (KPS) or Physical Performance Test (PPT)? That is the question. Crit Rev Oncol Hematol. 2011;77:142–7.
Schag CC, Heinrich RL, Ganz PA. Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol. 1984;2:187–93.
Buccheri G, Ferrigno D, Tamburini M. Karnofsky and ECOG performance status scoring in lung cancer: a prospective, longitudinal study of 536 patients from a single institution. Eur J Cancer. 1996;32A:1135–41.
Soubeyran P, Fonck M, Blanc-Bisson C, et al. Predictors of early death risk in older patients treated with first-line chemotherapy for cancer. J Clin Oncol. 2012;30:1829–34.
Fine H, Loeffler J. Primary central nervous system lymphoma. In: Canellos G, Lister T, Sklar J, editors. The lymphomas. Philadelphia: Saunders; 1998. p. 481–94.
Schultz C, Scott C, Sherman W, et al. Preirradiation chemotherapy with cyclophosphamide, doxorubicin, vincristine, and dexamethasone for primary CNS lymphomas: initial report of Radiation Therapy Oncology Group protocol 88-06. J Clin Oncol. 1996;14:556–64.
O'Neill BP, O'Fallon JR, Earle JD, et al. Primary central nervous system non-Hodgkin's lymphoma: survival advantages with combined initial therapy? Int J Radiat Oncol Biol Phys. 1995;33:663–73.
O'Brien PC, Roos DE, Pratt G, et al. Combined-modality therapy for primary central nervous system lymphoma: long-term data from a Phase II multicenter study (Trans-Tasman Radiation Oncology Group). Int J Radiat Oncol Biol Phys. 2006;64:408–13.
Abrey LE, DeAngelis LM, Yahalom J. Long-term survival in primary CNS lymphoma. J Clin Oncol. 1998;16:859–63.
DeAngelis LM, Yahalom J, Thaler HT, Kher U. Combined modality therapy for primary CNS lymphoma. J Clin Oncol. 1992;10:635–43.
Ferreri AJ, Reni M, Foppoli M, et al. High-dose cytarabine plus high-dose methotrexate versus high-dose methotrexate alone in patients with primary CNS lymphoma: a randomised phase 2 trial. Lancet. 2009;374:1512–20.
Poortmans PM, Kluin-Nelemans HC, Haaxma-Reiche H, et al. High-dose methotrexate-based chemotherapy followed by consolidating radiotherapy in non-AIDS-related primary central nervous system lymphoma: European Organization for Research and Treatment of Cancer Lymphoma Group phase II trial 20962. J Clin Oncol. 2003;21:4483–8.
• Correa DD, Shi W, Abrey LE, et al. Cognitive functions in primary CNS lymphoma after single or combined modality regimens. Neuro Oncol. 2012;14:101–8. In this cross-sectional analysis, treatment-related neurotoxicity was assessed in 50 patients with PCNSL who received either chemotherapy alone or chemotherapy with WBRT. Patients had comprehensive neuropsychologic, mood, and quality of life testing. Patients treated with WBRT demonstrated a diffuse pattern of moderate to severe neuropsychologic deficits. Patients treated with chemotherapy did not meet the criteria for cognitive impairment, but test scores were one standard deviation below normal, suggesting subtle neurotoxicity associated with chemotherapy.
Fisher B, Seiferheld W, Schultz C, et al. Secondary analysis of Radiation Therapy Oncology Group study (RTOG) 9310: an intergroup phase II combined modality treatment of primary central nervous system lymphoma. J Neurooncol. 2005;74:201–5.
Shibamoto Y, Hayabuchi N, Hiratsuka J, et al. Is whole-brain irradiation necessary for primary central nervous system lymphoma? Patterns of recurrence after partial-brain irradiation. Cancer. 2003;97:128–33.
Shah GD, Yahalom J, Correa DD, et al. Combined immunochemotherapy with reduced whole-brain radiotherapy for newly diagnosed primary CNS lymphoma. J Clin Oncol. 2007;25:4730–5.
Correa DD, DeAngelis LM, Shi W, et al. Cognitive functions in survivors of primary central nervous system lymphoma. Neurology. 2004;62:548–55.
Correa DD, Rocco-Donovan M, DeAngelis LM, et al. Prospective cognitive follow-up in primary CNS lymphoma patients treated with chemotherapy and reduced-dose radiotherapy. J Neurooncol. 2009;91:315–21.
Sandor V, Stark-Vancs V, Pearson D, et al. Phase II trial of chemotherapy alone for primary CNS and intraocular lymphoma. J Clin Oncol. 1998;16:3000–6.
Batchelor T, Carson K, O'Neill A, et al. Treatment of primary CNS lymphoma with methotrexate and deferred radiotherapy: a report of NABTT 96-07. J Clin Oncol. 2003;21:1044–9.
Herrlinger U, Schabet M, Brugger W, et al. German Cancer Society Neuro-Oncology Working Group NOA-03 multicenter trial of single-agent high-dose methotrexate for primary central nervous system lymphoma. Ann Neurol. 2002;51:247–52.
Herrlinger U, Kuker W, Uhl M, et al. NOA-03 trial of high-dose methotrexate in primary central nervous system lymphoma: final report. Ann Neurol. 2005;57:843–7.
• Welch MR, Omuro A, Deangelis LM. Outcomes of the oldest patients with primary CNS lymphoma treated at Memorial Sloan-Kettering Cancer Center. Neuro Oncol. 2012;14:1304–11. This study is notable because it specifically examined outcomes in patients older than 80 years with PCNSL and included quality of life surrogates, such as number of days hospitalized. MTX-based therapy was well tolerated and effective. Initial response to induction therapy was also identified as a predictor of overall survival, suggesting that continued treatment in those without an initial response may not improve clinical and functional outcome and may compromise quality of life.
Ruhstaller TW, Amsler U, Cerny T. Rituximab: active treatment of central nervous system involvement by non-Hodgkin's lymphoma? Ann Oncol. 2000;11:374–5.
Pels H, Schulz H, Manzke O, et al. Intraventricular and intravenous treatment of a patient with refractory primary CNS lymphoma using rituximab. J Neurooncol. 2002;59:213–6.
Akyuz C, Aydin GB, Cila A, et al. Successful use of intraventricular and intravenous rituximab therapy for refractory primary CNS lymphoma in a child. Leuk Lymphoma. 2007;48:1253–5.
Chamberlain MC, Johnston SK. High-dose methotrexate and rituximab with deferred radiotherapy for newly diagnosed primary B-cell CNS lymphoma. Neuro Oncol. 2010;12:736–44.
Fritsch K, Kasenda B, Hader C, et al. Immunochemotherapy with rituximab, methotrexate, procarbazine, and lomustine for primary CNS lymphoma (PCNSL) in the elderly. Ann Oncol. 2011;22:2080–5.
Batchelor TT, Grossman SA, Mikkelsen T, et al. Rituximab monotherapy for patients with recurrent primary CNS lymphoma. Neurology. 2011;76:929–30.
Enting RH, Demopoulos A, DeAngelis LM, Abrey LE. Salvage therapy for primary CNS lymphoma with a combination of rituximab and temozolomide. Neurology. 2004;63:901–3.
Nayak L, Abrey LE, Drappatz J, et al. Multicenter phase II study of rituximab and temozolomide in recurrent primary central nervous system lymphoma. Leuk Lymphoma. 2013;54:58–61.
Jahnke K, Thiel E, Martus P, et al. Relapse of primary central nervous system lymphoma: clinical features, outcome and prognostic factors. J Neurooncol. 2006;80:159–65.
Ekenel M, Iwamoto FM, Ben-Porat LS, et al. Primary central nervous system lymphoma: the role of consolidation treatment after a complete response to high-dose methotrexate-based chemotherapy. Cancer. 2008;113:1025–31.
Reni M, Ferreri AJ, Guha-Thakurta N, et al. Clinical relevance of consolidation radiotherapy and other main therapeutic issues in primary central nervous system lymphomas treated with upfront high-dose methotrexate. Int J Radiat Oncol Biol Phys. 2001;51:419–25.
Ferreri AJ, Reni M, Pasini F, et al. A multicenter study of treatment of primary CNS lymphoma. Neurology. 2002;58:1513–20.
Laack NN, Ballman KV, Brown PB, et al. Whole-brain radiotherapy and high-dose methylprednisolone for elderly patients with primary central nervous system lymphoma: Results of North Central Cancer Treatment Group (NCCTG) 96-73-51. Int J Radiat Oncol Biol Phys. 2006;65:1429–39.
Ney DE, Abrey LE. Maintenance therapy for central nervous system lymphoma with rituximab. Leuk Lymphoma. 2009;50:1548–51.
Abrey LE, Moskowitz CH, Mason WP, et al. Intensive methotrexate and cytarabine followed by high-dose chemotherapy with autologous stem-cell rescue in patients with newly diagnosed primary CNS lymphoma: an intent-to-treat analysis. J Clin Oncol. 2003;21:4151–6.
Illerhaus G, Marks R, Ihorst G, et al. High-dose chemotherapy with autologous stem-cell transplantation and hyperfractionated radiotherapy as first-line treatment of primary CNS lymphoma. J Clin Oncol. 2006;24:3865–70.
Colombat P, Lemevel A, Bertrand P, et al. High-dose chemotherapy with autologous stem cell transplantation as first-line therapy for primary CNS lymphoma in patients younger than 60 years: a multicenter phase II study of the GOELAMS group. Bone Marrow Transplant. 2006;38:417–20.
Montemurro M, Kiefer T, Schuler F, et al. Primary central nervous system lymphoma treated with high-dose methotrexate, high-dose busulfan/thiotepa, autologous stem-cell transplantation and response-adapted whole-brain radiotherapy: results of the multicenter Ostdeutsche Studiengruppe Hamato-Onkologie OSHO-53 phase II study. Ann Oncol. 2007;18:665–71.
Illerhaus G, Muller F, Feuerhake F, et al. High-dose chemotherapy and autologous stem-cell transplantation without consolidating radiotherapy as first-line treatment for primary lymphoma of the central nervous system. Haematologica. 2008;93:147–8.
Yoon DH, Lee DH, Choi DR, et al. Feasibility of BU, CY and etoposide (BUCYE), and auto-SCT in patients with newly diagnosed primary CNS lymphoma: a single-center experience. Bone Marrow Transplant. 2011;46:105–9.
Soussain C, Suzan F, Hoang-Xuan K, et al. Results of intensive chemotherapy followed by hematopoietic stem-cell rescue in 22 patients with refractory or recurrent primary CNS lymphoma or intraocular lymphoma. J Clin Oncol. 2001;19:742–9.
Cheng T, Forsyth P, Chaudhry A, et al. High-dose thiotepa, busulfan, cyclophosphamide and ASCT without whole-brain radiotherapy for poor prognosis primary CNS lymphoma. Bone Marrow Transplant. 2003;31:679–85.
Soussain C, Hoang-Xuan K, Taillandier L, et al. Intensive chemotherapy followed by hematopoietic stem-cell rescue for refractory and recurrent primary CNS and intraocular lymphoma: Societe Francaise de Greffe de Moelle Osseuse-Therapie Cellulaire. J Clin Oncol. 2008;26:2512–8.
Brevet M, Garidi R, Gruson B, et al. First-line autologous stem cell transplantation in primary CNS lymphoma. Eur J Haematol. 2005;75:288–92.
Hottinger AF, DeAngelis LM, Yahalom J, Abrey LE. Salvage whole brain radiotherapy for recurrent or refractory primary CNS lymphoma. Neurology. 2007;69:1178–82.
Plotkin SR, Betensky RA, Hochberg FH, et al. Treatment of relapsed central nervous system lymphoma with high-dose methotrexate. Clin Cancer Res. 2004;10:5643–6.
Herrlinger U, Brugger W, Bamberg M, et al. PCV salvage chemotherapy for recurrent primary CNS lymphoma. Neurology. 2000;54:1707–8.
Arellano-Rodrigo E, Lopez-Guillermo A, Bessell EM, et al. Salvage treatment with etoposide (VP-16), ifosfamide and cytarabine (Ara-C) for patients with recurrent primary central nervous system lymphoma. Eur J Haematol. 2003;70:219–24.
Radiation Therapy Oncology Group. Combination chemotherapy, monoclonal antibody, and radiation therapy in treating patients with primary central nervous system lymphoma. http://www.clinicaltrials.gov/show/NCT0068250. Accessed Jan 2013.
Assistance-Publique-Hopitaux de Paris. Methotrexate and temozolomide versus methotrexate, procarabazine, vincristine, and cytarabine (CNS lymphoma). http://www.clinicaltrials.gov/show/NCT00503594. Accessed Jan 2013.
Iwamoto FM, Schwartz J, Pandit-Taskar N, et al. Study of radiolabeled indium-111 and yttrium-90 ibritumomab tiuxetan in primary central nervous system lymphoma. Cancer. 2007;110:2528–34.
Mayo Clinic. Study of pomalidomide for treatment of relapsed/refractory primary central nervous system lymphoma and newly diagnosed or relapsed/refractory intraocular lymphoma. http://www.clinicaltrials.gov/show/NCT01722305. Accessed Jan 2013.
OHSU Knight Cancer Institute. Rituximab and methotrexate chemotherapy with blood brain barrier disruption and sodium thiosulfate chemoprotection for patients with newly diagnosed PCNSL. http://www.clinicaltrials.gov/show/NCT00293475. Accessed Jan 2013.
Pels H, Juergens A, Glasmacher A, et al. Early relapses in primary CNS lymphoma after response to polychemotherapy without intraventricular treatment: results of a phase II study. J Neurooncol. 2009;91:299–305.
Conflict of Interest
Mariza Daras declares no conflict of interest.
Lisa M. DeAngelis has served on the BTG International Scientific Advisory Board.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Neuro-Oncology
Rights and permissions
About this article
Cite this article
Daras, M., DeAngelis, L.M. Management of Elderly Patients with Primary Central Nervous System Lymphoma. Curr Neurol Neurosci Rep 13, 344 (2013). https://doi.org/10.1007/s11910-013-0344-5
Published:
DOI: https://doi.org/10.1007/s11910-013-0344-5