Abstract
Background
Elderly patients with primary central nervous system malignant lymphoma (EL-PCNSL) may not be given sufficient treatment due to their poor pre-treatment Karnofsky Performance Status (KPS) and comorbidities. Therefore, a retrospective, cohort study was performed to evaluate risk factors associated with a poor prognosis of EL-PCNSL in the Tohoku Brain Tumor Study Group.
Methods
Patients aged ≥ 71 years with PCNSL were enrolled from eight centers. Univariate analysis was performed with the log-rank test. A Cox proportional hazards model was used for multivariate analysis.
Results
Three of the total 142 cases received best supportive care (BSC). Treatment was given to 30 cases without a pathological diagnosis, 3 cases with cerebrospinal fluid (CSF) cytology, and 100 cases with a pathological diagnosis. After confirmation of no differences in progression-free survival (PFS) and overall survival (OS) between the group treated without pathology and the groups diagnosed by pathology or CSF cytology and between median age ≥ 76 years and < 76 years, a total of 133 patients were studied. The median pre-treatment KPS was 50%. Median PFS and median OS were 16 and 24 months, respectively. Risk factors associated with poor prognosis on Cox proportional hazards model analysis were pre-treatment cardiovascular disease and central nervous system disease comorbidities, post-treatment pneumonia and other infections, and the absence of radiotherapy or chemotherapy.
Conclusions
Pre-treatment comorbidities and post-treatment complications would affect the prognosis. Radiation and chemotherapy were found to be effective, but no conclusions could be drawn regarding the appropriate content of chemotherapy and whether additional radiotherapy should be used.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system malignant lymphoma (PCNSL) is a rare disease, and usually more than half of the patients are over 60 years of age [1]; however, the percentage of PCNSL among all brain tumors has been increasing in recent years. In the Report of the Brain Tumor Registry of Japan, the percentage of all-age PCNSLs among all brain tumors increased from 3.2% in 2004 to 4.5% in 2008. The proportion of PCNSL occurring in patients aged 70 years or older (elderly patients with PCNSL (EL-PCNSL)) has also increased, from 28.1 to 35.9% [2, 3]. However, this applies not only to Japan, but also to other countries [2,3,4].
The Eastern Cooperative Oncology Group Performance Status (ECOG-PS) and Karnofsky Performance Status (KPS) before treatment are worse in EL-PCNSL than in younger patients, as reported by Zeremiski et al. [5], and more pre-treatment comorbidities have been reported [6]. Therefore, it is expected that EL-PCNSL would show the same tendency in Japan, which may lead to unavoidable best supportive care (BSC), omitted biopsies, and unsatisfactory treatment due to various pre-treatment comorbidities. In addition, EL-PCNSL are rarely included in prospective clinical trials [7, 8] making it difficult to determine their actual treatment status precisely [5, 9].
Therefore, how many patients are actually diagnosed and treated is not known. To answer this question, the incidence, treatment, and final outcome of PCNSL in elderly patients in the Tohoku and Niigata regions in the Tohoku Brain Tumor Study Group were examined to identify factors associated with a poor prognosis, and the Real-World status of PCNSL in elderly patients was examined.
Materials and methods
A Real-World study of all patients with immunocompetent EL-PCNSL aged 71 years or older who were treated or not treated including BSC at 8 centers participating in the Tohoku Brain Tumor Study Group from January 2011 to the end of December 2018 was performed. Cases diagnosed as PCNSL without biopsy or resection, cases treated based on cerebrospinal fluid (CSF) cytology, and cases treated based on biopsy or resection were included. To exclude secondary malignant lymphoma, pre-treatment CT, MRI, perfusion MRI, 8F-fluorodeoxyglucose (FDG) positron emission tomography (PET), blood sampling, and whole-body CT were performed in patients treated with or without biopsy. In patients who were treated without biopsy or resection, the response rate on MRI after treatment, and the overall course of the disease were reviewed to exclude other possible enhancing malignant tumors, and it was confirmed that they did not deviate from the clinical characteristics of lymphoma. Finally, the patients were enrolled at the discretion of the attending physician [10, 11]. Patients who underwent biopsy or resection were diagnosed as having CD-20-positive PCNSL by central pathological diagnosis.
An Excel questionnaire was sent to each institution, and the survey was conducted by linkable anonymizing from each patient’s medical record and image server. The survey items included basic patient information, time from initial symptom to diagnosis, pre-treatment KPS, pre-treatment comorbidities, target lesion location, maximum tumor diameter, multiple lesions or no, presence of dissemination on MRI or clinical symptoms, surgery, radiotherapy (RT), dose and technique of RT, presence of chemotherapy and number of cycles, presence of new post-treatment complications, and best MRI response at the end of treatment (within 3 months). KPS at 3 months, progression-free survival (PFS), treatment at recurrence, overall survival (OS), and cause of death were also investigated.
The start date of treatment was defined as the start date of chemotherapy or RT. For patients who could not receive chemotherapy or radiation for various reasons after biopsy or resection, the date of surgery was defined as the date of treatment initiation. PFS was defined as the date of confirmation of tumor growth or until the date of death. OS was defined as the date of final confirmation of survival or until the date of death. The last follow-up was December 31, 2018. Tumor size was determined using the Macdonald Criteria [12], and the response rate was determined according to the International Primary CNS Lymphoma Collaborative Group (IPCNSLCG) [13]. For the determination of the MRI best response rate within 3 months after treatment, the complete response rate (CRR) was defined as CR + CRu/CR + CRu + PR + SD + PD + NA (not determined). Pre-treatment comorbidity was defined as disease under treatment or follow-up at the time of initiation of treatment, and included previous treatment in the case of cancer.
In the statistical analysis, Mann–Whitney's U test, Fisher’s exact test, and the chi-squared test were used for comparisons between groups. For pre-treatment comorbidities and new post-treatment complications, only items with more than 10 comorbidities and complications were subjected to statistical analysis. Univariate analysis was performed by the log-rank test using the Kaplan–Meier method. A Cox proportional hazards model was used for multivariate analysis of risk factors. The entire statistical analysis was performed on a Mac OSX 10.15.7 operating system, using the JMP®14 (SAS Institute, Cary, NC, USA) statistical software.
Results
Patients’ background characteristics
A total of 142 patients were enrolled. Of these, two patients were excluded due to secondary central nervous system lymphoma. There were 3 cases of BSC without aggressive treatment based on imaging diagnosis alone. Thirty-one patients were treated with radiation or chemotherapy without surgery. Of these, 1 case was excluded due to difficulty in MRI follow-up, and only 3 cases were treated as PCNSL based on imaging diagnosis, cytological diagnosis by lumbar puncture, and abnormally high levels of IL-2R in CSF. A total of 103 patients underwent surgical removal or biopsy for tissue confirmation, and they were treated at each institution. These specimens were reviewed, but two cases had very little tumor cell component and could not be diagnosed by central pathological review, and one case had no tumor cell component and could not be diagnosed. All of the 100 cases with tissue confirmation were CD-20-positive, diffuse large B cell malignant lymphoma (DLBCL). A total of 133 cases, including 30 cases without tissue confirmation, 3 cases diagnosed by CSF examination, and 100 cases with tissue confirmation, were examined (Table 1 and Fig. 1).
CONSORT-style flow diagram of the study. The study involved 133 of 142 consecutive elderly patients with primary central nervous system malignant lymphoma in three groups. The first group was three patients in the best supportive care group of treatment without biopsy. The second group included 30 patients in the treatment group without biopsy. The third group included three patients in the cerebrospinal fluid cytology group and 100 patients in the biopsy and central pathological confirmation group
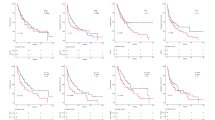
Table 2 shows the results for the no-surgery or biopsy group and the surgery or CSF cytology group. There was no significant difference between the two groups. However, the no-surgery and biopsy group had significantly more patients with a small tumor, CSF seeding, or a deep tumor (corpus callosum, basal ganglia, thalamus, corona radiata, ventricle, hypothalamus, and others). The median (m)PFS of the no-surgery and biopsy group and the surgery or CSF cytology group was 16 months (95% confidence interval (CI), 11–21 months) and 15 months (95% CI 11–21 months), respectively, with no significant difference (p = 0.79). The median (m)OS was 27 months (95% CI 12–52 months) and 21 months (95% CI 15–32 months), respectively, with no significant difference (p = 0.91) between the two groups (Fig. 2a, b).
Kaplan–Meier survival curves of progression-free survival (PFS) and overall survival (OS). a Kaplan–Meier survival curves of PFS comparing the no-surgery or biopsy group (gray line) and the surgery or CSF cytology group (black line). The median (m)PFS of the no-surgery and biopsy group and that of the surgery or CSF cytology group are not significantly different (p = 0.79). b Kaplan–Meier survival curves of OS comparing the no-surgery or biopsy group (gray line) and the surgery or CSF cytology group (black line). The mOS of the no-surgery and biopsy group and that of the surgery or CSF cytology group are not significantly different (p = 0.91). c Kaplan–Meier survival curves of PFS comparing the younger than 76 years group (gray line) and the group aged 76 years or older (black line). mPFS of the younger than 76 years group (gray line) and that of the group aged 76 years or older (black line) are not significantly different (p = 0.56). d Kaplan–Meier survival curves of OS comparing the younger than 76 years group (gray line) and the group aged 76 years or older (black line). mOS of the younger than 76 years group (gray line) and that of the group aged 76 years or older (black line) are not significantly different (p = 0.92)
Table 3 shows the comparison between the age groups using a cut-off of the median age of 76 years. There was no significant difference in mPFS between patients aged 76 years or older and patients younger than 76 years, except for the significant difference in bilateral disease in patients younger than 76 years; mPFS for patients aged 76 years or older and for those younger than 76 years was 16 months (95% CI 11–21 months) and 15 months (95% CI 11–21 months), respectively, with no significant difference (p = 0.56); mOS was 24 months (95% CI 12–30 months) and 21 months (95% CI 15–35 months; p = 0.92), respectively, with no significant difference between the two groups (Fig. 2c, d).
After these investigations, it was determined that there was little variation between the groups and ages, and a total of 133 patients were studied (Fig. 1). The characteristics of the 133 cases (65 males and 68 females; median age 76 years) are shown in Table 4. The pre-treatment KPS ranged from 30 to 90% (median 50%). As initial treatment, 110 patients (82.7%) received RT, and 97 patients (72.9%) received chemotherapy. RT alone was used in 32 patients (24.1%), with high-dose methotrexate (HD-MTX) + RT in 59 patients (44.4%), R-MPV (rituximab, MTX, procarbazine, and vincristine) (including MPV or R-MPV-A (rituximab, MTX, procarbazine, vincristine. and Ara-C)) + RT in 14 patients (10.5%); chemotherapy alone was used in only 14 patients (10.5%), and R-MPV (including MPV or R-MPV-A) was used in four patients (3.6%). In addition, four patients (3.0%) who were dropout cases in the early treatment phase failed to receive treatment in the initial phase (details below).
There were 61 cases of relapse during the follow-up period. Of these, 32 (52.5%) were given BSC as second-line therapy, accounting for about half of the cases. Salvage RT was added in 8 cases (13.1%), salvage RT and chemotherapy were added in 8 cases (13.1%), and salvage chemotherapy alone was added in 13 cases (21.3%). The final outcome at the end of follow-up was survival in 39 patients (29.3%) and death in 76 patients (57.1%), and no outcome information was available in 18 patients (13.5%) (Table 1).
Treatment and response rate
The overall m PFS was 16 months (95% CI 12–20 months) and m OS was 24 months (95% CI 16–30 months), despite the variety of treatments, RT, chemotherapy, and number of cycles. In addition, there was a significant difference in mOS between the 32 patients treated with RT alone and the 59 patients treated with HD-MTX + RT (12 months and 32 months, respectively; p < 0.001). A comparison of 32 patients in the RT alone group and 14 patients in the R-MPV + RT (including MPV or R-MPV-A) group also showed a significant difference (p = 0.036), although the R-MPV group had not yet reached mOS. There was no significant difference between the HD-MTX + RT treatment group and the R-MPV + RT (or MPV or R-MPV-A) group (p = 0.79). R-MPV or R-MPV therapy is a recently introduced therapy, with a maximum follow-up of 48 months.
The best response within the first 3 months of treatment was interpreted as CR in 35 (26.3%), CRu in 52 (39.1%), PR in 40 (30.1%), SD in 0 (0.0%), and PD in 3 (2.3%) cases. Thus, the CRR was 65.4% (87/133 cases) (Table 4 and Fig. 3).
Kaplan–Meier survival curves of progression-free survival (PFS) and overall survival (OS), and OS according to treatments. a PFS (gray line) and OS (black line) as a whole. b OS in patients who received radiotherapy (RT) (gray line) alone and high-dose methotrexate (HD-MTX) + RT (black line) (p < 0.001). OS in patients who received RT (gray line) alone and R-MPV (or MPV, or R-MPV-A) + RT (gray dot line) (p = 0.036). OS in patients who received HD-MTX (black line) + RT and R-MPV (or MPV, or R-MPV-A) + RT (gray dot line) (p = 0.36)
Pre-treatment comorbidities
There were 117 patients (88.0%) with pre-treatment comorbidities and 16 patients (12.0%) with no comorbidities. The total number of comorbidities was 213, or 1.8 comorbidities per patient. The most common pre-treatment comorbidity was hypertension, with 56 cases (26.3%). This was followed by central nervous system diseases such as post-stroke syndrome and dementia, with 24 cases (11.3%). Cardiovascular diseases such as arrhythmia, heart failure, angina pectoris, and myocardial infarction accounted for 21 cases (9.9%), comorbidities of systemic cancer other than brain tumor accounted for 20 cases (9.4%), and diabetes mellitus accounted for 17 cases (8.0%) (Tables 1 and 4).
Surgical complications within 1 month postoperatively and early treatment dropouts within 3 months
There were a total of 10 surgical complications within 1 month after surgery (9.7% of surgical cases). These included 2 cases of postoperative bleeding, 3 cases of deep vein thrombosis (DVT), 2 cases of pneumonia (1 case of Pneumocystis carinii pneumonia), and 1 case each of spontaneous pneumothorax, upper gastrointestinal bleeding, and urinary tract infection. A total of 15 (11.3%) patients dropped out within 3 months after the start of treatment, including those with complications from the above surgery, all of which occurred within 2 months. The breakdown was as follows: four patients died of complications including operation-related complications (26.7%), four patients died of tumors (26.7%), one patient refused treatment (6.7%), and six patients were lost to follow-up due to hospital transfer (40.0%). The breakdown of the four deaths due to complications was: one patient died of Pneumocystis carinii pneumonia, one patient died of pulmonary embolism (PE) due to upper gastrointestinal bleeding and deep venous thrombosis (DVT), one patient died of myelosuppression, cholecystitis, and pseudoenteritis, and one patient died of postoperative biopsy hemorrhage.
Post-treatment complications and causes of death
Tables 1 and 4 show the post-treatment complications (complications during the course of treatment), including the above early dropout cases. Fifty-four patients (40.6%) had some complications during the course of treatment, and 79 patients (59.4%) had no complications. The total number of complications was 84 in 54 patients, or a rate of 1.6 per patient. The most common complication was pneumonia and other infections in 28 patients (33.3%), followed by DVT, PE, and cardiac disease in 12 patients (14.3%), and renal dysfunction including delayed MTX excretion in 11 patients (13.1%). There were two cases of postoperative hemorrhage, including the above-mentioned fatal case.
The number of deaths at the last follow-up was 76 (57.1%), of which 38 (50.0%) were apparent tumor deaths, 33 (43.4%) were complication deaths, and 5 (6.6%) were deaths of unknown cause, accounting for about half of the deaths and about one-quarter of the total population. The breakdown of deaths due to complications was pneumonia and other infections in 15 patients (45.5%), accounting for about half of the deaths due to complications.
Risk factors associated with a poor prognosis
Univariate analysis
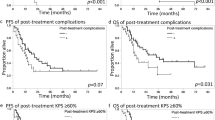
Significant differences in mPFS and mOS were observed for cardiovascular disease (PFS: + 8 months vs − 18 months, p = 0.004; OS: + 11 months vs. 27 months, p = 0.001), central nervous system disease (PFS: + 6 months vs − 18 months, p = 0.033; OS: + 9 months vs. − 26 months, p = 0.038), post-treatment KPS (PFS: < 60 11 months vs ≥ 60 19 months, p = 0.005; OS: < 60% 12 months vs. ≥ 60% 34 months, p < 0.001), presence of chemotherapy (PFS: + 7 months vs − 19 months, p < 0.001; OS: + 30 months vs. − 12 months, p < 0.001), presence of radiotherapy (PFS: + 7 months vs − 16 months, p = 0.029; OS: + 25 months vs. − 9 months, p = 0.045), best response of CRR within 3 months (PFS: CRR 20 months vs non-CRR 9 months, p = 0.032; OS: CRR 30 months vs. non-CRR 12 months, p = 0.013), post-treatment pneumonia and other infections (PFS: + 11 months vs − 19 months, p = 0.003; OS: + 16 months vs. 27 months, p < 0.001), and post-treatment DVT, PE, and cardiac complications (PFS: + 8 months vs − 16 months, p = 0.001; OS: + 11.5 months vs. 26 months, p = 0.001) (Table 4 and Fig. 4).
Kaplan–Meier survival curves of independent variables. a OS in patients with pre-operative cardiovascular disease (gray line) and without pre-operative cardiovascular disease (black line) (p = 0.001). b OS in patients with pre-operative central nervous disease (gray line) and without pre-operative central nervous disease (black line) (p = 0.038). c OS in patients who received radiotherapy (black line) and who did not receive radiotherapy (gray line) (p = 0.045). d OS in patients who received chemotherapy (black line) and who did not receive chemotherapy (gray line) (p < 0.001). e OS in patients who achieved post-treatment he complete response rate (CRR) (black line) and who did not achieve CRR (gray line) (p = 0.013). f: OS in patients with a post-treatment KPS score ≥ 60 (black line) and < 60 (gray line) (p < 0.001). g OS in patients with post-treatment pneumonia or other infections (gray line) and without post-treatment pneumonia and other infections (black line) (p < 0.001). h OS in patients with post-treatment deep venous thrombosis (DVT), pulmonary embolism (PE), or cardiovascular complications (gray line) and without post-treatment DVT, PE, and cardiovascular complications (black line) (p = 0.001)
Cox proportional hazards model
Multivariate analysis was performed using a Cox proportional hazards model for PFS. The results showed that there were significant associations with age (HR 1.993; 95%CI 1.1186–3.358; p = 0.009), pre-treatment cardiovascular disease (HR 3.008; 95%CI 1.508–5.803; p = 0.002), pre-treatment central nervous system disease (HR 2.686; 95%CI 1.318–5.233; p = 0.007), radiotherapy (− / + HR 3.064; 95% CI 1.573–5.965; p = 0.001), chemotherapy (− / + HR 4.615; 95% CI 2.563–8.274; p < 0.001), best response rate of CRR within 3 months (HR 1.863; 95% CI 1.090–3.137; p = 0.023), and post-treatment pneumonia and other infections (HR 2.936; 95% CI 1.586–5.352; p < 0.001). Multivariate analysis was performed using a Cox proportional hazards model for OS. The results showed that there were significant associations of OS with pre-treatment cardiovascular disease (HR 3.432; 95% CI 1.612–7.065; p = 0.002), pre-treatment central nervous system disease (HR 2.869; 95% CI 1.280–6.126; p = 0.012), radiotherapy(− / +) (HR 3.536; 95% CI 1.748–6. 854; p = 0.001), chemotherapy(− / +) (HR 3.733; 95%CI 1.994–6.959; p < 0.001), and post-treatment pneumonia and other infections (HR 3.505; 95% CI 1.827–6.665; p < 0.001); these were all determined to be independent prognostic factors (Table 5).
Discussion
The increase in the number of elderly patients with malignant lymphoma with a high rate of pre-treatment comorbidities and treatment-related complications is a common problem worldwide [6]. In the case of patients aged 70 years or older, PFS was 16.1 months in the elderly group compared to 35 months in the young group, even in CR cases, and there are reports that salvage therapy at the time of recurrence, including chemotherapy, was not performed[14], indicating that patients may not be treated satisfactorily. Previously, there was no definition of elderly and younger age groups using a cut-off value [15]. There are many reports that elderly patients have a worse prognosis, but the cut-off age ranged from 60 to 80 years [16,17,18,19], and a systematic review defined it as 75 years [20]. However, few cohorts have been directly compared. Zeremski et al. [5] retrospectively compared 20 consecutive cases in German Primary Central Nervous System Lymphoma Study Group-1 (G-PCNSL-SG-1). A comparative study was conducted between the HD-MTX basic therapy with whole-brain irradiation group as initial treatment and the irradiation avoidance group in which whole-brain irradiation was replaced with HD-AraC therapy, with 66 consecutive cases in the ‘real-life group’ treated otherwise. The median age was 62 and 70 years, with the real-life group being older, median KPS was 80% vs 70%, which also shows the poor condition of the real-life group, mOS was 33.4 months and 9.3 months, and mPFS was 24.8 months and 3.4 months, indicating that the elderly population was clearly in worse condition. Thus, there are very few studies of EL-PCNSL that are based on actual clinical practice, and in fact, there are probably quite a few cases that are not treated BSC cases. In the present study, only 3 of 142 enrolled patients had BSC, and it was shown that EL-PCNSL was treated fairly actively. Compared with the 'real-life group' of Zeremski et al. [5], the present cases had a higher median age of 76 years (vs. 70 years) and a lower pre-treatment KPS of 50% (vs. 70%). However, the treatment outcome was good, with PFS of 16 months (vs 3.4 months) and OS of 24 months (vs 9.3 months). The results of the present study are highly reliable because they are based on Real-World data collected from all patients in a regional center hospital, and one can assume that the data are almost complete.
In addition, although some cases of PCNSL are difficult to image, Japanese patients usually have non-germinal center type DLBCL(non-GCB) [21], and if PCNSL is immunocompetent, specific imaging findings such as CT, MRI, and FDG-PET, as well as clinical and spinal fluid examination findings, can be evaluated [22]. The risk of postoperative hemorrhage is also observed in a certain percentage of biopsy procedures [23]. In fact, in the present study, two cases of postoperative hemorrhage were observed, and one was a case of early death and dropout. Therefore, before treatment, the patient should be checked by CSF cytology if possible, whole-body FDG-PET CT, enhanced dynamic susceptibility weighted magnetic resonance (DSC-MR) perfusion imaging MRI, testicular ultrasound if possible, liquid biopsy for MYD88 mutation, and so on [10, 11, 24,25,26,27]. A liquid biopsy for MYD88 mutation to differentiate from glioblastoma or metastatic brain tumor, followed by a skip biopsy, may be one option for EL-PCNSL. In view of the potential complications of biopsy and the time required for diagnosis, the usefulness of liquid biopsy is also important [24, 27]. Although biopsy is the gold standard, it is useful to note that there were 30/142 (21.1%) such cases. In fact, in the comparison of differences between the biopsy group and the non-biopsy group, most of the patients with small deep dissemination were in the non-biopsy group, which clearly shows selection bias (Table 2). However, there was no significant difference in PFS or OS between the biopsy and non-biopsy groups (Fig. 2a, b). In fact, the Japanese Brain Tumor Society guidelines (JSNO) also mention that surgery is difficult for elderly and at-risk patients, which might be the Real-World situation in Japan [28]. In addition, the percentage of bilateral disease was higher in younger patients and lower in elderly patients when comparing patients aged 76 years or older and those younger (Table 3). One possible reason for this is that if PCNSL is generally divided into germinal center type (GCB) and non-GCB, GCB is more common in the middle line, whereas non-GCB is more likely to occur laterally [29]. Hans et al. reported that there is no difference between GCB and non-GCB depending on age [30], but there are many differences between GCB and non-GCB depending on race, with Japanese and other Asian people having more non-CGB [21] and non-GCB being more common in older age groups [31, 32]. Therefore, it is possible that bilateral disease is more common in patients under 76 years of age because of the high incidence of middle line disease, and less common in the elderly. In addition, although there were no significant differences in PFS and OS, elderly patients over 76 years of age tended not to receive chemotherapy (Tables 3 and 4). This includes old cases from around 2011, when MTX-based chemotherapy with high nephrotoxicity was avoided in the elderly and RT was used instead. As a result, no significant differences in PFS and OS were observed. In the present study as well, treatment mainly by HD-MTX has been performed for the past 10 years, but it is thought that treatment has been performed for each case according to the patient’s condition, and the number of treatment cycles and radiation methods varied. Under such circumstances, on both univariate and multivariate analyses of the presence or absence of RT and the presence or absence of chemotherapy, the prognosis of patients treated with RT and chemotherapy was significantly different from that of those treated without RT and chemotherapy. These results are noteworthy. The disadvantages of HD-MTX-based chemotherapy for EL-PCNSL are low rates of CR and PR and the short mPFS and mOS. A sub-analysis of the elderly patients in the G-PCMD-SG-1 trial also showed that the CR + PR rate was 44%, mPFS 4.0 was months, and mOS was 12.5 months, which was significantly worse than in the younger patients [14]. Furthermore, in the present study, 3 months CRR was 65.4% (87/133). Therefore, since Morris et al. [33] reported R-MPV therapy in 2013, R-MPV therapy has been introduced, but not all centers are on the same start, and the maximum follow-up period is 48 months, so the comparison with HD-MTX is short. In fact, this is the limitation of a retrospective study (Fig. 3).
Some reports have shown that pre-treatment low PS or KPS is associated with a poor prognosis in EL-PCNSL [16, 18,19,20, 34]. The report by Kasenda et al. [20] showing that pre-operative KPS ≥ 70% is the strongest prognostic factor for mortality in their large systematic review of 783 elderly PCNSL is particularly compelling. In the present cases, however, univariate analysis showed that pre-treatment KPS was irrelevant, but that there was a significant difference in KPS improvement after treatment. The reason for this might be that KPS would improve and the prognosis would improve if a therapeutic response were seen by aggressive intervention for EL-PCNSL patients. However, we believe that the cause of it not being identified as related to prognosis in the Cox proportional hazards model is stronger factor of systemic pre-treatment comorbidities and after treatment complications. In the analysis of factors associated with a poor prognosis, the results for OS were close to those for PFS, which may be attributed to the fact that 52.5% of patients (about half) received BSC as second-line treatment after relapse (Tables 4 and 5, Fig. 3). The significance of this suggestion that pre-treatment comorbidities, especially cardiac and central nervous system comorbidities, and post-treatment new infectious complications affect prognosis is great, and this is a point of focus that has not received much attention. In other words, if we pay attention to patients with pre-treatment comorbidities, minimize new post-treatment complications, and aggressively intervene in the treatment of patients with low PS, long-term survival could be expected even in EL-PCNSL patients.
This study has several inherent limitations, which has potential implications for its interpretation. First, this was a retrospective study, the data were provided by eight centers, and all patients with low KPS and various comorbidities were included. In addition, because the data were obtained from various centers, the treatment strategy was not uniform, and the overall PFS and OS may be biased. Second, it is difficult to make comparisons according to the type of chemotherapy because of the variety of treatments. Similarly, it is difficult to compare treatment outcomes due to the variety of radiotherapy techniques. Third, non-surgical cases were also included. Before and after treatment, fairly strict patient selection criteria were required, and the final decision was made by the attending physician. Although the possibility of misdiagnosis seems small, it cannot be ruled out that cases with misdiagnosis may be included. Fourth, the no-surgery cases showed selection bias for small, deep-seated, and disseminated tumors. Fifth, 6 (40%) of the patients who dropped out of treatment within 3 months included patients who were missing, which is a slightly high percentage and may potentially affect PFS and OS. Therefore, prospective studies with appropriately designed allocation factors including all elderly patients and patients with low PS are needed in the future. Sub-analyses of biological factors, MRI, cognitive function, and changes in PS are also necessary.
In conclusion, we have presented the Real-World status of EL-PCNSL. Patients were treated actively even at an advanced age, but further prospective studies are needed to determine the appropriate treatment. Factors associated with a poor prognosis included lack of radiation or chemotherapy, pre-treatment cardiovascular complications, history of brain disease, and new post-treatment infections.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Daras M, DeAngelis LM (2013) Management of elderly patients with primary central nervous system lymphoma. Curr Neurol Neurosci Rep 13(5):344. https://doi.org/10.1007/s11910-013-0344-5
Shibui S (2014) Report of brain tumor registry of Japan (2001–2005). Neurol Med Chir 54:10–102, 13th edn
Narita Y (2017) Report of brain tumor registry of Japan (2005–2008). Neurol Med Chir 57:9–102, 14th edn
Villano JL, Koshy M, Shaikh H et al (2011) Age, gender, and racial differences in incidence and survival in primary CNS lymphoma. Br J Cancer 105(9):1414–1418. https://doi.org/10.1038/bjc.2011.357
Mendez JS, Ostrom QT, Gittleman H et al (2018) The elderly left behind-changes in survival trends of primary central nervous system lymphoma over the past 4 decades. Neuro Oncol 20(5):687–694. https://doi.org/10.1093/neuonc/nox187
Ostrom QT, Gittleman H, Xu J et al (2016) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2009–2013. Neuro Oncol 18(Suppl_5):v1–v75. https://doi.org/10.1093/neuonc/now207
Zeremski V, Koehler M, Fischer T et al (2016) Characteristics and outcome of patients with primary CNS lymphoma in a “real-life” setting compared to a clinical trial. Ann Hematol 95(5):793–799. https://doi.org/10.1007/s00277-016-2602-5
Siegal T, Bairey O (2019) Primary CNS lymphoma in the elderly: the challenge. Acta Haematol 141(3):138–145. https://doi.org/10.1159/000495284
Ferreri AJ, Cwynarski K, Pulczynski E et al (2016) Chemoimmunotherapy with methotrexate, cytarabine, thiotepa, and rituximab (MATRix regimen) in patients with primary CNS lymphoma: results of the first randomisation of the International Extranodal Lymphoma Study Group-32 (IELSG32) phase 2 trial. Lancet Haematol 3(5):e217-227. https://doi.org/10.1016/s2352-3026(16)00036-3
Schorb E, Finke J, Ferreri AJ et al (2016) High-dose chemotherapy and autologous stem cell transplant compared with conventional chemotherapy for consolidation in newly diagnosed primary CNS lymphoma–a randomized phase III trial (MATRix). BMC Cancer 16:282. https://doi.org/10.1186/s12885-016-2311-4
Fallah J, Qunaj L, Olszewski AJ (2016) Therapy and outcomes of primary central nervous system lymphoma in the United States: analysis of the National Cancer Database. Blood Adv 1(2):112–121. https://doi.org/10.1182/bloodadvances.2016000927
Fox CP, Phillips EH, Smith J et al (2019) Guidelines for the diagnosis and management of primary central nervous system diffuse large B-cell lymphoma. Br J Haematol 184(3):348–363. https://doi.org/10.1111/bjh.15661
Goyal P, Kumar Y, Gupta N et al (2017) Usefulness of enhancement-perfusion mismatch in differentiation of CNS lymphomas from other enhancing malignant tumors of the brain. Quant Imaging Med Surg 7(5):511–519. https://doi.org/10.21037/qims.2017.09.03
Macdonald DR, Cascino TL, Schold SC Jr et al (1990) Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 8(7):1277–1280. https://doi.org/10.1200/jco.1990.8.7.1277
Abrey LE, Batchelor TT, Ferreri AJ et al (2005) Report of an international workshop to standardize baseline evaluation and response criteria for primary CNS lymphoma. J Clin Oncol 23(22):5034–5043. https://doi.org/10.1200/jco.2005.13.524
Roth P, Martus P, Kiewe P et al (2012) Outcome of elderly patients with primary CNS lymphoma in the G-PCNSL-SG-1 trial. Neurology 79(9):890–896. https://doi.org/10.1212/WNL.0b013e318266fcb2
Roth P, Hoang-Xuan K (2014) Challenges in the treatment of elderly patients with primary central nervous system lymphoma. Curr Opin Neurol 27(6):697–701. https://doi.org/10.1097/wco.0000000000000145
Ney DE, Reiner AS, Panageas KS et al (2010) Characteristics and outcomes of elderly patients with primary central nervous system lymphoma: the Memorial Sloan-Kettering Cancer Center experience. Cancer 116(19):4605–4612. https://doi.org/10.1002/cncr.25363
Schlegel U, Schmidt-Wolf IG, Deckert M (2000) Primary CNS lymphoma: clinical presentation, pathological classification, molecular pathogenesis and treatment. J Neurol Sci 181(1–2):1–12. https://doi.org/10.1016/s0022-510x(00)00385-3
Xie H, Dahiya S, Murphy ES et al (2013) Primary central nervous system lymphoma in the elderly: the Cleveland clinic experience. Anticancer Res 33(8):3251–3258
Lee SY, Okoshi Y, Kurita N et al (2014) Prognosis factors in Japanese elderly patients with primary central nervous system lymphoma treated with a nonradiation, intermediate-dose methotrexate-containing regimen. Oncol Res Treat 37(7–8):378–383. https://doi.org/10.1159/000363435
Kasenda B, Ferreri AJ, Marturano E et al (2015) First-line treatment and outcome of elderly patients with primary central nervous system lymphoma (PCNSL)—a systematic review and individual patient data meta-analysis. Ann Oncol 26(7):1305–1313. https://doi.org/10.1093/annonc/mdv076
Shiozawa E, Yamochi-Onizuka T, Takimoto M et al (2007) The GCB subtype of diffuse large B-cell lymphoma is less frequent in Asian countries. Leuk Res 31(11):1579–1583. https://doi.org/10.1016/j.leukres.2007.03.017
Chiavazza C, Pellerino A, Ferrio F et al (2018) Primary CNS lymphomas: challenges in diagnosis and monitoring. Biomed Res Int 2018:3606970. https://doi.org/10.1155/2018/3606970
Mizobuchi Y, Nakajima K, Fujihara T et al (2019) The risk of hemorrhage in stereotactic biopsy for brain tumors. J Med Invest 66(34):314–318. https://doi.org/10.2152/jmi.66.314
Baraniskin A, Schroers R (2021) Liquid biopsy and other non-invasive diagnostic measures in PCNSL. Cancers 13(11):2665. https://doi.org/10.3390/cancers13112665
Barajas RF, Politi LS, Anzalone N et al (2021) Consensus recommendations for MRI and PET imaging of primary central nervous system lymphoma: guideline statement from the International Primary CNS Lymphoma Collaborative Group (IPCG). Neuro Oncol 23(7):1056–1071. https://doi.org/10.1093/neuonc/noab020
Hiemcke-Jiwa LS, Leguit RJ, Snijders TJ et al (2018) Molecular analysis in liquid biopsies for diagnostics of primary central nervous system lymphoma: review of literature and future opportunities. Crit Rev Oncol Hematol 127:56–65. https://doi.org/10.1016/j.critrevonc.2018.05.010
Watanabe J, Natsumeda M, Kanemaru Y et al (2019) Comparison of circulating tumor DNA between body fluids in patients with primary central nervous system lymphoma. Leuk Lymphoma 60(14):3587–3589. https://doi.org/10.1080/10428194.2019.1639169
Neuro-Oncology TJSf (2019) The Japan Society for Neuro-Oncology, The Japan Neurosurgical Society (2019) Practical Guideline for Neuro-Oncology. Kanahara
Kinoshita M, Sasayama T, Narita Y et al (2014) Different spatial distribution between germinal center B and non-germinal center B primary central nervous system lymphoma revealed by magnetic resonance group analysis. Neuro Oncol 16(5):728–734. https://doi.org/10.1093/neuonc/not319
Hans CP, Weisenburger DD, Greiner TC et al (2004) Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 103(1):275–282. https://doi.org/10.1182/blood-2003-05-1545
Phang KC, Hussin NH, Abdul RF et al (2019) Characterisation of immunogenotypes of diffuse large B-cell lymphoma. Malaysian J Pathol 41(2):101–124
Umemura H, Homma M, Shiozwa E et al (2012) Immunohistochemical analysis of the cell cycle-associated proteins in diffuse large B-cell lymphoma. Showa IKaishi 72(1):108–117
Morris PG, Correa DD, Yahalom J et al (2013) Rituximab, methotrexate, procarbazine, and vincristine followed by consolidation reduced-dose whole-brain radiotherapy and cytarabine in newly diagnosed primary CNS lymphoma: final results and long-term outcome. J Clin Oncol 31(31):3971–3979. https://doi.org/10.1200/jco.2013.50.4910
Schuurmans M, Bromberg JE, Doorduijn J et al (2010) Primary central nervous system lymphoma in the elderly: a multicentre retrospective analysis. Br J Haematol 151(2):179–184. https://doi.org/10.1111/j.1365-2141.2010.08328.x
Acknowledgements
The authors would like to express their appreciation to all those who contributed to this study. Yuichi Sato MD, PhD (Department of Neurosurgery, Iwate Medical University), Masazumi Fujii MD, PhD (Department of Neurosurgery, Fukushima Medical University), Yoshihiro Kameoka MD, PhD, (Department of Hematology, Nephrology and Rheumatology, Akita University Graduate School of Medicine), all the doctors at all the institutions and the members of the Tohoku Brain Tumor Study Group, and all the staff of the Department of Anatomic Pathology, Hirosaki University Graduate School of Medicine.
Funding
This study did not receive any funding.
Author information
Authors and Affiliations
Contributions
KA and HO contributed to the concept and design of the study. KA and MM contributed to the acquisition and analysis of the data. AK contributed to central pathological diagnosis. All authors contributed to drafting the text and preparing the figure. KA, YY, TO, MN, TB, KM, MI, and MK contributed to acquisition of the data in individual institutions. KS, YS, KO, YF, HS, HO, and TT contributed to supervision in individual institutions. YS, CK, TK, and TT contributed to supervision and advising on the whole project.
Corresponding author
Ethics declarations
Conflict of interest
M. Natsumeda has received honoraria from Novocure; Y. Sonoda has received honoraria from Eisai, Dai-ichi Sankyo, and Chugai and research grants from Astellas, Eisai, Otsuka, Dai-ichi Sankyo, Chugai, Tsumura, Bayer, Pfizer, Fuji-film, and HOYA PENTAX; K. Asano, Y. Yamashita, T. Ono, T. Beppu, K. Matsuda, M. Ichikawa, M. Kanamori, M. Matsuzaka, A. Kurose, K. Saito, K. Ogasawara, Y. Fujii, H. Shimizu, H. Ohkuma, C. Kitanaka, T. Kayama, and T. Tominaga have no conflict of interest to declare.
Ethical approval
This study was conducted with the approval of the ethics committees of Hirosaki University Graduate School of Medicine (2018-118) and individual institutions. In addition, since this was a retrospective study, notifications to patients to opt-out were given on the homepage of each hospital.
Consent to participate
The institutional review board waived the requirement for informed consent, owing to the retrospective nature of the study. However, the details of the study are posted on the hospital’s homepage (http://www.med.hirosaki-u.ac.jp/~neuros/).
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Asano, K., Yamashita, Y., Ono, T. et al. The Real-World status and risk factors for a poor prognosis in elderly patients with primary central nervous system malignant lymphomas: a multicenter, retrospective cohort study of the Tohoku Brain Tumor Study Group. Int J Clin Oncol 27, 77–94 (2022). https://doi.org/10.1007/s10147-021-02042-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-021-02042-3