Abstract
Background A systemic and intraventricular polychemotherapy regimen (the Bonn protocol) without radiotherapy resulted in durable responses in 75% of patients <60 years with primary CNS lymphoma (PCNSL), but was complicated by a high rate of Ommaya reservoir infections. Here, the efficacy and toxicity of this regimen without intraventricular treatment was evaluated in PCNSL. Patients and methods From August 2003 to November 2005, 18 patients with PCNSL <60 years (median age, 53 years) were treated in a phase II trial with a high-dose methotrexate (MTX; cycles 1, 2, 4 and 5) and cytarabine (Ara-C; cycles 3 and 6) based systemic therapy including dexamethasone, vinca-alkaloids, ifosfamide and cyclophosphamide. Results Study accrual was prematurely stopped in November 2005 due to a high rate of early relapses. Seventeen of 18 patients were assessable for response: nine (53%) achieved complete response (CR), two (12%) complete response/unconfirmed (CRu) and two (12%) partial response (PR); four (24%) showed progressive disease (PD). One treatment was stopped due to toxicity. Median follow-up was 23 months, median response duration was only 10 months in responding patients, and median time to treatment failure (TTF) was 8 months in the whole group. Median overall survival (OS) has not been reached. Systemic toxicity was mainly hematologic. Conclusions In PCNSL patients <60 years, polychemotherapy without intraventricular treatment results in a high response rate, but is associated with early relapses in the majority of cases. This is in contrast to the results achieved with the same protocol but with intraventricular treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary CNS lymphomas (PCNSL) represent 3.1% of all primary brain tumors in the US [1]; the majority of these are classified as diffuse large cell lymphomas (DLCL) of the B-cell type [2]. Optimal treatment has not yet been defined. In 2003 we reported the results of a pilot/phase II study on a novel combined systemic and intraventricular chemotherapy regimen without radiotherapy in 65 consecutive patients [3]. The overall response rate was 71% for the whole group, median time to treatment failure (TTF) 21 months, and median overall survival (OS) 50 months. Results were significantly better in patients <60 years of age with a 86% overall response rate and a 75% survival fraction at 5 years. However, Ommaya reservoir infection occurred in 19% of the whole group and represented a serious complication in some patients, resulting in interruption or delay of chemotherapy [3]. Therefore, and considering data from the literature questioning the benefit of intraventricular chemotherapy in PCNSL [4, 5], we treated patients with systemic therapy only in a subsequent phase II trial initiated in August 2003.
Patients and methods
Inclusion criteria
All eligible patients had newly diagnosed histologically proven non-Hodgkin’s lymphoma (NHL) according to the REAL and WHO classifications [6, 7]. Patients with lymphoma at presentation involving sites other than the brain, meninges, cerebrospinal fluid (CSF) or the eyes were not included. Patients to be enrolled in this trial were stratified for age to make sure all patients <60 years of age received the same systemic chemotherapy as previously applied in the former pilot/phase II trial [3] but no intraventricular treatment, whereas patients 60–75 years of age received a modified regimen. Therefore, only patients <60 years of age were considered in this analysis. Exclusion criteria were age <18 years, inadequate bone marrow capacity, defined as neutrophils <1.5 × 109/l, platelets <100 × 109/l, and hemoglobin level <8 g/dl, known causes of immunosuppression, any previous malignancies, creatinine clearance below 60 ml/min, heart insufficiency NYHA grade IIIb, IV, uncontrolled infection or non-compensated active pulmonary or liver disease. Patients previously treated for PCNSL, except by steroids, were not included. Local ethics committees of all participating centers approved the study. All patients gave informed consent.
Baseline studies
Baseline studies were carried out in line with current recommendations of a workshop consensus of the International Primary CNS Lymphoma Collaborative Group (IPCG) [8] and consisted of magnetic resonance imaging (MRI) of the brain, CSF evaluation, bone marrow biopsy and cytology, chest and abdominal computed tomography (CT), and ophthalmologic evaluation including slit-lamp examination.
Treatment protocol and study design
The initial protocol has been applied in a pilot/phase II trial including intraventricular therapy with MTX, Ara-C and dexamethasone during each cycle [3]. The clinical trial cited here was an open-label, non-randomized study. Treatment consisted of six chemotherapy cycles separated by 2 weeks between each cycle. In contrast to the previously published pilot/phase II trial [3], neither intraventricular nor intrathecal therapy was administered. Details of the protocol are given in Table 1. Systemic chemotherapy was administered as described [3].
Evaluation of response and toxicity
Response was determined after the second and the sixth chemotherapy cycle by contrast-enhanced MRI of the brain. Response criteria were used as recommended by the IPCG consensus; all respective MRI studies were re-evaluated for this analysis according to these criteria [8]: Complete response (CR) was defined as the disappearance of all enhancing lesions on MRI of the brain in patients who were off steroids, unconfirmed complete response (CRu) was defined as a minimal residual enhancing lesion in the region of biopsy/hemorrhage without change or with involution during follow-up, partial response (PR) as a reduction of enhancing tumor volume by more than 50%, progressive disease (PD) as an increase of tumor volume of more than 25% or occurrence of new lesions, and stable disease (SD) as any other situation [9]. Treatment failure was defined as PD or SD, relapse after initial response, death or discontinuation of chemotherapy due to any cause. Acute toxicity was graded according to the WHO system [10].
Follow-up
All patients were followed every 3 months within the 1st year after therapy and every 6 months thereafter. Follow-up comprised neurological examination, MRI, CSF examination and ophthalmologic evaluation.
Prognostic factors
The current study population and patients <60 years of age treated in the former trial with systemic and intraventricular chemotherapy [3] were analyzed for factors proposed to have prognostic significance [11, 12].
Neuroradiological findings at relapse
In order to evaluate if relapse patterns would be different in patients being treated with or without intraventricular chemotherapy, all MR images at relapse were evaluated and were re-assessed in the cohort of the former trial. Meningeal involvement was defined as confluent leptomeningeal contrast enhancement and was not diagnosed if only juxtameningeal or periventricular lesions were detectable.
Statistics
Primary endpoint was response. The design of the study was a non-inferiority design: It was hypothesized that the response rate to the treatment protocol would not be inferior to the response rate in the published phase II trial (including intraventricular treatment). Assuming this response rate of 86% [3], inclusion of 110 patients would result in a response rate of >75% with a 95% confidence interval and a power of 90% at a level of significance of 0.05. Secondary endpoints were TTF, OS, response duration and treatment-related morbidity. OS and TTF were calculated from the date of histological diagnosis to death, treatment failure or last date of follow-up, respectively. Response duration was defined as the date CR, CRu or PR was first documented until the date of relapse, disease progression, death of any cause or last follow-up, respectively. Relapse or progression was defined as (re)growth of the tumor at any site within or outside the CNS. TTF and response duration were estimated by the Kaplan-Meier method [13]. Annual interim analyses were carried out in order to assess pre-defined criteria resulting in premature termination of the trial: (1) a mortality rate due to treatment of >20% or (2) a response rate of <75% if the power analysis would then reveal that the aim of the trial could no longer be achieved.
Results
Between August 2003 and an interim analysis in November 2005, 44 consecutive patients from seven centers were enrolled in this phase II trial. Of these, 18 were <60 years of age. In this age group no component of the prior protocol had been changed with the exception of omitting intraventricular therapy. Since systemic treatment was modified in patients ≥60 years, only the results in the younger patients are presented here: Their median age was 53 years (range, 27–59 years), and their median Karnofsky performance score (KPS) was 80% (range, 50–100%).
In total, 97 cycles of chemotherapy were administered. Complete treatment without modification was given to ten patients. Four patients received a modification of treatment, since a reduction of MTX dosage was necessary due to a transient decrease of creatinine clearance. Reasons for incomplete treatment were termination of therapy due to toxicity (one patient) and discontinuation of treatment due to PD under therapy (four patients).
Treatment response
One patient was not assessable for response because therapy was terminated after the first cycle due to hepatotoxicity, grade IV. From the remaining 17, 9 (53%) showed CR, 2 (12%) CRu and 2 (12%) PR. In four (24%) the tumor was progressive despite therapy. None of the patients with PR or CRu received any further initial therapy.
Time to treatment failure, overall survival and response duration
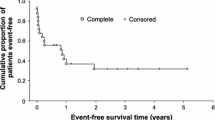
Follow-up was 2–41 months (median: 23 months) in the whole group and 2–41 months (median 24 months) for surviving patients. During follow-up, 14 events defined as treatment failures and 4 deaths occurred. The Kaplan–Meier estimate for median TTF was 8 months (95% CI, 6–9 months); the median OS is not yet reached. The median response duration in 13 patients with CR, CRu or PR was 10 months (95% CI, 4–15 months). The Kaplan–Meier analysis of response duration is depicted in Fig. 1a and of TTF in Fig. 1b in comparison to data of patients <60 years having received the same protocol with inclusion of intraventricular treatment [3]. The median response duration in patients of this former trial had not been reached after a follow-up of 3–87 months (median, 32 months); therefore, the difference between response duration/TTF of patients treated with and without intraventricular chemotherapy is highly significant with P < 0.005/P = 0.007. In this former trial, median TTF and median OS for patients <60 years have not yet been reached [3].
In order to analyze if differences in prognostic scores [11, 12] may have influenced the different outcomes in the current versus the historical study population, these factors were evaluated. Data to classify patients according to a prognostic score as published by the IELSG [11] were completed for 10 out of 18 patients of the current trial and for 24 out of 30 patients of the former trial. Comparing the different risk scores (IELSG score 0–1: low risk; 2–3: intermediate risk; 4–5: high risk), there was a trend towards a lower risk of the patients in the current trial. All patients from both study groups could also be classified according to the Memorial Sloan Kettering Cancer Center prognostic model [12]. Again, a trend towards a better prognostic score for the patients in the current treatment trial could be found when applying this model. Both classifications showed no significant difference between the two patient groups (data not shown).
Toxicity
Toxicity could be analyzed in 60 chemotherapy cycles administered in ten patients. WHO grade IV leucopenia (thrombocytopenia) occurred in one patient (two) and was short lasting. WHO grade III leucopenia (thrombocytopenia) occurred in three (two) patients. Nine patients experienced WHO grade 3/4 infections. Two patients developed episodes of transient nephrotoxicity WHO grade II, and four suffered from mucositis. In one patient, therapy had to be discontinued due to treatment-induced hepatotoxicity, grade IV. No therapy-associated cognitive dysfunction was found in any of the patients after chemotherapy or at follow-up; however, formal neuropsychometric testing was not carried out.
Treatment at relapse
In four patients, the disease was progressive; nine patients relapsed. Salvage treatment was carried out according to the treating physician’s decision with different regimens, including high-dose chemotherapy with stem-cell rescue in three patients (n = 1 for PD and n = 2 for relapse) [14]. All three showed CR. Eight patients were irradiated either at progression (n = 3) or at relapse (n = 5). Three of those showed CR, two achieved a PR, one patient showed a SD, and in two patients a tumor progression was diagnosed. Two patients suffered from a second relapse after salvage therapy. One patient, treated with high-dose chemotherapy, achieved a CR; the other patient was irradiated and achieved a PR thereafter.
Neuroradiological findings at relapse
MRI findings at progression or relapse were evaluable in 12 patients. Leptomeningeal involvement was found in 6/12 patients (1 isolated leptomeningeal relapse and 5 combined parenchymatous and leptomeningeal). In six other patients an isolated parenchymatous relapse was seen. For localization of primary tumor manifestation and at tumor relapse or progression, see Table 2. Re-evaluation of MRI scans in patients suffering either from relapse (n = 6) or PD (n = 2) in the former trial with intraventricular therapy [3] showed leptomeningeal involvement only in one.
Discussion
Clinical trials in PCNSL have exploited therapy with high-dose MTX alone [15–17], MTX-based polychemotherapy [3, 18] and a combination of MTX-based chemotherapy with whole-brain radiotherapy [19–23]. MTX as a sole treatment in two multicenter trials at a dosage of 8 g/m2 every 14 days for six cycles has resulted in complete response (CR) rates of 29%/52% and in a median survival of 25/55.8 months, respectively [16, 24, 25]. Combination chemo-/radiotherapy has resulted in OS rates of up to 60 months [21]; however, careful follow-up has identified a large fraction of such patients suffering from late treatment-related neurotoxicity [21, 26–28]. Treatment-induced neurotoxicity is less frequent in long-term survivors after chemotherapy alone for PCNSL [29–31]. Therefore, optimizing chemotherapy regimens in order to defer whole-brain radiotherapy is essential.
This trial aimed at reproducing the results after combined systemic and intraventricular chemotherapy in PCNSL patients <60 years of age with a 5-year survival fraction of 75% [3]. Reasons to omit intraventricular therapy in the current trial were a high Ommaya reservoir infection rate and data from retrospective analysis putting into doubt the necessity of intraventricular treatment [4, 5]. However, an interim analysis 2 years after initiation of this trial revealed an unexpectedly high relapse rate with a median response duration of only 10 months in responding patients. In comparison, the response duration has not been reached after 32 months of median follow-up in the former trial [3]. Though poor response duration had not been a predefined criterion for premature study termination, the trial committee decided to close the trial after 26 months of patient accrual. At this time 18 patients <60 years had been enrolled and were further followed; 17 of these were evaluable for response.
The overall response rate in this group was 76% and therefore comparable with the respective value of 86% in the former trial [3]. However, TTF and response durations in the whole group as well as response durations in responding patients were significantly lower with a significance level of P < 0.01. In order to analyze whether this difference was due to an imbalance of patients with worse clinical prognosis — independent of treatment — we evaluated patients of both trials for established prognostic factors [11, 12]. No such differences could be detected. Re-evaluation of MR images at relapse in the former and in the current trial suggested a higher incidence of leptomeningeal tumor manifestation in patients not treated with intraventricular therapy. However, this finding is not sturdy data, since routine CSF examination has not been carried out in all patients at relapse. It is important to point out that the majority of patients suffering from either relapse or tumor progression in the current study showed response to salvage therapy. In both trials, in the current study and in the former trial, OS has not been reached yet. However follow-up in the current study is rather short; therefore, no comparison of OS data between the two trials is possible.
Two retrospective analyses addressing the efficacy of intrathecal chemotherapy in PCNSL [4, 5] did not find the inclusion of this modality to influence survival. Precise dosage, application route and schedule of intrathecal therapy were not given in a retrospective analysis on 109 out of 363 PCNSL patients treated with heterogeneous regimens, including chemotherapy alone, radiotherapy (RT) alone, RT followed by chemotherapy and vice versa [4]. However, only 11 out of the 109 patients treated with intrathecal chemotherapy had not been treated with RT in this series [4]. Given the fact that RT is an efficient modality to control lymphomatous meningial tumor manifestation, a possible prophylactic or therapeutic effect of intrathecal chemotherapy might have been obscured by whole-brain RT. In a retrospective single-center case-controlled study [5], the outcome of 14 PCNSL patients not being treated with intrathecal chemotherapy was compared with that of 28 matched patients having received five serial weekly dosages of 12 mg MTX via an Ommaya reservoir alternating with systemic MTX. Patient groups were balanced for clinical prognostic factors as well as for the percentage having received irradiation. Neither event-free survival nor OS was influenced by the addition of intraventricular therapy in this retrospective case-controlled series [5]. Therapeutic differences in this analysis [5] in comparison with our former series [3] were dosage, timing and composition of intraventricular treatment. Irrespective of the question, if these differences are sufficient to explain the discrepancy between our observation and data in the literature, the results of the present trial suggest that long-term tumor control in PCNSL with a polychemotherapy regimen developed by our group [3] is only possible if local treatment of the CSF compartment is included. Since in young patients with PCNSL cure is the aim, it is disappointing that just omitting intraventricular treatment leaves this protocol no more efficient than other less demanding regimens [15–17]. However, a possible role of the CSF compartment as a sanctuary for lymphomatous tumor cells in PCNSL is suggested by this observation, which might be more important in chemotherapy-alone protocols than previously acknowledged.
References
Central Brain Tumor Registry of the United States (2005) Statistical report: primary brain tumors in the United States. Chicago, IL
Harris NL, Jaffe ES, Diebold J et al (2000) Lymphoma classification—from controversy to consensus: the REAL and WHO Classification of lymphoid neoplasms. Ann Oncol 11(Suppl 1):3–10. doi:10.1023/A:1008383406103
Pels H, Schmidt-Wolf IG, Glasmacher A et al (2003) Primary central nervous system lymphoma: results of a pilot and phase II study of systemic and intraventricular chemotherapy with deferred radiotherapy. J Clin Oncol 21:4489–4495. doi:10.1200/JCO.2003.04.056
Ferreri AJ, Reni M, Pasini F et al (2002) A multicenter study of treatment of primary CNS lymphoma. Neurology 58:1513–1520
Khan RB, Shi W, Thaler HT et al (2002) Is intrathecal methotrexate necessary in the treatment of primary CNS lymphoma? J Neurooncol 58:175–178. doi:10.1023/A:1016077907952
Harris NL, Jaffe ES, Stein H et al (1994) A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood 84:1361–1392
Gatter KCWR (2001) Diffuse large cell lymphoma. IARC Press, Lyon, France
Abrey LE, Batchelor TT, Ferreri AJ et al (2005) Report of an international workshop to standardize baseline evaluation and response criteria for primary CNS lymphoma. J Clin Oncol 23:5034–5043. doi:10.1200/JCO.2005.13.524
Macdonald DR, Cascino TL, Schold SC Jr et al (1990) Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 8:1277–1280
World Health Organization (1979) WHO handbook for reporting results of cancer treatment. In: WHO offset publication no 48. World Health Organization, Geneva, Switzerland, pp 14–21
Ferreri AJ, Blay JY, Reni M et al (2003) Prognostic scoring system for primary CNS lymphomas: the International Extranodal Lymphoma Study Group experience. J Clin Oncol 21:266–272. doi:10.1200/JCO.2003.09.139
Abrey LE, Ben-Porat L, Panageas KS et al (2006) Primary central nervous system lymphoma: the Memorial Sloan-Kettering Cancer Center prognostic model. J Clin Oncol 24:5711–5715. doi:10.1200/JCO.2006.08.2941
Kaplan ELMP (1958) Non parametric estimations from complete observations. J Am Stat Assoc 53:163–179. doi:10.2307/2281868
Soussain C, Hoang-Xuan K, Levy V (2004) Results of intensive chemotherapy followed by hematopoietic stem-cell rescue in 22 patients with refractory or recurrent primary CNS lymphoma or intraocular lymphoma. Bull Cancer 91:189–192
Batchelor T, Carson K, O’Neill A et al (2003) Treatment of primary CNS lymphoma with methotrexate and deferred radiotherapy: a report of NABTT 96-07. J Clin Oncol 21:1044–1049. doi:10.1200/JCO.2003.03.036
Herrlinger U, Kuker W, Uhl M et al (2005) NOA-03 trial of high-dose methotrexate in primary central nervous system lymphoma: final report. Ann Neurol 57:843–847. doi:10.1002/ana.20495
Guha-Thakurta N, Damek D, Pollack C et al (1999) Intravenous methotrexate as initial treatment for primary central nervous system lymphoma: response to therapy and quality of life of patients. J Neurooncol 43:259–268. doi:10.1023/A:1006210703827
Hoang-Xuan K, Taillandier L, Chinot O et al (2003) Chemotherapy alone as initial treatment for primary CNS lymphoma in patients older than 60 years: a multicenter phase II study (26952) of the European Organization for Research and Treatment of Cancer Brain Tumor Group. J Clin Oncol 21:2726–2731. doi:10.1200/JCO.2003.11.036
DeAngelis LM, Seiferheld W, Schold SC et al (2002) Combination chemotherapy and radiotherapy for primary central nervous system lymphoma: Radiation Therapy Oncology Group Study 93-10. J Clin Oncol 20:4643–4648. doi:10.1200/JCO.2002.11.013
O’Brien P, Roos D, Pratt G et al (2000) Phase II multicenter study of brief single-agent methotrexate followed by irradiation in primary CNS lymphoma. J Clin Oncol 18:519–526
Abrey LE, Yahalom J, DeAngelis LM (2000) Treatment for primary CNS lymphoma: the next step. J Clin Oncol 18:3144–3150
Bessell EM, Lopez-Guillermo A, Villa S et al (2002) Importance of radiotherapy in the outcome of patients with primary CNS lymphoma: an analysis of the CHOD/BVAM regimen followed by two different radiotherapy treatments. J Clin Oncol 20:231–236. doi:10.1200/JCO.20.1.231
Poortmans PM, Kluin-Nelemans HC, Haaxma-Reiche H et al (2003) High-dose methotrexate-based chemotherapy followed by consolidating radiotherapy in non-AIDS-related primary central nervous system lymphoma: European Organization for Research and Treatment of Cancer Lymphoma Group Phase II Trial 20962. J Clin Oncol 21:4483–4488. doi:10.1200/JCO.2003.03.108
Batchelor T (2005) Neuro-oncology update: 2005. Curr Opin Neurol 18:631. doi:10.1097/01.wco.0000189873.92362.dc
Batchelor T, Loeffler JS (2006) Primary CNS lymphoma. J Clin Oncol 24:1281–1288. doi:10.1200/JCO.2005.04.8819
Harder H, Holtel H, Bromberg JE et al (2004) Cognitive status and quality of life after treatment for primary CNS lymphoma. Neurology 62:544–547
Fisher B, Seiferheld W, Schultz C et al (2005) Secondary analysis of Radiation Therapy Oncology Group study (RTOG) 9310: an intergroup phase II combined modality treatment of primary central nervous system lymphoma. J Neurooncol 74:201–205. doi:10.1007/s11060-004-6596-9
O’Brien PC, Roos DE, Pratt G et al (2006) Combined-modality therapy for primary central nervous system lymphoma: long-term data from a phase II multicenter study (Trans-Tasman Radiation Oncology Group). Int J Radiat Oncol Biol Phys 64:408–413. doi:10.1016/j.ijrobp.2005.07.958
Correa DD, DeAngelis LM, Shi W et al (2004) Cognitive functions in survivors of primary central nervous system lymphoma. Neurology 62:548–555
Fliessbach K, Helmstaedter C, Urbach H et al (2005) Neuropsychological outcome after chemotherapy for primary CNS lymphoma: a prospective study. Neurology 64:1184–1188
Neuwelt EA, Guastadisegni PE, Varallyay P et al (2005) Imaging changes and cognitive outcome in primary CNS lymphoma after enhanced chemotherapy delivery. AJNR Am J Neuroradiol 26:258–265
Author information
Authors and Affiliations
Corresponding author
Additional information
H. Pels and A. Juergens contributed equally.
Rights and permissions
About this article
Cite this article
Pels, H., Juergens, A., Glasmacher, A. et al. Early relapses in primary CNS lymphoma after response to polychemotherapy without intraventricular treatment: results of a phase II study. J Neurooncol 91, 299–305 (2009). https://doi.org/10.1007/s11060-008-9712-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-008-9712-4