Abstract
The aim of this paper was to critically evaluate recent publications on hypertension treatment and control in regions by income. Prevalence of hypertension is increasing worldwide, most prominently in low-income countries. Awareness, treatment, and control are most successful in North America while remaining a challenge in middle- and low-income countries. Easy access to medical care and aggressive use of pharmacotherapy are the key strategies which have proved to be successful in reducing the burden of hypertension on the population level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An estimated 17.5 million people died from cardiovascular disease (CVD) in 2012, representing 31 % of all global deaths. Of these deaths, an estimated 7.4 million were due to coronary heart disease and 6.7 million were due to stroke [1].
For CVD, hypertension is the most important risk factor [2]. The magnitude of the hypertension problem globally was highlighted by a study of Patricia Kearney et al. [3].
In the year 2000, the overall worldwide prevalence of hypertension was estimated at 26.4 % of the adult population. While the prevalence of hypertension was lower in developing countries because of their larger populations, the estimated total number of adults with hypertension was 333 million in economically developed countries, and 639 million in economically developing countries. It was estimated that the number of persons with hypertension will increase from 972 million to 1.56 billion in 2025.
In 2010, hypertension was the leading risk factor for death from CVD, chronic kidney disease, and diabetes in every region causing over 40 % of worldwide deaths from these diseases [4••].
Until the 1950s, there was no effective treatment of hypertension available; the dizzying progress of pharmacotherapy after the 1950s has made it possible to successfully treat almost all types and stages of hypertension.
Despite this progress, until the early years of the 21st century, in the developed, high-income countries, epidemiology of hypertension still followed the “rule of halves” defined in 1972 [5], whereby half of the hypertensive individuals were not aware of their condition, only half of those who are aware were treated, and only half of those treated actually had their blood pressure (BP) under control, representing 12.5 % of all hypertensives. A publication by Wolf-Maier comparing the prevalence, awareness, treatment, and control of hypertension in five European countries, Canada, and the USA found a substantially lower prevalence of hypertension in the USA (28 %) and Canada (27 %) compared with the European countries (Sweden, 38 %; Italy, 38 %; England, 42 %; Spain, 47 %; and Germany, 55 %; age-adjusted data for the 35–64-year olds) [6]. Similar differences between North America and Europe were found for awareness, treatment, and control of hypertension; 28.6 % of the population had hypertension controlled in the USA compared with only 5–10 % in the European countries, with Canada being somewhere in between (17.2 %). It is important to underline that the population surveys used for the analysis dated back to the late 1980s (USA 1978–1994; Canada 1986–1992) and the 1990s (Europe 1990–1999).
The aim of this paper was to critically evaluate the literature on hypertension treatment and control rates in different countries over the past 3 years. We decided to review the topic by regions defined by income (high-, middle-, and low-income countries).
Epidemiology of Hypertension in High-Income Countries
In the 2011–2014 period, the prevalence of hypertension among US adults was 29.0 %, and increased with age, being 7.3 % among those aged 18–39 years, 32.2 % in the 40–59 age group, and 64.9 % among those aged 60 and over. The prevalence of hypertension remained unchanged between 1999 and 2014.
The prevalence of controlled hypertension among known and treated hypertensives was 53.0 %; extrapolated to the totality of the hypertension population, it would represent about 12.5 %.
Adults aged 18–39 were less likely to have their hypertension controlled than those aged 60 and over [7].
In another high-income industrialized country, Canada, the population prevalence of hypertension was stable at 19.7–21.6 % between 1992 and 2009. The hypertension control levels related to all hypertension subjects resembled those in the USA and hovered between 13 and 15 % in the 1990s.
It was a survey of a random sample of the Ontario population (the largest province in Canada) conducted in the years 2006–2007 which ascertained, for the first time, a significant improvement of hypertension awareness (86.3 %), treatment (80.5 %), and control (65.9 %) [8].
Another Canadian population survey confirmed to the full extent the results of the Ontario study [9] and compared the changes of key indicators of hypertension status in 1992 with those in 2009. In those two decades, the hypertension control improved from 13.2 to 64.6 % (2009). The proportion of treated hypertensives increased in 20 years of follow-up from 34.6 to 79.0 % in 2009. The population mean systolic BP decreased significantly.
In the second Canadian survey in 2009, there was a change in the method of BP measurement. The conventional mercury sphygmomanometer was used in the first survey, while an automated electronic oscillometric device (BpTRU Medical Devices Ltd, Coquitlam, British Columbia, Canada) in the second one. The BpTRU monitor gives lower values than the standard mercury sphygmomanometer [10]. Therefore, the values for BP as measured by the BpTRU device were adjusted using a linear regression equation [8] so they could be compared with readings taken by sphygmomanometer.
In Europe, hypertension control is less impressive. In Sweden, the MONICA surveys conducted between 1986 and 2009 showed a gradual improvement of hypertension control reaching 63.9 % in individuals with a BMI <25kg/m2, but only 48.8 % in those with a BMI >25kg/m2 [11]. It is important to remember that these figures relate to previously known hypertensive individuals. If projected to the large number of those unaware of their hypertension, the unsatisfactory control of elevated BP on the population level becomes obvious.
In Germany, a study by Rückert et al. [12] found that hypertension awareness and control considerably improved in the entire German population; it nevertheless remained insufficient; hypertension control was achieved in about 50 % of patients with Type-2 diabetes and in about 60 % of individuals without Type-2 diabetes.
Most recently, Neuhauser et al. [13] reported on BP distribution and hypertension management in 7108 adult participants of the German National Health Interview and Examination Survey 1998, and in 7095 individuals examined within the German Health Interview and Examination Survey for Adults conducted between 2008 and 2011. The latter study involved 3795 persons participating already in the first survey (response rate, 64 %) and 4193 adults newly recruited (response rate, 42 %). During this observation period, awareness of hypertension increased from 69 to 82 %, treatment increased from 55 to 72 %, and control increased from 23 to 51 %.
However, men aged 18–29 years had an opposite trend with a 1.5 mmHg higher systolic BP and an increased prevalence of hypertension, which was mostly uncontrolled.
Although the German figures show a profile similar to reports from the USA and Canada, they may be overestimated as a substantial proportion of the examined individuals (3795, i.e., 53.5 %) might have been affected by the cohort effect.
A population study from Portugal [14] known as a West European country with high stroke mortality and poor control of hypertension reported an improvement in the awareness (from 45.7 to 76.6 %), treatment (from 38.9 to 74.9 %), and control (from 11.2 to 42.5 %) of hypertension over a decade (2003 vs. 2011–2012), whereas the overall prevalence of hypertension remained stable (42 %).
Reliable data from Eastern Europe on the epidemiology of hypertension are still scarce. A paper by Reklaitiene reporting on the population (aged 45–64 years) of Kaunas, capital of Lithuania, shows no significant change in the prevalence of hypertension in males (from 1983 to 2002), whereas there was a significant decrease in the prevalence of hypertension in women (from 61 to 51 %) [15]. Awareness of hypertension increased in both genders, but there was a significant increase in the proportion of treated individuals only in males. Control of hypertension during the baseline evaluation from 1983 to 1984 was extremely low (3.6 % in males, 3.5 % in females) and did not improve significantly (2001–2002: males 12.6 %; females 16.6 %).
Epidemiology of Hypertension in Middle-Income Countries
There are also data on the epidemiology of HNT from Romania and Serbia, two European countries still classified by the World Bank in 2014 as upper-middle-income countries.
Data from Romania collected 7 years apart (2005 to 2011–2012) from a representative population sample aged 18–80 years showed a decrease in the prevalence of hypertension (from 44.9 to 40.4 %), and an increase in the awareness (from 44.2 to 69.6 %), treatment (from 38.9 to 59.2 %), and control of hypertension (from 19.9 to 25.0 %) [16].
A similar prevalence of hypertension (42.7 %) was found in Serbia in a population aged over 18 years in 2012. Awareness of hypertension in the first cross-sectional study ever conducted in Serbia was only 43 %. Control of hypertension is reported only in treated individuals being 27.7 % [17].
Recent Chinese data indicate that the prevalence of hypertension increased from 23.8 % in 1991 to 31.5 % in 2009. The proportion of those aware of their condition is now 51.1 %; the proportion of those treated is high (89.7 %), but only 32.1 % is controlled, representing only 19 % of all hypertensives [18]. Health insurance increased the probability of receiving treatment in diagnosed hypertensives by 28.7 % (95 % CI 10.6–46.7 %).
Poor control of hypertension is reported from Turkey [19] and India [20•] where a tenth of the rural and a fifth of urban populations have their BP under control.
Generally, hypertension is less common in Asian countries (despite their heterogeneity) than in some Western countries, but the much larger Asian population results in a considerably larger absolute number of individuals affected. Therefore, the burden of hypertension in Asia is higher than that in Western countries [21]. Populations living in rural areas have the prevalence of hypertension 2–3 times lower than those living in urban areas of Asia. However, with urbanization and westernization of lifestyle in many developing countries, the lower prevalence of hypertension in rural areas will be gradually replaced by a higher prevalence of hypertension. Hypertension and stroke occur at a relatively younger age in Asia.
The WHO study on Global Aging and Adult Health (SAGE) assessed data of nationally representative cohorts from six countries experiencing rapid economic development (China, Ghana, India, Mexico, Russia, and South Africa). Hypertension prevalence ranged from 23 % (India) to 52 % (Russia). The highest proportion of individuals with undiagnosed hypertension was found in Ghana (83 %) and South Africa (81 %), and the lowest in Russia (30 %). Overall, 73 % of hypertensives were untreated (from 35 % in Russia to 87 % in Ghana). Insurance status and income were significantly correlated with diagnosis and treatment of hypertension. Hypertension was uncontrolled in 90 % of hypertensive individuals in the above six countries. Obesity was significantly associated with the risk of developing hypertension and was found even among the lowest income quintile (13 % obesity). Hypertension control was generally poor in adult males irrespective of the geographic location [22•].
Epidemiology of Hypertension in Low-Income Countries
However, truly alarming reports are those from Africa. A systematic review and meta-analysis of studies from sub-Saharan Africa, published between 2000 and 2013 [23•], found an estimated pooled 30 % prevalence of hypertension across ages 30–60 years. Only 27 % of respondents were aware of their hypertension before the surveys, 8 % were receiving treatment, and only about 7 % had their hypertension controlled.
Bosu [24] noted a high prevalence of hypertension among West Africa’s workforce, of which a significant proportion is undiagnosed, severe, or complicated. The crude prevalence of hypertension increased progressively from 12.9 % in studies published in the 1980s to 34.4 % in those published in 2010–2014. The proportions of hypertensives, who had been previously aware of their diagnosis, were on treatment or had their BP controlled, were 19.6–84.0 %, 0–79.2 %, and 0–12.7 %, respectively. Hypertensive subjects, including health workers, rarely checked their BP except when ill.
A systematic review and meta-analysis of hypertension prevalence in the member countries of the South Asian Association for Regional Cooperation (SAARC) found a variable prevalence of hypertension, with a number of countries with BP levels above the global average [25]. However, the studies are not consistent in their collection of data regarding hypertension and other CVD risk factors.
Discussion
Population studies do not have a uniform design, they differ in population selection (age range, mean age of the population), response rates, methods (number of BP readings and BP measurement devices). Therefore, direct comparison of results is difficult, if not impossible.
Surrogate indicators of insufficient hypertension control, e.g., stroke mortality, are useful tools for international comparisons.
The Prevención de Riesgo de Ictus (PREV-ICTUS) study, a community-based study including more than 7000 individuals from primary care centers throughout Spain (about 1200 physicians), found a significant relationship between stroke mortality and poor hypertension control and presence of EKG left ventricular hypertrophy (after controlling by age, sex, obesity, diabetes, and urban setting) [26]. In his editorial commentary to PREV-ICTUS, Cooper suggested that stroke mortality could be used to monitor progress in hypertension control [27]. The assumption that stroke mortality can serve as a proxy for average BP in a population was used in the analysis by Redón et al. of stroke mortality and trends from 1990 to 2006 in 39 European and Central Asian countries [28].
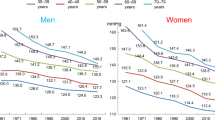
Feigin et al. provided recently data on global and regional burden of stroke during 1990–2010 [29••]. They included 58 studies from high-income and 61 from low- and middle-income countries. Mortality rates decreased significantly in both high-income (37 %; 31–41 %) and low- and middle-income countries (20 %; 15–30 %). Significant geographic differences in stroke mortality and in the burden of the disease were noted (Fig. 1), clearly showing higher mortality rates in low- and middle-income countries. Both the USA and Canada rank among countries with the lowest stroke mortality (blue) reflecting the low prevalence and extremely good control of hypertension.
How to Improve Hypertension Control
Contemplating about various aspects of hypertension during the first decade of the 21st century, the following facts are noteworthy: there is a steady increase in the awareness, treatment, and control of hypertension all over the world, most markedly in North America [30]. Prevalence of hypertension is increasing in most countries, most rapidly in low- and middle-income countries. There is also a continuing endeavor to try to control the hypertension epidemic, particularly in low-income, developing countries through population-level interventions.
Thus the High-level Meeting of the United Nations General Assembly in 2011 [31] recommended dietary salt restriction as a key community-based intervention to control hypertension ignoring the fact that the scientific evidence for the efficacy of this maneuver is somewhat shaky. Among 14 systematic reviews concerning the efficacy of this intervention, 5 were supportive and 9 were contradictory or inconclusive [32]. More importantly, the effectiveness of national strategies of salt reduction has failed in most countries where they were attempted; of the 32 countries, only 5 have demonstrated some impact [33].
One gets the impression that since there are no funds for really efficacious and effective interventions such as strengthening primary care and securing availability of antihypertensive drugs, these are replaced by exhortations addressed to populations to change nutrition and behavior,
A favorite recommendation to control hypertension is to reduce body mass index (BMI), as it is a well-documented fact that increased BMI is one of the reasons behind the increasing prevalence of hypertension. However, attempts at lowering BMI through population-wide interventions have so far failed [34].
Similar unrealistic recommendations for people living in low-income countries are to increase physical activity or avoid mental stress; this must puzzle those who are struggling just to secure sufficient food and shelter for the day.
The North American success in achieving impressive control of hypertension is due to easy access to primary care and aggressive use of antihypertensive drugs [35]. The majority of the presently used antihypertensive drugs, that is, diuretics, beta-blockers, ACE inhibitors, sartans, Ca-blockers, are all available in generic forms and the cost even in the developing world is low so that governments should be able to subsidize their provision to everyone who needs them. If there is the will…that is.
In the meantime, development of new devices and drugs continues. Transcatheter renal denervation and baroreflex activation therapy are already in clinical use for cases of resistant hypertension. Currently, 27 new drugs are in preclinical or stage I/II evaluation [36].
Having all the necessary tools to manage hypertension at their disposal, an efficient health care system providing low-cost clinical services in most countries should be a realistic goal for controlling the global problem of hypertension.
Conclusions
Hypertension is the most prevalent cardiovascular disease; its prevalence appears to be increasing in many countries not only because of aging of the population but also because of increasing obesity. Prevalence of hypertension has remained stable in the USA (1999–2014) and in Canada (1992–2009), the two countries with currently the best control of hypertension worldwide. Prevalence of hypertension in Europe is higher than that in North America, with control rates also lagging behind. Control of hypertension is poor in most middle- and low-income countries. To improve its worldwide control improved access the medical care and availability of antihypertensive drugs is needed.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
http://www.who.int/mediacentre/factsheets/fs317/en/accessed 18.04.2016.
Chobanian AV. Shattuck Lecture. The hypertension paradox—more uncontrolled disease despite improved therapy. N Engl J Med. 2009;361(9):878–87. doi:10.1056/NEJMsa0903829.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–23.
Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol. 2014;2(8):634–47. doi:10.1016/S2213-8587(14)70102-0. CVD, CKD, and diabetes mortality attributable to elevated BP and glucose serum cholesterol, and BMI were estimated.
Wilber JA, Barrow JG. Hypertension—a community problem. Am J Med. 1972;52(5):653–63.
Wolf-Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43(1):10–7.
Yoon SS, Fryar CD, Carroll MD. Hypertension prevalence and control among adults: United States, 2011–2014. U.S. National Center Health Statistics, Data Brief No. 220, 8 pp. (PHS) 2016-1209. November 2015.
Leenen FH, Dumais J, McInnis NH, Turton P, Stratychuk L, Nemeth K, Moy Lum-Kwong M, Fodor G. Results of the Ontario survey on the prevalence and control of hypertension. CMAJ 2008 20;178(11):1441–9. doi: 10.1503/cmaj.071340.
McAlister FA, Wilkins K, Joffres M, Leenen FH, Fodor G, Gee M, et al. Changes in the rates of awareness, treatment and control of hypertension in Canada over the past two decades. CMAJ. 2011;183(9):1007–13. doi:10.1503/cmaj.101767.
Myers MG, McInnis NH, Fodor GJ, Leenen FH. Comparison between an automated and manual sphygmomanometer in a population survey. Am J Hypertens. 2008;21(3):280–3. doi:10.1038/ajh.2007.54.
Törmä E, Carlberg B, Eriksson M, Jansson JH, Eliasson M. Long term trends in control of hypertension in the Northern Sweden MONICA study 1986-2009. BMC Public Health. 2015;15:957. doi:10.1186/s12889-015-2280-6.
Rückert IM, Baumert J, Schunk M, Holle R, Schipf S, Völzke H, et al. Blood pressure control has improved in people with and without type 2 diabetes but remains suboptimal: a longitudinal study based on the German DIAB-CORE consortium. PLoS One. 2015;10(7):e0133493. doi:10.1371/journal.pone.0133493. eCollection 2015.
Neuhauser HK, Adler C, Rosario AS, Diederichs C, Ellert U. Hypertension prevalence, awareness, treatment and control in Germany 1998 and 2008–11. J Hum Hypertens. 2015;29(4):247–53. doi:10.1038/jhh.2014.82.
Polonia J, Martins L, Pinto F, Nazare J. Prevalence, awareness, treatment and control of hypertension and salt intake in Portugal: changes over a decade. PHYSA study J Hypertens. 2014;32(6):1211–21. doi:10.1097/HJH.0000000000000162.
Reklaitiene R, Tamosiunas A, Virviciute D, Baceviciene M, Luksiene D. Trends in prevalence, awareness, treatment, and control of hypertension, and the risk of mortality among middle-aged Lithuanian urban population in 1983–2009. BMC Cardiovasc Disord. 2012;12:68. doi:10.1186/1471-2261-12-68.
Dorobanţu M, Darabont R, Ghiorghe S, Arsenescu-Georgescu C, Macarie C, Mitu F, et al. Hypertension prevalence and control in Romania at a seven-year interval. Comparison of SEPHAR I and II surveys. J Hypertens. 2014;32(1):39–47. doi:10.1097/01.hjh.0000434937.62412.24.
Lovic D, Stojanov V, Jakovljević B, Krotin M, Jurisic V, Djordjevic D, et al. Prevalence of arterial hypertension in Serbia: PAHIS study. J Hypertens. 2013;31(11):2151–7. doi:10.1097/HJH.0b013e328364c2a2. discussion 2157.
Liao Y, Gilmour S, Shibuya K. Health insurance coverage and hypertension control in China: results from the China Health and Nutrition Survey. PLoS One. 2016;11(3):e0152091. doi:10.1371/journal.pone.0152091. eCollection 2016.
Sengul S, Akpolat T, Erdem Y, Derici U, Arici M, Sindel S, Karatan O, Turgan C, Hasanoglu E, Caglar S, Erturk S; Turkish Society of Hypertension and Renal Diseases. Changes in hypertension prevalence, awareness, treatment, and control rates in Turkey from 2003 to 2012. J Hypertens 2016 Mar 17. [Epub ahead of print]
Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, et al. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32(6):1170–7. doi:10.1097/HJH.0000000000000146. A systematic review of epidemiology of hypertension in India from 1950 to 2013.
Jin C-N, Yu C-M, Sun J-P, Fang F, Wen Y-N, Liu M, et al. The healthcare burden of hypertension in Asia. Heart Asia. 2013;5:238–43.
Basu S, Millett C. Social epidemiology of hypertension in middle-income countries: determinants of prevalence, diagnosis, treatment, and control in the WHO SAGE study. Hypertension. 2013;62(1):18–26. doi:10.1161/HYPERTENSIONAHA.113.01374. Identification of socio-demographic predictors of hypertension prevalence, diagnosis, treatment, and control in 6 middle-income countries.
Ataklte F, Erqou S, Kaptoge S, Taye B, Echouffo-Tcheugui JB, Kengne AP. Burden of undiagnosed hypertension in sub-saharan Africa: a systematic review and meta-analysis. Hypertension. 2015;65(2):291–8. doi:10.1161/HYPERTENSIONAHA.114.04394. A systematic review of hypertension studies in sub-Saharan Africa between 2000 and 2013.
Bosu WK. The prevalence, awareness, and control of hypertension among workers in West Africa: a systematic review. Glob Health Action. 2015;8:26227. doi:10.3402/gha.v8.26227. eCollection 2015.
Neupane D, McLachlan CS, Sharma R, Gyawali B, Khanal V, Mishra SR, et al. Prevalence of hypertension in member countries of South Asian Association for Regional Cooperation (SAARC): systematic review and meta-analysis. Medicine (Baltimore). 2014;93(13):e74. doi:10.1097/MD.0000000000000074.
Redón J, Cea-Calvo L, Lozano JV, Martí-Canales JC, Llisterri JL, Aznar J. González-Esteban J; on behalf of the investigators of the PREV-ICTUS Study. Differences in blood pressure control and stroke mortality across Spain. The Prevención de Riesgo de Ictus (PREV-ICTUS) Study. Hypertension. 2007;49(4):799–805.
Cooper RS. Using public health indicators to measure the success of hypertension control. Hypertension 2007;49(4):773–4. Epub 2007 Feb 19. No abstract available.
Redon J, Olsen MH, Cooper RS, Zurriaga O, Martinez-Beneito MA, Laurent S, et al. Stroke mortality and trends from 1990 to 2006 in 39 countries from Europe and Central Asia: implications for control of high blood pressure. Eur Heart J. 2011;32(11):1424–31. doi:10.1093/eurheartj/ehr045.
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, Moran AE, Sacco RL, Anderson L, Truelsen T, O'Donnell M, Venketasubramanian N, Barker-Collo S, Lawes CM, Wang W, Shinohara Y, Witt E, Ezzati M, Naghavi M, Murray C; Global Burden of Diseases, Injuries, and Risk Factors Study 2010 (GBD 2010) and the GBD Stroke Experts Group. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2014;383(9913):245–54. Review. Erratum in: Lancet 2014;383(9913):218. This study is the first to report the global burden of stroke (incidence, prevalence, mortality, DALYs lost, and mortality-to-incidence ratios).
Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52(5):818–27. doi:10.1161/HYPERTENSIONAHA.108.113357.
http://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf; accessed 22.04.2016.
O'Donnell M, Mente A, Yusuf S. Commentary: accepting what we don't know will lead to progress. Int J Epidemiol. 2016;45(1):260–2. doi:10.1093/ije/dyw014.
Webster JL, Dunford EK, Hawkes C, Neal BC. Salt reduction initiatives around the world. J Hypertens. 2011;29(6):1043–50. doi:10.1097/HJH.0b013e328345ed83.
Semlitsch T, Jeitler K, Berghold A, Horvath K, Posch N, Poggenburg S, Siebenhofer A. Long-term effects of weight-reducing diets in people with hypertension. Cochrane Database of Systematic Reviews 2016, Issue 3. Art. No.: CD008274. DOI:10.1002/14651858.CD008274.pub3.
Cutler DM, Long G, Berndt ER, Royer J, Fournier AA, Sasser A, et al. The value of antihypertensive drugs: a perspective on medical innovation. Health Aff (Millwood). 2007;26(1):97–110.
Oparil S, Schmieder RE. New approaches in the treatment of hypertension. Circ Res. 2015;116(6):1074–95. doi:10.1161/CIRCRESAHA.116.303603.
Acknowledgments
The manuscript was supported by grant No. 15-27109A provided by the Ministry of Health of the Czech Republic.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Prof. Cifkova, Prof. Fodor and Dr. Wohlfahrt declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Novel Treatments for Hypertension
Rights and permissions
About this article
Cite this article
Cifkova, R., Fodor, G. & Wohlfahrt, P. Changes in Hypertension Prevalence, Awareness, Treatment, and Control in High-, Middle-, and Low-Income Countries: An Update. Curr Hypertens Rep 18, 62 (2016). https://doi.org/10.1007/s11906-016-0669-y
Published:
DOI: https://doi.org/10.1007/s11906-016-0669-y