Abstract
Hypertension is the leading source of morbidity and death. In the 21st century, there still is a major gap between high and low to middle-income countries in awareness, management, and control; countries in the Middle East represent an example of such disparities. In this review of the literature, light is shed on the prevalence and modifiable risk factors of hypertension specific to the region, as well as regional disparities in diagnosis and management. The crude prevalence rate is estimated to be around 29.5% with wide variability between countries. Various modifiable factors affect the prevalence of hypertension in this region such as excessively high rates of smoking, obesity, a sedentary lifestyle, some gender gap, and a suboptimal healthcare system; socio-economic factors and disparities in education, literacy, and urbanization play a significant role. Patient adherence to treatment is a determining factor of blood pressure control and nonadherence adversely affect outcomes. In addition, physician adherence to international guidelines is poor. Recognizing these barriers to hypertension management, this review serves as a call for increased national and regional efforts to implement favorable healthcare policies and improve clinical outcomes.
Similar content being viewed by others
Introduction
Hypertension (HTN) is the leading source of disability and death worldwide and is on the rise contributing to the present pandemic of cardiovascular and kidney diseases [1, 2]. Its burden is, however, uneven with a widening health disparity between high and low to middle-income countries in terms of awareness, diagnosis, treatment, and control [1]. The Middle East a diverse region located mostly in West Asia, is a perfect reflection of these disparities, as the Gulf region is mostly made up of high-income nations and the rest lies on the spectrum of low to middle-income countries [3]. This region is also mired in social, religious, and political differences and has large inequalities in regards to access to care, gender, daily habits, and work opportunities [4]. In recent years, it has undergone rapid urbanization, paralleled with an increased burden of chronic diseases whereas national preventive health systems have largely lagged behind [5]. HTN could be an essential target of a reproducible public health intervention there, since it is relatively easy to diagnose, treat and control [6]. In this review of the available literature on hypertension in the Middle East, we will be shedding the light on its prevalence, modifiable societal and risk factors specific to the area, as well as current disparities in diagnosis, management, and treatment across the region. Realizing the dearth of data about hypertension in this complex region, this article will present an overview of the current state of this common disorder in the hope of recognizing current gaps in research but also drive further public health interventions aimed at a better management of the disease. The Economic and Social Commission for Western Asia (ESCWA) a United Nations Organization considers constituents of the Middle East 18 Arab countries in Western Asia: Bahrain, Egypt, Iraq, Jordan, Kuwait, Lebanon, Libya, Mauritania, Morocco, Oman, Palestine, Qatar, Saudi Arabia, the Sudan, the Syrian Arab Republic, Tunisia, the United Arab Emirates, and Yemen. This review will be limited to these countries, which also represent the majority of the states in the World Health Organization (WHO), Eastern Mediterranean Region.
Search strategy
The MEDLINE/PubMed database was searched for publications on HTN in the Middle East from 1995 to January 2021 including a search for data from countries within the region. The search was performed with the following keywords: HTN, blood pressure, cardiovascular risk factors, cardiovascular diseases, diabetes, smoking, obesity, sedentarity, gender gap, access to care, healthcare systems, level of education and urbanization, combined with Arabs, Arab World, Arab countries, Middle East, North Africa, Arabian Gulf, and specific country names. A manual search of reference lists from identified papers supplemented the electronic search. We only included studies that were conducted in a middle-eastern country within the past 20 years. There were no set criteria for selecting specific papers given the scarcity and lack of reproducibility of data across the Middle East. Emphasis was put on papers stemming from large data sets and well-designed studies when available (e.g., the PURE study), although smaller local studies were also used when deemed suitable. Finally, both the World Bank and WHO databases were extensively searched for national data and relevant statistics concerning noncommunicable diseases in all concerned countries.
Prevalence of hypertension in the Middle East
HTN has a worldwide prevalence of around 30% [1, 7]. In a systematic review by Tailakh et al. citing 11 studies encompassing a population of more than 45,300 patients from the Arab world the overall crude prevalence of hypertension was 29.5% [8]; however, it was only 21.7% in a larger population of nearly 136,000 individuals from 24 studies analyzed by Motlagh et al. [9]. The Prospective Urban Rural Epidemiology (PURE) study, a cross-sectional analysis of baseline data from four Middle Eastern countries (Iran, Palestine, KSA, and UAE) calculated that number to be 33% [6]. Another set of data from the Africa Middle East Cardiovascular Epidemiological (ACE) study, included 7 countries from the Middle East with a prevalence of hypertension ranging from 25% in Tunisia to 50% in Egypt [5], while national studies conducted in several countries estimated this number to be for Lebanon, Oman and Morocco 36.9%, 25.2% and 39.6% respectively [10,11,12,13], and 27% for all of Iran [14] Kuwait [15] and Egypt [16]. Conversely, data from the UAE and Oman showed higher rates of 37% [17] and 40%, respectively [18]. The WHO data on hypertension prevalence summarized in Table 1 also illustrates a wide difference between countries and has some discrepancies with other sources with a prevalence ranging from 15.2% in Saudi Arabia to 35.8% in Palestine. This variability in estimation of prevalence between countries is likely caused to a certain extent by many factors related to differences in study design and time frame as speculated by Tailakh et al. Firstly, the age of the populations selected might have played a role in overestimating the prevalence of hypertension when excluding individuals under the age of 40 years [8]. Secondly, some of the studies that reported lower rates of hypertension are older studies (more than 15 years ago), where higher cutoffs were used to define hypertension. Thirdly, differences in the equipment used to measure blood pressure as well as the number and timing of measurements could at least partly explain this wide variation in results. Finally, there seems to be a role for ethnic, geographic, climatic, comorbidity burden and socio-cultural differences, affecting both study design and outcomes [8]. In addition, differences between countries in ageing, literacy, comorbidity burden, diet, and genetics may generally cause this difference in its prevalence. Tables 1 and 2 illustrate some of these differences.
Hypertension and cardiovascular disease in the Middle East
Ischemic heart disease and stroke have been the leading causes of death worldwide for the last 15 years [19] and have surpassed communicable diseases and malnutrition in the Middle East. Comorbid conditions to HTN such as diabetes, obesity, and dyslipidemia substantially increase cardiovascular morbidity and mortality. These risk factors are highly prevalent in hypertensive patients in the Middle East. For example, one study in Lebanon found that obesity, diabetes, and dyslipidemia in hypertensive patients had a prevalence of 20%, 24%, and 38%, respectively [10]. In Egypt, hypertensives were found to have higher rates of dyslipidemia and impaired glycemia as compared to normotensive subjects [20]. Similarly, higher rates of diabetes, dyslipidemia, and the metabolic syndrome were found in Saudi Arabians with hypertension [21]. In addition, there was a very high rate of comorbid diabetes in Palestinian refugees in Jordanian UNRWA camps nearing 50% [22]. Moreover, there seems to be a higher burden of cardiac disease on mortality outcomes, mirrored by noticeably higher rates of cardiovascular deaths in the Middle East region (ranging between 400 and 560 deaths per 100,000 people) when compared with developed Western societies (where numbers clustered around 100–200 deaths per 100,000 people) [2, 23]. This difference could be partially explained by suboptimal access to healthcare and education as well as societal factors affecting health awareness, levels of physical activity and effective treatment in the region. These aspects are discussed in varying levels of detail elsewhere in this article. A summary of some cardiovascular risk factors by countries can also be found in Table 1.
Modifiable factors affecting the prevalence and burden of hypertension in the Middle East
Heath care systems
At the image of social and revenue disparities in the region, there is an even progress towards universal health coverage. The WHO service coverage index that measures coverage of selected essential health services on a scale of 0–100, had in 2017 a global value of 66 [24]. It ranges from 42 for Yemen to 77 for Bahrain followed by 76 for Jordan, Kuwait, and the United Arab Emirates [25]. Furthermore, weak governance in many countries could complicate access to health products by fueling inefficiencies, corruption, waste, fraud and abuse. For instance, despite a relatively high coverage index, just 49% of individuals of individuals previously diagnosed with a chronic disease had access to medicines for their condition in Jordan [26]. The concentration of healthcare providers is also highly variable and suboptimal in many locations with according to the WHO Country Health Profiles, 2.5 physicians per 10,000 inhabitants for the Sudan as compared with 77.4 for Qatar. In addition, in many countries, some of the essential medicines for the treatment of noncommunicable diseases according to the WHO are not available in the public health sector. Finally, the availability of primary healthcare facilities is inadequate across the Region regardless of country income levels [25] (see Table 3 for a summary of this section).
Smoking rates
Smoking is associated with hypertension and is a known risk factor for cardiovascular disease [27]. Even though available data does not establish a direct causal relationship between chronic smoking and blood pressure, smoking-induced arterial stiffness and wave reflection might have detrimental effects on central blood pressure, a measure that is more closely related to target organ damage than brachial blood pressure [28]. Although smoking rates have declined over recent decades in developed countries, this has not been the case in developing countries where tobacco consumption is high and continues to rise [29]. This is not different in the Middle East where smoking rates are close to 30% in Middle Eastern participants of the PURE study [6] and range from 15.3% in Morocco to as high as 53.9% in Lebanon [29]. Also across the region, it seems that a sizeable proportion of hypertensive patients consume tobacco with 41% of more than 18,000 Palestinian refugees at UNRWA clinics in Jordan being smokers [22]. In addition, hypertension is more common in Lebanese tobacco users [13] higher in Emirati men who smoked [30] and three times more likely in Palestinian smokers [27]. It is also worth mentioning the potential impact of increased waterpipe smoking or hookah in this part of the world. In 2011, its use among adults (age > 18 years) was 15% in Lebanon, 9–12% in Syria, 4–12% in Arabic gulf countries, and 30% in Jordan [31]. Hookah users are exposed to many of the same toxic compounds/by-products as cigarette users though at much higher levels [32]. Unfortunately, awareness is limited regarding potential deleterious effects [31]. In young adult hookah smokers, a single smoking session causes an acute increase in arterial stiffness comparable in magnitude to what has been previously reported for cigarettes [33]. Furthermore, waterpipe smoking for as short as 15 min was found to have significant hemodynamic effects and increase systolic blood pressure (BP) and heart rate (HR) [34]. Nonetheless, further research is warranted to establish any chronic deleterious effect and determine whether habitual hookah smoking accelerates the development of hypertension.
Obesity and sedentary lifestyle
Obesity is a well-documented cause of hypertension [35] and obesity-related hypertension has become a major health issue worldwide. This relationship is multifactorial and is thought to be mediated by complex mechanisms such as altered hemodynamics, impaired sodium homeostasis, renal dysfunction, autonomic nervous system imbalance, endocrine alterations, oxidative stress and inflammation, and vascular injury [36]. Obesity rates are high in the Middle East nearing 13% for males and 25% for females [8]. This is often associated with hypertension as noticed in the Lebanese population [13]. In addition, more than a third of hypertensive Palestinian refugees in Jordanian UNRWA camps are obese [22] and a literature review by Arnaout et al. found that close to half of hypertensive urban residents in the Middle East were obese as well [23]. In addition, there was a younger onset of hypertension in Obese Kuwaiti individuals [37]. Table 1 shows alarming high rates of obesity and sedentary lifestyle in a large number middle-eastern countries.
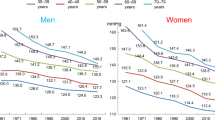
Gender gap
Although significant improvements have been made in the condition of women in fields of health and education, gender inequalities persist in the Middle East [38]. The gender gap is an important consideration in HTN even though data from the WHO (see Table 1) does not reflect it. In a systematic review by Motlagh et al., of more than 85,000 participants from 18 studies, the prevalence of HTN was greater in women than men, and was estimated at 23.0% in women and 20.1% in men [9]. In the Palestinian territories, women were also more than twice as likely to have hypertension as men [27]. Data from Iran, the Occupied Palestinian Territory, Saudi Arabia, and United Arab Emirates gathered in the PURE study, showed that the prevalence was higher in women, with an average of 33% compared to 29% in men [6]. Obesity could be a culprit as data from Tailakh et al. and the WHO (see Table 1) shows the prevalence of obesity in the Middle East to be considerably higher in women [8]. This prevalence is also elevated among young adolescent Bedouin Arab women and reaches 35% [30]. In addition, clustering of hypertension and obesity among other CVD risk factors appears to be especially common in Lebanese women [10]. Another factor could be a sedentary lifestyle. In a study by Donelly et al., women noted limited access and means to join exercise facilities as compared to men. Other socio-cultural factors such as expected gender roles for women as housekeepers, traditional dress requirements, and public modesty limited recreational and physical activity [39]. This was noted as well among Palestinian refugees in Jordan where nearly half of hypertensive women had a sedentary lifestyle and three quarters were obese [22]. Finally, rates of physical activity were lower in hypertensive women living in many Middle Eastern countries [6, 22, 23].
Education level
Large social and economic disparities exist in the Middle East leading to inequalities in access to education and gaps in literacy levels between countries. Literacy levels are also unequal among genders within one country (see Table 2). Lack of education can have direct repercussions on health. For instance, in the Palestinian territories, full-time students are 90% less likely to have hypertension, and individuals who are illiterate or have never attended school have a 3-fold risk increase to develop HTN [27]. In Yemen, hypertension is more common in patients who are illiterate, and there is an inversely proportional relationship between education level and rates of hypertension; individuals having received a high school education or higher had the lowest prevalence [40].
Urbanization
Worldwide data suggest that as people move to an urban environment, the burden of cardiovascular risk factors increases [5]. In the Middle East, its effect on HTN seems to be conflicting. Indeed, HTN seems to more common in the urban setting of some countries and conversely more prevalent in rural areas in others. For instance, in the UAE, there was a higher prevalence of hypertension in cities as compared to rural regions [30] and in Palestine, those living in a rural setting were also 23% less likely to have hypertension than their urban counterparts [27]. Conversely, prevalence was higher and awareness was lower in the rural setting in Iran, the UAE, the Occupied Palestinian Territories, and Saudi Arabia [6] as well as in Yemen where hypertension rates were considerably lower in city dwellers [40]. Alsheikh-Ali notes that although urban areas have a higher prevalence of hypertension overall in data from the PURE study, rural areas do not lag very far behind possibly because of the increasing adoption of urban lifestyles in rural communities as well as similar rates of smoking and obesity in both cities and rural areas of the region [5]. It is also possible that living in an urban setting comes with improved access to health-care facilities and increased level of education and that seems to decrease the burden of hypertension [40]. However, fast urbanization could also overwhelm current healthcare systems, and promote some of the less desirable aspects of urban life such as higher stress levels, less physical activity, and worse dietary habits.
Economic factors
Worldwide, there is a noticeable difference in the prevalence of hypertension between high-income (28.5%) [1] and low to middle-income countries (around 32%) [1, 7]. Also within countries, prevalence seems to be higher where there is economic prosperity. This is clear in Palestine where unemployed individuals are 3 times more likely to have hypertension than those who are employed [27]. In addition to a large gap in wealth distribution, mass displacement due to armed conflicts and strife in the region results in settlements of large populations of refugees with poor social and economic outlook, and adversely impacts health status [41]. For example, a Palestinian refugee has a higher risk for developing chronic diseases such as hypertension compared to a native resident of Palestine [27]. In addition, in the UAE, under-diagnosis of hypertension among non-Emiratis was much more common than among nationals possibly reflecting reduced access to healthcare for immigrants [30]. These findings are in line with other studies on displaced populations showing higher rates of hypertension and cardiovascular risk factors in Northern African Migrants to France, and higher rates of hypertension among immigrants in the Netherlands, Germany, and the United States [42].
Status of blood pressure control in the Middle East
Contemporary data from 44 low and middle-income countries suggests that on average, less than 50% of adults with hypertension receive antihypertensive medications and that around 10% only achieve control [43]. Contributory factors include lack of awareness, nonadherence to lifestyle measures and blood pressure-lowering agents, as well as social, cultural, economic, and gender-related issues that shape the individual’s access to adequate treatment [44]. In the Middle East, high rates of unawareness of the diagnosis of HTN prevail, with among patients from Iran, only 34% of middle-aged hypertensive patients being aware of their diagnosis [45]. The same applies to Palestine, Egypt, and Lebanon with a rate of awareness of around 50% [13, 23, 46]. In terms of treatment rates, just 30% of Egyptian [23, 24] and 40% of Palestinians [42] were found to be on blood pressure-lowering medications. In Lebanon, the overall percentage of treated patients was found to be 50% but increased dramatically in patients aware of their diagnosis to reach 93% [28]. However, nonadherence to antihypertensive treatment which is a poor prognostic factor [47] is another issue and affects around 45% of patients from Jordan and Lebanon [48]. In addition, data from the region show that blood pressure control in hypertensive individuals is suboptimal. Egyptian patients were reported to have low blood pressure control rates irrespective of treatment [23], and in the West Bank, only 33% of treated hypertensives had their blood pressure under control [46]. This number is slightly better in Jordan and Lebanon but remains suboptimal at 56% [48]. Data from UNRWA clinics in Jordan treating Palestinian refugees suggests substantial improvement in terms of blood pressure control when adequate follow up is implemented as 83% of hypertensive patients who attended regular clinic visits had their blood pressure under control [22]. Low blood pressure control rates in the region, could be secondary to the fact that that a very small portion only of treated hypertensive individuals is taking more than two antihypertensives (9% and 17%, respectively), with monotherapy being the most common scenario as suggested by data from Lebanon and the PURE study [6, 13]. Low rates of using two blood pressure-lowering agents or more in the region coupled with relatively low rates of blood pressure control reflect poor adherence with international guidelines that support double or triple agent therapy when monotherapy fail to control [44, 49]. Beta-blockers represent the most common class of agents prescribed in data from the PURE study coming from Iran, the Occupied Palestinian territories, Saudi Arabia, and the United Arab Emirates with around a quarter of hypertensive patients receiving them. The second most common class of medication is ACE inhibitors and ARBs [6]. In Lebanon, ACE inhibitors and ARBs are the most commonly used and are prescribed to 55% of hypertensive patients, followed by beta-blockers to 37% of patients [13]. The use of beta-blockers as the main therapeutic agent is also not aligned with most hypertension guidelines that do not recommend their use as first-line drugs due to concerns for worsening cardiovascular outcomes [44, 49]. This could be explained by the fact that hypertension is mostly treated in the region by cardiologists rather than primary care physicians which could lead to prescription bias. Regarding lifestyle factors such as high dietary salt intake, data from Iran shows that dietary salt intake reaches dangerously high levels in the general population, with nearly 98% of people consuming at least 5 g of salt a day and nearly 40% consuming at least twice the level of salt intake recommended by the WHO for adults [50]. In addition, data from Lebanon shows that nearly half of Lebanese consumers are concerned about the amount of salt in their diet however just a third of consumers are aware of the daily sodium intake limit while a similar proportion tries to buy low salt foods [51].
Potential Interventions to decrease the burden of Hypertension in the Middle East
These barriers to control shed light on the importance of a multifaceted approach to high blood pressure management with an emphasis on public health strategies aimed at increasing patient education about disease implications, adherence to lifestyle modifications, adherence to treatment and follow up. This can be achieved through nationwide measures aimed at improving health literacy [52], population-wide legislation, and voluntary agreements with food industries; mass media campaigns encouraging low dietary salt intake [7] and healthy food habits, as well as public health measures directed at encouraging physical activity. Regarding literacy, although Middle-Eastern states vary socioeconomically, they share a similar language, culture, and religion, all of which play a major role in designing and providing population-based health promotion and preventive care programs. In that regard, screening instruments such as the Eastern-Middle Eastern Adult Health Literacy test [52] could be helpful to engage the large portion of individuals with low health literacy and increase disease awareness to narrow the gap created by unequal access to education. This shared language and culture could also be used to design common screening programs and guidelines destined to general physicians. It would also be important to strengthen an underdeveloped primary care health network. This could increase access by a large part of the population to primary care evaluation. These steps would also enhance preventive screening programs and increase the affordability of comprehensive care and follow up.
Conclusion
The Middle East is a region of the world undergoing major transformations in terms of modernization; unfortunately factors such as armed conflicts and displacements are slowing down this progress. In addition, various factors specific to the region such as a high prevalence of smoking, obesity, and a sedentary lifestyle are contributing to increase the HTN burden. Moreover, wide variability exists in terms of prevalence, disease awareness, treatment rates, compliance, and blood pressure control rates. This is a reflection of the socio-economic diversity of the Middle East, as well as disparities in the medical research area, with some countries generating more solid data than others, and with wide differences in terms of research efforts pertaining to different areas or populations within a country. This calls for a multiplication of nationwide efforts across the region to improve data collection and implement better healthcare policies, in order to improve awareness and access to care, and create a more reliable health system. This would hopefully modify the course of this very common disorder and curb disability and death due to HTN and cardiovascular disease in the region.
References
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–50. https://doi.org/10.1161/CIRCULATIONAHA.115.018912. Epub 2016/08/10PubMed PMID: 27502908; PubMed Central PMCID: PMCPMC4979614
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–23. https://doi.org/10.1016/S0140-6736(05)17741-1. Epub 2005/01/18PubMed PMID: 15652604
UN. World Economic Situation and Prospects 2020. New York: UN; 2020.
Krishnan NLI, Gabriel; Narayan, Ambar; Tiwari, Sailesh; Vishwanath, Tara. 2016. Uneven Odds, Unequal Outcomes: Inequality of Opportunity in the Middle East and North Africa. Directions in Development-Poverty;. Washington, DC: World Bank. https://openknowledge.worldbank.org/handle/10986/24596
Alsheikh-Ali AA, Omar MI, Raal FJ, Rashed W, Hamoui O, Kane A, et al. Cardiovascular risk factor burden in Africa and the Middle East: the Africa Middle East Cardiovascular Epidemiological (ACE) study. PLoS One 2014;9:e102830 https://doi.org/10.1371/journal.pone.0102830. Epub 2014/08/05PubMed PMID: 25090638; PubMed Central PMCID: PMCPMC4121128
Yusufali AM, Khatib R, Islam S, Alhabib KF, Bahonar A, Swidan HM, et al. Prevalence, awareness, treatment and control of hypertension in four Middle East countries. J Hypertens. 2017;35:1457–64. https://doi.org/10.1097/HJH.0000000000001326. Epub 2017/05/10PubMed PMID: 28486270
Sarki AM, Nduka CU, Stranges S, Kandala NB, Uthman OA. Prevalence of hypertension in low- and middle-income countries: a systematic review and meta-analysis. Med (Baltim). 2015;94:e1959 https://doi.org/10.1097/MD.0000000000001959. Epub 2015/12/20PubMed PMID: 26683910; PubMed Central PMCID: PMCPMC5058882
Tailakh A, Evangelista LS, Mentes JC, Pike NA, Phillips LR, Morisky DE. Hypertension prevalence, awareness, and control in Arab countries: a systematic review. Nurs Health Sci. 2014;16:126–30. https://doi.org/10.1111/nhs.12060. Epub 2013/10/15PubMed PMID: 24118852; PubMed Central PMCID: PMCPMC4445843
Motlagh B, O’Donnell M, Yusuf S. Prevalence of cardiovascular risk factors in the Middle East: a systematic review. Eur J Cardiovasc Prev Rehabil. 2009;16:268–80. https://doi.org/10.1097/HJR.0b013e328322ca1b. Epub 2009/04/29PubMed PMID: 19398913
Tohme RA, Jurjus AR, Estephan A. The prevalence of hypertension and its association with other cardiovascular disease risk factors in a representative sample of the Lebanese population. J Hum Hypertens. 2005;19:861–8. https://doi.org/10.1038/sj.jhh.1001909. Epub 2005/07/22PubMed PMID: 16034449
Al Riyami AA, Afifi MM. Hypertension in Oman: distribution and correlates. J Egypt Public Health Assoc. 2002;77:383–407. Epub 2007/01/16. PubMed PMID: 17216969
Tazi MA, Abir-Khalil S, Chaouki N, Cherqaoui S, Lahmouz F, Srairi JE, et al. Prevalence of the main cardiovascular risk factors in Morocco: results of a National Survey, 2000. J Hypertens. 2003;21:897–903. https://doi.org/10.1097/00004872-200305000-00013. Epub 2003/04/26PubMed PMID: 12714863
Matar D, Frangieh AH, Abouassi S, Bteich F, Saleh A, Salame E, et al. Prevalence, awareness, treatment, and control of hypertension in Lebanon. J Clin Hypertens (Greenwich). 2015;17:381–8. https://doi.org/10.1111/jch.12485. Epub 2015/01/27PubMed PMID: 25619545
Esteghamati A, Meysamie A, Khalilzadeh O, Rashidi A, Haghazali M, Asgari F, et al. Third national Surveillance of Risk Factors of Non-Communicable Diseases (SuRFNCD-2007) in Iran: methods and results on prevalence of diabetes, hypertension, obesity, central obesity, and dyslipidemia. BMC Public Health. 2009;9:167 https://doi.org/10.1186/1471-2458-9-167. Epub 2009/06/02PubMed PMID: 19480675; PubMed Central PMCID: PMCPMC2697989
El-Reshaid K, Al-Owaish R, Diab A. Hypertension in kuwait: the past, present and future. Saudi J Kidney Dis Transpl. 1999;10:357–64. Epub 2008/01/24PubMed PMID: 18212446
Ashour Z, Ibrahim MM, Appel LJ, Ibrahim AS, Whelton PK. The Egyptian National Hypertension Project (NHP). Design and rationale. The NHP Investigative Team. Hypertension. 1995;26:880–5. https://doi.org/10.1161/01.hyp.26.6.880. Epub 1995/12/01PubMed PMID: 7490143
El-Shahat YI, Bakir SZ, Farjou N, Hashim T, Bohaliga A, Al-Hossani H, et al. Hypertension in UAE Citizens - Preliminary Results of a Prospective Study. Saudi J Kidney Dis Transpl. 1999;10:376–81. Epub 2008/01/24PubMed PMID: 18212449
Al-Noumani H, Wu JR, Barksdale D, Alkhasawneh E, Knafl G, Sherwood G. Relationship between medication adherence and health beliefs among patients with hypertension in Oman: pilot study. Sultan Qaboos Univ Med J. 2017;17:e329–e33. https://doi.org/10.18295/squmj.2017.17.03.012. Epub 2017/10/25PubMed PMID: 29062557; PubMed Central PMCID: PMCPMC5642364
Mathers C, Stevens G, Hogan D, Mahanani WR, Ho J. Global and regional causes of death: patterns and trends, 2000-15. In: Jamison DT, Gelband H, Horton S, Jha P, Laxminarayan R, et al., editors. Disease control priorities: improving health and reducing poverty. 3rd edition. Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2017.
Ibrahim MM. Epidemiology of hypertension in egypt. Saudi J Kidney Dis Transpl. 1999;10:352–6. Epub 2008/01/24. PubMed PMID: 18212445
Al-Nozha M, Al-Khadra A, Arafah MR, Al-Maatouq MA, Khalil MZ, Khan NB, et al. Metabolic syndrome in Saudi Arabia. Saudi Med J. 2005;26:1918–25.
Khader A, Farajallah L, Shahin Y, Hababeh M, Abu-Zayed I, Zachariah R, et al. Hypertension and treatment outcomes in Palestine refugees in United Nations Relief and Works Agency primary health care clinics in Jordan. Trop Med Int Health. 2014;19:1276–83. https://doi.org/10.1111/tmi.12356. Epub 2014/07/22PubMed PMID: 25039838
Arnaout MS, Almahmeed W, Ibrahim M, Ker J, Khalil MT, Van Wyk CT, et al. Hypertension and its management in countries in Africa and the Middle East, with special reference to the place of beta-blockade. Curr Med Res Opin. 2011;27:1223–36. https://doi.org/10.1185/03007995.2011.576239. Epub 2011/04/21PubMed PMID: 21504302
World health statistics 2020: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2020.
Health and well-being profile of the Eastern Mediterranean Region: an overview of the health situation in the Region and its countries in 2019. Cairo: WHO Regional Office for the Eastern Mediterranean; 2020.
Vialle-Valentin CE, Serumaga B, Wagner AK, Ross-Degnan D. Evidence on access to medicines for chronic diseases from household surveys in five low- and middle-income countries. Health Policy Plan. 2015;30:1044–52. https://doi.org/10.1093/heapol/czu107. Epub 2014/09/27PubMed PMID: 25255920; PubMed Central PMCID: PMCPMC4654757
Abukhdeir HF, Caplan LS, Reese L, Alema-Mensah E. Factors affecting the prevalence of chronic diseases in Palestinian people: an analysis of data from the Palestinian Central Bureau of Statistics. East Mediterr Health J. 2013;19:307–13. Epub 2013/07/26. PubMed PMID: 23882954; PubMed Central PMCID: PMCPMC4143143
Virdis A, Giannarelli C, Neves MF, Taddei S, Ghiadoni L. Cigarette smoking and hypertension. Curr Pharm Des. 2010;16:2518–25. https://doi.org/10.2174/138161210792062920. Epub 2010/06/17PubMed PMID: 20550499
Khattab A, Javaid A, Iraqi G, Alzaabi A, Ben Kheder A, Koniski ML, et al. Smoking habits in the Middle East and North Africa: results of the BREATHE study. Respir Med. 2012;106:S16–24. https://doi.org/10.1016/S0954-6111(12)70011-2. Suppl 2Epub 2013/02/08PubMed PMID: 23290700
Abdulle AM, Nagelkerke NJ, Abouchacra S, Pathan JY, Adem A, Obineche EN. Under- treatment and under diagnosis of hypertension: a serious problem in the United Arab Emirates. BMC Cardiovasc Disord. 2006;6:24 https://doi.org/10.1186/1471-2261-6-24. Epub 2006/06/07PubMed PMID: 16753071; PubMed Central PMCID: PMCPMC1501045
Qasim H, Alarabi AB, Alzoubi KH, Karim ZA, Alshbool FZ, Khasawneh FT. The effects of hookah/waterpipe smoking on general health and the cardiovascular system. Environ Health Prev Med. 2019;24:58 https://doi.org/10.1186/s12199-019-0811-y. Epub 2019/09/16PubMed PMID: 31521105; PubMed Central PMCID: PMCPMC6745078
Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. Am J Prev Med. 2009;37:518–23. https://doi.org/10.1016/j.amepre.2009.07.014. Epub 2009/12/01PubMed PMID: 19944918; PubMed Central PMCID: PMCPMC2805076
Rezk-Hanna M, Doering L, Robbins W, Sarna L, Elashoff RM, Victor RG. Acute effect of hookah smoking on arterial stiffness and wave reflections in adults aged 18 to 34 years of age. Am J Cardiol. 2018;122:905–9. https://doi.org/10.1016/j.amjcard.2018.05.033. Epub 2018/07/31PubMed PMID: 30057235
Azar RR, Frangieh AH, Mroue J, Bassila L, Kasty M, Hage G, et al. Acute effects of waterpipe smoking on blood pressure and heart rate: a real-life trial. Inhal Toxicol. 2016;28:339–42. https://doi.org/10.3109/08958378.2016.1171934. Epub 2016/04/26PubMed PMID: 27109645
Garrison RJ, Kannel WB, Stokes J 3rd, Castelli WP. Incidence and precursors of hypertension in young adults: the Framingham Offspring Study. Prev Med. 1987;16:235–51. https://doi.org/10.1016/0091-7435(87)90087-9. Epub 1987/03/01PubMed PMID: 3588564
Susic D, Varagic J. Obesity: a perspective from hypertension. Med Clin North Am. 2017;101:139–57. https://doi.org/10.1016/j.mcna.2016.08.008. Epub 2016/11/26PubMed PMID: 27884225
Channanath AM, Farran B, Behbehani K, Thanaraj TA. Association between body mass index and onset of hypertension in men and women with and without diabetes: a cross-sectional study using national health data from the State of Kuwait in the Arabian Peninsula. BMJ Open. 2015;5:e007043 https://doi.org/10.1136/bmjopen-2014-007043. Epub 2015/06/06PubMed PMID: 26044759; PubMed Central PMCID: PMCPMC4466600
Dalacoura K. Women and Gender in the Middle East and North Africa: Mapping the Field and Addressing Policy Dilemmas at the Post-2011 Juncture.MENARA Final Reports, 3. 2019. http://www.menaraproject.eu/wp-content/uploads/2019/03/menara_fr_3-1.pdf.
Donnelly TT, Al-Thani ABM, Benjamin K, Al-Khater AH, Fung TS, Ahmedna M, et al. Arab female and male perceptions of factors facilitating and inhibiting their physical activity: Findings from a qualitative study in the Middle East. PLoS One. 2018;13:e0199336 https://doi.org/10.1371/journal.pone.0199336. Epub 2018/07/17PubMed PMID: 30011280; PubMed Central PMCID: PMCPMC6047779
Modesti PA, Bamoshmoosh M, Rapi S, Massetti L, Al-Hidabi D, Al, et al. Epidemiology of hypertension in Yemen: effects of urbanization and geographical area. Hypertens Res. 2013;36:711–7. https://doi.org/10.1038/hr.2013.14. Epub 2013/03/15PubMed PMID: 23486167; PubMed Central PMCID: PMCPMC3734526
Mowafi H. Conflict, displacement and health in the Middle East. Glob Public Health. 2011;6:472–87. https://doi.org/10.1080/17441692.2011.570358. Epub 2011/05/19PubMed PMID: 21590557
Rosenthal T. Immigration and acculturation: impact on health and well-being of immigrants. Curr Hypertens Rep. 2018;20:70 https://doi.org/10.1007/s11906-018-0872-0. Epub 2018/07/05PubMed PMID: 29971699
Geldsetzer P, Manne-Goehler J, Marcus ME, Ebert C, Zhumadilov Z, Wesseh CS, et al. The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1.1 million adults. Lancet. 2019;394:652–62. https://doi.org/10.1016/S0140-6736(19)30955-9. Epub 2019/07/23PubMed PMID: 31327566
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75:1334–57. https://doi.org/10.1161/HYPERTENSIONAHA.120.15026. Epub 2020/05/07PubMed PMID: 32370572
Lotfaliany M, Akbarpour S, Mozafary A, Boloukat RR, Azizi F, Hadaegh F. Hypertension phenotypes and incident cardiovascular disease and mortality events in a decade follow-up of a Middle East cohort. J Hypertens. 2015;33:1153–61. https://doi.org/10.1097/HJH.0000000000000540. Epub 2015/02/24PubMed PMID: 25699976
Khdour MR, Hallak HO, Shaeen M, Jarab AS, Al-Shahed QN. Prevalence, awareness, treatment and control of hypertension in the Palestinian population. J Hum Hypertens. 2013;27:623–8. https://doi.org/10.1038/jhh.2013.26. Epub 2013/04/12PubMed PMID: 23575447
Gupta P, Patel P, Strauch B, Lai FY, Akbarov A, Maresova V, et al. Risk factors for nonadherence to antihypertensive treatment. Hypertension. 2017;69:1113–20. https://doi.org/10.1161/HYPERTENSIONAHA.116.08729. Epub 2017/05/04PubMed PMID: 28461599
Alhaddad IA, Hamoui O, Hammoudeh A, Mallat S. Blood pressure control in treated hypertensive Middle Eastern patients: a post hoc analysis based on JNC8 definitions. Vasc Health Risk Manag. 2019;15:35–46. https://doi.org/10.2147/VHRM.S188981. Epub 2019/03/19PubMed PMID: 30881006; PubMed Central PMCID: PMCPMC6410753
Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–324. https://doi.org/10.1161/HYP.0000000000000066. Epub 2017/11/15PubMed PMID: 29133354
zaei S, Mahmoudi Z, Sheidaei A, Aryan Z, Mahmoudi N, Gohari K, et al. Salt intake among Iranian population: the first national report on salt intake in Iran. J Hypertens. 2018;36:2380–9. https://doi.org/10.1097/HJH.0000000000001836. Epub 2018/07/14PubMed PMID: 30005027
Nasreddine L, Akl C, Al-Shaar L, Almedawar MM, Isma’eel H. Consumer knowledge, attitudes and salt-related behavior in the Middle-East: the case of Lebanon. Nutrients. 2014;6:5079–102. https://doi.org/10.3390/nu6115079. Epub 2014/11/18PubMed PMID: 25401502; PubMed Central PMCID: PMCPMC4245581
Nair SC, Satish KP, Sreedharan J, Ibrahim H. Assessing health literacy in the eastern and middle-eastern cultures. BMC Public Health. 2016;16:831 https://doi.org/10.1186/s12889-016-3488-9. Epub 2016/08/20PubMed PMID: 27538529; PubMed Central PMCID: PMCPMC4991078
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abboud, M., Karam, S. Hypertension in the Middle East: current state, human factors, and barriers to control. J Hum Hypertens 36, 428–436 (2022). https://doi.org/10.1038/s41371-021-00554-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00554-z
- Springer Nature Limited
This article is cited by
-
Evaluation of the prevalence of cardiometabolic disorders (diabetes, hypertension, and hyperlipidemia) diagnosed, undiagnosed, treated, and treatment goal in the elderly: Bushehr Elderly Health Program (BEH)
BMC Endocrine Disorders (2024)
-
Burden of diseases due to high systolic blood pressure in the Middle East and North Africa region from 1990 to 2019
Scientific Reports (2024)
-
The Pandemic of Coronary Heart Disease in the Middle East and North Africa: What Clinicians Need to Know
Current Atherosclerosis Reports (2023)
-
Roadmap for the Management of Type 2 Diabetes and Hypertension in the Middle East: Review of the 2022 EVIDENT Summit
Advances in Therapy (2023)
-
Spotlight on hypertension in the Middle-East
Journal of Human Hypertension (2022)