Abstract
Purpose of Review
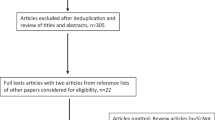
The number of bariatric surgeries for patients with type 1 or type 2 diabetes continues to grow. Clinicians are challenged to choose therapies that reach glycemic targets without inducing adverse effects in post-bariatric patients without published guidelines. This review evaluates data supporting the best strategies for diabetes management in patients undergoing bariatric surgery.
Recent Findings
Though few clinical trials have evaluated the safety and effectiveness of different glucose-lowering therapies following bariatric surgery, remission of diabetes or reduced medications is an established benefit of bariatric surgery. Adverse events including diabetic ketoacidosis in post-bariatric patients on sodium-glucose co-transporter 2 (SGLT2) inhibitors or inadequate insulin have been reported in patient's with both type 1 and type 2 diabetes. Metformin, glucagon-like peptide-1 (GLP-1) agonists, dipeptidyl peptidase-4 (DPP-4) inhibitors, SGLT2 inhibitors, insulin, and sulfonylureas have been used successfully in the perioperative period for other surgeries and guidelines recommend adjusting the doses of these medications especially in the perioperative period.
Summary
Clinicians should favor weight-neutral or weight-loss promoting therapies in post-bariatric surgery patients such as medical nutrition therapy, metformin, GLP-1 agonists, SGLT2 inhibitors, and DPP-4 inhibitors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the prevalence of obesity rises among patients with type 1 and type 2 diabetes, bariatric surgery is becoming increasingly more common. Individuals with type 2 diabetes (T2D) who undergo bariatric surgery have consistently shown superior health outcomes compared with those treated with medical management, as demonstrated by numerous randomized control trials (RCTs) [1, 2]. Fewer data are available for bariatric surgery in patients with type 1 diabetes (T1D). Several retrospective and observational studies and meta-analyses of such studies demonstrate consistent reduction in body weight, but inconsistent improvement of glycemic control [3,4,5,6,7,8]. From presurgical dietary changes to physiologic alterations occurring after surgery, clinicians should be aware of the challenges and potential pitfalls in diabetes management to achieve safe glucose targets and avoid adverse effects. Though few clinical trials have been performed evaluating management strategies and no guidelines exist, this review will discuss the strategies for managing diabetes perioperatively and postoperatively for bariatric surgery using available data.
Remission of Type 2 Diabetes
There is abundant evidence for the efficacy of bariatric surgery among patients with overweight/obesity and T2D including improvements in insulin sensitivity, reductions in glucose lowering medications, and complete remission [1], the mechanisms of which are discussed elsewhere [9]. Bariatric surgery has also been associated with lower mortality rates among people with obesity [10, 11]. Furthermore, observational data from the Swedish Obesity Study demonstrated that bariatric surgery reduces long-term mortality and is an effective tool for diabetes prevention [12]. Clinical trials have demonstrated significant improvements in blood pressure and cholesterol as well as reduced macrovascular [13,14,15,16] and microvascular complications in patients with T2D, compared to those treated with medical management [17, 18]. A recent large retrospective observational study involving 13,722 patients with type 2 diabetes showed that patients who received bariatric surgery had a significantly lower risk of incident major adverse cardiovascular events [19].
Diabetes remission has been defined as a primary outcome in all 12 RCTs reviewed by the latest diabetes surgery summit [1]. However, the definition of remission varied between trials, including hemoglobin A1C (HbA1c) < 6% without the use of medications for ≥ 1 but up to 5 years, fasting plasma glucose < 100 mg/dL (5.6 mmol/L) for ≥ 1 year, and a composite endpoint of HbA1c < 7%, LDL < 100 mg/dL, and systolic blood pressure < 130 mmHg. As there is no consensus on defining diabetes remission, this term implies restoration of normal glucose metabolism after bariatric surgery without medication. However, none of the cutoffs used to define diabetes remission have included parameters occurring below the threshold of impaired fasting glucose or impaired glucose tolerance which are known risk factors for cardiovascular disease (CVD) [20]. This does not, however, diminish the conclusion that bariatric surgery provides substantial metabolic benefits, and in appropriate patients, surpasses medical intervention, regardless of race or gender [21].
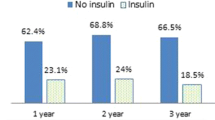
Diabetes remission rates varied among the RCTs investigating the effect of bariatric surgery versus medical management, which may be explained by study design, type of procedure, patient population, and study duration. The average percentage of patients meeting study-specific criteria for diabetes remission at the end of the study period was 68% after biliopancreatic diversion [22], 29–90% after Roux-en-Y gastric bypass (RYGB) [22,23,24,25,26,27,28,29], 23–65% after sleeve gastrectomy (SG) [27, 28], and 33–73% after laparoscopic adjustable band (LAGB) [23, 27, 30,31,32] compared with an average remission rate of 8% in the medical management cohort among all studies [22,23,24,25,26,27,28,29,30,31,32]. Although remission rates decreased over time, surgical intervention was superior to medical management for as long as 5 years post operatively in all but one study using laparoscopic adjustable gastric banding [30].
Individuals with diabetes have a greater risk of developing both microvascular and macrovascular complications, compared with those without. The risk of developing micro- and macrovascular complications increases with prolonged exposure to hyperglycemia, uncontrolled hypertension, and hyperlipidemia. Several trials have shown that intensive glucose control through medical management reduces the progression of microvascular but not macrovascular complications in patients with T2D [33,34,35]. Conversely, a significant risk of death was observed in the intensive glucose lowering arm in the ACCORD trial, ending it early after 3.5 years [36]. While the glucose lowering effect after metabolic surgery was comparable with that achieved in trials using intensive medical therapy, cardiovascular outcomes were superior and mortality rates were lower in patients with diabetes who received bariatric surgery [11, 13, 16, 37].
Glycemic Targets and Glycemic Monitoring
There is insufficient evidence to support specific glycemic targets prior to bariatric surgery. However, a review of the available evidence suggests that lower preoperative HbA1c predicts improved weight loss [38, 39] and fewer complications. Glycemic targets set by various bariatric surgery programs are often center specific, and extrapolated from non-bariatric surgery data. Higher preoperative HbA1c correlates with poor surgical outcomes, particularly after cardiac surgeries [40]. Preoperative HbA1c > 8% in non-cardiac surgery has been linked with prolonged hospitalization [41]; each percentage point increase over 6.5% was associated with a greater risk of major complications and ICU admissions [42••]. Elevated HbA1c is postulated to increase surgical complications due to long-term hyperglycemia and its impact on vasculature and wound healing. However, one retrospective study did not find an association between pre operative HbA1c and 30-day post operative mortality [43]. Despite the paucity of data in bariatric surgery patients, best practice guidelines endorse the following targets for glucose control in the pre operative period [44]:
-
i.
HbA1c ≤ 8%
-
ii.
Fasting blood glucose ≤ 110 mg/dL
-
iii.
two hour post prandial blood glucose ≤ 140 mg/dL
Glucose monitoring recommendations do not differ pre- or postoperatively except during the perioperative and immediate postoperative period, during which diet and insulin sensitivity will change considerably requiring more frequent assessment. Patients off insulin or only on basal insulin can monitor fasting glucose alone. Those with T1D or T2D requiring prandial insulin should monitor fasting, pre prandial and bedtime glucose levels, and more frequently during illness, stress, or with symptoms of hypo- or hyperglycemia. Some continuous glucose monitors (CGM) have been approved to be used instead of glucometers in insulin dosing. Accuracy of CGM has been evaluated in patients who have had bariatric surgery demonstrating the areas of concern during times of hypoglycemia and following meals. Changes in sensor glucose levels can lag behind venous and capillary glucose significantly during rapid glucose excursions associated with meals [45] and another study demonstrated that sensor glucose overestimated glucose levels by an average of 18 mg/dL when in the hypoglycemic range [46].
Nutrition Goals and Recommendations
A critical component of diabetes management is medical nutrition therapy, and these dietary recommendations evolve in relation to the pre- and postoperative time period for bariatric surgery. Patients entering bariatric surgery programs in the USA undergo rigorous nutrition education as well as medical and behavioral assessments preoperatively. However, the duration of preoperative management varies widely due to regional differences in wait times, often dictated by insurance-mandated preoperative weight loss requirements. Increased wait times in patients with complex medical histories had similar outcomes to patients with shorter wait times according to one study in Medicaid patients [47]. Although benefits of preoperative weight loss remain controversial, several studies demonstrated that following a low calorie diet for 2–6 weeks prior to the surgery date is associated with superior short- and long-term outcomes [48]. A systematic review of 15 studies including 942 participants using preoperative meal replacements for the intent of weight loss revealed that the most consistent impact of weight loss was on improvements in glucose control [49]. There is no consensus among experts regarding the best macronutrient composition, calories consumed, or duration of weight loss efforts preoperatively. However, most institutions recommend a “low-calorie” diet.
Postoperatively, patients undergo reintroduction of food in stages: liquid, pureed, and soft, followed by regular solids. The duration of each stage varies by type of surgery, institutional protocol, and individual response to the prior dietary stage. Achieving a regular solid diet can take up to three months postoperatively [50]. Patients are counseled to avoid sugary drinks and high glycemic index carbohydrates which can cause dumping syndrome; to drink water in-between instead of during meals; and to take vitamin and mineral supplements including iron, vitamin D, calcium, and vitamin B12; this is often managed with an experienced nutritionist [51]. Because calories and carbohydrates consumed differ significantly during the perioperative period, patients and physicians must be vigilant in assessing the glycemic response to pharmacotherapy and modify the medical regimen in order to safely achieve appropriate glycemic targets.
Medication Adjustments
Diabetes medication adjustments are necessary to achieve target glucose levels in the setting of the reduced calorie intake and altered insulin sensitivity. Most bariatric surgery programs recommend medically supervised weight loss with the intent of achieving a 5–10% reduction in body weight, reduction in liver size, improving metabolic markers including glucose profile, blood pressure, and lipids, and reducing postoperative complications [52, 53]. During this period as well as the period after surgery, patients taking medications to lower glucose may be at risk of hypoglycemia; therefore, we recommend the following adjustments (Table 1):
Insulin
A significant number of patients with T2D and all patients with T1D require insulin, either as basal insulin only, basal and bolus (prandial), mixed insulin, or continuous subcutaneous infusion of insulin via insulin pumps [58]. For insulin-requiring patients, a dose reduction should be implemented corresponding to dietary changes, subsequent weight loss, and improved insulin sensitivity [59]. When initiating preoperative reduced calorie intake, we recommend a 20% initial insulin dose reduction, and frequent adjustments at regular intervals should be made thereafter to avoid hypoglycemia.
Patients should be educated on self-titration of basal insulins to achieve fasting blood glucose of 80–110 mg/dL. The dose of basal insulin should be increased by two units every three days, or decreased by two to four units if hypoglycemia occurs. Basal insulin in patients with T2D with fasting blood glucose levels < 80 mg/dL may be discontinued if the dose drops to < 0.1–0.2 units/kg. Patients with T1D should never discontinue basal insulin.
Rapid-acting insulin analogues administered prior to food intake or in response to hyperglycemia are typically favored over regular human insulin due to pharmacokinetic properties and lower hypoglycemia rates [60]. A reduced calorie and carbohydrate intake leading to weight loss should improve insulin sensitivity; therefore, mealtime and corrective dosages would need to be reduced to avoid hypoglycemia. For patients on fixed doses of prandial insulin, we recommend a 20% or greater reduction in their dose with frequent adjustments based on blood glucose levels measured two hours after caloric intake.
For patients who are proficient with calculating prandial and corrective doses based on insulin-to-carbohydrate ratios and insulin sensitivity ratios, we recommend a similar adjustment (reduction of insulin to carbohydrate ratio and insulin sensitivity factors by 20%). For patients on prandial insulin, it is imperative to monitor blood glucose levels two hours after eating in order to titrate their prandial dose for a target of 120–140 mg/dL and to avoid hypoglycemia. Patients should be advised to increase the prandial dose by one to two units if remaining above target, or reduce by two units if experiencing hypoglycemia. In patients with T2D who consistently have blood glucose < 140 mg/dL two hours after eating, or if prandial insulin dose has dropped to < 10 units per meal to avoid hypoglycemia, consider discontinuing prandial insulin. Patients with T1D should not discontinue prandial insulin. Pre-mixed insulins are another option for patients who require both prandial and basal insulin coverage. They are best suited for patients who are unable to implement a complex regimen with two different insulins; however, it should be noted that these insulins lack ability to adjust long and short acting insulins independent of each other and may lead to more weight gain than other insulin formulations [61]. However, this formulation may be appropriate for some patients who struggle with the complexity of basal-bolus regimens but have prandial requirements that cannot be met with basal insulin alone [62]. The dose of mixed insulin should be reduced by at least 20%, as with other insulin formulations, and patients should attempt to adjust dose to the same fasting and post-prandial blood glucose targets.
Clinicians should be vigilant in the postoperative period for the risk of diabetic ketoacidosis (DKA), including euglycemic ketoacidosis in their patients on insulin, especially patients with T1D. One retrospective cohort analysis in two hospitals determined that 21% of patients with T1D developed DKA within the first month after surgery [63], supported by similar findings in a larger retrospective study of 107 patients [3]. Patients with T2D on insulin preoperatively have also developed DKA, especially if insulin is omitted [64,65,66]. Risk factors for development of DKA include poor oral intake, dehydration, post operative infection, and insulin omission including both accidental and iatrogenic. Screening for post operative DKA is important because symptoms of DKA including abdominal pain, nausea, and emesis can mirror those of postoperative complications such as gastric stenosis, intestinal obstruction, leak, or infection and can lead to unnecessary imaging studies [64].
Metformin
Metformin is a first-line pharmacotherapy for new onset T2D [58] and is beneficial in the prevention of progression of pre-diabetes to T2D [67]. It has multiple mechanisms of action including decreasing hepatic gluconeogenesis, increasing gut glucose utilization, increasing glucagon-like peptide-1 (GLP-1) [68], altering the gut microbiome [69] and enhancing insulin sensitivity via effects on fat metabolism [70]. GLP-1 increases following bariatric surgery [71] and is associated with postoperative weight loss [9]. Addition of metformin following bariatric surgery can improve glycemic control and contribute to sustained weight loss [72].
Metformin is contraindicated in severe chronic kidney disease (CKD) stage 4 (eGFR < 30 mL/min/1.73 m2) due to the risk of metformin accumulation and high anion gap lactic acidosis type B, a potentially fatal complication [73]. Starting metformin in patients with eGFR between 30 and 45 mL/min/1.73 m2 is not recommended. It is also recommended to temporarily discontinue metformin before an iodinated contrast imaging procedure in patients with an eGFR < 60 mL/min/1.73 m2, excessive acute or chronic alcohol use, hepatic insufficiency, or heart failure. However, the actual risk of lactic acidosis in patients who underwent bariatric surgery is unclear as limited and conflicting data exists regarding the actual levels of lactic acid in the perioperative period. Increased ketone levels and risk of lactic acidosis was reported [74], while other studies demonstrated no differences in patients taking metformin compared with patients not on metformin [75].
Despite widespread use of metformin, few studies have assessed its safety and efficacy perioperatively for bariatric surgery. Surgical guidelines recommend discontinuing metformin the day of surgery due to risks of metformin-associated lactic acidosis [76, 77]. These recommendations should be extrapolated to use in bariatric patients; metformin can be discontinued on the day of surgery. Administering metformin in the perioperative period requires careful dosing since metformin absorption has been shown to increase by up to 50% in patients who had bariatric surgery [78]. Metformin does not cause hypoglycemia and can be continued during the low-caloric diet phase prior to surgery.
One of the main reasons for non-adherence to metformin is gastrointestinal distress which can occur in up to 53% of patients [79]. Gastrointestinal discomfort is also common in patients who have undergone bariatric surgery; therefore, metformin should not be initiated during the immediate recovery period from surgery.
AACE/TOS/ASMBS guidelines for perioperative bariatric care recommend continuing metformin until resolution of diabetes is fully documented [44], although the recommendation is based on Grade D (low quality) evidence. Most surgeons tend to hold metformin for three days following a major surgery as the drug is not suitable to be used among those experiencing postoperative complications such as sepsis and acute renal failure, and those needing iodine-based diagnostic imaging. Therefore, it may be prudent to wait until tolerating a solid diet before resuming or initiating metformin in a patient with persistent T2D after surgery.
GLP-1 Agonists
GLP-1 agonists are a newer class of medications used to treat diabetes and obesity. GLP-1 agonists work through multiple signaling targets, leading to decreased glucagon concentrations, slowed gastric emptying, increased satiety, and decreased free fatty acid concentrations; all which contribute to improved insulin sensitivity, decreased HbA1c and decreased body weight [80, 81]. Liraglutide has been demonstrated to improve glycemic control along with weight loss in patients with T2D, and also to promote significant weight loss in overweight and obese patients without T2D [82]. The American Diabetic Association recommends GLP-1 agonists as one of the first medications after initiation of metformin for the treatment of T2D [58].
Since GLP-1 agonists can promote weight loss through multiple signaling mechanisms, they may be considered for post-bariatric surgery patients. Several studies have previously demonstrated a significant increase in GLP-1 concentrations in post-bariatric patients with post-prandial levels rising significantly after bariatric surgery, a physiologic state similar to GLP-1 agonist administration [83]. In non-bariatric patients, GLP-1 agonists have also been used perioperatively and compared with insulin with positive outcomes including more stable glucose levels requiring less sliding-scale corrective insulin in the perioperative period [84•].
Up to 50% of individuals taking GLP-1 agonists develop nausea, vomiting, and diarrhea, with the majority experiencing transient symptoms which resolve over time [55]. As these symptoms may overlap with symptoms of immediate postoperative complications, it would be prudent to hold GLP-1 agonists until the patient has progressed to tolerate a solid food, stage 5 diet. At the market introduction of these medications, there was concern regarding potential pancreatitis with several cases of acute pancreatitis reported via MedWatch system. However, overtime, these concerns have not been validated with sufficient evidence to confirm an increased risk [85].
Based on data from studies of perioperative glycemic control among patients undergoing non-bariatric surgery [84•], GLP-1 agonists are presumed to be suitable for use in patients with persistent or recurrent T2D after bariatric surgery, especially given their ability to promote weight loss. However, there is limited direct evidence to recommend their use. Further studies are needed to determine the safety of GLP-1 agonists in the postoperative period. Studies evaluating postoperative GLP-1 use in sleeve gastrectomy patients are underway to evaluate for potentially increased weight loss [86, 87].
DPP-4 Inhibitors
Dipeptidyl peptidase-4 (DPP-4) inhibitors block the enzyme that normally degrades GLP-1 by prolonging the half-life of circulating GLP-1 and thereby enhancing endogenous GLP-1 effect on glucose-stimulated insulin secretion, delayed gastric emptying, and inhibited post-prandial glucagon secretion [88]. The different DPP-4 inhibitors including alogliptin, linagliptin, saxagliptin, and sitagliptin lower HbA1c up to 0.7% in clinical trials [89, 90]. DPP-4 inhibitors are generally well tolerated, do not cause hypoglycemia and are weight neutral. They should be avoided in patients with a history of pancreatitis due to possible risk of exacerbation. FDA has issued warnings for increased risk of hospitalization for heart failure (HF) in patients with a history of HF, specifically for alogliptin and saxagliptin, so they should also be avoided in such patients. Dose adjustment is required in CKD for eGFR < 45 except for linagliptin which is cleared through the enterohepatic system. The benefit-risk profile of DPP-4 inhibitors has led clinicians to regard these as second-line therapeutic agents for T2D.
Preoperatively, sitagliptin has been demonstrated to be safe in inpatient general medicine and surgical patients in combination with basal insulin [91]. With regard to use of this class of drugs postoperatively, one RCT of 4 weeks duration which evaluated efficacy of sitagliptin in patients with T2D after RYGB surgery reported glucose-lowering benefit without significant adverse events [92].
Due to their relatively benign side effect profile, DPP-4 inhibitors are suitable agents for post-bariatric patients with mild hyperglycemia; however, they would not be appropriate as monotherapy for significant hyperglycemia or to induce weight loss given only modest improvement in A1c of 0.7% and no impact on weight.
SGLT2 Inhibitors
Sodium-glucose co-transporter 2 (SGLT2) inhibitors including canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin, are being increasingly used to treat T2D, obesity, CVD, HF, and CKD. Recent clinical trials have demonstrated benefits of SGLT2 inhibitors in reducing major adverse cardiovascular events, preserving renal function in CKD and reducing hospitalizations in patients with T2D and HF [54]. SGLT2 inhibitors have recently become first-line therapy for patients with T2D and an HbA1c above goal with a history of HF, CKD or a compelling need to promote weight loss [58, 93]. SGLT2 inhibitors increase urinary glucose excretion independent of insulin, leading to reduced blood glucose and blood pressure as well as modest weight loss. Other benefits of SGLT2 inhibitors include oral administration, once-daily dosing, and low hypoglycemia risk. Because SGLT inhibitors are not associated with weight gain or hypoglycemia, they may be suitable agents for post-bariatric surgery patients with persistent or new T2D [94].
Adverse effects of SGLT2 inhibitors include acute kidney injury, increased risk of distal extremity amputations, fractures, genitourinary tract infections, hypotension, DKA in addition to high cost that should be considered and which may limit their use in the peri- and postoperative periods. FDA has issued warnings regarding the risks of DKA, and serious urinary tract infections with rare cases of necrotizing fasciitis of the perineum, called Fournier’s gangrene with use of SGLT2 inhibitors [95, 96]. Among bariatric surgery patients, there are several case reports of postoperative DKA while taking an SGLT2 inhibitor [65, 97,98,99]. SGLT2 inhibitors may also increase the risk of DKA or euglycemic ketoacidosis in patients with T1D and ketosis-prone T2D [100,101,102]. In patients requiring insulin or with prior DKA, SGLT2 inhibitors should be used with caution, if at all, during the preoperative and early postoperative period. The American College of Endocrinology (ACE) and American Association of Clinical Endocrinologists (AACE) recommend holding SGLT2 inhibitors for > 24 h prior to elective surgery and until the patient has progressed to a solid diet; this strategy is reasonable to apply to patients undergoing bariatric surgery as well [103].
Though uncommon in adults with T2D before bariatric surgery, there is an increased risk of dehydration and orthostatic hypotension when SGLT2 inhibitors are used in combination with loop or thiazide diuretics, especially in patients over the age of 75 years [104]. Dehydration is the most-common cause for emergency room visits and hospital re-admissions following bariatric surgery [105, 106]. In addition to hypotension, cases of acute kidney injury were reported after dapagliflozin or canagliflozin use prompting the FDA to issue a series of safety warnings [107]. However, further analysis has determined that although SGLT2 inhibitors may cause an initial rise in serum creatinine levels, continued use does not lead to permanent kidney disease [108, 109]. An RCT in patients with T2D and kidney disease revealed reduced rates of kidney failure or CV events with canagliflozin compared with placebo [108].
There has been conflicting data on fracture risk after use of SGLT2 inhibitors, specifically canagliflozin, along with an association of reduced 1,25-dihydroxyvitamin D3, increased serum phosphate and reduced bone mineral density [110, 111]. One large population-based new-user cohort study of over 150,000 patients found no difference in fracture incidence of the humerus, forearm, pelvis, or hip in patients who had started canagliflozin compared with those who started a GLP-1 agonist; however, the follow-up period was only 200–264 days [112]. Because post-bariatric surgery patients often have deficiencies of vitamin D, calcium, and other micronutrients, careful monitoring of bone density and fracture risk is advised when using SGLT2 inhibitors in these patients.
Alpha-Glucosidase Inhibitors
Alpha-glucosidase (AG) inhibitors, including acarbose and miglitol, are another class of medications which delay the absorption of glucose and stabilize post-prandial peak glucose. They may be used in diabetes management for patients with mild hyperglycemia and residual beta cell function. They reduce post-prandial insulin levels, are weight-neutral, do not cause hypoglycemia, and are taken at the start of meals [113]. AG inhibitor-associated gastrointestinal adverse effects including flatulence, diarrhea, and abdominal discomfort lead to low compliance with use of these drugs [114]. Since gastrointestinal disturbances are common after bariatric surgery [115], use of AG inhibitors may further exacerbate these problems.
Sulfonylureas
Sulfonylureas (SUs), which block potassium-ATP channels in beta cells of the pancreatic islets eventually leading to increased plasma levels of insulin independent blood glucose levels, remain commonly prescribed medications for the management of T2D [116]. They are only utilized in patients with preserved beta-cell function.
The major concern with SUs is hypoglycemia, especially with long-acting formulations. SUs are also associated with weight gain, which limits use of these drugs in patients who plan to or have undergone bariatric surgery. No studies have been performed on using SU in patients who have had bariatric surgery. Due to the availability of several other medications for T2D that do not induce weight gain or increase the risk of hypoglycemia, SUs are not preferred for management of T2D in the perioperative or postoperative period.
Conclusion
Bariatric surgery is an increasingly utilized therapy for obesity, including in patients with either T2D or T1D. Management of patients with pre-existing diabetes or a new diagnosis of diabetes following bariatric surgery requires careful attention to the potential adverse effects and strengths of available pharmacotherapy. Therapies should be targeted to reduce hyperglycemia with the least adverse effects including avoidance of weight gain. Clinicians should pay careful attention during the early post operative period when the risk of dehydration, ketoacidosis, and hypoglycemia are the greatest.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Rubino F, Nathan DM, Eckel RH, Schauer PR, Alberti KGMM, Zimmet PZ, et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Diabetes Care. 2016;39(6):861–77. https://doi.org/10.2337/dc16-0236.
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219–34. https://doi.org/10.1111/joim.12012.
Kirwan JP, Aminian A, Kashyap SR, Burguera B, Brethauer SA, Schauer PR. Bariatric surgery in obese patients with type 1 diabetes. Diabetes Care. 2016;39(6):941–8. https://doi.org/10.2337/dc15-2732.
Ashrafian H, Harling L, Toma T, Athanasiou C, Nikiteas N, Efthimiou E, et al. Type 1 diabetes mellitus and bariatric surgery: a systematic review and meta-analysis. Obes Surg. 2015;26(8):1697–704. https://doi.org/10.1007/s11695-015-1999-6.
Landau Z, Kowen-Sandbank G, Jakubowicz D, Raziel A, Sakran N, Zaslavsky-Paltiel I, et al. Bariatric surgery in patients with type 1 diabetes: special considerations are warranted. Ther Adv Endocrinol Metab. 2019;10:2042018818822207. https://doi.org/10.1177/2042018818822207.
Chow A, Switzer NJ, Dang J, Shi X, de Gara C, Birch DW, et al. A systematic review and meta-analysis of outcomes for type 1 diabetes after bariatric surgery. J Obes. 2016;2016:1–7. https://doi.org/10.1155/2016/6170719.
Mahawar KK, De Alwis N, Carr WRJ, Jennings N, Schroeder N, Small PK. Bariatric surgery in type 1 diabetes mellitus: a systematic review. Obes Surg. 2015;26(1):196–204. https://doi.org/10.1007/s11695-015-1924-z.
Hussain A. The effect of metabolic surgery on type 1 diabetes: meta-analysis. Arch Endocrinol Metab. 2018;62(2):172–8. https://doi.org/10.20945/2359-3997000000021.
Mulla CM, Middelbeek RJW, Patti M-E. Mechanisms of weight loss and improved metabolism following bariatric surgery. Ann N Y Acad Sci. 2018;1411(1):53–64. https://doi.org/10.1111/nyas.13409.
Arterburn DE, Olsen MK, Smith VA, Livingston EH, Van Scoyoc L, Yancy WS, et al. Association between bariatric surgery and long-term survival. Jama. 2015;313(1):62–70. https://doi.org/10.1001/jama.2014.16968.
Cardoso L, Rodrigues D, Gomes L, Carrilho F. Short- and long-term mortality after bariatric surgery: a systematic review and meta-analysis. Diabetes Obes Metab. 2017;19(9):1223–32. https://doi.org/10.1111/dom.12922.
Carlsson LMS, Peltonen M, Ahlin S, Anveden Å, Bouchard C, Carlsson B, et al. Bariatric surgery and prevention of type 2 diabetes in Swedish Obese Subjects. N Engl J Med. 2012;367(8):695–704. https://doi.org/10.1056/NEJMoa1112082.
Fisher DP, Johnson E, Haneuse S, Arterburn D, Coleman KJ, O’Connor PJ, et al. Association between bariatric surgery and macrovascular disease outcomes in patients with type 2 diabetes and severe obesity. Jama. 2018;320(15):1570–82. https://doi.org/10.1001/jama.2018.14619.
Heneghan HM, Meron-Eldar S, Brethauer SA, Schauer PR, Young JB. Effect of bariatric surgery on cardiovascular risk profile. Drs. Heneghan and Meron-Eldar contributed equally to this article. Am J Cardiol. 2011;108(10):1499–507. https://doi.org/10.1016/j.amjcard.2011.06.076.
Schauer PR, Mingrone G, Ikramuddin S, Wolfe B. Clinical outcomes of metabolic surgery: efficacy of glycemic control, weight loss, and remission of diabetes. Diabetes Care. 2016;39(6):902–11. https://doi.org/10.2337/dc16-0382.
Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H, et al. Bariatric surgery and long-term cardiovascular events. Jama. 2012;307(1):56–65. https://doi.org/10.1001/jama.2011.1914.
Adams TD, Arterburn DE, Nathan DM, Eckel RH. Clinical outcomes of metabolic surgery: microvascular and macrovascular complications. Diabetes Care. 2016;39(6):912–23. https://doi.org/10.2337/dc16-0157.
O'Brien R, Johnson E, Haneuse S, Coleman KJ, O'Connor PJ, Fisher DP, et al. Microvascular outcomes in patients with diabetes after bariatric surgery versus usual care. Ann Intern Med. 2018;169(5):300–10. https://doi.org/10.7326/m17-2383.
Aminian A, Zajichek A, Arterburn DE, Wolski KE, Brethauer SA, Schauer PR, et al. Association of metabolic surgery with major adverse cardiovascular outcomes in patients with type 2 diabetes and obesity. Jama. 2019. https://doi.org/10.1001/jama.2019.14231.
Merino J, Leong A, Posner DC, Porneala B, Masana L, Dupuis J, et al. Genetically driven hyperglycemia increases risk of coronary artery disease separately from type 2 diabetes. Diabetes Care. 2017;40(5):687–93. https://doi.org/10.2337/dc16-2625.
Lee PC, Tham KW, Ganguly S, Tan HC, Eng AKH, Dixon JB. Ethnicity does not influence glycemic outcomes or diabetes remission after sleeve gastrectomy or gastric bypass in a multiethnic Asian cohort. Obes Surg. 2017;28(6):1511–8. https://doi.org/10.1007/s11695-017-3050-6.
Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Nanni G, et al. Bariatric–metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386(9997):964–73. https://doi.org/10.1016/s0140-6736(15)00075-6.
Courcoulas AP, Goodpaster BH, Eagleton JK, Belle SH, Kalarchian MA, Lang W, et al. Surgical vs medical treatments for type 2 diabetes mellitus. JAMA Surgery. 2014;149(7):707–15. https://doi.org/10.1001/jamasurg.2014.467.
Cummings DE, Arterburn DE, Westbrook EO, Kuzma JN, Stewart SD, Chan CP, et al. Gastric bypass surgery vs intensive lifestyle and medical intervention for type 2 diabetes: the CROSSROADS randomised controlled trial. Diabetologia. 2016;59(5):945–53. https://doi.org/10.1007/s00125-016-3903-x.
Ikramuddin S, Billington CJ, Lee W-J, Bantle JP, Thomas AJ, Connett JE, et al. Roux-en-Y gastric bypass for diabetes (the diabetes surgery study): 2-year outcomes of a 5-year, randomised, controlled trial. Lancet Diabetes Endocrinol. 2015;3(6):413–22. https://doi.org/10.1016/s2213-8587(15)00089-3.
Liang Z, Wu Q, Chen B, Yu P, Zhao H, Ouyang X. Effect of laparoscopic Roux-en-Y gastric bypass surgery on type 2 diabetes mellitus with hypertension: a randomized controlled trial. Diabetes Res Clin Pract. 2013;101(1):50–6. https://doi.org/10.1016/j.diabres.2013.04.005.
Parikh M, Chung M, Sheth S, McMacken M, Zahra T, Saunders JK, et al. Randomized pilot trial of bariatric surgery versus intensive medical weight management on diabetes remission in type 2 diabetic patients who do NOT meet NIH criteria for surgery and the role of soluble RAGE as a novel biomarker of success. Ann Surg. 2014;260(4):617–24. https://doi.org/10.1097/sla.0000000000000919.
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, Brethauer SA, et al. Bariatric surgery versus intensive medical therapy for diabetes — 5-year outcomes. N Engl J Med. 2017;376(7):641–51. https://doi.org/10.1056/NEJMoa1600869.
Simonson DC, Halperin F, Foster K, Vernon A, Goldfine AB. Clinical and patient-centered outcomes in obese patients with type 2 diabetes 3 years after randomization to Roux-en-Y gastric bypass surgery versus intensive lifestyle management: the SLIMM-T2D study. Diabetes Care. 2018;41(4):670–9. https://doi.org/10.2337/dc17-0487.
Ding S-A, Simonson DC, Wewalka M, Halperin F, Foster K, Goebel-Fabbri A, et al. Adjustable gastric band surgery or medical management in patients with type 2 diabetes: a randomized clinical trial. J Clin Endocrinol Metab. 2015;100(7):2546–56. https://doi.org/10.1210/jc.2015-1443.
Dixon JB, O’Brien PE, Playfair J, Chapman L, Schachter LM, Skinner S, et al. Adjustable gastric banding and conventional therapy for type 2 diabetes. Jama. 2008;299(3). https://doi.org/10.1001/jama.299.3.316.
Wentworth JM, Playfair J, Laurie C, Ritchie ME, Brown WA, Burton P, et al. Multidisciplinary diabetes care with and without bariatric surgery in overweight people: a randomised controlled trial. Lancet Diabetes Endocrinol. 2014;2(7):545–52. https://doi.org/10.1016/s2213-8587(14)70066-x.
Reaven PD, Emanuele NV, Wiitala WL, Bahn GD, Reda DJ, McCarren M, et al. Intensive glucose control in patients with type 2 diabetes — 15-year follow-up. N Engl J Med. 2019;380(23):2215–24. https://doi.org/10.1056/NEJMoa1806802.
Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360(2):129–39. https://doi.org/10.1056/NEJMoa0808431.
Group AC, Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–72. https://doi.org/10.1056/NEJMoa0802987.
Action to Control Cardiovascular Risk in Diabetes Study G, Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–59. https://doi.org/10.1056/NEJMoa0802743.
Eliasson B, Liakopoulos V, Franzén S, Näslund I, Svensson A-M, Ottosson J, et al. Cardiovascular disease and mortality in patients with type 2 diabetes after bariatric surgery in Sweden: a nationwide, matched, observational cohort study. The Lancet Diabetes & Endocrinology. 2015;3(11):847–54. https://doi.org/10.1016/s2213-8587(15)00334-4.
Ortega CB, Lee H-J, Portenier D, Guerron AD, Tong J. Preoperative hemoglobin A1c predicts postoperative weight loss following bariatric surgery in patients with diabetes. 2018;67(Supplement 1):2045–P. https://doi.org/10.2337/db18-2045-P%JDiabetes.
Syed S, Finks J, Wood M, Carlin A, Wohaibi E, Kole K, et al. Effect of preoperative hemoglobin A1c on bariatric surgery outcomes. Surg Obes Relat Dis. 2015;11(6):S43–S4. https://doi.org/10.1016/j.soard.2015.08.479.
Carson JL, Scholz PM, Chen AY, Peterson ED, Gold J, Schneider SH. Diabetes mellitus increases short-term mortality and morbidity in patients undergoing coronary artery bypass graft surgery. J Am Coll Cardiol. 2002;40(3):418–23. https://doi.org/10.1016/s0735-1097(02)01969-1.
Underwood P, Askari R, Hurwitz S, Chamarthi B, Garg R. Response to comment on underwood et al. preoperative a1c and clinical outcomes in patients with diabetes undergoing major noncardiac surgical procedures. Diabetes Care. 2014;37:611–6. Diabetes Care. 2014;37(8):e191-e. https://doi.org/10.2337/dc14-0738.
•• Yong PH, Weinberg L, Torkamani N, Churilov L, Robbins RJ, Ma R, et al. The presence of diabetes and higher Hba1care independently associated with adverse outcomes after surgery. Diabetes Care. 2018;41(6):1172–9. https://doi.org/10.2337/dc17-2304 This prospective observational study of over 7500 patients undergoing bariatric surgery found an increased risk of major complications, ICU admission, and longer length of hospital stay with each point rise in hemoglobin A1c. This suggests that pre-operative and post-operative glucose management may lead to less post-operative complications.
van den Boom W, Schroeder RA, Manning MW, Setji TL, Fiestan G-O, Dunson DB. Effect of A1C and glucose on postoperative mortality in noncardiac and cardiac surgeries. Diabetes Care. 2018;41(4):782–8. https://doi.org/10.2337/dc17-2232.
Mechanick J, Youdim A, Jones D, Garvey W, Hurley D, McMahon M, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocr Pract. 2013;19(2):337–72. https://doi.org/10.4158/ep12437.Gl.
Laguna Sanz AJ, Mulla CM, Fowler KM, Cloutier E, Goldfine AB, Newswanger B, et al. Design and clinical evaluation of a novel low-glucose prediction algorithm with mini-dose stable glucagon delivery in post-bariatric hypoglycemia. Diabetes Technol Ther. 2018;20(2):127–39. https://doi.org/10.1089/dia.2017.0298.
Nielsen JB, Abild CB, Pedersen AM, Pedersen SB, Richelsen B. Continuous glucose monitoring after gastric bypass to evaluate the glucose variability after a low-carbohydrate diet and to determine hypoglycemia. Obes Surg. 2016;26(9):2111–8. https://doi.org/10.1007/s11695-016-2058-7.
Alvarez R, Bonham AJ, Buda CM, Carlin AM, Ghaferi AA, Varban OA. Factors associated with long wait times for bariatric surgery. Ann Surg. 2018:1. https://doi.org/10.1097/sla.0000000000002826.
Hutcheon DA, Hale AL, Ewing JA, Miller M, Couto F, Bour ES, et al. Short-term preoperative weight loss and postoperative outcomes in bariatric surgery. J Am Coll Surg. 2018;226(4):514–24. https://doi.org/10.1016/j.jamcollsurg.2017.12.032.
Ross LJ, Wallin S, Osland EJ, Memon MA. Commercial very low energy meal replacements for preoperative weight loss in obese patients: a systematic review. Obes Surg. 2016;26(6):1343–51. https://doi.org/10.1007/s11695-016-2167-3.
Isom KA, Andromalos L, Ariagno M, Hartman K, Mogensen KM, Stephanides K, et al. Nutrition and metabolic support recommendations for the bariatric patient. Nutr Clin Pract. 2014;29(6):718–39. https://doi.org/10.1177/0884533614552850.
Sherf Dagan S, Goldenshluger A, Globus I, Schweiger C, Kessler Y, Kowen Sandbank G, et al. Nutritional recommendations for adult bariatric surgery patients: clinical practice. Advances in Nutrition: An International Review Journal. 2017;8(2):382–94. https://doi.org/10.3945/an.116.014258.
Brethauer S. ASMBS position statement on preoperative supervised weight loss requirements. Surg Obes Relat Dis. 2011;7(3):257–60. https://doi.org/10.1016/j.soard.2011.03.003.
Fris RJ. Preoperative low energy diet diminishes liver size. Obes Surg. 2004;14(9):1165–70. https://doi.org/10.1381/0960892042386977.
Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019;393(10166):31–9. https://doi.org/10.1016/s0140-6736(18)32590-x.
Shyangdan DS, Royle P, Clar C, Sharma P, Waugh N, Snaith A. Glucagon-like peptide analogues for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2011;10:CD006423. https://doi.org/10.1002/14651858.CD006423.pub2.
Sherifali D, Nerenberg K, Pullenayegum E, Cheng JE, Gerstein HC. The effect of oral antidiabetic agents on A1C levels: a systematic review and meta-analysis. Diabetes Care. 2010;33(8):1859–64. https://doi.org/10.2337/dc09-1727.
Vasilakou D, Karagiannis T, Athanasiadou E, Mainou M, Liakos A, Bekiari E, et al. Sodium–glucose cotransporter 2 inhibitors for type 2 diabetes. Ann Intern Med. 2013;159(4):262–74. https://doi.org/10.7326/0003-4819-159-4-201308200-00007.
9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes—2019. Diabetes Care. 2019;42(Supplement 1):S90–S102. https://doi.org/10.2337/dc19-S009.
Demma LJ, Carlson KT, Duggan EW, Morrow JG, Umpierrez G. Effect of basal insulin dosage on blood glucose concentration in ambulatory surgery patients with type 2 diabetes. J Clin Anesth. 2017;36:184–8. https://doi.org/10.1016/j.jclinane.2016.10.003.
Hirsch IB. Insulin analogues. N Engl J Med. 2005;352(2):174–83. https://doi.org/10.1056/NEJMra040832.
Elizarova S, Galstyan GR, Wolffenbuttel BH. Role of premixed insulin analogues in the treatment of patients with type 2 diabetes mellitus: a narrative review. J Diabetes. 2014;6(2):100–10. https://doi.org/10.1111/1753-0407.12096.
Riddle MC, Rosenstock J, Gerich J. The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26(11):3080–6. https://doi.org/10.2337/diacare.26.11.3080.
Rottenstreich A, Keidar A, Yuval JB, Abu-Gazala M, Khalaileh A, Elazary R. Outcome of bariatric surgery in patients with type 1 diabetes mellitus: our experience and review of the literature. Surg Endosc. 2016;30(12):5428–33. https://doi.org/10.1007/s00464-016-4901-2.
Aminian A, Kashyap SR, Burguera B, Punchai S, Sharma G, Froylich D, et al. Incidence and clinical features of diabetic ketoacidosis after bariatric and metabolic surgery. Diabetes Care. 2016;39(4):e50–3. https://doi.org/10.2337/dc15-2647.
Andalib A, Elbahrawy A, Alshlwi S, Alkhamis A, Hu W, Demyttenaere S, et al. Diabetic ketoacidosis following bariatric surgery in patients with type 2 diabetes: table 1. Diabetes Care. 2016;39(8):e121–e2. https://doi.org/10.2337/dc16-0280.
Rizo IM, Apovian CM. Diabetic ketoacidosis post bariatric surgery. Front Endocrinol (Lausanne). 2018;9:812. https://doi.org/10.3389/fendo.2018.00812.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. https://doi.org/10.1056/NEJMoa012512.
Bahne E, Sun EWL, Young RL, Hansen M, Sonne DP, Hansen JS, et al. Metformin-induced glucagon-like peptide-1 secretion contributes to the actions of metformin in type 2 diabetes. JCI Insight. 2018;3(23). https://doi.org/10.1172/jci.insight.93936.
Wu H, Esteve E, Tremaroli V, Khan MT, Caesar R, Mannerås-Holm L, et al. Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug. Nat Med. 2017;23(7):850–8. https://doi.org/10.1038/nm.4345.
Rena G, Hardie DG, Pearson ER. The mechanisms of action of metformin. Diabetologia. 2017;60(9):1577–85. https://doi.org/10.1007/s00125-017-4342-z.
Dimitriadis GK, Randeva MS, Miras AD. Potential hormone mechanisms of bariatric surgery. Curr Obes Rep. 2017;6(3):253–65. https://doi.org/10.1007/s13679-017-0276-5.
Malin SK, Kashyap SR. Effects of metformin on weight loss. Current Opinion in Endocrinology & Diabetes and Obesity. 2014;21(5):323–9. https://doi.org/10.1097/med.0000000000000095.
Moioli A, Maresca B, Manzione A, Napoletano AM, Coclite D, Pirozzi N, et al. Metformin associated lactic acidosis (MALA): clinical profiling and management. Journal of Nephrology. 2016;29(6):783–9. https://doi.org/10.1007/s40620-016-0267-8.
Aberle J, Reining F, Dannheim V, Flitsch J, Klinge A, Mann O. Metformin after bariatric surgery – an acid problem. Exp Clin Endocrinol Diabetes. 2011;120(03):152–3. https://doi.org/10.1055/s-0031-1285911.
Deden LN, Aarts EO, Aelfers SCW, van Borren MMGJ, Janssen IMC, Berends FJ, et al. Risk of metformin-associated lactic acidosis (MALA) in patients after gastric bypass surgery. Obes Surg. 2017;28(4):1080–5. https://doi.org/10.1007/s11695-017-2974-1.
Sudhakaran S, Surani SR. Guidelines for perioperative management of the diabetic patient. Surgery Research and Practice. 2015;2015:1–8. https://doi.org/10.1155/2015/284063.
Duggan EW, Klopman MA, Berry AJ, Umpierrez G. The Emory University perioperative algorithm for the management of hyperglycemia and diabetes in non-cardiac surgery patients. Current Diabetes Reports. 2016;16(3):34. https://doi.org/10.1007/s11892-016-0720-z.
Padwal RS, Gabr RQ, Sharma AM, Langkaas LA, Birch DW, Karmali S, et al. Effect of gastric bypass surgery on the absorption and bioavailability of metformin. Diabetes Care. 2011;34(6):1295–300. https://doi.org/10.2337/dc10-2140.
Razavi N, Siavash M, Tabbakhian M, Sabzghabaee A. Severity of gastrointestinal side effects of metformin tablet compared to metformin capsule in type 2 diabetes mellitus patients. J Res Pharm Pract. 2017;6(2):73–6. https://doi.org/10.4103/jrpp.JRPP_17_2.
Hinnen D. Glucagon-like peptide 1 receptor agonists for type 2 diabetes. Diabetes Spectrum. 2017;30(3):202–10. https://doi.org/10.2337/ds16-0026.
Drucker DJ. Biologic actions and therapeutic potential of the proglucagon-derived peptides. Nat Clin Pract Endocrinol Metab. 2005;1(1):22–31. https://doi.org/10.1038/ncpendmet0017.
Pi-Sunyer X, Astrup A, Fujioka K, Greenway F, Halpern A, Krempf M, et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med. 2015;373(1):11–22. https://doi.org/10.1056/NEJMoa1411892.
Jirapinyo P, Jin DX, Qazi T, Mishra N, Thompson CC. A meta-analysis of GLP-1 after Roux-En-Y gastric bypass: impact of surgical technique and measurement strategy. Obes Surg. 2017;28(3):615–26. https://doi.org/10.1007/s11695-017-2913-1.
• Kaneko S, Ueda Y, Tahara Y. GLP1 receptor agonist liraglutide is an effective therapeutic option for perioperative glycemic control in type 2 diabetes within enhanced recovery after surgery (ERAS) protocols. Eur Surg Res. 2018;59(5–6):349–60. https://doi.org/10.1159/000494768 This study demonstrated the safety and efficacy of a GLP-1 agonist in the perioperative setting and supports utilization of this class of medications due to their weight loss and cardiovascular and renoprotactive benefits.
Egan AG, Blind E, Dunder K, de Graeff PA, Hummer BT, Bourcier T, et al. Pancreatic safety of incretin-based drugs — FDA and EMA assessment. N Engl J Med. 2014;370(9):794–7. https://doi.org/10.1056/NEJMp1314078.
ClinicalTrials.gov. Evaluation of liraglutide 3.0 mg in patients with poor weight-loss and a suboptimal glucagon-like peptide-1 response (BARIOPTIMISE). Available at: https://clinicaltrials.gov/ct2/show/NCT03341429. Accessed on: 6 September 2019.
ClinicalTrials.gov. Effect of GLP-1 receptor agonism after sleeve gastrectomy. Available at: https://clinicaltrials.gov/ct2/show/NCT03115424. Accessed on: 6 September 2019.
Thornberry NA, Gallwitz B. Mechanism of action of inhibitors of dipeptidyl-peptidase-4 (DPP-4). Best Pract Res Clin Endocrinol Metab. 2009;23(4):479–86. https://doi.org/10.1016/j.beem.2009.03.004.
Amori RE, Lau J, Pittas AG. Efficacy and safety of incretin therapy in type 2 diabetes. JAMA. 2007;298(2):194–206. https://doi.org/10.1001/jama.298.2.194.
Richter B, Bandeira-Echtler E, Bergerhoff K, Lerch C. Dipeptidyl peptidase-4 (DPP-4) inhibitors for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2008;2:CD006739. https://doi.org/10.1002/14651858.CD006739.pub2.
Umpierrez GE, Gianchandani R, Smiley D, Jacobs S, Wesorick DH, Newton C, et al. Safety and efficacy of sitagliptin therapy for the inpatient management of general medicine and surgery patients with type 2 diabetes: a pilot, randomized, controlled study. Diabetes Care. 2013;36(11):3430–5. https://doi.org/10.2337/dc13-0277.
Shah A, Levesque K, Pierini E, Rojas B, Ahlers M, Stano S, et al. Effect of sitagliptin on glucose control in type 2 diabetes mellitus after Roux-en-Y gastric bypass surgery. Diabetes Obes Metab. 2018;20(4):1018–23. https://doi.org/10.1111/dom.13139.
Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of endocrinology on the comprehensive type 2 diabetes management algorithm – 2019 executive summary. Endocr Pract. 2019;25(1):69–100. https://doi.org/10.4158/cs-2018-0535.
Kheniser K, Kashyap SR. Canagliflozin versus placebo for post-bariatric surgery patients with persistent type II diabetes: a randomized controlled trial (CARAT). Diabetes Obes Metab. 2017;19(4):609–10. https://doi.org/10.1111/dom.12860.
Food and Drug Administration. FDA drug safety communication: FDA revises labels of SGLT2 inhibitors for diabetes to include warnings about too much acid in the blood and serious urinary tract infections. 2015. Available from: https://www.fda.gov/media/94822/download.
Food and Drug Administration. FDA warns about rare occurrences of a serious infection of the genital area with SGLT2 inhibitors for diabetes. 2018. Available from: https://www.fda.gov/media/115602/download.
van Niekerk C, Wallace J, Takata M, Yu R. Euglycaemic diabetic ketoacidosis in bariatric surgery patients with type 2 diabetes taking canagliflozin. BMJ Case Reports. 2018;2018. https://doi.org/10.1136/bcr-2017-221527.
Hoenes C, Rashid Q, Pimentel J. Diabetic ketoacidosis in a postoperative gastric bypass patient. Journal of Surgical Case Reports. 2017;2017(7):rjx148. https://doi.org/10.1093/jscr/rjx148.
Elasha HEA, Wafa W, Meeran K. SGLT2 inhibition may precipitate euglycemic DKA after bariatric surgery. Clinical Diabetes and Research. 2018;2(1):40–2.
Umpierrez GE. SGLT2 inhibitors and diabetic ketoacidosis — a growing concern. Nat Rev Endocrinol. 2017;13(8):441–2. https://doi.org/10.1038/nrendo.2017.77.
Levine JA, Karam SL, Aleppo G. SGLT2-I in the hospital setting: diabetic ketoacidosis and other benefits and concerns. Current Diabetes Reports. 2017;17(7):54. https://doi.org/10.1007/s11892-017-0874-3.
Meyer EJ, Gabb G, Jesudason D. SGLT2 inhibitor–associated euglycemic diabetic ketoacidosis: a South Australian clinical case series and Australian spontaneous adverse event notifications. Diabetes Care. 2018;41(4):e47–e9. https://doi.org/10.2337/dc17-1721.
Handelsman Y, Henry RR, Bloomgarden ZT, Dagogo-Jack S, DeFronzo RA, Einhorn D, et al. American Association of Clinical Endocrinologists and American College of endocrinology position statement on the association of Sglt-2 inhibitors and diabetic ketoacidosis. Endocr Pract. 2016;22(6):753–62. https://doi.org/10.4158/ep161292.Ps.
Gomez-Peralta F, Abreu C, Lecube A, Bellido D, Soto A, Morales C, et al. Practical approach to initiating SGLT2 inhibitors in type 2 diabetes. Diabetes Therapy. 2017;8(5):953–62. https://doi.org/10.1007/s13300-017-0277-0.
Chen J, Mackenzie J, Zhai Y, O’Loughlin J, Kholer R, Morrow E, et al. Preventing returns to the emergency department following bariatric surgery. Obes Surg. 2017;27(8):1986–92. https://doi.org/10.1007/s11695-017-2624-7.
Alvarenga ES, Lo Menzo E, Szomstein S, Rosenthal RJ. Safety and efficacy of 1020 consecutive laparoscopic sleeve gastrectomies performed as a primary treatment modality for morbid obesity. A single-center experience from the metabolic and bariatric surgical accreditation quality and improvement program. Surg Endosc. 2015;30(7):2673–8. https://doi.org/10.1007/s00464-015-4548-4.
Food and Drug Administration. FDA drug safety communication: FDA strengthens kidney warnings for diabetes medicines canagliflozin (Invokana, Invokamet) and dapagliflozin (Farxiga, Xigduo XR). Available from: https://www.fda.gov/media/98683/download.
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380(24):2295–306. https://doi.org/10.1056/NEJMoa1811744.
Seidu S, Kunutsor SK, Cos X, Gillani S, Khunti K. SGLT2 inhibitors and renal outcomes in type 2 diabetes with or without renal impairment: a systematic review and meta-analysis. Primary Care Diabetes. 2018;12(3):265–83. https://doi.org/10.1016/j.pcd.2018.02.001.
Taylor SI, Blau JE, Rother KI. Possible adverse effects of SGLT2 inhibitors on bone. The Lancet Diabetes & Endocrinology. 2015;3(1):8–10. https://doi.org/10.1016/s2213-8587(14)70227-x.
Bilezikian JP, Watts NB, Usiskin K, Polidori D, Fung A, Sullivan D, et al. Evaluation of bone mineral density and bone biomarkers in patients with type 2 diabetes treated with canagliflozin. The Journal of Clinical Endocrinology & Metabolism. 2016;101(1):44–51. https://doi.org/10.1210/jc.2015-1860.
Fralick M, Kim SC, Schneeweiss S, Kim D, Redelmeier DA, Patorno E. Fracture risk after initiation of use of canagliflozin. Ann Intern Med. 2019;170(3):155–63. https://doi.org/10.7326/m18-0567.
Rosak C, Mertes. Critical evaluation of the role of acarbose in the treatment of diabetes: patient considerations. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2012;5:357–67. https://doi.org/10.2147/dmso.S28340.
Catalan VS, Couture JA, LeLorier J. Predictors of persistence of use of the novel antidiabetic agent acarbose. Arch Intern Med. 2001;161(8):1106–12.
Potoczna N, Harfmann S, Steffen R, Briggs R, Bieri N, Horber FF. Bowel habits after bariatric surgery. Obes Surg. 2008;18(10):1287–96. https://doi.org/10.1007/s11695-008-9456-4.
Sola D, Rossi L, Schianca GPC, Maffioli P, Bigliocca M, Mella R, et al. State of the art paper sulfonylureas and their use in clinical practice. Arch Med Sci. 2015;4(4):840–8. https://doi.org/10.5114/aoms.2015.53304.
Acknowledgments
We would like to thank Dr. Bethany M. Mulla, MD, for proofreading the manuscript.
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Army, Department of Defense, or the U.S. Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Obesity
Rights and permissions
About this article
Cite this article
Mulla, C.M., Baloch, H.M. & Hafida, S. Management of Diabetes in Patients Undergoing Bariatric Surgery. Curr Diab Rep 19, 112 (2019). https://doi.org/10.1007/s11892-019-1242-2
Published:
DOI: https://doi.org/10.1007/s11892-019-1242-2