Abstract
Hypoglycemia is a common problem in hospitalized patients, particularly the elderly, frail, and severely ill. Hypoglycemia has been implicated in the development of adverse clinical outcomes, including increased mortality. Fear of iatrogenic hypoglycemia remains an obstacle to adequate inpatient glycemic control. However, evidence from large clinical trials is mixed: several intensive care unit studies have shown either reduced or no change in mortality with intensive glycemic control, despite high rates of iatrogenic hypoglycemia, and only 1 large study showed higher mortality. In the general ward setting, the association of hypoglycemia with worse outcomes and mortality has been frequently reported, but after multivariate adjustment for comorbidities this association disappears. Spontaneous hypoglycemia, rather than iatrogenic hypoglycemia, is strongly associated with mortality suggesting that hypoglycemia behaves as a biomarker rather than a causative factor of adverse outcomes. Inpatient glycemic management should be patient-centered, follow the current guidelines, and aimed at preventing hypoglycemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
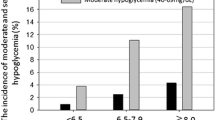
Achieving normoglycemia in hospitalized patients is crucial, as both hyperglycemia and hypoglycemia can be harmful [1••]. The goal of inpatient glycemic control is to avoid extremes of dysglycemia with a patient-centered approach that is straightforward, cost-effective, and appropriate for the individual patient (as shown in Fig. 1). Hypoglycemia and fear of hypoglycemia are major clinical concerns when treating both outpatients and hospitalized patients, resulting in inadequate treatment of hyperglycemia. Hypoglycemia is common in hospitalized patients, and its prevalence varies according to the definition used. In non-ICU patients hypoglycemia, defined as point-of-care (POC) blood glucose ≤70 mg/dL, has been reported on 3.5 % of patient-days or 4.2 % of all inpatient blood glucose measurements nationwide [2]. When hypoglycemia is defined as POC blood glucose ≤60 mg/dL, this estimate can increase to 9.5 % of inpatients receiving antihyperglycemic agents [3], and it is even more common in the sick and elderly [4••]. In general, the overall prevalence of hypoglycemia among medical and surgical patients with type 2 diabetes (T2DM) treated with insulin ranges from 3 %–29 % [5, 6, 7•]. Hypoglycemia has been associated with increased hospital length of stay, greater cost of hospitalization, and higher mortality both during hospitalization, and after discharge [8••, 9, 10]. Observational studies have demonstrated a J-shaped relationship between inpatient glycemic control and mortality, with increased risk of death at both the high and low extremes of dysglycemia [11–14]. Although the association between inpatient hypoglycemia and mortality is well-established, it is still unclear if hypoglycemia, per se, is the cause of increased mortality, or just a biomarker. Nonetheless, it is important to recognize, treat, and attempt to avoid hypoglycemia using effective inpatient protocols for glycemic management.
Conceptual depiction of elements influencing clinical decision-making in glycemic control of hospitalized patients. Those with “healthier” characteristics shown on the left should have a narrower glycemic range. For “sicker” patients shown on the right wider glycemic targets are acceptable. Hypoglycemia should be avoided in all and particularly the “sicker” patients. (Adapted with permission from: Ismail-Beigi F, Moghissi E, Tiktin M, Hirsch IB, Inzucchi SE, Genuth S. Individualizing glycemic targets in type 2 diabetes mellitus: implications of recent clinical trials. Ann Intern Med. 2011;154:554–9.) [58]
Definitions and Controversies
A brief definition of some of the major issues and controversies surrounding inpatient hypoglycemia is helpful in framing the discussion.
Hypoglycemia
A blood glucose of <70 mg/dL is often used to define hypoglycemia for safety reasons. However, “true hypoglycemia” is defined when counterregulation occurs, which varies among individuals. Epinephrine and glucagon release are triggered at blood glucose <70 mg/dL, followed by growth hormone, and cortisol at blood glucose <60 mg/dL [15]. Hypoglycemic autonomic symptoms require even lower blood glucose levels, often <50 mg/dL [15]. Severe hypoglycemia has been defined as blood glucose <50 mg/dL, or symptoms of hypoglycemia requiring assistance [16]. Therefore a safe, reasonable goal of glycemic control is to avoid blood glucose levels of <70 mg/dL in hospitalized patients [1••, 17]. Clinical manifestations of hypoglycemia can be divided into 2 major groups: autonomic counterregulation (ie, tachycardia, tremor, diaphoresis, and hunger), and neuroglycopenia (ie, dizziness, confusion, tiredness, seizures, and coma) due to insufficient fuel in the brain. It is also important to stress that lack of hypoglycemic symptoms is common among elderly and sick patients.
Hypoglycemia-Associated Autonomic Failure
Patients with recurrent hypoglycemia may develop hypoglycemia-associated autonomic failure (HAAF), in which the catecholamine-mediated autonomic effects and symptoms of hypoglycemia are blunted [18, 19]. Loss of autonomic symptoms leads to lack of recognition of hypoglycemia until neuroglycopenic symptoms are precipitated. While this phenomenon is well-characterized in patients with type 1 diabetes (T1DM), particularly those with longstanding disease, it is also common in sick and elderly hospitalized patients. Thus, physicians and nursing staff need to be aware of “silent” or asymptomatic hypoglycemia, and altered cognitive function should prompt a POC blood glucose measurement.
Hypoglycemia-Induced Mortality
Although hypoglycemia is common, hypoglycemia-induced death from cardiac or neuronal causes is rare. Investigations into the mechanisms of hypoglycemia-induced cardiac death have shown that hypoglycemia is associated with QT prolongation and reentrant arrhythmias, often quoted as the underlying cause of the “dead in bed” syndrome [20–22]. Patients with diabetes and a history of recurrent hypoglycemia, particularly those with longstanding disease and organ failure, may be more susceptible to such arrhythmias due to cardiac autonomic neuropathy (CAN), which manifests as decreased baroreflex sensitivity after antecedent hypoglycemia [23]. However, rarely has a definitive “cause-and-effect” relationship between hypoglycemia and mortality due to arrhythmias been established [24, 25]. Furthermore, patients with diabetes and CAN do not have greater QT prolongation than patients with diabetes and no history of CAN during episodes of experimental hypoglycemia. Those with CAN often do not counter-regulate with excessive catecholamine release, similar to patients with HAAF, thus decreasing the likelihood of reentrant arrhythmias via this mechanism. Hence, the fact that hypoglycemia is common but is rarely the immediate cause of death raises the possibility that HAAF may actually be cardioprotective by blunting the catecholamine-mediated response to recurrent hypoglycemia [26].
Brain death from hypoglycemia is also rare, and requires a prolonged and profound degree of hypoglycemia. Insulin-induced hypoglycemia in primates can cause brain death when glucose concentrations are maintained at levels ≤20 mg/dL for more than 5 hours [27]. The mechanism of brain death at the neuronal level in such cases is multifactorial and incompletely understood, and neuronal cell death is exacerbated by overly aggressive correction of hypoglycemia to the hyperglycemic range [28]. In rats brain cell death can occur with glucose levels of ≤35 mg/dL, but similar data at the cellular level is not available in humans [29]. Human studies are scarce, but the best evidence we have is the Diabetes Control and Complications Trial (DCCT). Careful monitoring of patients in the intensive arm showed that although they experienced severe and repeated episodes of hypoglycemia, and cognitive impairments occurred at the time of hypoglycemia, there was no evidence of central nervous system injury [30]. Similarly, in hospitalized patients with severe iatrogenic hypoglycemia, hypoglycemia not only did not result in central neurologic deficits, but was actually associated with favorable outcomes [31]. Thus brain death from hypoglycemia, while possible, is rare.
Risk Factors for Hypoglycemia
Key predictors of hypoglycemic events in hospitalized patients include older age, more severe illness (presence of septic shock, mechanical ventilation, renal failure, malignancy, and hypoalbuminemia), diabetes and longer disease duration, and treatment for hyperglycemia [10, 32]. Other risk factors include altered nutritional intake due to illness itself, as well as the placement of patients on nothing-by-mouth status for purposes of inpatient testing, without concomitant appropriate adjustment of glycemic regimen [32, 33].
Types of Hypoglycemia
It is important to distinguish between spontaneous and iatrogenic hypoglycemia. Spontaneous hypoglycemia occurs in sick hospitalized patients with organ failure, malnutrition, or those taking predisposing medications. Iatrogenic hypoglycemia originates from treatment, and occurs with overly aggressive glycemic therapy (usually insulin), but it can also include drug-to-drug interactions, and patients who develop organ failure while already taking antidiabetic agents.
Blood Glucose Measurement
Glucose values vary depending on the sampling method, and they differ when obtained from the venous, arterial, or capillary system. Venous blood is the preferred laboratory determination, but because of the widespread use of POC glucose meters, fingerstick capillary blood samples have also become standard. Glucose values from arterial blood, measured on a blood gas analyzer are more accurate than those obtained from capillary blood using a handheld glucose meter, which have up to 20 % allowable error [34•]. In critically ill patients handheld glucometer measurements can be even more inaccurate due to anemia and hypoxia, an issue of particular concern in a group of patients for whom tighter glucose control is recommended [35, 36]. Anemia can falsely elevate POC glucometer values, leading to over-treatment and hypoglycemia [37].
Feeding
Prolonged fasting or starvation alone does not cause hypoglycemia, but is a contributing factor in sick individuals who have decreased caloric intake. Nutritional intake impacts glycemic management, and insulin, an important anabolic hormone, is frequently withheld in patients with poor enteral intake due to fear of hypoglycemia. Therefore, such patients remain hyperglycemic and catabolic. Proper nutrition together with insulin should be provided to ill patients in a catabolic state. Few randomized trials of feeding strategies in hospitalized patients are available. The recent EPaNIC trial, which is discussed in more detail elsewhere in this issue, compared early (within 48 hours) vs late (starting day 8 or later) initiation of parenteral nutrition in critically ill patients. The results of the trial support late initiation of parenteral nutrition in the critically ill—despite significantly higher rates of hypoglycemia to blood glucose <40 mg/dL in the late-initiation group, recovery time was shorter and both complications and costs of hospitalization were reduced [38••].
Consequences of Inpatient Hypoglycemia
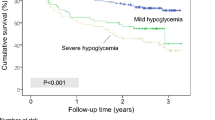
Tight glycemic management leads to higher rates of hypoglycemia. Patients with hypoglycemia can have complications related to consequent cognitive dysfunction, such as falls, and can also have neuroglycopenic manifestations such as seizures. Such complications may be part of the reason hypoglycemia can be associated with longer lengths of stay or the need for higher levels of monitoring in some cases [8••]. The most crucial issue is whether inpatient hypoglycemia leads to increased mortality. In Table 1 we summarize the major inpatient trials of glycemic management in the ICU and non-ICU settings with regard to mortality. Although the adult Leuven SICU and MICU trials and the pediatric ICU trial all showed a decrease in mortality with intensive insulin therapy, others have not. The Leuven SICU trial is the best evidence that severe and protracted hypoglycemia is associated with improved outcomes, reporting significantly decreased mortality despite high rates of hypoglycemia in intensively treated patients. The Leuven MICU trial showed an increase in mortality with intensive insulin therapy in the first 3 days of hospitalization, but overall mortality was decreased or unchanged with intensive therapy. Only 1 large multicenter trial, NICE-SUGAR, reported an overall increase in mortality with intensive insulin therapy [31, 39, 40, 41••]. Other trials such as VISEP and Glucontrol were terminated early due to unacceptably high rates of severe hypoglycemia, without increased mortality up to the point of study termination [42, 43]. Of note, there were important differences between the original Leuven studies and the NICE-SUGAR trial, including patient populations studied, blood glucose goals, methods of blood glucose measurement, feeding strategies, and achievement of glycemic targets. Only 50 % of intensively treated patients in NICE-SUGAR maintained the target of normoglycemia throughout the study, so that the difference in mean blood glucose levels between the control and intervention arms was not as wide as that achieved in the Leuven trials [14]. Thus, although profound hypoglycemia to ≤40 mg/dL was more common with intensive insulin therapy in all the ICU studies, ultimately only NICE-SUGAR reported overall higher mortality.
The DIGAMI trials have been the only studies addressing intensive glycemic control in patients with diabetes and acute myocardial infarction [44, 45]. The initial DIGAMI trial showed decreased mortality in patients with acute myocardial infarction treated intensively with insulin-glucose infusion followed by basal-bolus insulin compared with standard therapy, but only at 1 and 5 years of follow-up [44]. The DIGAMI-2 trial failed to demonstrate better long-term outcomes with more aggressive insulin regimens, although glycemic control did not differ greatly between the conventional and intensive arms [45]. Overall, the major inpatient trials from the ICU and non-ICU settings have provided a mixed set of results, with improved or unchanged mortality with tight glycemic control. Because NICE-SUGAR showed an increased mortality rate, it contributed to fear of iatrogenic hypoglycemia, and was critical in changing policy recommendations [1••]. When examined together the inpatient glycemic management trials do not clearly establish hypoglycemia as a cause of increased mortality in hospitalized patients. In fact, a recent meta-analysis of 26 ICU trials found no benefit or harm of intensive glycemic therapy, despite higher rates of hypoglycemia with intensive treatment [46]. We use these controversial results to highlight that patient-centered glycemic management, as illustrated in Fig. 1, is more appropriate than a “one-size-fits-all” approach.
The major outpatient clinical trials of diabetic glycemic management also, as expected, reported much higher rates of hypoglycemia with intensive glycemic control. It is difficult to translate these studies to the inpatient population given the differences in type of hyperglycemia treatment, length of diabetes treatment, and differences in acute illness. However, outpatient trials are often applied to hospitalized patients in the general medical ward setting. It is noteworthy that only a single study, the ACCORD trial, demonstrated increased mortality with intensive glycemic therapy in patients with T2DM [47], and the increased mortality was not due to hypoglycemia [16]. All other landmark outpatient clinical trials comparing intensive glycemic control with standard therapy showed no significant differences in macrovascular outcomes or mortality, in spite of higher rates of hypoglycemia in the intensive treatment arms [48–53]. The posited link between hypoglycemia and cardiovascular events has also been examined in the BARI 2D study of high-risk patients with well-established ischemic heart disease. No difference in mortality or major cardiovascular events was reported in the intensively treated patients despite higher rates of hypoglycemia [54]. More recently, the EURODIAB Prospective Complications Trial of patients with T1DM reported that intensively treated patients with higher rates of hypoglycemia did not have higher incidence of cardiovascular disease or increased serum markers of inflammation [55••].
Robust data in the inpatient general medical ward setting illuminates the crucial role of underlying disease burden in determining the impact of hypoglycemia on mortality. A recent large retrospective cohort study showed a significant association between inpatient hypoglycemia and mortality in the hospital and at 1 year after discharge; the odds of inpatient mortality progressively increased as severity of hypoglycemia worsened [8••]. The higher mortality at 1 year after discharge in patients with prior, non-temporally associated inpatient hypoglycemia strongly suggests that hypoglycemia was a biomarker of disease severity rather than a direct cause of death. Further studies have bolstered this hypothesis, and highlight the importance of distinguishing between spontaneous and iatrogenic hypoglycemia. This was confirmed in a study of patients with acute myocardial infarction (about half had diabetes) which found that hypoglycemia (defined as blood glucose ≤60 mg/dL) was a predictor of in-hospital mortality only in patients with spontaneous hypoglycemia and more severe medical illness. Iatrogenic hypoglycemia was not associated with a high mortality rate [56]. This was also consistent with the DIGAMI-2 trial, which showed that hypoglycemia was not an independent predictor of mortality or cardiovascular events (up to 3 years of follow-up) once corrected for severity of underlying illness [57]. Most recently, the largest retrospective cohort study analyzing the relationship between inpatient hypoglycemia (defined as blood glucose ≤70 mg/dL) and mortality among patients with and without diabetes admitted to general medical wards confirmed that spontaneous hypoglycemia, but not iatrogenic hypoglycemia, was associated with increased risk of inpatient mortality [4••]. After multivariate adjustment for patient demographics and comorbidities, hypoglycemia was no longer associated with mortality. These findings established that spontaneous hypoglycemia behaves as a biomarker of disease severity, rather than a direct cause of death.
Implications for Inpatient Glycemic Management and Transitions of Care
The evidence of the impact of hypoglycemia on hospitalized patients’ outcomes supports several management strategies. Key principles include avoiding dysglycemia in hospitalized patients, avoiding iatrogenic hypoglycemia, and practicing patient-centered care, especially in elderly and sick patients in whom glycemic goals may be more liberal (as shown in Fig. 1). Glycemic regimens should be reevaluated when blood glucose falls below 100 mg/dL, and altered when blood glucose falls below 70 mg/dL [1••]. There are few randomized clinical trials to guide glycemic management on the general medical wards, where most hospitalized patients are cared for. The RABBIT-2 trial established the superiority of basal-bolus insulin to sliding scale insulin therapy in hospitalized patients with T2DM [6], highlighting the ineffectiveness of a reactive sliding scale approach and its propensity to cause more hypoglycemia. In addition, the DEAN trial showed that insulin regimens comprised of NPH and regular insulin achieved similar glycemic control to basal-bolus regimens of detemir and aspart in hospitalized patients with type 2 diabetes, without significant differences in hypoglycemia or other outcomes. [7•]. Oral hypoglycemic agents are typically not recommended for inpatient management, and the use of non-hypoglycemic agents needs to be studied. There may be a role for inpatient use of incretin-based therapies that have low risk of hypoglycemia when used alone, such as GLP-1 agonists and particularly DPP4-inhibitors. However, clinical trials are necessary in order to establish their role in hospitalized patients. Effective and straightforward inpatient glycemic regimens, including protocols for management of hypoglycemic events and insulin dose adjustments, are of paramount importance. Finally, maintenance of normoglycemia is important when care is transitioned from the inpatient to the outpatient setting.
Conclusions
We have discussed that hypoglycemia is common, particularly in elderly and sick patients. It remains unclear whether episodic inpatient hypoglycemia is a direct mediator of adverse outcomes and mortality or merely a biomarker of disease burden and severity. Although evidence supports the latter theory, hypoglycemic events are certainly associated with the potential for harm and should be avoided. More aggressive insulin regimens appear to be beneficial in some patient populations, but should be avoided in frail, ill patients with truncated life expectancy. Hospitalized patients suffering from hypoglycemia, particularly spontaneous hypoglycemia, carry a poor prognosis. When hypoglycemia occurs, the cause needs to be elucidated and treatment regimen adjusted appropriately. Inpatient glycemic protocols should be effective, not labor-intensive, and patient-centered.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Umpierrez G, Hellman R, Korytkowski MT, et al. Management of hyperglycemia in hospitalized patients in non-critical care setting: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2012;97:16–38. These are the most recent guidelines for management of hyperglycemia in patients on the general wards.
Cook CB, Kongable GL, Potter DJ, et al. Inpatient glucose control: a glycemic survey of 126 U.S. hospitals. J Hosp Med. 2009;4:E7–E14.
Varghese P, Gleason V, Sorokin R, et al. Hypoglycemia in hospitalized patients treated with antihyperglycemic agents. J Hosp Med. 2007;2:234–40.
•• Boucai L, Southern WN, Zonszein J. Hypoglycemia-associated mortality is not drug-associated but linked to comorbidities. Am J Med. 2011;124:1028–35. This large retrospective cohort study showed that spontaneous hypoglycemia, but not iatrogenic hypoglycemia, is associated with mortality.
Umpierrez GE, Smiley D, Jacobs S, et al. Randomized study of basal bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery). Diabetes Care. 2011;34:256–61.
Umpierrez GE, Smiley D, Zisman A, et al. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT-2 trial). Diabetes Care. 2007;2181–6.
• Umpierrez GE, Hor T, Smiley D, et al. Comparison of inpatient insulin regimens with detemir plus aspart vs neutral protamine hagedorn plus regular in medical patients with type 2 diabetes. J Clin Endocrinol Metab. 2009;94:564–9. This multicenter RCT showed that inpatient basal-bolus therapy achieves equivalent glycemic control to a split-mixed mixed regimen of NPH and regular insulin, with no difference in hypoglycemic events.
•• Turchin A, Matheny ME, Shubina M, et al. Hypoglycemia and clinical outcomes in patients with diabetes hospitalized in the general ward. Diabetes Care. 2009;32:1153–7. This retrospective cohort trial showed that inpatient hypoglycemia in patients with diabetes in the general wards is associated with increased mortality.
Curkensall SM, Natoli JL, Alexander CM, et al. Economic and clinical impact of inpatient diabetic hypoglycemia. Endocr Pract. 2009;15:302–12.
Kagansky N, Levy S, Rimon E, et al. Hypoglycemia as a predictor of mortality in hospitalized elderly patients. Arch Intern Med. 2003;163:1825–9.
Pinto DS, Skolnick AH, Kirtane AJ, et al. U-shaped relationship of blood glucose with adverse outcomes among patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2005;46:178–80.
Pinto DS, Kirtane AJ, Pride YB, et al. Association of blood glucose with angiographic and clinical outcomes among patients with ST-segment elevation myocardial infarction (from the CLARITY-TIMI-28 study). Am J Cardiol. 2008;101:303–7.
Kosiborod M, Inzucchi SE, Krumholz HM, et al. Glucose normalization and outcomes in patients with acute myocardial infarction. Arch Intern Med. 2009;169:438–46.
Mesotten D, Van den Berghe G. Glycemic targets and approaches to management of the patient with critical illness. Curr Diab Rep. 2012;12:101–7.
Schwartz NS, Clutter WE, Shah SD, Cryer PE. Glycemic thresholds for activation of glucose counterregulatory systems are higher than the threshold for symptoms. JCI. 1987;79:777–81.
Bonds DE, Miller ME, Bergenstal RM, et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study. BMJ. 2010;340:b4909.
Moghissi ES, Korytkowski MT, DiNardo M, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care. 2009;32:1119–31.
Dagogo-Jack SE, Craft S, Cryer PE. Hypoglycemia-associated autonomic failure in insulin-dependent diabetes mellitus. JCI. 1993;91:819–28.
Davis MR, Mellman M, Shamoon H. Further defects in counterregulatory responses induced by recurrent hypoglycemia in IDDM. Diabetes. 1992;41:1335–40.
Nordin C. The case for hypoglycaemia as a proarrythmic event: basic and clinical evidence. Diabetologia. 2010;53:1552–61.
Tattersall RB, Gill GV. Unexplained deaths of type 1 diabetic patients. Diabet Med. 1991;8:49–58.
Robinson RTCE, Harris ND, Ireland RH, et al. Mechanisms of abnormal cardiac repolarization during insulin-induced hypoglycemia. Diabetes. 2003;52:1469–74.
Adler GK, Bonyhay I, Failing H, et al. Antecedent hypoglycemia impairs autonomic cardiovascular function: implications for rigorous glycemic control. Diabetes. 2009;58:360–6.
Desouza C, Salazar H, Cheong B, et al. Association of hypoglycemia and cardiac ischemia: a study based on continuous monitoring. Diabetes Care. 2003;26:1485–9.
Johnston SS, Connor C, Aagren M, et al. Evidence linking hypoglycemic events to an increased risk of acute cardiovascular events in patients with type 2 diabetes. Diabetes Care. 2011;34:1164–70.
Lee SP, Yeoh L, Harris ND, et al. Influence of autonomic neuropathy on QTc lengthening during hypoglycemia in type 1 diabetes. Diabetes. 2004;53:1535–42.
Kahn KJ, Myers RE. Insulin-induced hypoglaecyemia in the non-human primate. I. Clinical consequences. Clin Dev Med. 1971;39/40:185–94.
Suh SW, Gum ET, Hamby AM, et al. Hypoglycemic neuronal death is triggered by glucose reperfusion and activation of neuronal NADPH oxidase. J Clin Invest. 2007;117:910–8.
Tkacs NC, Pan Y, Raghupathi R, et al. Cortical Fluoro-Jade staining and blunted adrenomedullary response to hypoglycemia after noncoma hypoglycemia in rats. J Cereb Blood Flow Metab. 2005;25:1645–55.
The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group. Long-term effects of diabetes and its treatment on cognitive function. N Engl J Med. 2007;356:1842–52.
Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–67.
Krinsley JS, Grover A. Severe hypoglycemia in critically ill patients: risk factors and outcomes. Crit Care Med. 2007;35:2262–7.
Smith WD, Winterstein AG, Johns T, et al. Causes of hyperglycemia and hypoglycemia in adult inpatients. Am J Health Syst Pharm. 2005;62:714–9.
• Karon BS, Boyd JC, Klee GG. Glucose meter performance criteria for tight glycemic control estimated by simulation modeling. Clin Chem. 2010;56:1091–7. Handheld point-of-care glucose meters have up to 20% allowable error.
Karon BS, Griesmann L, Scott R, et al. Evaluation of the impact of hematocrit and other interference on the accuracy of hospital-based glucose meters. Diabetes Technol Ther. 2008;10:111–20.
Tang Z, Louie RF, Lee JH, et al. Oxygen effects on glucose meter measurements with glucose dehydrogenase- and oxidase-based test strips for point-of-care testing. Crit Care Med. 2001;29:1062–70.
Pidcoke HF, Wade CE, Mann EA, et al. Anemia causes hypoglycemia in intensive care unit patients due to error in single-channel glucometers: methods of reducing patient risk. Crit Care Med. 2010;38:471–6.
•• Casaer MP, Mesotten D, Hermans G, et al. Early vs late parenteral nutrition in critically ill adults. N Engl J Med. 2011;365:506–17. This multicenter RCT showed that late initiation of parenteral nutrition is associated with fewer complications and decreased cost of hospitalization compared with early initiation.
Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354:449–61.
Vlasselaers D, Milants I, Desmet L, et al. Intensive insulin therapy for patients in paediatric intensive care: a prospective, randomized controlled study. Lancet. 2009;373:547–56.
•• Finfer S, Chittock DR, Su SY, et al. Intensive vs conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283–97. This multicenter RCT showed that intensive insulin therapy was associated with increased mortality compared with standard therapy.
Brunkhorst F, Engel C, Bloos F, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–39.
Preiser JC, Devos P, Ruiz-Santana S, et al. A prospective randomized multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med. 2009;35:1738–48.
Malmberg K. Prospective randomized study of intensive insulin treatment on long term survival after acute myocardial infarction in patients with diabetes mellitus. BMJ. 1997;314:1512–5.
Malmberg K, Ryden L, Wedel H, et al. Intense metabolic control by means of insulin in patients with diabetes mellitus and acute myocardial infarction (DIGAMI 2): effects on mortality and morbidity. Eur Heart J. 2005;26:650–61.
Griesdale DEG, de Souza RJ, van Dam RM, et al. Intensive insulin therapy and mortality among critically ill patients: a meta-analysis including the NICE-SUGAR study data. CMAJ. 2009;180:821–7.
Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59.
Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with Type 2 diabetes. N Engl J Med. 2008;358:2560–72.
Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with Type 2 diabetes. N Engl J Med. 2009;360:129–39.
The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86.
The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study Research Group. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643–53.
Shichiri M, Kishikawa H, Ohkubo Y, Wake N. Long-term results of the Kumamoto study on optimal diabetes control in type 2 diabetic patients. Diabetes Care. 2000;S2:B21–9.
UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–53.
The BARI 2D Study Group. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009;360:2503–15.
•• Gruden G, Barutta F, Chaturvedi N, et al. Severe hypoglycemia and cardiovascular disease incidence in type 1 diabetes: the EURODIAB Prospective Complications Trial. Diabetes Care. 2012;35:1598–604. This multicenter prospective trial showed that severe hypoglycemia in patients with type 1 diabetes did not increase the risk of cardiovascular disease.
Kosiborod M, Inzucchi SE, Goyal A, et al. Relationship between spontaneous and iatrogenic hypoglycemia and mortality in patients hospitalized with acute myocardial infarction. JAMA. 2009;301:1556–64.
Mellbin LG, Malmberg K, Waldenstrom A, et al. Prognostic implications of hypoglycaemic episodes during hospitalization for myocardial infarction in patients with type 2 diabetes: a report from the Digami 2 Trial. Heart. 2009;95:721–7.
Ismail-Beigi F, Moghissi E, Tiktin M, Hirsch IB, Inzucchi SE, Genuth S. Individualizing glycemic targets in type 2 diabetes mellitus: implications of recent clinical trials. Ann Intern Med. 2011;154:554–9.
Disclosure
Conflicts of interest: M. Carey: none; L. Boucai: none; J. Zonszein: serves as a speaker for Takeda Pharmaceutical North America, Amylin Pharmaceuticals, Eli Lilly, Merck, Novo Nordisk, and Sanofi-Aventis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carey, M., Boucai, L. & Zonszein, J. Impact of Hypoglycemia in Hospitalized Patients. Curr Diab Rep 13, 107–113 (2013). https://doi.org/10.1007/s11892-012-0336-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11892-012-0336-x