Abstract
Hypoglycemia is common among hospitalized patients with diabetes mellitus (DM), and is associated with increased morbidity and mortality. Identify pre-admission risk factors associated with in-hospital hypoglycemia. Historical prospectively collected data of adult DM patients hospitalized to medical wards between 2011 and 2013. Hypoglycemia and serious hypoglycemia were defined as at least one blood glucose measurement ≤ 70 and < 54 mg/dl, respectively, during hospitalization. The primary outcome was in-hospital hypoglycemia. The cohort included 5301 patients (mean age 73 ± 13 years, 51% male), including 792 patients (15%) with hypoglycemia, among them 392 patients (7%) with serious hypoglycemia. Patients with hypoglycemia or serious hypoglycemia during hospitalization were older, compared to patients without hypoglycemia and more likely to have chronic renal failure and cerebrovascular disease. Malignancy and female gender were risk factors for hypoglycemia, but not for serious hypoglycemia, while congestive heart failure was associated with increased risk only for serious hypoglycemia. Diabetes mellitus’ duration over 10 years was associated with an almost threefold increased risk for hypoglycemia, compared to DM duration less than a year. Insulin treatment and glycated hemoglobin > 9% were also more common in patients with hypoglycemia. Insulin treatment was associated with a fourfold increase in the risk for hypoglycemia among all glycated hemoglobin categories. Our results identified several risk factors for in-hospital hypoglycemia in patients with DM. These findings may lead to appropriate monitoring and early intervention to prevent hypoglycemia and to reduce morbidity and mortality associated with in-hospital hypoglycemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypoglycemia is not uncommon in hospitalized patients with diabetes mellitus (DM), with an incidence ranging between less than 1% and over 32% [1,2,3,4,5,6,7,8,9]. This wide range of incidence rates in different studies probably stems from the poor definition of hypoglycemia. While in previous guidelines published by the American Diabetes Association in-hospital hypoglycemia was defined as any blood glucose level below 70 mg/dl [10], in the current guidelines from the International Hypoglycaemia Study Group, serious, clinically significant hypoglycemia (serious hypoglycemia) is now defined as glucose < 54 mg/dl, while glucose alert value is defined as ≤ 70 mg/dl, and can be important for adjustment of glucose lowering drugs [11].
Hypoglycemia is a major limiting factor in achieving optimal glycemic control in patients with DM, with solid evidence indicating that intensive insulin therapy leads to more episodes of hypoglycemia [12,13,14,15]. Many factors may contribute to development of hypoglycemia in admitted patients, including poor nutrition, renal failure, heart failure, advanced liver disease, advance age, infections, and the intensity of treatment regimen [16,17,18,19].
We have previously reported increased short- and long-term mortality in patients with spontaneous and insulin-related hypoglycemia in hospitalized patients [8]. One of the most critical components of DM management includes prevention of hypoglycemia, thus, while our previous study focused on the detrimental effects of in-hospital hypoglycemia, in the current study we aim to take a step back and identify predictors and risk factors for in-hospital hypoglycemia in patients with DM.
Methods
The study was conducted at a large 1300-bed university-affiliated tertiary medical center. The vast majority of admissions to the ten medical wards are through an emergency department. All patient data are recorded in electronic medical charts, based on the same database platform used in the community primary care facilities.
The study was approved by the hospital’s Institutional Review Board.
For the present study, historical prospectively collected observational data were extracted from the medical records of all patients with DM, admitted for any cause to the hospital’s medical wards between January 1, 2011 and December 31, 2013. Self-reported data regarding alcohol use, smoking and body mass index (BMI), as well as comorbidities were also collected from the database.
Diabetes mellitus was defined as a previous diagnosis of DM coded in the medical records or use of any oral hypoglycemic agent, glucagon-like peptide 1 (GLP-1) agonist, or insulin at time of admission. Blood glucose values were based on point-of-care bedside measurements in capillary blood as well as serum glucose levels in venous samples. We excluded patients with no glucose measurement during the hospitalization or recorded glycated hemoglobin levels in the year prior to the index admission. Hypoglycemia was defined as at least one blood glucose measurement ≤ 70 mg/dl, with serious hypoglycemia defined as values < 54 mg/dl during the hospitalization.
Our aim is to identify pre-admission risk factors for in-hospital hypoglycemia and serious hypoglycemia in patients with DM, including age, gender, BMI, comorbidities, glycemic control based on glycated hemoglobin, drug treatment and duration of DM.
Statistical analysis
The statistical analysis for this paper was generated using SAS Software, Version 9.4.
Continuous variables were presented by mean ± SD, categorical variables were presented by (N, %). Odds ratios, for testing the univariate predictive value of all study covariates, were calculated by logistic regression. Logistic regression was also used for multivariate models. Two sided p values less than 0.05 were considered statistically significant.
Results
Study cohort
After exclusion of patients without DM, repeat admissions, patients with no glucose measurements during the hospitalization or available glycated hemoglobin levels during the year prior to admission, the study cohort includes 5301 patients with DM; 2708 (51%) were male, and mean age was 73 years (range 18–103 years).
Data on DM type were available for 4984 of the 5301 patients with DM: 45 (0.9%) had type 1 and 4635 (93%) had type 2. In the remainder, type 2 DM was likely in most cases but this could not be confirmed. Due to the small number of patients with type 1 DM, we did not analyze the data specifically in this population.
DM duration data were available for 4715 patients (89%). In the entire study cohort, the mean ± SD duration of DM was 12 ± 11 years, and most patients had DM for over 10 years (2509 patients, 53%). The mean glycated hemoglobin levels in the year prior to admission were 7.6 ± 2%, including 2223 patients (42%) with glycated hemoglobin < 7%, 2220 patients (42%) with glycated hemoglobin 7–9% and 858 patients (16%) with values > 9%. A similar rate of patients were insulin-treated (2190 patients, 41%) or treated by non-insulin glucose lowering medication (2343 patients, 44%) before the admission, while only a minority (758 patients, 14%) was not treated medically for DM. Long-acting basal insulin (insulin glargine or insulin detemir) was the most common insulin treatment in our cohort (74%), including basal-only (38%) or basal-bolus (34%) regimen. Pre-mixed insulin preparations were used by 20% of the patients. Pre-hospitalization metformin monotherapy was the most common non-insulin treatment (61%), followed by the combination of metformin with another non-insulin treatment (16%). Sulfonylurea or repaglinide was used in less than 1% of patients.
A total of 792 patients (15%) had at least one blood glucose value ≤ 70 mg/dl (hypoglycemia), including 379 patients (7%) with at least one glucose value < 54 mg/dl (serious hypoglycemia).
The most common discharge diagnoses in the entire cohort were diseases of the circulatory system (1789 patients, 34%) and infectious diseases (1189 patients, 22%). Compared to patients without hypoglycemia, in patients with hypoglycemia the reported admission rate for infectious diseases was higher (26 vs. 22%), as for diseases of the genitourinary system (9 vs. 6%), and endocrine, nutritional and metabolic diseases (10 vs. 5%).
Patients with in-hospital hypoglycemia or serious hypoglycemia during the hospitalization were older (mean age 74 ± 14 and 75 ± 13, respectively) compared to patients without hypoglycemia (72 ± 12 years). While in the group of patients with hypoglycemia there was a significant gender difference with female preponderance (52 vs. 48%), this difference was not evident in the group of patients with serious hypoglycemia. Patients with hypoglycemia or serious hypoglycemia were more likely to have chronic renal failure and cerebrovascular disease compared to those without hypoglycemia. Insulin treatment was more common in patients with hypoglycemia (68 vs. 37%, p < 0.001) or serious hypoglycemia (71 vs. 39%, p < 0.001). Compared to patients without hypoglycemia, basal-only (15 vs. 8%) and basal-bolus (19 vs. 8%) insulin regimens were more common among patients with hypoglycemia. Significant findings were evident with serious hypoglycemia, compared to patients without serious hypoglycemia (15 vs. 8% and 21 vs. 9%, respectively).
There was no difference in hypoglycemia rate between patients with non-insulin treatment for DM compared to non-medically treated patients. Malignancy was significantly more common in patients with hypoglycemia compared to patients without hypoglycemia (16 vs. 13%), while congestive heart failure was more common only in the group of patients with serious hypoglycemia, compared to those without serious hypoglycemia (21 vs. 15%). The adjusted odds ratios for the association of each characteristic with hypoglycemia or serious hypoglycemia are shown in Table 1.
Corticosteroid treatment prior to the hospitalization was similar among patients with and without hypoglycemia or serious hypoglycemia. During the hospitalization, dose reduction or treatment discontinuation was recorded in 28 patients, including three patients with hypoglycemia, but not in the group of patients with serious hypoglycemia. New corticosteroid treatment was recorded in a total of 434 patients, more frequently among patients with hypoglycemia (12 vs. 7%) or serious hypoglycemia (12 vs. 8%), compared to patients without hypoglycemia.
The mean DM duration was significantly longer in the group of patients with hypoglycemia (15 ± 11 vs. 12 ± 10 years, p < 0.001) or serious hypoglycemia (15 ± 11 vs. 12 ± 11 years). In patients with shorter duration of DM the risks for hypoglycemia or serious hypoglycemia were lower (DM duration > 10 vs. < 1 year: OR 2.76, 95% CI 1.75–4.35 and OR 3.86, 95% CI 1.80–8.27, respectively).
Glycated hemoglobin and DM treatment
Analysis of the interaction between hypoglycemia, glycated hemoglobin and treatment for DM indicated a significant interaction (p < 0.05), thus we analyzed the data separately according to glycated hemoglobin levels and DM treatment. The interaction between insulin treatment, comorbidities and in-hospital hypoglycemia was evident with glycated hemoglobin of < 7% (p < 0.0001), 7–9% (p < 0.0001), and < 9% (p = 0.003).
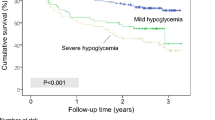
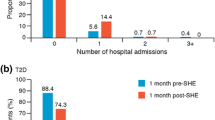
The mean glycated hemoglobin was higher in patients with hypoglycemia (7.8 ± 2.0) and serious hypoglycemia (7.9 ± 2.0), compared to patients without hypoglycemia or serious hypoglycemia (7.5 ± 2.0 and 7.6 ± 2.0, respectively, p < 0.01 for both comparisons). Glycated hemoglobin above 9% was more common in the group of patients with hypoglycemia (20 vs. 15%). (Table 2, Fig. 1).
While most patients with glycated hemoglobin < 7% were treated with a non-insulin glucose lowering drug, most patients with glycated hemoglobin > 9% were insulin-treated.
Compared to no medical treatment for DM, the risk for hypoglycemia associated with insulin treatment was greater in patients with better glycemic control—sixfold increase for hypoglycemia risk in patients with well-controlled DM (glycated hemoglobin < 7%), while in those with uncontrolled DM (glycated hemoglobin > 9%) insulin treatment was not associated with increased risk for hypoglycemia. However, compared to non-insulin glucose lowering treatment, the risk for hypoglycemia was increased by fourfold in all glycated hemoglobin categories (Tables 2a, 3).
Similarly, the risk for serious hypoglycemia with insulin treatment, compared to no medical treatment, was greater in patients with better glycemic control. In patients with glycated hemoglobin > 9%, the only significant difference in the risk for serious hypoglycemia according to treatment was evident with insulin treatment compared to non-insulin glucose lowering treatment (Tables 2b, 3).
Discussion
Hypoglycemia is a major complication in the treatment of patients with DM, and hospitalization is associated with an increased risk for this common event. Following our recent study demonstrating increased mortality rate in patients with in-hospital hypoglycemia [8], in this study we aim to identify pre-admission risk factors and predictors of in-hospital hypoglycemia.
While previous studies report varying rates of hypoglycemia [1,2,3,4,5,6,7,8,9], mainly due to differences in patients characteristics and in the definition of hypoglycemia, our study is based on the recent American Diabetes Association guidelines’ definitions of hypoglycemia (≤ 70 mg/dl) and serious, clinically significant hypoglycemia (< 54 mg/dl) [11]. We have completed a separate analysis of the risk for hypoglycemia and for serious hypoglycemia. Globally, 15% of the patients in our cohort experienced hypoglycemia, and 7% experienced serious hypoglycemia.
Our results identify several risk factors for in-hospital hypoglycemia and serious, hypoglycemia in patients with DM. These include age, BMI, chronic renal failure, cerebrovascular disease, duration of diabetes, glycated hemoglobin in the year prior to admission and insulin treatment. Malignancy and female gender are identified as risk factors for hypoglycemia, but not for serious hypoglycemia, while congestive heart failure is associated with increased risk only for serious hypoglycemia. While this is not the first study to identify predictors of hypoglycemia in hospitalized patients [2,3,4], our study is novel in that it was based on the new hypoglycemia definitions by the American Diabetes Association, and investigated separately the predictors for hypoglycemia (≤ 70 mg/dl) and serious, clinically significant hypoglycemia (< 54 mg/dl). Furthermore, as our data indicates, a significant interaction between hypoglycemia, glycated hemoglobin and the type of treatment for DM, we analyzed the data according to these variables. As there is a clear difference in the risk for hypoglycemia in patients with well-controlled DM without drug treatment, compared to patients with well-controlled DM using insulin treatment, this analysis has important clinical implications.
In accordance with previous studies that have reported increased risk for hypoglycemia in older patients, our results indicate an 11% increase in the risk for hypoglycemia for each additional decade of age. This increase in risk with age may be related to polypharmacy, reduced drug clearance and slow counter-regulatory response in the elderly [3, 20].
Similar to previous reports and not surprisingly, our data clearly indicate increased risk for in-hospital hypoglycemia in insulin-treated patients [4, 7]. This may be related to failure to take into account important factors in the treatment of hospitalized patients with DM, including poor/different nutrition, renal and hepatic failure, advanced age, or hospitalization for infectious diseases, and adjusting the treatment accordingly [16,17,18,19]. In this context, the possible interaction of antimicrobial drugs that favors hypoglycemia should be considered, given the association between in-hospital hypoglycemia and both infections and diseases of genitourinary system. Reduced renal function was also reported previously as a risk factor for in-hospital hypoglycemia, and may be attributed to impaired gluconeogenesis and glycogenolysis, as well as impaired renal insulin degradation and clearance [3, 21,22,23]. We assume these mechanisms also apply in the possible association between congestive heart failure and serious hypoglycemia, though there is limited data on this matter. Cerebrovascular disease may lead to increased risk for hypoglycemia due to poor nutrition or cognitive impairment following the acute insult. The objective of our study is identification of pre-admission risk markers for in-hospital hypoglycemia, but it must be noted that a pre-existing characteristic may interact with other occurring events during the hospitalization in a sort of causal pathway, such as development of malnutrition, renal or liver failure.
Borzi et al. report that hypoglycemia is more frequent among patients with cognitive dysfunction, and this is an independent predictor of hypoglycemia [3]. Similarly, many of these factors, including poor nutrition, renal failure, heart failure, advanced liver disease, advance age, or infections, may contribute to development of hypoglycemia in the hospital setting even in patients without any drug treatments for DM, providing an explanation for the hypoglycemia episodes evident in a significant portion of patients with no glucose lowering treatment in our study [16,17,18,19].
There are several possible explanations for the association between BMI and in-hospital hypoglycemia in our study. First, certain comorbidities, such as malignancy, renal or liver failure, malnutrition, and others, may lead to weight loss, as well as to increased risk for hypoglycemia. Furthermore, the increased in-hospital hypoglycemia risk in the lowest BMI category may be related to maltreatment, poor glycemic control, or poor health conditions [24]. Jackson et al. report that individuals with poorly controlled new-onset DM may have low BMI due to advanced disease state. During the treatment titration period, high glucose variability and increased risk for hypoglycemia may be expected.
Our study shows an interaction between insulin treatment, comorbidities and in-hospital hypoglycemia, indicating that insulin treatment per se, is associated with increased risk for in-hospital hypoglycemia. It is possible that insulin has a more important role in the cumulative risk for hypoglycemia among patients with well-controlled glycemic control, who may be more prone to insulin-induced hypoglycemia, compared to patients with higher HbA1c levels, in which it is possible that comorbidities have a bigger part in the risk for hypoglycemia.
Long-term DM is also associated with increased risk of hypoglycemia, while in patients with DM of less than 10 years there is no increased risk. These findings are most likely due to increased risk of microvascular and macrovascular complications with long-term disease, loss of glucagon response, hypoglycemia unawareness and more advanced treatment.
The glycemic control of patients with hypoglycemia is different from that of patients without hypoglycemia. Only 36% of patients with hypoglycemia have well-controlled DM, compared to 43% of patients without hypoglycemia, whereas glycated hemoglobin > 9% is more common in patients with hypoglycemia. Analysis of the risk of hypoglycemia according to glycated hemoglobin and DM treatment indicates that compared to no glucose lowering treatment, insulin treatment is associated with a significant increased risk (sixfold) in those with well-controlled DM, while the increase is less pronounced (3.6-fold) with glycated hemoglobin between 7 and 9% and insignificant in those with glycated hemoglobin > 9%. However, compared to non-insulin glucose lowering treatment, the increase in risk of hypoglycemia with insulin treatment is fourfold in all glycated hemoglobin categories. The possible explanation for these finding is that in insulin-treated patients with glycated hemoglobin < 7%, the treatment regimen and tight glycemic control is associated with hypoglycemic episodes, while in those with glycated hemoglobin > 9%, the glucose levels are far above the cutoff used to define hypoglycemia. There is no significant difference in the risk of hypoglycemia with non-insulin glucose lowering medication, compared to non-medically treated DM, other than in patients with glycated hemoglobin > 9%. However, due to the small sample size of the latter group, no firm conclusion can be made.
Our study has several limitations. First, the retrospective design of the study, basing data regarding comorbidities solely on the medical records and basing smoking and alcohol on self-report. Further limitation is that patients with a prior history of hyperglycemia or hypoglycemia have a greater chance of having their blood glucose measured more often, with a higher probability of detecting hypoglycemia. Data regarding previous hypoglycemia episodes and hypoglycemia unawareness, as well as diabetic autonomic neuropathy, or possible development of hypoglycemia-associated autonomic failure with defective counter-regulatory and autonomic responses to hypoglycaemia is another important limitation.
Furthermore, the clinical presentation of hypoglycemia, if at all present, was not recorded in the database, as well as the critical problems associated or triggered by in-hospital hypoglycaemia (such as increase in blood pressure, heart rate, cardiovascular events).
The major strengths of our study are the large cohort of patients admitted solely to medical wards, representing real-life experience, as opposed to prospective randomized-controlled studies in which patients undergo intensive monitoring and treatment adjustments. Our definitions are based on the recent guidelines, with separate analysis of patients with hypoglycemia and those with serious hypoglycemia. We also present analysis of the risk of hypoglycemia according to glycemic control and DM treatment.
In conclusion, our findings highlight several independent risk factors associated with in-hospital hypoglycemia and serious hypoglycemia in patients with DM. The present data analysis adds data to previous studies that investigated predictors of in-hospital hypoglycemia and thus can be used to identify hospitalized patients at the highest risk for hypoglycemia. These findings may lead to appropriate monitoring and early intervention, resulting in reduction of morbidity and mortality associated with in-hospital hypoglycemia.
References
Turchin A, Matheny ME, Shubina M, Scanlon SV, Greenwood B, Pendergrass ML (2009) Hypoglycemia and clinical outcomes in patients with diabetes hospitalized in the general ward. Diabetes Care 32:1153–1157. https://doi.org/10.2337/dc08-2127
Elliott MB, Schafers SJ, McGill JB, Tobin GS (2012) Prediction and prevention of treatment-related inpatient hypoglycemia. J Diabetes Sci Technol 6:302–309. https://doi.org/10.1177/193229681200600213
Borzì V, Frasson S, Gussoni G, Di Lillo M, Gerloni R, Augello G et al (2016) Risk factors for hypoglycemia in patients with type 2 diabetes, hospitalized in internal medicine wards: findings from the FADOI-DIAMOND study. Diabetes Res Clin Pract 115:24–30. https://doi.org/10.1016/j.diabres.2016.01.020
Dendy JA, Chockalingam V, Tirumalasetty NN, Dornelles A, Blonde L, Bolton PM et al (2014) Identifying risk factors for severe hypoglycemia in hospitalized patients with diabetes. Endocr Pract 20:1051–1056. https://doi.org/10.4158/EP13467.OR
Eiland L, Goldner W, Drincic A, Desouza C (2014) Inpatient hypoglycemia: a challenge that must be addressed. Curr Diabetes Rep 14:1–9. https://doi.org/10.1007/s11892-013-0445-1
Umpierrez GE, Smiley D, Jacobs S, Peng L, Temponi A, Mulligan P et al (2011) Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery). Diabetes Care 34:256–261. https://doi.org/10.2337/dc10-1407
Varghese P, Gleason V, Sorokin R, Senholzi C, Jabbour S, Gottlieb JE (2007) Hypoglycemia in hospitalized patients treated with antihyperglycemic agents. J Hosp Med 2:234–240. https://doi.org/10.1002/jhm.212
Akirov A, Grossman A, Shochat T, Shimon I (2016) Mortality among hospitalized patients with hypoglycemia: insulin-related and non-insulin related. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2016-2653
Pieralli F, Bazzini C, Casati C, Fabbri A, Crociani A, Corradi F et al (2016) The classification of hospitalized patients with hyperglycemia and its implication on outcome: results from a prospective observational study in internal medicine. Intern Emerg Med 11:649–656. https://doi.org/10.1007/s11739-015-1358-6
American Diabetes Association (2016) Standards of medical care in diabetes—2016. Diabetes Care 37:14–80. https://doi.org/10.2337/dc14-S014
American Diabetes Association (2017) Standards of medical care in diabetes—2017. Diabetes Care. https://doi.org/10.2337/dc14-s014
Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD et al (2009) Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 360:129–139. https://doi.org/10.1056/NEJMoa0808431
The Action to Control Cardiovascular Risk in Diabetes Study Group (2008) Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 358:2545–2559
NICE-SUGAR Study Investigators, Finfer S, Liu B, Chittock DR, Norton R, Myburgh JA et al (2012) Hypoglycemia and risk of death in critically ill patients. N Engl J Med 367:1108–1118. https://doi.org/10.1056/nejmoa1204942
McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA (2012) Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care 35:1897–1901. https://doi.org/10.2337/dc11-2054
Griesdale DEG, de Souza RJ, van Dam RM, Heyland DK, Cook DJ, Malhotra A et al (2009) Intensive insulin therapy and mortality among critically ill patients: a meta-analysis including NICE-SUGAR study data. CMAJ 180:821–827. https://doi.org/10.1503/cmaj.090206
Wiener RS, Wiener DC, Larson RJ (2008) Benefits and risks of tight glucose control in critically ill adults: a meta-analysis. JAMA 300:933–944. https://doi.org/10.1001/jama.300.8.933
Fischer KF, Lees JA, Newman JH (1986) Hypoglycemia in hospitalized patients. Causes and outcomes. N Engl J Med 315:1245–1250. https://doi.org/10.1056/NEJM198611133152002
Cook CB, Potter DJ, Kongable GL (2012) Characterizing glucose changes antecedent to hypoglycemic events in the intensive care unit. Endocr Pract 18:317–324. https://doi.org/10.4158/ep11215.or
Miller ME, Bonds DE, Gerstein HC, Seaquist ER, Bergenstal RM, Calles-Escandon J et al (2010) The effects of baseline characteristics, glycaemia treatment approach, and glycated haemoglobin concentration on the risk of severe hypoglycaemia: post hoc epidemiological analysis of the ACCORD study. BMJ 340:b5444. https://doi.org/10.1136/bmj.b5444
van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M et al (2001) Intensive insulin therapy in critically ill patients. N Engl J Med 345:1359–1367. https://doi.org/10.1056/NEJMoa011300
Rubin DJ, Rybin D, Doros G, McDonnell ME (2011) Weight-based, insulin dose-related hypoglycemia in hospitalized patients with diabetes. Diabetes Care 34:1723–1728. https://doi.org/10.2337/dc10-2434
Arem R (1989) Hypoglycemia associated with renal failure. Endocrinol Metab Clin N Am 18:103–121
Jackson CL, Yeh H-C, Szklo M, Hu FB, Wang N-Y, Dray-Spira R et al (2014) Body-mass index and all-cause mortality in US adults with and without diabetes. J Gen Intern Med 29:25–33. https://doi.org/10.1007/s11606-013-2553-7
Acknowledgements
The authors have no conflicts of interest to disclose. The authors received no external funding for this study. A.A. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Contributions
AA substantial contributions to conception and design, acquisition of data or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, final approval of the version to be published. OA substantial contributions to conception and design, acquisition of data or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, final approval of the version to be published. HMI substantial contributions to conception and design, acquisition of data or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, final approval of the version to be published. TDC substantial contributions to conception and design, acquisition of data or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, final approval of the version to be published. TS substantial contributions to conception and design, acquisition of data or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, final approval of the version to be published. IS substantial contributions to conception and design, acquisition of data or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of retrospective study formal consent is not required.
Rights and permissions
About this article
Cite this article
Akirov, A., Amitai, O., Masri-Iraqi, H. et al. Predictors of hypoglycemia in hospitalized patients with diabetes mellitus. Intern Emerg Med 13, 343–350 (2018). https://doi.org/10.1007/s11739-018-1787-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-018-1787-0