Abstract
Purpose of Review
The aim is to provide a description of the most important echocardiographic features in systemic amyloidosis.
Recent Findings
Amyloidosis is a heterogeneous group of multisystem disorders, characterized by an extracellular deposition of amyloid fibrils. Several imaging tests are available for the diagnosis; however, echocardiography is the cornerstone of the non-invasive imaging modality for cardiac amyloidosis. So far, little is known about the diagnosis of cardiac amyloidosis through imaging modalities.
Summary
We summarized the most important echocardiographic findings in cardiac amyloidosis. Hence, we offered a systematic report of the diagnostic performance of cardiac amyloidosis using echocardiography.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Amyloidosis is a heterogeneous group of diseases caused by the pathological deposition in the extracellular space of misfolded proteins, which subverts the normal structure of various tissues and leads, in the end, to the dysfunction of the organs involved.
The term amyloid derives from the Greek word “άμυλο,” which refers to the starch. In fact, in the past, it was believed that the infiltrative protein mentioned above was made of starch. Subsequently, in the twentieth century, the discovery of the correlation between amyloidosis and multiple myeloma unveiled the composition of the amyloidotic substance [1].
According to the number of the organs involved, amyloidosis can be defined as localized or systemic. The most frequent types of systemic amyloidosis are as follows:
-
1.
Light chain (AL) amyloidosis, in which the precursors of amyloid fibrils are immunoglobulin light chain produced in high concentration due to plasma cellular dyscrasia
-
2.
Mutant transthyretin-related form (ATTRm), caused by more than 100 mutations in the gene codifying for transthyretin, a transport protein synthesized in the liver [2, 3].
-
3.
Wild-type transthyretin-related form (ATTRwt), which differs from the latter because it is not hereditary and affects mainly elderly people.
Amyloid is structurally composed by a principal proteinaceous part and by other substances, such as serum amyloid P component (SAP), apolipoprotein E, connective tissue components (glycosaminoglycans, collagen), and basement membrane components (fibronectin, laminin) [4].
The proteinaceous part, despite some differences depending on the subtype of amyloidosis, is made of monomeric proteins organized in insoluble fibrins, stabilized by cross-b-sheet. More than 30 different proteins are described as involved in the constitution in vivo of the amyloid fibrils. The latter are insoluble, rigid, and resistant to proteolytic degradation [5].
The deposition of amyloidotic fibrils can affect structural and functional alterations of many organs or organ systems (heart, kidney, peripheral nerves, gastrointestinal tract, eyes).
Worldwide, amyloidosis is a rare systemic disorder. The incidence is uncertain, but the most frequent diagnosed, AL amyloidosis, has an annual incidence of 6 to 10 cases per million population in the UK and USA [4].
Diagnosis of Systemic Amyloidosis
Systemic amyloidosis may involve several organs with varying degree of severity. Usually, the diagnosis is determined through histological material from the biopsy of a clinically affected organ. However, when amyloidosis is only suspected, a “screening biopsy” from specific sites (rectum, salivary gland, or fat) is useful in the definitive diagnosis. The sensitivity and the diagnostic value of the biopsy are variable according to the considered tissue.
With regard to cardiac amyloidosis, endocardial biopsy is currently considered the gold standard to diagnose amyloidosis. However, the invasive nature of the biopsy and the low, although not entirely negligible, risk (access site hematoma, transient right bundle branch block, transient arrhythmias, tricuspid regurgitation, and occult pulmonary embolism) limits its use.
Amyloidotic deposits are detected with the Congo red stain in association with polarized light microscopy. The test is based on a peculiar histological feature of amyloidotic substance: it shows a typical red-green birefringence and dichroism effect if analyzed under polarized light microscopy.
However, amyloid deposits are usually irregularly distributed in the tissue. In this case, multiple tissue samplings are needed in order to avoid false negative results.
Cardiac Amyloidosis
The features of cardiac involvement differ according to the stages of diseases. The first phase begins with a subclinical stage characterized by mild and unspecific cardiac symptoms. In this phase, amyloid deposition can involve atria, atrioventricular valves, mild left ventricular (LV) wall thickness (< 15 mm), mild diastolic dysfunction, and mild impaired LV longitudinal strain.
The typical clinical scenario (‘hypertrophic’ stage), in the fully developed disease, is characterized by a marked thickening of the LV wall (> 15 mm) and congestive heart failure with preserved ejection fraction (EF) with a restrictive diastolic pattern with nonspecific symptoms including weakness, fatigue, weight loss or weight gain, and shortness of breath.
Progressively, in the advanced phase of the disease, biventricular systolic function deteriorates, and symptoms of heart failure become refractory to medical therapy (end-stage phase). In most cases, death occurs for electromechanical dissociation or arrhythmia.
Irrespective of the subtype of systemic amyloidosis, cardiac involvement worsens the prognosis and reduces the survival [6,7,8]. Little is known about the relation between the types and severity of cardiac involvement [9•]. AL amyloidosis is associated with a more rapid progression of heart failure than transthyretin-related form (TTR-related) amyloidosis with a median survival of approximately 6 months in untreated AL amyloidosis with heart failure (HF) compared with 6 years in ATTRwt. However, the myocardial involvement is more extensive in ATTRwt than in AL amyloidosis [10••].
There are two reasons why amyloidosis is usually considered a little known pathology: rarity and heterogeneity [11].
Ruberg defined the amyloidotic cardiomyopathy as a “zebra hiding in plain sight.” Although the rarity of this disease is undeniable, we should consider that cardiac amyloidosis is much more common than we would normally think. In fact, a lot of not diagnosed cases of heart failure conceal unrecognized cardiac amyloidosis. Left ventricular wall thickening is sometimes due to multiple factors, such as hypertension, aortic stenosis, long-term training, or amyloidosis. Therefore, the discovery of the main reason provoking the left ventricular hypertrophy should not exclude a secondary rare cause because concomitant cardiac amyloidosis may also be present [12].
Cardiac involvement in systemic amyloidosis is seen in 50% of patients with AL amyloidosis, whereas the prevalence decreases approximately to 2% in patients with TTR-related amyloidosis. However, myocardial amyloidotic deposits have been found even in elderly without systemic amyloidosis.
Cardiac amyloidosis can be diagnosed, excluding the tissue biopsy, with a non-invasive approach, using the advanced imaging techniques. Cardiac magnetic resonance (CMR) has a high specificity. Vogelsberg et al. demonstrated, on a pool of 33 consecutive patients, that in cardiac amyloidosis, late gadolinium enhancement has a peculiar distribution, in the subendocardial layer, extending in various degree in the rest of the myocardium. Besides, they reported that CMR sensibility for diagnosing cardiac amyloidosis is of 80% and specificity is of 94% [13••]. These typical CMR findings observed in hypertrophic stage of cardiac amyloidosis were confirmed by many authors [14•, 15•, 16, 17].
Di Bella et al. have shown that patients without or with only mild LV hypertrophy may have an unusual focal late gadolinium enhancement patterns of inferior and/or inferolateral LV accompanied by enhancement of the atria, tricuspid valve, or the right ventricle.
Nuclear medicine imaging plays a crucial role in the non-invasive diagnosis of cardiac amyloid deposition.
Bone-seeking radiotracers, such as 99mTc-pyrophosphate (99mTc-PYP), 99mTc-methylene diphosphonate (99mTc-MDP), 99mTc-hydroxymethylene-diphosphonate (99mTc-HDP), and 99mTc-3,3-diphosphono-1,2-propanodicarboxylic acid (99mTc-DPD), may differentiate AL from TTR cardiac amyloidosis.
99mTc-DPD and 99mTc-HDP scintigraphy are capable of identifying amyloid deposition in the myocardium of patients with TTR cardiac amyloidosis (i.e., TTR-familial amyloid polyneuropathy and systemic senile amyloidosis) allowing an early diagnosis of the disease, even before the appearance of echocardiographic abnormalities [18]. On the contrary, less intense radiotracer accumulation has been observed in some cases of AL cardiac amyloidosis [19••]. This is helpful in differentiating the diagnosis of ATTR and AL cardiac amyloidosis. In fact, an AL cardiac amyloidosis diagnosis is to consider when the tracer retention is less intense or absent. Additionally, myocardial uptake of bone-seeking radiotracers is correlated with disease severity [20].
Echocardiography Is the First-Line Screening Tool for Cardiac Amyloidosis
The most important echocardiographic feature predictive, although not specific, of cardiac amyloidosis is the left ventricular hypertrophy. The hypertrophy can be symmetric or, in the most of cases, mainly evident in the interventricular septum and it is caused by the deposition of amyloid fibrils. The latter increase the stiffness of the ventricular wall because they compromise the contractile function of the myocardium. Besides, amyloid deposits produce, in fundamental (nonharmonic) imaging, a pathognomonic hyperreflective appearance, defined as “granular sparkling,” of the thickened ventricular myocardium. In addition, harmonic 2D imaging often gives a speckled appearance to the myocardium, which is suggestive of cardiac amyloidosis. Granular sparkling can be observed in a diffuse and uniform pattern or, sometimes, localized in specific segments of the ventricular wall. The most common areas with granular sparkling are the ventricular septum or the posterior wall, whereas the apex does not show indirect sign of amyloidotic presence. This particular distribution reflects the site-specific deposition of the fibrils and justifies the peculiar preservation of the contractile function of the ventricular apex until the last stage of the disease. In the advanced stages of cardiac amyloidosis and, sometimes, in the early stage, even papillary muscles are thickened [21•, 22••].
Accordingly, when cardiac involvement of amyloidosis is revealed by the hypertrophy, the ventricular mass index is increased too. However, cardiac size is usually normal or reduced, whereas the atria are enlarged with a thickened interatrial septum. Right ventricle is normal or thickened, especially in the anterior wall, and enlarged. In patients with right ventricular enlargement, signs of pulmonary hypertension are not rare.
Each one of the four cardiac valves might be affected by amyloidosis and shows themselves thickened, flat, and sometimes with verrucous amyloid deposits [23]. All these morphological abnormalities contribute to functional diastolic and systolic malfunctions [24••, 25, 26, 27].
Left Ventricular Hypertrophy
The thickening of left ventricular wall in cardiac amyloidosis (CA) is the typical morphological finding.
The low voltage on an ECG is an important marker of suspected cardiac amyloidosis if integrated with the echocardiographic evidence of LV hypertrophy [28]. Such a dissociation between echocardiographic and electrocardiographic findings reflects the difference between the amyloidosis and the rest of all the hypertrophic cardiomyopathies. In fact, in amyloidosis, the increase of the left ventricular mass is caused by the infiltrative amyloidotic process and this is not an effective growth, in number or size, of the cardiomyocytes. Therefore, amyloidosis can be considered a “pseudo-hypertrophic cardiomyopathy.” This voltage/mass ratio was summarized by Carroll et al.; they showed that there is an inverse correlation between voltage and muscle cross-sectional area (r = − 0.79) in patients with amyloidosis. Besides, they demonstrated that voltage/mass ratio is directly associated with worst prognostic results. This correlation is consistent with the predictive value of the degree of the infiltration of the myocardium on clinical signs and mortality [29•].
Cardiac amyloidosis is associated with abnormal echogenicity. Therefore, in the past, in order to evaluate the myocardial structure in CA, a non-invasive method called integrated backscatter (IB) was used [30••]. Traditionally, acoustic quantification with IB ultrasonic imaging was performed in several conditions such as hypertrophic cardiomyopathy, myocardial ischemia, and aging heart. IB utilizes the specific acoustic properties of the myocardium to obtain an analysis of the composition of the tissue. In CA, the cycle-dependent variation of myocardial integrated backscatter (CV-IB) analysis also has a prognostic value [31••].
Systolic Left Ventricular Deformation and Function
Cardiac amyloidosis is also called “heart stiff syndrome” because it causes myocardial relaxation abnormalities in early stage and systolic dysfunction in advanced stages. Therefore, a global evaluation of the cardiac performance in amyloidosis can be useful. Myocardial performance index (MPI) or Tei index [32•] combines diastolic and systolic time intervals. It is defined as the sum of isovolumetric contraction time and isovolumetric relaxation time divided by ejection time.
In CA, isovolumetric contraction and relaxation times are prolonged and ejection time is shortened. This justifies the increase of the Tei index in cardiac amyloidosis. Tei et al. demonstrated, contrary to the previous beliefs [33], that isovolumetric relaxation time (IVRT) is prolonged both in early and advanced stage of cardiac amyloidosis, especially in patients with left ventricular wall more than 15 mm. As a consequence, the pre-ejection time is prolonged, whereas the ejection time is shortened. The latter is explained by the impairment of the relaxation properties of the heart in amyloidosis: this implies that the left ventricular end-diastolic volumes cannot increase. The shortening of the ejection time is associated with a decreased left ventricular stroke volume. Hence, in advanced amyloidosis, when the stroke volume starts to decrease, Tei index is high.
In patients with CA, the isovolumetric contraction time (IVCT) is abnormally prolonged, even when the systolic function is not compromised. Koyama et al. [34••], by using strain and strain rate imaging, showed, for the first time, the impairment in systolic function when fractional shortening is still normal.
Therefore, in cardiac amyloidosis, IVCT is a more sensible and earlier marker of systolic dysfunction than ejection fraction.
Tissue Doppler Imaging (TDI) allows to distinguish the true hypertrophy from cardiac amyloidotic “pseudohypertrophy.” TDI measures the longitudinal function of the myocardium through the evaluation of the annular displacement toward the ventricular apex in systole and away from the same in diastole [35•]. The myocardial profiles of the systolic and diastolic curves of velocity recorded from septal or lateral mitral annulus in amyloidosis patients are significantly reduced because the amyloidotic infiltration decreases myocyte longitudinal motion. On the contrary, in the true hypertrophy, the systolic and diastolic curves of velocity are not compromised.
A limitation of TDI consists in reciprocal dependence in the motion of the myocardial segments [22]. In fact, the velocities measured by TDI in one myocardial segment can be influenced by the translation motion driven by the adjacent segments [36•]. TDI is also affected by translational and tethering movements of the heart. On the contrary, Speckle Tracking Echocardiography (STE) has a high special and temporal resolution.
Bellavia et al. [37] showed that in CA strain and strain rate, values are reduced compared with healthy people, even with a completely normal ejection fraction (60%). On the contrary, TDI velocities are less impaired, in particular, in the early stage of the disease. Besides, they reported that strain and strain rate anteroseptal values are significantly higher in patients with advanced CA compared with patients with AL-normal-wall-thickness, even though the same patients with advanced CA had significantly impaired longitudinal systolic function.
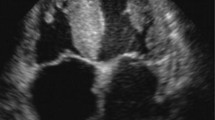
Besides, STE is useful in discerning the cause underlying the ventricular hypertrophy. Global myocardial deformation is lower in CA than in left ventricular hypertrophy. However, in patients with CA, myocardial deformation is not only globally reduced, but it is impaired mostly in the basal segments, whereas the apical contractility is preserved. This expected “apical sparing” is clearly observed on longitudinal speckle tracking [38] (Fig. 1).
Longitudinal deformation by 2D-strain shows severe impairment of global longitudinal deformation (− 11.9%, panel A) with apical sparing due to a lower deformation in basal (green segments) compared to apical segments (blue arrows on panel C). However, the global systolic function is preserved (panel B). (From Di Bella et al. Eur Heart J Cardiovasc Imaging. 2014 Dec;15(12):1307–15, by permission of Oxford University Press) [24••]
The presence of apical sparing is defined through the visual assessment as a reduction of the longitudinal strain in the basal and middle segment relative to apical. However, apical sparing can be calculated as the Relative apical LS index (RapLSI) [39••] as follows:
The apico-basal gradient of longitudinal strain or apical sparing is typically described in patients with advanced cardiac amyloidosis, whereas it is rarely found in the early stage of the disease.
Lee et al. [40] investigated about the benefit of finding the apical sparing in the early stage of CA in order to improve the prognosis. In particular, they demonstrated that patients with left ventricular wall thickness ≤ 14 mm (with no advanced CA) had the apical sparing pattern; however, they have lower RapLSI than patients with advanced CA. This suggests that RapLSI should change over the disease course of CA, maybe depending on the extent of extracellular deposition of the amyloidotic protein.
In particular, in this study, patients with early stage of CA showed a profile characterized by normal ventricular ejection fraction, preserved deceleration time and E/e′, and the highest global longitudinal strain.
Relative apical sparing is distinct, easily recognizable, and specific. In fact, among patients with increased left ventricular wall thickness, RapLSI has incremental value in predicting CA over more traditional parameters.
Furthermore, apical sparing helps to distinguish CA from other cardiomyopathies such as the hypertrophic cardiomyopathy (HCM) [39••]. In fact, HCM is characterized by a marked reduction in longitudinal strain at the septum with normal/super-normal strain values in the resting segments.
The mechanism of the apical sparing is the distribution of the amyloid deposition, which is more expressed in the base than in the apex. Therefore, the apex is less resistant to the deformation and, to compensate the basal and medial segments, increases the myocytes contraction. Another explanation of apical sparing refers to the preserved short-axis function against the impaired longitudinal function in CA. In fact, the short-axis function reflects mainly the apex deformation.
As further proof of the fact that the sparing of apical longitudinal strain is a real phenomenon, an analysis of CMR images in a subgroup of patients with CA showed a significant improvement in regional wall motion score from base to apex [41].
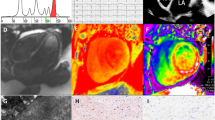
In order to study the complex relationship between systolic and diastolic function in CA, a research group [42] compared the mean strain values in a group of patients with systemic amyloidosis without cardiac involvement (NCA) with a control group. The investigators demonstrated that in NCA the strain values were lower than the control group. Therefore, they showed that is not possible to exclude a systolic impairment even in patients with no evidence of cardiac involvement. In fact, the previous belief, according to which systolic dysfunction occurs only in the advanced stage of CA, is based on studies that do not consider the myocardial longitudinal function. The latter is given by the motion of the subendocardial fibers. To support this, Vogelsberg et al. [13••] found a distinct pattern of myocardial late gadolinium enhancement (LGE) in the group with biopsy-proven cardiac amyloidosis. Most of these patients had LGE distributed over the entire subendocardial circumference, where there are the fibers responsible of the myocardial longitudinal function (Fig. 2).
Longitudinal, circumferential, and radial strain in the different stages of CA. (From Di Bella et al. Eur Heart J Cardiovasc Imaging. 2014 Dec;15(12):1307–15, by permission of Oxford University Press) [24••]
Diastolic Function
The deposition of amyloidotic substance in the myocardial interstitium causes the increase of both the thickness and the stiffness of the ventricular wall thickness. As a consequence, the diastolic ventricular filling is rapid and interrupted in the early phase.
Traditionally, cardiac amyloidosis has been considered to be a “restrictive cardiomyopathy” showing the “square root sign”; however, the hemodynamic filling shows different patterns. The diastolic dysfunction in amyloidosis begins from the atria: the reduced atrial compliance, due to amyloid infiltration, increases the diastolic atrial pressure. Consequently, less interval time of diastole is spent for the atrial and the ventricular filling. Furthermore, a high prevalence [43•] of mitral regurgitation in primary amyloidosis was found. The increase of the atrial volumes due to the mitral regurgitation could significantly elevate early diastolic atrial pressure. As consequence, the transmitral blood flow is rapid. The latter, in association with the high atrial pressure, gives the false impression of a diastolic “restrictive pattern.”
>Early cardiac amyloidosis (with a wall thickness between 12 and 15 mm) shows an abnormal relaxation pattern characterized by a decreased early filing velocity-to-atrial filing velocity ratio (E/A ratio), a normal-to-prolonged deceleration time, and a prolonged isovolumetric relaxation time. This stage is similar to the Doppler flow patterns found in hypertension, coronary artery disease, hypertrophic cardiomyopathy, and the aging process. In contrast, advanced cardiac amyloidosis (with a wall thickness equal to 15 mm or more) showed a short deceleration time and an increasing E/A ratio, which are consistent with restrictive physiology.
The latter diastolic pattern is due to a greater infiltration of the amyloid fibrils of the myocardial cells. Therefore, there is a markedly shortened deceleration time and normal isovolumic relaxation time. The shortened deceleration time is the result of the rapidly increasing early left ventricular diastolic pressure for a small change in volume and an abrupt termination of filling seen classically in restrictive cardiomyopathy (dip and plateau).
However, in the advanced stage of the disease, the evolution of the ventricular filling is controversial. Plehn et al. [44]demonstrated that in the subclinical stage of CA, the low early diastolic filling is compensated by a more intensive late diastolic filling. This provides a pseudonormalization of the diastolic pattern in the advanced stage of the disease. On the contrary, Hongo et al. [45] observed that with the progression of the disease the diastolic pattern continues to deteriorate in the early phase of the diastole. However, it is difficult to discriminate if the decrease of the early diastolic filling is due to the progression of the disease or to the physiological deterioration of the old age. Besides, it is appropriate to draw two considerations [46]: the first one is that the mitral valve involvement in amyloidosis influences the diastolic pattern. The second consideration is that the various amyloid protein types have a specific predilection for infiltration of the mitral valve. Therefore, the filling pattern has complex mechanisms and could be dependent on protein type.
In the early CA, the pulmonary vein flow pattern is quite normal. Pulmonary vein flow is abnormal in the advanced CA: it presents a decreased systolic flow velocity and an increased diastolic flow velocity. In particular, left ventricular inflow and pulmonary vein flow velocities are reciprocal dependent: both peak E velocity and peak diastolic flow velocity increase. The increase in pulmonary vein diastolic flow may result from a rapid decrease in left atrial filling after the increased rapid filling (E velocity) into the stiff ventricle.
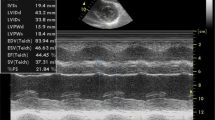
Most of the ventricular filling occurs in the first part of the diastole and is due to the ventricular suction. The latter is influenced by the stored energy generated by the previous systolic contraction. Therefore, diastolic function depends on the myocardial long-axis systolic function. In conclusion, diastolic impairment and longitudinal systolic dysfunction are the signs of cardiac amyloidosis in the earlier stage (Fig. 3).
Moderate increase of LV thickness (20 mm) (A), severe longitudinal dysfunction (S wave 0.03 m/s) on TDI (C), and severe diastolic dysfunction (E/E′23) (B). Note the absence of atrial function on PW Doppler. White arrows indicate a small pericardial effusion. (From Di Bella et al. Eur Heart J Cardiovasc Imaging. 2014 Dec;15(12):1307–15, by permission of Oxford University Press) [24••]
Conclusion
Non-invasive diagnosis of cardiac amyloidosis requires an integrated approach with imaging data obtained using MRI and nuclear medicine. However, conventional echocardiography and the development of strain imaging represent a keystone in the diagnosis and follow-up of patients with suspected and/or definite diagnosis of cardiac amyloidosis.
The main common findings of CA in echocardiography are the following:
-
1.
Increased LV wall thickness in the absence of secondary causes.
-
2.
“Mismatch” between echocardiographic and electrocardiographic findings.
-
3.
“Granular sparkling” appearance of myocardial walls in the nonharmonic imaging.
-
4.
Biatrial dilatation and normal or reduced LV cavity dimensions [47].
-
5.
LV Longitudinal dysfunction and diastolic dysfunction are common findings but not specific signs of CA.
-
6.
Apical sparing is easily recognizable and a specific sign in predicting CA over more traditional parameters. Furthermore, apical sparing helps to distinguish CA from other cardiomyopathies such as the hypertrophic HCM.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Primer on the rheumatic diseases. In JohnH. Klippel, John H. Stone, L Eslie J. Crofford, Patience H. White. Patience H. White, editors. 28th chapter. Springer-Verlag New York. 2008
Mazzeo A, Russo M, Di Bella G, Minutoli F, Stancanelli C, Gentile L, et al. Transthyretin-related familial amyloid polyneuropathy (TTR-FAP): a single-center experience in Sicily, an Italian endemic area. J Neuromuscul Dis. 2015;2(s2):S39–48.
Russo M, Mazzeo A, Stancanelli C, Di Leo R, Gentile L, Di Bella G, et al. Transthyretin-related familial amyloidotic polyneuropathy: description of a cohort of patients with Leu64 mutation and late onset. J Peripher Nerv Syst. 2012;17(4):385–90.
Banypersad SM, Moon JC, Whelan C, Hawkins PN, Wechalekar AD. Updates in cardiac amyloidosis: a review. J Am Heart Assoc. 2012;1:e000364 originally published April 23, 2012.
Flodrova P, Flodr P, Pika T, Vymetal J, Holub D, Dzubak P, et al. Cardiac amyloidosis: from clinical suspicion to morphological diagnosis. Pathology. 2018 Apr;50(3):261–8.
Knight DS,Zumbo G, Barcella W, Steeden JA, Muthurangu V, Martinez-Naharro A, Treibel TA, Abdel-Gadir, et al. Cardiac structural and functional consequences of amyloid deposition by cardiac magnetic resonance and echocardiography and their prognostic roles. JACC Cardiovasc Imaging. 2018.
Mohty D, Damy T, Cosnay P, Echahidi N, Casset-Senon D, Virot P, et al. Cardiac amyloidosis: updates in diagnosis and management. Arch Cardiovasc Dis. 2013;106(10):528–40.
Kotecha T, Martinez-Naharro A, Treibel TA, Francis R, Nordin S, Abdel-Gadir A, et al. Myocardial edema and prognosis in amyloidosis. J Am Coll Cardiol. 2018;71(25):2919–31.
• Stancanelli C, Gentile L, Di Bella G, Minutoli F, Russo M, Vita G, et al. Phenotypic variability of TTR Val122Ile mutation: a Caucasian patient with axonal neuropathy and normal heart. Neurol Sci. 2017;38(3):525–6 This study shows some phenotypical features of TTR amyloidosis.
•• Rapezzi C, Merlini G, Quarta CC, Riva L, Longhi S, Leone O, et al. Systemic cardiac amyloidoses: disease profiles and clinical courses of the 3 main types. Circulation. 2009;120:1203–12 This study provides a global description of systemic cardiac amyloidosis.
Mesquita ET, Jorge AJL, Junior CVS, de Andrade TR. Cardiac amyloidosis and its new clinical phenotype: heart failure with preserved ejection fraction. Arq Bras Cardiol. 2017;109(1):71–80.
Ruberg FL. Cardiac amyloidosis: a zebra hiding in plain sight? Circ Cardiovasc Imaging. 2017;10:e006186.
•• Vogelsberg H, Mahrholdt H, Deluigi CC, Yilmaz A, Greulich S, et al. Cardiovascular magnetic resonance in clinically suspected cardiac amyloidosis: noninvasive imaging compared to endomyocardial biopsy. J Am Coll Cardiol. 2008;51(10):1022–30 This study is important because shows the diagnostic power of cardiac magnetic resonance in amyloidosis.
• Di Bella G, Minutoli F, Mazzeo A, Vita G, Oreto G, Carerj S, et al. MRI of cardiac involvement in transthyretin familial amyloid polyneuropathy. AJR Am J Roentgenol. 2010;195:W394–9 This study demonstrates the diagnostic importance of MRI in cardiac amyloidosis.
• Minutoli F, Di Bella G, Mazzeo A, Donato R, Russo M, Scribano E, et al. Comparison between (99m)Tc-diphosphonate imaging and MRI with late gadolinium enhancement in evaluating cardiac involvement in patients with transthyretin familial amyloid polyneuropathy. AJR Am J Roentgenol. 2013;200(3):W256–65 The study provides a view of two diagnostic tools in cardiac amyloidosis.
Maceira AM, Prasad SK, Hawkins PN, Roughton M, Pennell DJ. Cardiovascular magnetic resonance and prognosis in cardiac amyloidosis. J Cardiovasc Magn Reson. 2008;10:54.
Jason N. Dungu, Oswaldo Valencia, Jennifer H. Pinney, Simon D.J. Gibbs, Dorota Rowczenio, Janet A. Gilbertson, Helen J. Lachmann, et al. CMR-Based Differentiation of AL and ATTR Cardiac Amyloidosis. JACC: Cardiovascular Imaging. 2014;7(2):133–142).
Minutoli F, Di Bella G, Sindoni A, Vita G, Baldari S. Effectiveness of skeletal scintigraphy in transthyretin-related amyloidosis. Int J Cardiol. 2013;168(5):4988–9.
•• Bokhari S, Castanõ A, Pozniakoff T, Deslisle S, Latif F, Maurer MS. (99m) Tcpyrophosphate scintigraphy for differentiating light-chain cardiac amyloidosis from the transthyretin-related familial and senile cardiac amyloidoses. Circ Cardiovasc Imaging. 2013;6:195–201 This study provides the way for differentiating the various types of amyloidosis.
Bokhari S, Castaño A, Pozniakoff T, Deslisle S, Latif F, Maurer MS. 99mTc-Pyrophosphate scintigraphy for differentiating light-chain cardiac amyloidosis from the transthyretin-related familial and senile cardiac amyloidosis. Circ Cardiovasc Imaging. 2013;6(2):195–201.
• Quarta CC, Solomon SD, Uraizee I, Kruger J, Longhi S, Ferlito M, et al. Left ventricular structure and function in transthyretin-related versus light-chain cardiac amyloidosis. Circulation. 2014;129:1840–9 This study provides a differentiation of two types of Cardiac Amyloidosis.
•• Cacciapuoti F. The role of echocardiography in the non-invasive diagnosis of cardiac amyloidosis. J Echocardiogr. 2015;13(3):84–9. https://doi.org/10.1007/s12574-015-0249-1 In this review the most common echocardiographic features of CA are summarised.
Siqueira-Filho AG, Cunha CL, Tajik AJ, Seward JB, Schattenberg TT, Giuliani ER. M-mode and two-dimensional echocardiographic features in cardiac amyloidosis. Circulation. 1981;63:188–96.
•• Di Bella G, Pizzino F, Minutoli F, Zito C, Donato R, Dattilo G, et al. The mosaic of the cardiac amyloidosis diagnosis: role of imaging in subtypes and stages of the disease. Eur Heart J Cardiovasc Imaging. 2014;15(12):1307–15 The review depicts the changes in cardiac imaging among the different stages of the disease.
Koyama J, Davidoff R, Falk RH. Longitudinal myocardial velocity gradient derived frompulsed Doppler tissue imaging in AL amyloidosis: a sensitive indicator of systolic and diastolic dysfunction. J Am Soc Echocardiogr. 2004;17:36–44.
Koyama J, Ray-Sequin PA, Falk RH. Longitudinal myocardial function assessed by tissue velocity, strain, and strain rate tissue Doppler echocardiography in patients with AL (primary) cardiac amyloidosis. Circulation. 2003;107:2446–52.
Bellavia D, Pellikka PA, Abraham TP, Al-Zahrani GB, Dispenzieri A, Oh JK, et al. Evidence of impaired left ventricular systolic function by Doppler myocardial imaging in patients with systemic amyloidosis and no evidence of cardiac involvement by standard two-dimensional and Doppler echocardiography. Am J Cardiol. 2008;101:1039–45.
Di Bella G, Minutoli F, Piaggi P, Casale M, Mazzeo A, Zito C, et al. Usefulness of combining electrocardiographic and echocardiographic findings and brain natriuretic peptide in early detection of cardiac amyloidosis in subjects with transthyretin gene mutation. Am J Cardiol. 2015;116(7):1122–7.
• Carroll JD, Gaasch WH, McAdam KP. Amyloid cardiomyopathy: characterization by a distinctive voltage/mass relation. Am J Cardiol. 1982;49(1):9–13 The review explains the differences in the structure of the left ventricular hypertrophy.
•• Cacciapuoti F. The role of echocardiography in the non-invasive diagnosis of cardiac amyloidosis. J Echocardiogr. 2015;13(3):84–9 This is a complete review of the diagnostic power of echocardiography in amyloidosis.
•• Koyama J, Ray-Sequin PA, Falk RH. Prognostic significance of ultrasound myocardial tissue characterization in patients with cardiac amyloidosis. Circulation. 2002;106(5):556–61 This study demonstrates that myocardial tissue plays a diagnostic and prognostic role in cardiac amyloidosis.
• Tei C, Dujardin KS, Hodge DO, Kyle RA, Tajik AJ, Seward JB. Doppler index combining systolic and diastolic myocardial performance: clinical value in cardiac amyloidosis. J Am Coll Cardiol. 1996;28(3):658–64 This is one of the most complete study about the diastolic disfunction in cardiac amyloidosis.
Klein AL, Hatle LK, Burstow DJ, et al. Doppler characterization of left ventricular diastolic function in cardiac amyloidosis. J Am Coll Cardiol. 1989;1(3):1017–26.
•• Koyama J, Ray-Sequin PA, Falk RH. Longitudinal myocardial function assessed by tissue velocity, strain, and strain rate tissue Doppler echocardiography in patients with AL (primary) cardiac amyloidosis. Circulation. 2003;107:2446–52 This is a complete view about longitudinal ventricular function in patients with cardiac amyloidosis.
• Di Bella G, Minutoli F, Piaggi P, Casale M, Mazzeo A, Zito C, et al. Quantitative comparison between amyloid deposition detected by (99m)Tc-diphosphonate imaging and myocardial deformation evaluated by strain echocardiography in transthyretin-related cardiac amyloidosis. Circ J. 2016;80(9):1998–2003 This study provides a multiparametric description of the amyloid deposition.
• Di Bella G, Minutoli F, Pingitore A, Zito C, Mazzeo A, Aquaro GD, et al. Endocardial and epicardial deformations in cardiac amyloidosis and hypertrophic cardiomyopathy. Circ J. 2011;75(5):1200–8 The review specifies the different motion of epicardial end endocardial layers.
Bellavia D, Abraham TP, Pellikka PA, Al-Zahrani GB, Dispenzieri A, Oh JK, et al. Detection of left ventricular systolic dysfunction in cardiac amyloidosis with strain rate echocardiography. J Am Soc Echocardiogr. 2007;20(10):1194–202.
Belkin RN, Kupersmith AC, Kalique O, et al. A novel two-di- mensional echocardiographic finding in cardiac amyloidosis. Echocardiography. 2010;27:1171–6.
•• Phelan D, Collier P, Thavendiranathan P, Popović ZB, Hanna M, Plana JC, et al. Relative apical sparing of longitudinal strain using two-dimensional speckle-tracking echocardiography is both sensitive and specific for the diagnosis of cardiac amyloidosis. Heart. 2012;98:1442–8 This is a complete and detailed view about apical sparing in cardiac amyloidosis.
Lee GY, Kim HK, Choi JO, Chang SA, Oh JK, Jeon ES, et al. Visual assessment of relative apical sparing pattern is more useful than quantitative assessment for diagnosing cardiac amyloidosis in borderline or mildly increased left ventricular wall thickness. Circ J. 2015;79(7):1575–84.
Austin BA, Tang WH, Rodriguez ER, et al. Delayed hyper-enhancement magnetic resonance imaging provides incremental diagnostic and prognostic utility in suspected cardiac amyloidosis. JACC Cardiovasc Imaging. 2009;2:1369e77.
Porciani MC, Lilli A, Perfetto F, Cappelli F, Massimiliano Rao C, Del Pace S, et al. Tissue Doppler and strain imaging: a new tool for early detection of cardiac amyloidosis. Amyloid. 2009;16(2):63–70.
• Plehn JF, Huntington M, Skinner M, Cohen A. Valvular regurgitation in primary amyloidosis: an early sign of cardiac involvement (abstr). Clin Res. 1988;36:308A This study explains the valvular involvement in the early stage of amyloidosis.
Plehn J, Dilsizian V, Skinner M, Cohen AS. Ventricular diastolic abnormalities in primary amyloidosis without obvious cardiac involvement (abstr). Circulation. 1986;74(suppl II):II-1800.
Hongo M, Fujii T, Jirayama J, et al. Radionuclide angiographic assessment of left ventricular diastolic filling in amyloid heart disease: a study of patients with familial amyloid polyneuropathy. J Am Coll Cardiol. 1989;13:4853.
Plehn JF, Facc, Friedman BJ. Diastolic dysfunction in amyloid heart disease: restrictive cardiomyopathy or not? Editorial Comment JACC. 1989;13(I):6.
Di Bella G, Minutoli F, Madaffari A, Mazzeo A, Russo M, Donato R, et al. Left atrial function in cardiac amyloidosis. J Cardiovasc Med (Hagerstown). 2016;17(2):113–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dalia Di Nunzio, Antonino Recupero, Cesare de Gregorio, Concetta Zito, Scipione Carerj, and Gianluca Di Bella declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Echocardiography
Rights and permissions
About this article
Cite this article
Di Nunzio, D., Recupero, A., de Gregorio, C. et al. Echocardiographic Findings in Cardiac Amyloidosis: Inside Two-Dimensional, Doppler, and Strain Imaging. Curr Cardiol Rep 21, 7 (2019). https://doi.org/10.1007/s11886-019-1094-z
Published:
DOI: https://doi.org/10.1007/s11886-019-1094-z