Abstract
There is a spectrum of disorders that clinically manifest as a result of mast cell activation. A non-clonal form has emerged in the literature where many of the clinical features of systemic mastocytosis are shared despite having a distinct mast cell biology. In this review, we summarize key features of the science behind mast cell activation relevant to what is now known as non-clonal mast cell activation syndrome (nc-MCAS). We highlight the clinical manifestations of nc-MCAS with a focus on diagnosis and treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The collection of signs and symptoms that results from mast cell activation has been well documented in patients with systemic mastocytosis [1, 2]. Many of the clinical features attributable to the systemic effects of mast cell mediators are also seen in patients with allergic diseases and anaphylaxis [3].
Over the past several years, a new clinical disorder has emerged in the literature. In what is now known as non-clonal mast cell activation syndrome (nc-MCAS), patients may exhibit all the signs and symptoms of mast cell activation without evidence for mast cell clonality or obvious allergic phenomena. Although populations of patients with nc-MCAS have been recognized in previous studies, definitions and diagnostic criteria [4•, 5] for nc-MCAS have only been recently proposed and backed by expert opinion [6]. It is therefore possible to study this unique population of patients in order to validate the clinical and diagnostic features of nc-MCAS in various clinical settings. In this review, we will provide an overview of the biology of mast cell activation within the framework of the clinical disorder. We will also discuss the pertinent clinical manifestations of nc-MCAS with an emphasis on diagnosis and treatment in adults.
Biology of Mast Cell Activation
Role of Mast Cells
Mast cells are hematopoietically derived immune cells that home to tissue compartments to carry out physiologic roles in innate host defense against infectious pathogens, neutralization of toxins, and both positive and negative regulation of the adaptive immune response (reviewed in Metcalfe [7] and Galli [8]). In various disease states, mast cells have pathologic roles including the clonal mast cell disorders (e.g. systemic mastocytosis, SM), immediate hypersensitivity reactions, and anaphylaxis (reviewed in Metcalfe [7], Frieri [9] and Brown [10]).
Perhaps not surprisingly, given the complexity and diversity of the mediators and mechanisms by which they are activated, mast cells may also play a pathologic role even in the absence of allergy or clonality.
The majority of patients with SM have mutations of the tyrosine kinase receptor c-KIT, including the D816V activating mutation, which induces constitutional phosphorylation of c-KIT and mast cell activation [8]. The mechanisms by which mast cells are aberrantly activated in nc-MCAS remain unclear. Initial efforts have focused on cKIT, possibly to extend what is known about mast cell activation in SM [11, 12]. Molderings et al. have reported the presence of multiple cKIT mutations and alternative splicing variants in patients with a history suggestive of mast cell activation using peripheral blood-derived CD117+ cells and whole-exome DNA sequencing [13, 14]. Although these are novel findings in a mast cell regulatory gene, functional studies need to be carried out to determine the pathologic significance of these changes. Whichever mechanisms emerge, it is already clear that the pathophysiology of nc-MCAS differs from the disorders characterized by a clonal expansion of mast cells.
Actions of Mediators
Mast cells may be activated in a variety of ways depending on the stimulus coming from the surrounding microenvironment. When the high-affinity IgE receptor is engaged with crosslinked IgE, mast cells may exhibit an “anaphylactic” response where the majority of the mediators are released (Fig. 1). These mediators are responsible for many of the immunomodulatory and inflammatory roles played by mast cells [15] and may be categorized as preformed or newly synthesized. The former include biogenic amines (such as histamine and serotonin), chemokines [such as monocyte chemoattractant protein 1 (MCP-1) and IL-8], and enzymes (such as tryptase and chymase); the latter include cytokines (such as IL-1, 3–6, 13) and lipid mediators (such as LTC4 and PGD2) [16]. With possible relevance to nc-MCAS, mast cells contain many other cell surface receptors that when activated by external stimuli may result in a more selective, non-“anaphylactic” release of mediators. These receptors include Toll-like receptors (TLRs)[17], hormone receptors (for estrogen, progesterone, α-MSH, CRH), cytokine and chemokine receptors (for ligands such as stem cell factor (SCF), nerve growth factor (NGF), macrophage inflammatory protein-1α (MIP-1α)), receptors for the anaphylatoxins (C3a, C5a) [18], and others (reviewed in Akin, [4•]). Conversely, mast cells contain multiple inhibitory receptors, including the low affinity IgG receptor (FcγRIIb), CD200R, the 49-kd surface glycoprotein, the Ig-like receptor p60, the myeloid-associated Ig-like receptor, mast cell function-associated antigen, and the paired Ig-like receptor B [19–21]. Investigation into the roles of these inhibitory receptors has been limited, but may have the potential to explain differential activation and release of mast cell mediators.
Selective release of mediators during mast cell activation may be accomplished in three important and possibly interrelated ways. One is by activation via one of the mast cell’s non-IgE receptors, for instance, through the activation of the IL-1 receptor. Kandere-Grzybowska et al. demonstrated that human mast cells preferentially secrete IL-6 when treated in vitro with IL-1 without cellular signs of traditional degranulation [22]. This type of selective secretion of mediators has also been shown to occur upon the activation of other non-IgE receptors such as TLRs [23]. Another way in which mast cells may selectively activate is through ‘piecemeal’ release of mediators stored in the secretory granules (such as histamine and serotonin). This mechanism entails the extrusion of granule contents through intermediary secretory vesicles without exocytosis of the granules themselves [24–26]. Lastly, downstream signaling pathways may affect mast cell activation. As reviewed by Gilfillan, cross-linked IgE bound to its high affinity receptor (FcER1) leads to signaling through two complementary but independent pathways resulting in the activation of phosphatidylinositol 3-kinase (PI3K) and phospholipase Cγ (PLCγ), each pathway reliant on multiple distinct linker molecules and signaling kinases [27]. Differential activation of mast cells in any of these ways may clinically manifest as nc-MCAS.
From this review of mast cell activation presented thus far, one would have to postulate that stimuli external to mast cells cause aberrant activation in patients with nc-MCAS. It is also conceivable that mast cells in this group of patients may aberrantly possess a lower threshold to release mediators. This may be on display in nc-MCAS patients who become symptomatic with various physical stimuli (e.g., temperature and touch) and medications (e.g., narcotics and alcohol). It is also conceivable that patients with nc-MCAS are symptomatic because of an abnormal tissue response to physiologically appropriate release of MC mediators. For example, some have proposed that a deficiency in the enzymes responsible for histamine metabolism, diamine oxidase (DAO) and histamine N-methyltransferase, leads to excess levels of histamine and therefore histamine intolerance, with clinical manifestations not unlike those described for nc-MCAS [28]. While these hypotheses have to be acknowledged, there is no scientific literature to support their relevance to nc-MCAS.
Multiple mast cell mediators are implicated in nc-MCAS. Because many of the signs and symptoms of clonal mast cell disorders are similar to those of patients with nc-MCAS, the roles of the various mediators can be gleaned from the SM literature and small studies of nc-MCAS patients. As previously reviewed by our group [29], chronic diarrhea is a common symptom of patients with systemic mastocytosis. Use of antihistamines successfully controlled diarrhea in two thirds of a cohort of patients with nc-MCAS [30•]. Similarly, flushing is a common symptom in systemic mastocytosis, and a study performed in patients with nc-MCAS revealed that it can be treated with the careful use of aspirin [31]. Since NSAIDS inhibit the enzyme cyclooxygenase (COX) required for the production of PGD2, this suggests an association between PGD2 and MCAS [32]. The mast cell mediators TNF-alpha, IL-1β, and IL-6 are thought to be implicated in the fatigue observed in some patients with SM; however, it must be noted that evidence is not available to implicate mast cells as the source responsible for these mediators in exclusion of other cell types (reviewed in Castells [29]). Furthermore, actions of these mediators in SM may or may not extrapolate to patients with nc-MCAS.
Clinical Aspects of nc-MCAS
Guidelines and Clinical Manifestations
Several clinical studies have been published that refer to a “mast cell activation syndrome,” “mast cell activation disease,” or “idiopathic mast cell activation syndrome” [33]. “Non-clonal mast cell activation syndrome” is the nomenclature we have used in this review because it implies an idiopathic cause and distinguishes this disorder from the clonal forms. Conditions such as chronic infections, autoimmune conditions, physical urticarias, and certain neoplasms may display release of mast cell mediators, which is defined as “secondary mast cell activation” [6]. It should be noted that nc-MCAS is distinct from idiopathic anaphylaxis (IA), which has its own set of diagnostic criteria that must be rigorously applied [4•, 34, 35].
A diagram that outlines the pathway to a diagnosis of nc-MCAS and that incorporates the proposed diagnostic criteria for nc-MCAS is in Fig. 2. After a careful history, physical exam and basic clinical testing, other medical disorders that may better explain the predominant signs and symptoms observed in mast cell activation must be ruled out. For example, a patient who presents with flushing warrants a diagnostic consideration of carcinoid syndrome, pheochromocytoma, vasoactive intestinal peptide (VIP)-secreting tumors, and medullary carcinoma of the thyroid. In this scenario, tests for urine 5-hydroxyindoleacetic acid (5-HIAA), urine catecholamines, serum VIP, and serum calcitonin levels may be appropriate [36]. A proper evaluation for underlying allergy and atopic diseases should be applied to all MCAS patients.
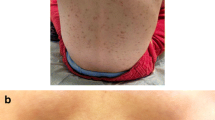
The diagnosis of nc-MCAS must include symptoms from at least two different organ systems. Examples of common organ systems with associated mast cell activation signs and symptoms are the skin (flushing, urticaria, pruritus, dermatographism), gastrointestinal (abdominal pain and diarrhea), pulmonary (wheezing and shortness of breath), upper respiratory (nasal congestion or pruritus, throat swelling), cardiac (tachycardia, syncope or near-syncope), and neurologic (concentration difficulties, headache). In the clinical series of MCAS patients that have been analyzed to date [14, 30•, 37••, 38], the most prominent symptoms consistently described are flushing, abdominal pain, diarrhea, headache, and memory and concentration difficulties.
In a patient who meets these symptom criteria, a clonal mast cell disorder must be considered, keeping in mind the current guidelines for SM and MMAS [1, 39] and the fact that many of the signs and symptoms overlap with nc-MCAS. To this end, baseline levels of mast cell mediators should be checked, in particular serum tryptase. Alvarez-Twose et al. designed an algorithm to predict clonality for patients with mast cell activation using clinical and laboratory parameters derived from patients with nc-MCAS compared with patients with indolent SM. Clonality was found to be associated with male gender, absence of urticaria and angioedema, presyncope, and/or syncope, and a serum total tryptase level of > 25 ng/ml, with scores above a certain threshold having a sensitivity of 92 % and positive predictive value (PPV) of 89 % for clonality [37••]. It is currently accepted that a bone marrow biopsy should be considered in patients with a serum total tryptase >20 ng/ml, or > 11.4 ng/ml (or greater than the upper limit of normal) in patients with a history of hypotensive episodes and/or syncope. Additional clinical findings that may warrant bone marrow examination include urticaria pigmentosa (UP) on skin examination of adult patients; peripheral blood abnormalities [which may suggest an alternative diagnosis, such as SM with an associated hematologic non-mast cell lineage disease (SM-AHNMD), myeloid or mastocytic leukemia, myeloproliferative or myelodysplastic disease, among other diagnostic considerations] [1, 40, 41], or unexplained anaphylaxis including that provoked with hymenoptera sting (especially in the setting of negative specific IgE testing to hymenoptera [42]).
Immunophenotypic evaluation of bone marrow aspirates for mast cell surface expression of CD2 and CD25 is recommended as it increases the PPV of the test and is typically not seen in patients with nc-MCAS [43, 44]. In patients with a suspected clonal mast cell disorder, the D816V cKIT mutation should be tested not only in serum but also in bone marrow aspirate mast cells, as the sensitivity of the assay is greater in the latter [45–47]. Upper endoscopy and colonoscopy should be considered in patients with prominent gastrointestinal symptoms. Biopsies of abnormal and normal areas of bowel with special stains for mast cells (cKIT and tryptase) will allow for an evaluation for the sheets and clusters of mast cells in the mucosal layer that is diagnostic for SM. Immunostains for aberrant CD25 expression on mast cells provide supporting evidence for clonality [48, 49]. Suspicious skin lesions may be biopsied to evaluate for the histologic features of mastocytosis, but this finding alone would not rule in systemic disease [50].
In patients who continue to exhibit signs and symptoms of a mast cell disorder despite lacking evidence for clonality, it is next helpful to obtain objective data in the form of laboratory studies. As noted in the consensus guidelines for nc-MCAS, an increase in serum total tryptase by at least 20 % above baseline plus 2 ng/ml during or within 4 h of characteristic symptoms is evidence for mast cell activation [6]. Additionally, a 24-h urine collection for the measurement of N-methylhistamine and prostaglandin-D2, or its metabolite 11β-prostaglandin F2α, should be obtained after the onset of symptoms. Although the criteria for what constitutes adequate elevation in mediator levels to confirm mast cell activation need to be validated in prospective studies, these are the only laboratory tests that are considered to be clinically relevant to diagnose nc-MCAS at this time. Multiple additional assays exist to evaluate those and other mast cell mediators, but have either an inferior positive predictive value or a lower specificity with respect to mast cell disorders, and therefore should not be routinely used to make a diagnosis of nc-MCAS. More studies are needed to determine specific and reliable assays for mast cell activation.
Limitations of Current Laboratory Tests
Serum tryptase is typically detected using immunoassays, with the B12 monoclonal antibody (mAb) binding to both alpha and beta tryptase, and the G5mAb binding with 10× more affinity to beta tryptase than to alpha tryptase. Thus, alpha tryptase is calculated as the difference between total and beta tryptase [51]. There is some evidence to suggest that rheumatoid factor (RF) interferes with the tryptase assay to yield falsely elevated levels and that the use of heterophile antibody blocking tubes normalizes the levels in more than half of RF + samples with elevated total tryptase [52].
The measurement of serum histamine has several shortcomings that may result in false-positive tests. The assay may detect histamine released by basophils. As reviewed by Oosting et al., false tests may also occur during blood collection and sample preparation due to tissue injury, venous stasis, hemolysis, or clotting, and also by improper centrifugation or storage; a diet rich in histamine may also result in higher serum histamine levels [53]. Tests for serum PGD2 have similar drawbacks, as processing of peripheral blood samples can trigger non-MC cellular elements to release PGD2; ingestion of niacin is also associated with elevations in serum PGD2 [54].
As mentioned previously, there are no other validated clinical tests beyond laboratory studies at this time that can provide objective evidence for nc-MCAS. Bone marrow examination (authors’ unpublished observations) is generally normal, and our group reported that the gastrointestinal biopsies of patients with nc-MCAS displayed normal numbers of dispersed normal-appearing mast cells throughout the gastrointestinal mucosa that were CD25 negative [30•]. It is important to note that there are currently no criteria to determine what constitutes an elevated number of mast cells in the gastrointestinal tract so it may not be helpful to make a diagnosis of a mast cell disorder by number criteria alone.
Treatment
The final useful piece of information to support the diagnosis of nc-MCAS is the patient response to medications that block mast cell mediators. When nc-MCAS is strongly suspected with laboratory evidence of mast cell mediator release, medical treatment using a standard stepwise approach can have excellent results [6] (Table 1). Standard and proven therapy includes use of type I and II histamine blockers and mast cell membrane-stabilizing agents (such as Cromolyn sodium and Ketotifen) [55]. Cysteinyl leukotriene receptor 1 blockers and 5-lipoxygenase inhibitors may be considered in patients with symptoms refractory to the above medications, particularly those with pulmonary symptoms. Aspirin therapy may be especially useful in carefully selected patients who tolerate NSAIDs and who have persistent flushing and elevated urinary 11β-prostaglandin F2 levels [31]. Case reports and case series have suggested that omalizumab may be helpful in controlling refractory symptoms (particularly anaphylaxis) in both patients with nc-MCAS and with systemic mastocytosis, with and without atopic sensitization [56–59]. Systemic or topical steroids, in addition to other immunosuppressants and immunomodulators, may be considered for more refractory or aggressive symptoms, although experience is limited with non-steroid immunosuppressants. Medications that treat pain pathways may be a useful adjunctive therapy. The most important treatment of all, however, may be avoidance of known triggers, so it is important for patients to understand their mast cell-related symptoms and to keep track of provoking factors. Special attention should also be directed towards the patient’s nutritional and mental state.
Special Situations
Many other clinical manifestations of MCAS have been described in the literature based on reports and small patient series [60–64]. Also, there are several clinical associations with nc-MCAS that deserve special attention in this review. Patients who have had life-threatening anaphylactic reactions, especially those without urticaria and with increased baseline levels of tryptase in between episodes [34], should be evaluated for a clonal mast cell disorder with a bone marrow biopsy. If clonality is not seen, then certain patients may be better classified as having idiopathic anaphylaxis [35] using current diagnostic guidelines [4•, 34]. Patients who may have attendant prominent mast cell activation symptoms in addition to syncope and near syncope may be categorized as nc-MCAS with IA, and future diagnostic algorithms should take this subtlety in to account. With this in mind, it is important to recognize that patients with nc-MCAS may be at higher risk for invasive procedures, particularly those requiring general anesthesia. Several studies have documented the potential hazards of muscle relaxants and anesthetics in patients with SM [37••, 65, 66], and only small case series has suggested such risk for patients with nc-MCAS [67]. Thus, it is advisable to take extra precaution, and procedures should be done in close consultation with an anesthesiologist. Perioperative medications should be limited as possible to those that have been tolerated in the past. It is our experience to pre-treat patients with mast cell disorders with type I and II histamine receptor blockers along with steroids and to ensure ready access to an epinephrine pen in those patients with a history of anaphylaxis or syncope. A guide for the care of mast cell patients who present to the emergency department and for invasive and radiologic procedures can be found on the Mastocytosis Society website [68].
In another clinical situation, Shibao et al. and colleagues studied a small cohort of patients who had evidence of mast cell activation as evidenced by elevated urine levels of N-methylhistamine after flushing episodes and who had orthostatic intolerance [69]. Detailed studies revealed a profound hyperadrenergic response to standing characterized by tachycardia and hypertension consistent with postural orthostatic tachycardia syndrome, or POTS. This phenomenon is felt to be due the release of vasoactive mediators such as histamine that act locally on sympathetic nerves; autonomic function was assessed to be normal in these patients. The authors have used methyldopa, an alpha-adrenergic agonist, with some success in these patients along with standard medications to block mast cell mediators. They caution against the use of beta-blockers, which may exacerbate mast cell activation.
Conclusions
Mast cells are complex, multi-faceted immune cells that carry out a range of both homeostatic and pathologic functions in the tissues where they reside. The spectrum of clinical disorders that may arise from aberrant number or function of these mast cells highlights their broad-reaching significance. Non-clonal MCAS has emerged as a clinical disorder, likely with a distinct pathophysiology to the clonal disorders that manifest with mast cell activation. Although proposed criteria exist, larger populations of nc-MCAS must be studied to validate these criteria. This unique population of patients will allow for future studies to identify objective markers of mast cell activation. Lastly, improved identification and awareness of patients with nc-MCAS will allow for more effective and timely therapy.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Valent P, Akin C, Escribano L, Fodinger M, Hartmann K, Brockow K, et al. Standards and standardization in mastocytosis: consensus statements on diagnostics, treatment recommendations and response criteria. Eur J Clin Investig. 2007;37(6):435–53. PubMed PMID: 17537151. Epub 2007/06/01. eng.
Roberts 2nd LJ, Oates JA. Biochemical diagnosis of systemic mast cell disorders. J Investig Dermatol. 1991;96(3):19S–24. discussion S-5S. PubMed PMID: 2002247. Epub 1991/03/01. eng.
Frieri M. Anaphylaxis. In: Raoof S, editor. Manual of critical care. Philadelphia, PA: American College of Physicians, McGraw Hill Co; 2009. p. 721–30.
• Akin C, Valent P, Metcalfe DD. Mast cell activation syndrome: proposed diagnostic criteria. J Allergy Clin Immunol. 2010;126(6):1099–104 e4. PubMed PMID: 21035176. Epub 2010/11/03. eng. This article summarizes the consensus conference where experts proposed diagnostic criteria for non-clonal (idiopathic) mast cell activation syndrome as a distinct disease entity.
Molderings GJ, Brettner S, Homann J, Afrin LB. Mast cell activation disease: a concise practical guide for diagnostic workup and therapeutic options. J Hematol Oncol. 2011;4:10. PubMed PMID: 21418662. Pubmed Central PMCID: 3069946. Epub 2011/03/23. eng.
Valent P, Akin C, Arock M, Brockow K, Butterfield JH, Carter MC, et al. Definitions, criteria and global classification of mast cell disorders with special reference to mast cell activation syndromes: a consensus proposal. Int Arch Allergy Immunol. 2012;157(3):215–25. PubMed PMID: 22041891. Pubmed Central PMCID: 3224511. Epub 2011/11/02. eng.
Metcalfe DD. Mast cells and mastocytosis. Blood. 2008;112(4):946–56. PubMed PMID: 18684881. Pubmed Central PMCID: 2515131. Epub 2008/08/08. eng.
Galli SJ, Grimbaldeston M, Tsai M. Immunomodulatory mast cells: negative, as well as positive, regulators of immunity. Nat Rev Immunol. 2008;8(6):478–86. PubMed PMID: 18483499. Pubmed Central PMCID: 2855166. Epub 2008/05/17. eng.
Frieri M. Mastocytosis. In: Mahmoudi M, editor. Challenges Cases in Allergy Immunology: Humana Press; 2009. p. 201–12.
Brown JM, Wilson TM, Metcalfe DD. The mast cell and allergic diseases: role in pathogenesis and implications for therapy. Clin Exp allergy J Br Soc Allergy Clin Immunol. 2008;38(1):4–18. PubMed PMID: 18031566. Epub 2007/11/23. eng.
Nagata H, Worobec AS, Oh CK, Chowdhury BA, Tannenbaum S, Suzuki Y, et al. Identification of a point mutation in the catalytic domain of the protooncogene c-kit in peripheral blood mononuclear cells of patients who have mastocytosis with an associated hematologic disorder. Proc Natl Acad Sci U S A. 1995;92(23):10560–4. PubMed PMID: 7479840. Pubmed Central PMCID: 40651. Epub 1995/11/07. eng.
Bodemer C, Hermine O, Palmerini F, Yang Y, Grandpeix-Guyodo C, Leventhal PS, et al. Pediatric mastocytosis is a clonal disease associated with D816V and other activating c-KIT mutations. J Investig Dermatol. 2010;130(3):804–15. PubMed PMID: 19865100. Epub 2009/10/30. eng.
Molderings GJ, Kolck UW, Scheurlen C, Bruss M, Homann J, Von Kugelgen I. Multiple novel alterations in Kit tyrosine kinase in patients with gastrointestinally pronounced systemic mast cell activation disorder. Scand J Gastroenterol. 2007;42(9):1045–53. PubMed PMID: 17710669. Epub 2007/08/22. eng.
Molderings GJ, Meis K, Kolck UW, Homann J, Frieling T. Comparative analysis of mutation of tyrosine kinase kit in mast cells from patients with systemic mast cell activation syndrome and healthy subjects. Immunogenetics. 2010;62(11–12):721–7. PubMed PMID: 20838788. Epub 2010/09/15. eng.
Castells M. Mast cell mediators in allergic inflammation and mastocytosis. Immunol Allergy Clin. 2006;26(3):465–85. PubMed PMID: 16931289. Epub 2006/08/26. eng.
Theoharides TC, Kempuraj D, Tagen M, Conti P, Kalogeromitros D. Differential release of mast cell mediators and the pathogenesis of inflammation. Immunol Rev. 2007;217:65–78. PubMed PMID: 17498052. Epub 2007/05/15. eng.
Kulka M, Alexopoulou L, Flavell RA, Metcalfe DD. Activation of mast cells by double-stranded RNA: evidence for activation through Toll-like receptor 3. J Allergy Clin Immunol. 2004;114(1):174–82. PubMed PMID: 15241362. Epub 2004/07/09. eng.
Woolhiser MR, Brockow K, Metcalfe DD. Activation of human mast cells by aggregated IgG through FcgammaRI: additive effects of C3a. Clin Immunol. 2004;110(2):172–80. PubMed PMID: 15003814. Epub 2004/03/09. eng.
Rivera J, Gilfillan AM. Molecular regulation of mast cell activation. J Allergy Clin Immunol. 2006;117(6):1214–25. quiz 26. PubMed PMID: 16750977. Epub 2006/06/06. eng.
Katz HR. Inhibitory receptors and allergy. Curr Opin Immunol. 2002;14(6):698–704. PubMed PMID: 12413518. Epub 2002/11/05. eng.
Castells MC, Klickstein LB, Hassani K, Cumplido JA, Lacouture ME, Austen KF, et al. gp49B1-alpha(v)beta3 interaction inhibits antigen-induced mast cell activation. Nat Immunol. 2001;2(5):436–42. PubMed PMID: 11323698. Epub 2001/04/27. eng.
Kandere-Grzybowska K, Letourneau R, Kempuraj D, Donelan J, Poplawski S, Boucher W, et al. IL-1 induces vesicular secretion of IL-6 without degranulation from human mast cells. J Immunol. 2003;171(9):4830–6. PubMed PMID: 14568962. Epub 2003/10/22. eng.
Varadaradjalou S, Feger F, Thieblemont N, Hamouda NB, Pleau JM, Dy M, et al. Toll-like receptor 2 (TLR2) and TLR4 differentially activate human mast cells. Eur J Immunol. 2003;33(4):899–906. PubMed PMID: 12672055. Epub 2003/04/03. eng.
Dvorak AM, Tepper RI, Weller PF, Morgan ES, Estrella P, Monahan-Earley RA, et al. Piecemeal degranulation of mast cells in the inflammatory eyelid lesions of interleukin-4 transgenic mice. Evidence of mast cell histamine release in vivo by diamine oxidase-gold enzyme-affinity ultrastructural cytochemistry. Blood. 1994;83(12):3600–12. PubMed PMID: 7515717. Epub 1994/06/15. eng.
Dvorak AM, McLeod RS, Onderdonk A, Monahan-Earley RA, Cullen JB, Antonioli DA, et al. Ultrastructural evidence for piecemeal and anaphylactic degranulation of human gut mucosal mast cells in vivo. Int Arch Allergy Immunol. 1992;99(1):74–83. PubMed PMID: 1483068. Epub 1992/01/01. eng.
Dvorak AM. Piecemeal degranulation of basophils and mast cells is effected by vesicular transport of stored secretory granule contents. Chem Immunol Allergy. 2005;85:135–84. PubMed PMID: 15970657. Epub 2005/06/23. eng.
Gilfillan AM, Tkaczyk C. Integrated signalling pathways for mast-cell activation. Nat Rev Immunol. 2006;6(3):218–30. PubMed PMID: 16470226. Epub 2006/02/14. eng.
Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007;85(5):1185–96. PubMed PMID: 17490952. Epub 2007/05/11. eng.
Castells M, Austen KF. Mastocytosis: mediator-related signs and symptoms. Int Arch Allergy Immunol. 2002;127(2):147–52. PubMed PMID: 11919427. Epub 2002/03/29. eng.
• Hamilton MJ, Hornick JL, Akin C, Castells MC, Greenberger NJ. Mast cell activation syndrome: a newly recognized disorder with systemic clinical manifestations. J Allergy Clin Immunol. 2011;128(1):147–52 e2. PubMed PMID: 21621255. Epub 2011/05/31. eng. This study reports on valuable clinical data of patients with non-clonal mast cell activation syndrome. Provides data on therapeutic response to the stepwise approach of mast cell mediator blockade.
Butterfield JH, Weiler CR. Prevention of mast cell activation disorder-associated clinical sequelae of excessive prostaglandin D(2) production. Int Arch Allergy Immunol. 2008;147(4):338–43. PubMed PMID: 18622141. Epub 2008/07/16. eng.
Schwartz LB, Metcalfe DD, Miller JS, Earl H, Sullivan T. Tryptase levels as an indicator of mast-cell activation in systemic anaphylaxis and mastocytosis. N Engl J Med. 1987;316(26):1622–6. PubMed PMID: 3295549. Epub 1987/06/25. eng.
Frieri M PR, Celestin J Mast Cell Activation Syndrome: A Review. Current allergy and asthma reports. 2012;published in this issue.
Akin C. Anaphylaxis and mast cell disease: what is the risk? Curr Allergy Asthma Rep. 2010;10(1):34–8. PubMed PMID: 20425512. Epub 2010/04/29. eng.
Akin C, Scott LM, Kocabas CN, Kushnir-Sukhov N, Brittain E, Noel P, et al. Demonstration of an aberrant mast-cell population with clonal markers in a subset of patients with "idiopathic" anaphylaxis. Blood. 2007;110(7):2331–3. PubMed PMID: 17638853. Pubmed Central PMCID: 1988935. Epub 2007/07/20. eng.
Metcalfe DD. Differential diagnosis of the patient with unexplained flushing/anaphylaxis. Allergy Asthma Proc official J Reg State Allergy Soc. 2000;21(1):21–4. PubMed PMID: 10748948. Epub 2000/04/05. eng.
•• Alvarez-Twose I, Gonzalez De Olano D, Sanchez-Munoz L, Matito A, Esteban-Lopez MI, Vega A, et al. Clinical, biological, and molecular characteristics of clonal mast cell disorders presenting with systemic mast cell activation symptoms. J Allergy Clin Immunol. 2010;125(6):1269–78 e2. PubMed PMID: 20434205. Epub 2010/05/04. eng. This study compares clinical and laboratory characteristics of different groups with mast cell disease, including non-clonal and monoclonal mast cell activation syndrome, in addition to those with systemic mastocytosis. Offers a predictive formula for monoclonality for patients with a clinical picture suggestive of mast cell activation, based on clinical assessments.
Kassab D, Koterba A, Jiang Y, Akin C. Elevated baseline tryptase levels in patients with mast cell activation syndromes without evidence of mastocytosis. J Allergy Clin Immunol. 2008;121(2):S67.
Valent P, Horny HP, Escribano L, Longley BJ, Li CY, Schwartz LB, et al. Diagnostic criteria and classification of mastocytosis: a consensus proposal. Leuk Res. 2001;25(7):603–25. PubMed PMID: 11377686. Epub 2001/05/30. eng.
Frieri M, Linn N, Schweitzer M, Angadi C, Pardanani B. Lymphadenopathic mastocytosis with eosinophilia and biclonal gammopathy. J Allergy Clin Immunol. 1990;86(1):126–32.
Lindner PS, Pardanani B, Angadi C, Frieri M. Acute nonlymphocytic leukemia in systemic mastocytosis with biclonal gammopathy. J Allergy Clin Immunol. 1992;90(3 Pt 1):410–2.
Sonneck K, Florian S, Mullauer L, Wimazal F, Fodinger M, Sperr WR, et al. Diagnostic and subdiagnostic accumulation of mast cells in the bone marrow of patients with anaphylaxis: monoclonal mast cell activation syndrome. Int Arch Allergy Immunol. 2007;142(2):158–64. PubMed PMID: 17057414. Epub 2006/10/24. eng.
Escribano L, Diaz-Agustin B, Lopez A, Nunez Lopez R, Garcia-Montero A, Almeida J, et al. Immunophenotypic analysis of mast cells in mastocytosis: when and how to do it. Proposals of the Spanish Network on Mastocytosis (REMA). Cytometry B Clin Cytom. 2004;58(1):1–8. PubMed PMID: 14994369. Epub 2004/03/03. eng.
Escribano L, Diaz-Agustin B, Bellas C, Navalon R, Nunez R, Sperr WR, et al. Utility of flow cytometric analysis of mast cells in the diagnosis and classification of adult mastocytosis. Leuk Res. 2001;25(7):563–70. PubMed PMID: 11377681. Epub 2001/05/30. eng.
Akin C. Molecular diagnosis of mast cell disorders: a paper from the 2005 William Beaumont Hospital Symposium on Molecular Pathology. J Mol Diagnostics. 2006;8(4):412–9. PubMed PMID: 16931579. Pubmed Central PMCID: 1867614. Epub 2006/08/26. eng.
Garcia-Montero AC, Jara-Acevedo M, Teodosio C, Sanchez ML, Nunez R, Prados A, et al. KIT mutation in mast cells and other bone marrow hematopoietic cell lineages in systemic mast cell disorders: a prospective study of the Spanish Network on Mastocytosis (REMA) in a series of 113 patients. Blood. 2006;108(7):2366–72. PubMed PMID: 16741248. Epub 2006/06/03. eng.
Worobec AS, Semere T, Nagata H, Metcalfe DD. Clinical correlates of the presence of the Asp816Val c-kit mutation in the peripheral blood mononuclear cells of patients with mastocytosis. Cancer. 1998;83(10):2120–9. PubMed PMID: 9827716. Epub 1998/11/25. eng.
Horny HP, Sotlar K, Valent P. Evaluation of mast cell activation syndromes: impact of pathology and immunohistology. Int Arch Allergy Immunol. 2012;159(1):1–5. PubMed PMID: 22555026. Epub 2012/05/05. eng.
Hahn HP, Hornick JL. Immunoreactivity for CD25 in gastrointestinal mucosal mast cells is specific for systemic mastocytosis. Am J Surg Pathol. 2007;31(11):1669–76. PubMed PMID: 18059223. Epub 2007/12/07. eng.
Schwartz LB. Clinical utility of tryptase levels in systemic mastocytosis and associated hematologic disorders. Leuk Res. 2001;25(7):553–62. PubMed PMID: 11377680. Epub 2001/05/30. eng.
Hogan AD, Schwartz LB. Markers of mast cell degranulation. Methods. 1997;13(1):43–52. PubMed PMID: 9281467. Epub 1997/09/01. eng.
Sargur R, Cowley D, Murng S, Wild G, Green K, Shrimpton A, et al. Raised tryptase without anaphylaxis or mastocytosis: heterophilic antibody interference in the serum tryptase assay. Clin Exp Immunol. 2011;163(3):339–45. PubMed PMID: 21303361. Pubmed Central PMCID: 3048617. Epub 2011/02/10. eng.
Oosting E, Neugebauer E, Keyzer JJ, Lorenz W. Determination of histamine in human plasma: the European external quality control study 1988. Clin Exp allergy J Br Soc Allergy Clin Immunol. 1990;20(4):349–57. PubMed PMID: 2198083. Epub 1990/07/01. eng.
Awad JA, Morrow JD, Roberts 2nd LJ. Detection of the major urinary metabolite of prostaglandin D2 in the circulation: demonstration of elevated levels in patients with disorders of systemic mast cell activation. J Allergy Clin Immunol. 1994;93(5):817–24. PubMed PMID: 8182221. Epub 1994/05/01. eng.
Frieri M, Alling DW, Metcalfe DD. Comparison of the therapeutic efficacy of cromolyn sodium with that of combined chlorpheniramine and cimetidine in systemic mastocytosis. Results of a double-blind clinical trial. Am J Med. 1985;78(1):9–14.
Douglass JA, Carroll K, Voskamp A, Bourke P, Wei A, O'Hehir RE. Omalizumab is effective in treating systemic mastocytosis in a nonatopic patient. Allergy. 2010;65(7):926–7. PubMed PMID: 19889117. Epub 2009/11/06. eng.
Carter MC, Robyn JA, Bressler PB, Walker JC, Shapiro GG, Metcalfe DD. Omalizumab for the treatment of unprovoked anaphylaxis in patients with systemic mastocytosis. J Allergy Clin Immunol. 2007;119(6):1550–1.
Bell MC, Jackson DJ. Prevention of anaphylaxis related to mast cell activation syndrome with omalizumab. Ann Allergy Asthma Immunol official publ Am Coll Allergy Asthma Immunol. 2012;108(5):383–4. PubMed PMID: 22541416. Pubmed Central PMCID: 3340573. Epub 2012/05/01. eng.
Molderings GJ, Raithel M, Kratz F, Azemar M, Haenisch B, Harzer S, et al. Omalizumab treatment of systemic mast cell activation disease: experiences from four cases. Intern Med. 2011;50(6):611–5. PubMed PMID: 21422688. Epub 2011/03/23. eng.
Afrin LB. Polycythemia from mast cell activation syndrome: lessons learned. Am J Med Sci. 2011;342(1):44–9. PubMed PMID: 21642812. Epub 2011/06/07. eng.
Afrin LB. Mast cell activation syndrome masquerading as agranulocytosis. Military Med. 2012;177(1):113–7. PubMed PMID: 22338992. Epub 2012/02/22. eng.
Afrin LB. Burning mouth syndrome and mast cell activation disorder. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(4):465–72. PubMed PMID: 21420635. Epub 2011/03/23. eng.
Afrin LB. Sclerosing mediastinitis and mast cell activation syndrome. Pathol Res Pract. 2012;208(3):181–5. PubMed PMID: 22296862. Epub 2012/02/03. eng.
Gonzalez-de-Olano D, Matito A, Sanchez-Lopez P, Sanchez-Munoz L, Morgado JM, Teodosio C, et al. Mast cell-related disorders presenting with Kounis syndrome. Int J Cardiol. 2012;161(1):56–8. PubMed PMID: 22748285. Epub 2012/07/04. eng.
Bilo MB, Frontini F, Massaccesi C, Cinti B, Antonicelli L. Mast cell diseases and the severity and course of intraoperative anaphylaxis. Ann Allergy Asthma Immunol official publ Am Coll Allergy Asthma Immunol. 2009;103(2):175–6. PubMed PMID: 19739433. Epub 2009/09/11. eng.
Brockow K, Jofer C, Behrendt H, Ring J. Anaphylaxis in patients with mastocytosis: a study on history, clinical features and risk factors in 120 patients. Allergy. 2008;63(2):226–32. PubMed PMID: 18186813. Epub 2008/01/12. eng.
Brockow K, Bonadonna P. Drug allergy in mast cell disease. Curr Opin Allergy Clin Immunol. 2012;12(4):354–60. PubMed PMID: 22744266. Epub 2012/06/30. eng.
Slee V, RN, BSN. Emergency Room Protocol: The Mastocytosis Society, Inc.; 2010 [cited 2010 2010].
Shibao C, Arzubiaga C, Roberts 2nd LJ, Raj S, Black B, Harris P, et al. Hyperadrenergic postural tachycardia syndrome in mast cell activation disorders. Hypertension. 2005;45(3):385–90. PubMed PMID: 15710782. Epub 2005/02/16. eng.
Weidner N, Horan RF, Austen KF. Mast-cell phenotype in indolent forms of mastocytosis. Ultrastructural features, fluorescence detection of avidin binding, and immunofluorescent determination of chymase, tryptase, and carboxypeptidase. Am J Pathol. 1992;140(4):847–57. PubMed PMID: 1562049. Pubmed Central PMCID: 1886368.
Sheffer AL, Tong AK, Murphy GF, Lewis RA, McFadden Jr ER, Austen KF. Exercise-induced anaphylaxis: a serious form of physical allergy associated with mast cell degranulation. J Allergy Clin Immunol. 1985;75(4):479–84.
Castells M, Metcalfe DD, Escribano L. Diagnosis and treatment of cutaneous mastocytosis in children: practical recommendations. Am J Clin Dermatol. 2011;12(4):259–70.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cardet, JC., Castells, M.C. & Hamilton, M.J. Immunology and Clinical Manifestations of Non-Clonal Mast Cell Activation Syndrome. Curr Allergy Asthma Rep 13, 10–18 (2013). https://doi.org/10.1007/s11882-012-0326-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11882-012-0326-8