Abstract
Introduction
The present study evaluated intimacy as a mechanism for the effects of relationship-enhancing (self-disclosure, mutual constructive communication) and relationship-compromising communication (holding back, mutual avoidance, and demand-withdraw communication) on couples’ psychological distress.
Methods
Seventy-five men diagnosed with localized prostate cancer in the past year and their partners completed surveys about communication, intimacy, and distress.
Results
Multi-level models with the couple as unit of analyses indicated that the association between mutual constructive communication, mutual avoidance, and patient demand-partner withdraw and distress could be accounted for by their influence on relationship intimacy. Intimacy did not mediate associations between self-disclosure, holding back, and partner demand-patient withdraw communication and distress.
Discussion/conclusions
These findings indicate that the way in which couples talk about cancer-related concerns as well as the degree to which one or both partners avoid talking about cancer-related concerns can either facilitate or reduce relationship intimacy, and that it is largely by this mechanism that these three communication strategies impact psychological distress.
Implications for cancer survivors
Relationship intimacy and how patients and partners communicate to achieve this intimacy is important for the psychological adjustment of early stage prostate cancer survivors and their partners.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The diagnosis and treatment of localized prostate cancer can affect patients’ physical and emotional quality of life. Along with the emotional and practical challenges that accompany the diagnosis of any cancer, the high rates of permanent erectile, urinary, and bowel dysfunction can pose a significant challenge to men’s psychosocial well-being. Indeed, some research suggests that a significantly higher proportion of patients report psychological distress in a clinically-significant range than the general population (20–38%) [1–3]. Partners’ mental health and quality of life can also be adversely affected. Psychological distress among female partners is typically higher than levels of distress reported by patients [3–5] with some studies indicating that 22% of partners meet the criteria for a major depressive or anxiety disorder [6, 7].
In addition to its’ potential adverse psychological impact on patients and partners, prostate cancer may impact the marital relationship. Research suggests that the ways in which patients and partners help each other cope with cancer-related stressors such as worries about cancer recurrence and progression, handle changes in personal and relationship priorities, and maintain a sense of “normalcy” in their relationship [8], may impact the quality of their relationship. However, stressors which are unique to the prostate cancer experience such as ED, incontinence, and compromised masculinity can add to the stress and have a detrimental effect on couples’ sexual and emotional intimacy [9].
Evidence suggests that a higher quality marital relationship may facilitate psychosocial adaptation. For example, Banthia and colleagues [10] found that higher relationship quality predicted lower patient distress and that relationship quality moderated the association between cancer-specific avoidance and intrusions on distress. Specifically, avoidance and intrusions were not associated with distress for men in more satisfactory relationships, but they were associated with greater distress for men in less satisfactory relationships. Relationship quality did not moderate the role of coping among partners. The authors concluded that relationship quality was important for both partners but may play a more important role for patients [11].
Unfortunately, while a better quality relationship can facilitate adaptation for couples, the limited literature published to date suggests that couples may struggle to communicate effectively about prostate cancer. Boehmer and Clarke [12] interviewed 20 men diagnosed with prostate cancer and their wives in order to identify how couples communicate about the impact of prostate cancer. Interviews revealed that there was little direct communication between partners about the disease. Men were not comfortable disclosing their feelings about erectile dysfunction (ED) and other physical changes to their wives. Holding back fears and concerns was common. Wives expressed a wish to share their emotional reactions to the cancer with their spouses but described a similar tendency to hold back discussing their worries and concerns. Couples did not discuss the loss of sexual intercourse with one another. Similar findings were reported by Garos and colleagues [13] who found that couples dealing with early stage prostate cancer reported poorer quality communication about sexual issues than the general population. Lepore and Helgeson [14] evaluated the role of social constraints, defined as avoidance of discussion regarding cancer-related concerns or discomfort talking about cancer with their spouses and family and friends, on the association between intrusive thoughts and prostate cancer patients’ distress. Intrusive thoughts were more strongly associated with greater psychological distress among men perceiving more spousal constraints than among men perceiving fewer spousal constraints. Spousal constraints were also more strongly related to patient distress than were constraints from family and friends.
An interesting set of findings was reported by Kershaw and colleagues [15], who studied the role of spousal communication about cancer (e.g., “We spend a lot of time talking about how things are going with the cancer”) on feelings of hopelessness and illness uncertainty among couples coping with early stage prostate cancer. They found that spouses benefited from better communication with patients because it reduced their uncertainty about the illness. Although patients who reported greater communication had spouses who were less hopeless about the future at the 4-month follow-up, spouse reports of greater communication predicted greater hopelessness for patients. The scale did not distinguish between different types of communication strategies and therefore it is not clear whether the communication used was helpful. These findings suggest that prostate cancer patients and their partners may have different needs and concerns and that greater communication alone may not always be beneficial.
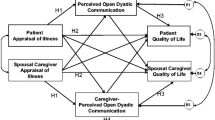
As noted above, communication about prostate cancer may impact distress by influencing illness uncertainty and the degree of engagement in active coping strategies [15]. It may also impact distress by influencing the level of emotional intimacy or closeness each partner experiences. Indeed, the Relationship Intimacy Model of Cancer Adaptation [16] proposes that relationship communication influences couples’ psychological adaptation by its effects on relational intimacy. According to this model, communication can be either “relationship-enhancing” or “relationship-compromising”. Relationship-enhancing communication improves relationship closeness and includes greater cancer-related disclosure and mutual constructive communication (e.g., mutual discussion and expression of feelings about cancer-related concerns). Self-disclosure has been linked with greater intimacy in previous studies of couples coping with other types of cancer [17, 18]. Mutual constructive communication has been associated with lower psychological distress among couples coping with early stage breast cancer [19], and with greater marital satisfaction among couples coping with prostate cancer [8].
Relationship-compromising behaviors such as holding back concerns, actively avoiding cancer-related discussions, and one partner pressuring the other to discuss concerns while the other partner withdraws (demand-withdraw communication) can reduce relationship closeness. Although each of these behaviors has been associated with marital and/or psychological outcomes, they have not been well-investigated in terms of their effects on relational intimacy. For example, holding back has been associated with reduced intimacy and with greater psychological distress [18]. Mutual avoidance has been associated with lower marital quality among men with prostate cancer and their partners [8] as well as directly associated with greater psychological distress [20]. Demand-withdraw communication has been associated with greater marital and psychological distress among men diagnosed with prostate cancer and their spouses [8, 19].
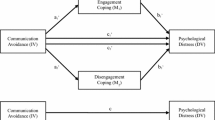
In the present study, we evaluated intimacy as a mechanism or mediator for the effects of four types of cancer-related relationship communication on couples’ psychological distress in a sample of men diagnosed with localized prostate cancer in the past year and their partners. Consistent with the Relationship Intimacy Model, we expected that relationship-enhancing communication (i.e., greater self-disclosure and mutual constructive communication) would be associated with greater relationship intimacy, which in turn would be associated with lower levels of distress for both patients and their partners. We also expected that relationship-compromising communication (i.e., more mutual avoidance, holding back, and demand-withdraw) would be associated with decreased relationship intimacy, which in turn would be associated with greater distress for patients and their partners. The proposed model is shown in Fig. 1. Because studies have shown that medical factors and stressors unique to the prostate cancer experience can adversely effect patients’ communication about cancer-related concerns and their perceptions of intimacy [9], as well as patients’ [5, 21, 22] and partners’ [3, 4] distress responses, our analyses took into account medical side effects including erectile, urinary, and bowel function, as well as Gleason score, cancer stage, and time since diagnosis.
Methods
Participants
The sample was comprised of men diagnosed with localized prostate cancer who were seen at two cancer centers in the Northeastern United States (Fox Chase Cancer Center and Memorial Sloan-Kettering Cancer Center). These data were collected as part of a randomized clinical pilot study of a couple-focused intervention (Manne et al., unpublished data). Eligibility criteria for patients were: diagnosed with localized prostate cancer in the last year, Eastern Cooperative Oncology Group (ECOG) [23] performance status score of 0 or 1, and married or living with a significant other of either gender. In addition, patients and partners had to be 18 years or older, could not have a hearing impairment, live within a two hour commuting distance of the center they were recruited from, and be English speaking.
In all, 330 couples were approached to participate. One hundred fifty eight couples agreed to participate but did not return surveys. Seventy-five consented and completed the survey (22.7% acceptance). The most common reasons for refusal were that the study would take “too much time” (18%) and that the they would not benefit from participation (13%). Comparisons were made between patient participants and refusers on available data (i.e., age, Gleason score, time since diagnosis, cancer stage). Results indicated that participants were significantly younger (t (320) = 3.6, p < .001; M refusers = 63.8, M participants = 59.8) and had been diagnosed for a longer period of time (t (320) = 3.5, M refusers = 6.44 months, M participants = 8.26 months).
Procedures
Participants were identified and letters sent regarding the study. Next, they were contacted by the research assistant either after an outpatient visit (if one was scheduled within the next two weeks) or by telephone. If patient and partner indicated an interest in participating during a contact, they were provided with a written informed consent and the study questionnaire to complete and return by mail. Participants were contacted starting two weeks after the questionnaire was sent if the consent and survey were not returned. Participants were contacted by telephone weekly until the consent and survey were returned. If the material was not returned after two months, a reminder letter was sent. Three final contact calls were made over the course of the two weeks after the reminder letter was sent. If the material was not returned after three months of attempts to contact the individual, the participant was labeled a study refuser.
All participants signed an informed consent approved by each institution’s Institutional Review Board.
Measures
Erectile, bowel, and urinary dysfunction
The International Index of Erectile Function (IIEF) Erectile Domain subscale consists of 5 items assessing erection frequency, firmness, penetration ability, and difficulty maintaining an erection. This widely used scale has excellent reliability (.92-.93) [24]. Scores between 26 and 32 indicate no ED, scores between 22 and 25 indicate mild ED, scores between 17 and 21 indicate moderate ED, and scores between 6 and 10 indicate severe ED [25]. The urinary and bowel scales of the UCLA Prostate Cancer Index (PCI) were administered [26]. The scale has demonstrated excellent reliability [27]. In the present study, internal consistency reliability (Cronbach’s alpha) for the IIEF–ED scale was .97. For the PCI-Urinary function scale, the internal consistency was α = .87, and for the PCI-Bowel function the internal consistency was α = .69.
Relationship-enhancing communication
Self-disclosure
We used a 10-item measure adapted from Pistrang and Barker [28] used previously by Porter and colleagues [18] with gastrointestinal cancer patients. Patients and partners rated how much they talked to their partner about ten cancer-related problems (e.g., concerns about your/your partner’s physical symptoms, concerns about your/your partner’s sexual function) in the past week on a 6-point scale ranging from 0 (not at all) to 5 (a lot). Internal reliability coefficients in the present study were α = .91 for patients and α = .85 for partners. These figures are similar to those reported in research with early stage breast cancer patients and their partners (αpatients = .86; α partners = .85) [17] and those reported by the scale’s authors (α wives = .84; α husbands = .82) [29].
Mutual constructive communication
The Mutual Constructive Communication subscale of the Communications Pattern Questionnaire (CPQ) [30–32] is a 5-item scale that has been adapted for use in the cancer setting by asking the couple to rate how they typically deal with cancer-related stressors or problems [19]. All items are rated on a 9-point Likert scale. The scale has shown good reliability in our prior work with cancer patients and their partners (α = .63–.80) [19]. In the present study, internal consistency was α>.84 for patients and for partners.
Relationship-compromising communication
Mutual avoidance
The Mutual Avoidance subscale of the CPQ [29, 30] is a 3-item scale that has been adapted for use in the cancer setting by asking the couple to rate on a 9-point Likert scale how they typically deal with cancer-related relationship stressors or problems [19]. The scale has shown reasonable reliability in prior work with cancer patients and their partners (α = .63–.79) [8, 19]. Internal consistency reliability for this study was α = .50 for patients and partners.
Holding back
A 10-item measure adapted from Pistrang and Barker was used [28]. Participants rated how much they held back talking to their partner about ten cancer-related problems (e.g., concerns about your/your partner’s physical symptoms, concerns about sexual function) in the past week on a scale ranging from 0 to 5 with higher scores indicating greater levels of holding back. Internal consistency reliabilities in the present study, α=.89 for patients and α = .89 for partners, were similar to those reported in prior research (α = .85 for patients and for partners) [18].
Patient demand-partner withdraw (PtD-PaW) and partner demand-patient withdraw (PaD-PtW)
The Demand-Withdraw subscale of the CPQ [30–32] is a 6-item scale that has been adapted for use in the cancer setting by asking respondents to rate how they typically deal with cancer-related stressors or problems on a 9-point Likert scale that ranged from ‘unlikely’ to ‘likely’ [19]. Items assess the frequency of one partner pressuring to talk about an issue and the other partner withdrawing from or avoiding the discussion. Three items assess patient demand-partner withdraw, and three items assess partner demand-patient withdraw. A sample item is, “Your partner nags and demands while you withdraw, become silent, or refuse to discuss the matter further.” These scales have shown good reliability in our prior work with cancer patients and their partners (α = .63–.79) [8, 19]. In this study, internal consistency reliabilities were: patient ratings for patient demand-partner withdraw α = .64, partner demand-patient withdraw α = .73; partner ratings for patient demand-partner withdraw α = .79, partner demand-patient withdraw α = .70.
Relationship adjustment
The well-validated 32-item Dyadic Adjustment Scale (DAS) is the most widely used measure of relationship functioning and satisfaction [33]. Scores can range from 0 to 151; scores below 97 indicate relationship distress. Participants rated the frequency with which they engaged in specific behaviors with their partners and the level of agreement on relationship issues. This scale has good content validity and demonstrated excellent reliability in the present study (αpatients = .91, α partners = .91).
Mediator and outcome
Global relationship intimacy
The Personal Assessment of Intimacy in Relationships (PAIR) [34] is a 7-item scale assessing emotional closeness. It has been used in studies of relationship intimacy among healthy married couples [35]. The scale has demonstrated good internal consistency in previous work focusing on women diagnosed with early stage breast cancer and their partners (α patients = .90; α partners = .88). In the current study, the internal consistencies were: αpatients = .83, αpartners = .85.
Distress
The BSI-18 is a brief version of the BSI-53 [36]. It yields a global rating of psychological distress called the Global Severity Index (GSI). The scale had excellent reliability in the present study (αpatients = .91, αpartners = .91). The cutoff for clinically-significant levels of distress is a T-score of ≥ 63.
Analytic strategy
Descriptive statistics (e.g., means, standard deviations, and correlations) were calculated for each of the major study variables and potential mean differences on the major study variables based on social role (i.e., whether an individual was a patient or partner) were examined.
Because data from couples tend to be related, analyses must adjust for this non-independence so that statistical significance tests are not biased. A multilevel modeling approach was used whereby data from both members of the couple were treated as nested scores within the same group (i.e., the couple) [37]. Based on the Relationship Intimacy Model [13] (see Fig. 1), a series of analyses were conducted to examine the associations between patients’ and partners’ own distress and their reports of relationship-enhancing (i.e., self-disclosure, mutual constructive communication) and relationship compromising communication (i.e., holding back, mutual avoidance, patient demand- partner withdraw, partner demand- patient withdraw) and to determine whether perceptions of relationship intimacy (PAIR scores) mediated these associations.
All the predictor variables were grand-mean centered by subtracting the sample mean from each individual score. Six multilevel models (one for each communication predictor) were tested using the causal steps approach [38]. This approach for testing mediation, which has been used extensively in the marital literature to test mediation when data is collected from both members of the couple (see [39, 40]); is based on the classic Baron and Kenny [41] method. It is appropriate because the links relevant to the mediational analyses involved fixed rather than random effects [42]. Basically, in addition to establishing a significant association between the predictor and the outcome, four additional steps are required to establish mediation and each step must produce a significant result in order to proceed to the next step [35]. For example, for the predictor mutual constructive communication (MCC), we first tested whether MCC was significantly associated with the proposed mediator, intimacy. Then, we tested whether the mediator (intimacy) predicted the outcome, distress, after controlling for MCC. Next, we tested the mediated paths from MCC via intimacy to distress using bootstrap analysis. Bootstrapping was chosen as opposed to other methods (i.e., Sobel’s Test) because it is a more sensitive test, is appropriate for smaller samples (as is the case here), and does not assume a normal distribution [35]. If the 95% confidence interval that is generated by the bootstrap test does not include zero, significant mediation is achieved. Finally, we tested the direct paths from MCC to distress when controlling for intimacy to determine whether mediation was partial or complete. If the direct effect of the predictor on the criterion remains significant after controlling for the mediator, partial (as opposed to complete) mediation is indicated. The same procedure was followed for each of the remaining communication predictors (i.e., self-disclosure, holding back, mutual avoidance, and demand-withdraw communication).
Results
Descriptive results
Sample characteristics are shown in Table 1. The sample was primarily Caucasian and relatively well-educated. Approximately half of the sample had undergone surgery. Among the 44 patients having surgery, 45.5% had radical prostatectomy and 54.5% had robotic assisted laparoscopic surgery. About a third of the sample underwent radiation therapy, and a small percentage had hormonal therapy alone or with radiation. Among the 24 patients having radiation therapy, 83.3% had intensity-modulated radiation therapy (IMRT) and 16.7% had brachytherapy. Scores on the IIEF Erectile Dysfunction (ED) subscale indicated that 42.5% of men had severe ED and 10% of men had moderate ED.
Descriptive information for variables included in the analyses is shown in Table 2. Average levels of disclosure were relatively high (6-point scale) with a significantly higher mean for patients’ self-disclosures as compared to partners’ self- disclosures (t (141) = 3.8, p < .05). Conversely, average levels of holding back were low with a relatively higher level of holding back among partners (M = 1.5) as compared with patients (M = 1.1) (0 = not at all, 5 = all the time). Mutual constructive communication scores were similar to our previous work with breast cancer patients [43]. Mutual avoidance was lower than mean scores reported by Badr and Carmack Taylor [8] in their study of prostate cancer patients (M patients = 8.37, M partners = 8.38) (t patients (189) = 2.5, p < .05; t partners (189) = 2.75, p < .05), but similar to our previous studies of early stage breast cancer patients [43]. Analysis of DAS and BSI scores indicated that the sample reported a high degree of relationship satisfaction and was not clinically distressed. Only 3 patients (4.1%) and 5 partners (7%) scored below the DAS cut off for relationship distress; 5 patients (6.7%) and 5 partners (6.7%) met the BSI criteria for psychological distress.
Analysis of the item means for the self-disclosure and holding back scales showed that patients were most likely to disclose concerns about cancer treatment (e.g., medical or surgical treatments, interactions with doctors and nurses, being in the hospital) (M = 4.1, SD = 1.3) and about sexual functioning (M = 3.7, SD = 1.3). Partners were most likely to disclose concerns about the patient’s cancer treatment (M = 3.3, SD = 1.6) and the patient’s physical symptoms such as pain, fatigue, and bowel function (M = 3.1, SD = 1.6). Patients were most likely to hold back from sharing concerns about sexual functioning (M = 1.6, SD = 1.6) and about their worries about disease progression/death (M = 1.5, SD = 1.6). Partners were most likely to hold back from sharing emotional reactions (M = 2.1, SD = 1.6) and fears and worries about disease progression or death (M = 2.4, SD = 1.9).
Table 2 displays correlations, means, and standard deviations for the major study variables. As expected, patient and partner reports of distress, intimacy, and relationship adjustment were significantly correlated. The only medical factor that was significantly associated with intimacy was patient erectile function; bowel function was the only medical factor associated with distress. Interestingly, erectile, urinary, and bowel function were not significantly associated with patient reports of relationship-enhancing or relationship-compromising communication behaviors. With regard to mean differences, patients reported greater intimacy, mutual constructive communication and self-disclosure than partners; partners reported greater holding back than patients.
Prior to conducting multilevel analyses, correlations between participant distress and demographic (i.e., age, income, length of relationship) and social factors (i.e., relationship adjustment) were examined across both members of the couple. Differences in distress based on participant ethnicity and employment status were also examined. In addition to the correlations between distress and patient medical factors (i.e., IIEF-Erectile Function, PCI-Urinary Function, and PCI-Bowel Function) reported in Table 2, correlations between distress and time since diagnosis, type of treatment (radiation, surgery, hormonal therapy), and Gleason score were examined, as were mean differences on distress based on disease stage. Variables with p-values less than .05 were retained as model covariates. The variables included as covariates in the final model were: participant age (r = -.17, p = .04), participant relationship satisfaction (r = -.44, p = .001), and patient PCI-Bowel Function (r = -.53, p = .001).
Multilevel modeling results
Relationship-enhancing communication
Mutual constructive communication (MCC)
As Table 3 shows, patients and partners who reported greater MCC regarding their cancer-related concerns reported lower levels of distress and greater intimacy. Greater intimacy was associated with less distress after controlling for reports of MCC. The total effect of MCC and intimacy on distress was -.26, and the mediated effect was -.06 (SE = .04). The 95% bias corrected and accelerated confidence interval (CI) from the bootstrap analysis was (-.15, -.01). Based on the decomposition of the total effect into direct and indirect effects, we calculated that 28% of the relationship between MCC and distress for patients and their partners was explained by intimacy. Because the direct path from MCC to distress was not significant after controlling for intimacy, results were consistent with full mediation.
Self-disclosure
When analyzed at the couple level, self-disclosure was not significantly related to intimacy (b = .02, SE = .04, t (122) = .51, p = .61) or distress (b = .49, SE = .47, t (131) = 1.03, p = .31). Mediation requires significant associations between the predictor, mediator, and outcome, so no further analyses were conducted.
Relationship-compromising communication
Mutual avoidance (MA)
Patients and partners who reported greater MA of cancer-related concerns reported higher levels of distress and lower levels of intimacy (see Table 3). Lower levels of intimacy were also associated with greater distress after controlling for reports of MA. The total effect of MA and intimacy on distress was estimated to be .44 and the mediated effect was .08 (SE = .06, 95% CI = .01, .25), which is consistent with full mediation. Based on this, we calculated that 22% of the overall relationship between MA and distress for patients and their partners was explained by intimacy.
Holding back
When patients and partners reported holding back more of their cancer-related concerns, they reported greater distress and less intimacy. However, the association between intimacy and distress was only marginally significant after controlling for the effects of holding back (p = .06), suggesting that intimacy did not mediate the association between holding back and distress (see Table 3).
Patient demand- partner withdraw (PtD-PaW) communication
Patients and partners who reported greater patient demand-partner withdraw communication, also reported greater distress and less intimacy. Lower levels of intimacy were also related to greater distress after controlling for reports of PtD-PaW communication (see Table 3). The total effect of PtD-PaW communication and intimacy on distress was .31 and the mediated effect was .08 (SE = .05, 95% CI = .003, .23), which is consistent with full mediation. Thus, 35% of the overall relationship between PtD-PaW communication and distress for patients and their partners was explained by intimacy.
Partner withdraw—patient demand (PaW-PtD) communication
Although greater PaW-PtD Communication was associated with less intimacy for patients and partners (b = -.04, SE = .01, t (122) = -4.27, p = .001), it was not associated with distress (b = .10, SE = .10, t (136) = .98, p = .33). Given this, no further tests of mediation were conducted.
Discussion
It is surprising given the potentially significant impact of prostate cancer on the intimate relationship that there has been relatively little empirical attention paid to the topic of how couples communicate with one another about this illness or the mechanisms for how couples’ communication impacts distress. The little empirical evidence offered to date suggests that couples may have difficulty openly communicating their concerns. Surprisingly, the results of the present study suggest that the majority of couples had relatively high levels of disclosure with one another (Ms = 2.5 – 3.3 on a 0–5 point scale). With a few exceptions in terms of topics (e.g., sharing worries about disease recurrence), couples engaged in relatively low levels of holding back sharing concerns. Levels of mutual constructive communication were high, with average levels of 35 to 37 on a 45-point scale. It is also interesting to note that patients disclosed significantly more than partners. Although it is possible that the higher level of disclosure among the men reflects that fact that these men agreed to a couple-focused intervention study which entailed sessions focusing on disclosure and intimacy (if randomly assigned to that condition), future studies should compare self-disclosure between partners. The main goal of this study was to evaluate whether couples’ communication strategies influenced distress through their influence on relationship intimacy. Whereas three of our models were supportive of this hypothesis, three others were not. We discuss each finding below.
The association between a positive strategy that couples used to discuss cancer-related problems and concerns, mutual constructive communication, and distress was accounted for by its’ influence on relationship intimacy. Two unconstructive strategies, mutual avoidance and patient demand-partner withdraw, were also associated with reduced intimacy and, in turn, greater distress. Together, these findings suggest that the way in which couples talk about, and importantly, the degree to which one or both partners avoid talking about cancer-related concerns, can either facilitate or reduce relationship closeness, and that it is largely through this process that these three communication strategies impact psychological distress.
The fact that full as opposed to partial mediation was consistently indicated regardless of the communication predictor examined (i.e., mutual constructive communication, mutual avoidance, and patient demand — partner withdraw communication) deserves mention and suggests that intimacy is an important mechanism that may help to explain how couples’ communication and interaction patterns influence individual psychological distress. Although a prospective study design would provide a more stringent test of mediation, our findings provide support for the Relationship Intimacy Model of Cancer Adaptation [16], and suggest that intimacy may be a key target for future couples interventions aimed at reducing distress and improving both partners’ psychosocial adaptation to prostate cancer.
The associations between three communication strategies and psychological distress were not mediated by intimacy. First, self-disclosure was not associated with distress and therefore intimacy could not be evaluated as a mediator. Even more surprising is the fact that the associations between patient and partner self-disclosure and intimacy were not significant (r = .11 and .13, respectively). These findings are not consistent with associations between patient self-disclosure and patient relationship intimacy reported by Porter and colleagues [18]. A possible explanation is that it is the level of mutuality—that is, the perception that both partners are expressing feelings, both partners are discussing the concern and suggesting ideas for how to manage the issue, and a feeling that both partners feel understood, are greater determinants of relationship intimacy, and ultimately, of distress. Our findings regarding mutual constructive communication, which assesses a mutuality and reciprocity in couples’ approaches, support this explanation. Recent work by Berg and colleagues [44] on collaborative or communal coping suggests that it may be the perception of collaboration or joint coping that reduces emotional distress among prostate cancer patients and their partners. In our results, self-disclosure alone did not facilitate intimacy, without considering the perception of what the partner did in response.
Second, whereas intimacy mediated the association between patient demand- partner withdraw and distress, intimacy did not mediate the association between partner demand-patient withdraw, because this strategy was not associated with distress. These findings indicate that withdrawal may be more detrimental when patients desire to talk about cancer-related issues than vice versa. One possible explanation for this finding is that caregivers are expected to discuss the patient’s concerns, whereas the expectations of patients to discuss partner concerns may not be as high. A second explanation is that the most highly rated concerns that were shared by patients regarded sexual functioning and the cancer treatment. If partners withdraw when these topics are discussed, given the expectation for caregiver responsiveness, this may have a stronger effect on intimacy and distress than when patients withdraw when partner’s concerns are raised.
The third finding that was not consistent with the Relationship Intimacy Model was the fact that intimacy did not mediate the associations between holding back of cancer-related concerns and distress, particularly given the fact that holding back was associated with lower intimacy. However, this finding is partially explained by the fact that, although partner holding back was associated with increased distress (r = .66, p < .001), patient holding back was not associated with distress (r = .12). It is possible that couples hold back in order to reduce their distress. Therefore, while it reduces relationship intimacy, it may not lead to distress reactions as the well-intentioned stance is intuitively understood by the other partner.
We originally predicted that greater erectile, bowel, and urinary dysfunction would be associated with higher levels of relationship-compromising communication as well as with greater distress; however, this was only the case for bowel dysfunction. Although the association between these symptoms and relationship communication has not been studied among couples coping with prostate cancer, studies of couples coping with breast cancer [45] and studies of couples dealing with other chronic illnesses (e.g., [46, 47]) have shown that spouses are more likely to engage in unsupportive behaviors when the ill partner reports higher levels of physical disability. One possible explanation for these findings is that erectile and urinary symptoms are not disabling in the same way as problems completing activities of daily living and engaging in social activities as the disability associated with other illnesses such as rheumatoid arthritis. On the other hand, problems with bowel habits (e.g., leaking stool, rectal pain, abdominal cramping) can dramatically interfere with daily functioning. However, the fact that erectile dysfunction was not associated with communication is curious, particularly in light of the fact that patients disclosed more about their concerns about sexual functioning than other concerns and that patients held back from disclosing about sexual concerns more than the majority of other concerns. It is possible that these couples, who were in relationships of a long duration, may have focused more on the relationship as a determinant of their distress than upon the physical symptoms the patient was experiencing. Future studies should evaluate more closely the association between these symptoms and couples’ communication about sexuality, together with couples’ pre-cancer treatment sexual functioning.
There are limitations of the study which need to be noted. Most importantly, the cross-sectional design limits conclusions about the directionality of effects. Although we controlled for the effects of global marital satisfaction on the model, pre-existing distress may influence the communication strategies that both partners use as well as relationship intimacy. Extending the evaluating to longitudinal outcomes would provide a stronger test of the model, as well as evaluating the effects of earlier distress on later communication and intimacy. Although our measure of mutual avoidance was from a published scale which has demonstrated adequate internal consistency reliability in previous studies of cancer patients and their partners, reliability for this study was low. While this is a concern, there are two reasons why the present findings regarding mutual avoidance are likely to be valid. First, low reliability has been shown to affect Type II but not Type I error rates, meaning it can make it less likely to observe significant results but does not cause spuriously significant findings [48]. Second, Schmitt [49] noted that the .70 alpha criterion for reliability is not always appropriate when scale length is short (MA had three items) and demonstrated that reliabilities as low as .50 do not seriously attenuate validity coefficients. He further argued that when measures have other desirable properties such as meaningful content coverage, low alphas need not deter their use. Another limitation is the study acceptance rate. This may in part be due to the fact that these couples were being approached for a couple-focused intervention study which required them to come to the hospital where they were being treated for five 90-minute sessions. Our acceptance rates are lower than those reported by Northouse and colleagues [50] who used a combination of home visit and telephone counseling rather than in-person sessions. Unfortunately, Canada and colleagues [51] did not report their acceptance rates. The acceptance rate is of particular concern because we found that participants were younger and had been diagnosed for a longer period of time. The ability to generalize our findings to older couples may be compromised. Fourth, the sample was comprised of relatively well-educated couples who have been married or cohabitating a lengthy period of time and report high levels of marital satisfaction. In addition, the sample was primarily comprised of heterosexual couples. This sample does not allow any conclusions to be drawn about same-gender relationships. Whether our findings generalize to less well-educated couples in relationships of shorter duration and lower marital quality is not clear. Fifth, the sample exhibited relatively low levels of clinically-relevant distress. Whether our findings generalize to a more distressed sample of couples is not known. Finally, our measures of communication are self-report, which may not reflect actual communication behaviors and may be biased by personality features. However it is important to note that perceptions of one’s partner’s behaviors are likely key determinants of experienced closeness than observed behaviors.
Despite its limitations, this study had several strengths. First, unlike many studies of couples’ adjustment to prostate cancer (e.g., [52, 53]) we examined the role of relationship processes in both partner’s adjustment. Second, the role of constructive as well as unconstructive communication behaviors was examined. Third, analyses were conducted at the couple-level and showed that intimacy mediated the association between spousal communication and distress in a similar fashion for both patients and their partners. Fourth, unlike many studies of couples’ adaptation to prostate cancer, the role of patients’ physical symptomatology was included in the analyses.
Taken together, findings suggest that clinicians working with men diagnosed with prostate cancer should evaluate how both partners communicate about cancer concerns. Couple-focused interventions whose goal is to reduce psychological distress may benefit from enhancing relationship closeness. Specifically, couples’ interventions which facilitate constructive discussions about concerns, reducing the use of mutual avoidance, and facilitating greater responsiveness on the part of partners to patients in order to alleviate the demand-withdraw dynamic may all prove helpful. An intimacy-enhancing intervention which targets these specific relationship processes may prove beneficial. The fact that these associations remained even after accounting for the influence of global marital satisfaction suggests that, if intimacy and communication can be modified, clinicians can affect couples’ distress.
References
Balderson N, Towell T. The prevalence and predictors of psychological distress in men with prostate cancer who are seeking support. Br J Health Psychol. 2003;8:125–34.
Bisson JI, Chubb HL, Bennett S. The prevalence and predictors of psychological distress in patients with early localized prostate cancer. BJU International. 2002;90:56–61.
Cliff A, Macdonagh R. Psychosocial morbidity in prostate cancer: ll. A comparsion of patients and partners. BJU International. 2000;86:834–9.
Kornblith AB, Herr HW. Quality of life of patients with prostate cancer and their spouses. Cancer. 1994;73:2791–802.
Eton DT, Lepore SJ. Prostate cancer and health-related quality of life: a review of the literature. Psycho-Oncol. 2002;11(4):307–26.
Couper JW, Bloch S, Love A, Duchesne G, Macvean M, Kissane DW. The psychosocial impact of prostate cancer on patients and their partners. Med J Aust. 2006;185(8):428–32.
Street AF, Couper JW, Love AW, Bloch S, Kissane DW, Street BC. Psychosocial adaptation in female partners of men with prostate cancer. Eur J Cancer Care (Engl). 2009. Jul 20.
Badr H, Carmack Taylor CL. Sexual dysfunction and spousal communication in coupels coping with prostate cancer. Psych-Oncology. 2008. [Epub ahead of print].
Gray RE, Fitch M, Davis C, Phillips C. Interviews with men with prostate cancer about their self-help group experience. J Palliat Care. 1997;13(1):15–21.
Banthia R, Malcarne VL, Varni JW, Ko CM, Sadler GR, Greenbergs HL. The effects of dyadic strength and coping styles on psychological distress in couples faced with prostate cancer. J Behav Med. 2003;26(1):31–52.
Perez MA, Skinner EC, Meyerowitz BE. Sexuality and intimacy following radical prostatectomy: patient and partner perspectives. Health Psychol. 2002;21:288–93.
Boehmer U, Clark J. Communication about prostate cancer between men and their wives. J Fam Pract. 2001;50:226–31.
Garos S, Kluck A, Aronoff D. Prostate cancer patients and their partners: differences in satisfaction indices and psychological variables. (J Sex Marital Ther. 2007;4(5):1394–403. Epub 2007 Jul 18.
Lepore SJ, Helgeson VS. Social constraints, intrusive thoughts, and mental health after prostate cancer. J Soc Clin Psychol. 1998;17(1):89–106.
Kershaw TS, Mood DW, Newth G, Ronis DL, Sanda MG, Vaishampayan U, et al. Longitudinal analysis of a model to predict quality of life in prostate cancer patients and their spouses. Ann Behav Med. 2008;36(2):117–28.
Manne S, Badr H. Intimacy and relationship processes in couples' psychosocial adaptation to cancer. Cancer. 2008;112(S11):2541–55.
Manne SL, Ostroff J, Rini C, Fox K, Goldstein L, Grana G. The interpersonal process model of intimacy: the role of self-disclosure, partner disclosure and partner responsiveness in interactions between breast cancer patients and their partners. J Fam Psychol. 2004;18:589–99.
Porter L, Keefe F, Hurwitz H, Faber M. Disclosure between patients with gastrointestinal cancer and their spouses. Psycho-Oncol. 2005;14(12):1030–42.
Manne SL, Ostroff J, Norton T, Fox K, Goldstein L, Grana G. Cancer-related relationship communication in couples coping with early stage breast cancer. Psycho- Oncol. 2006;15(3):234–47.
Manne SL, Ostroff J, Winkel G, Grana G, Fox K. Partner unsupportive responses, avoidant coping, and distress among women with early stage breast cancer: patient and partner perspectives. Health Psychol. 2005;24(6):635–41.
Clark J, Bokhour B, Inui T, Silliman R, Talcott J. Measuring patient' perceptions of the outcomes of treatment for early prostate cancer. Med Care. 2003;41(8):923–36.
Lilleby W, Fossa SD, Waehre HR, Olsen DR. Long-term morbidity and quality of life in patients with localized prostate cancer undergoing definitive radiotherapy or radical prostatectomy. Int J Radiat Oncol Biol Phys. 1999;43(4):735–43.
Zubrod CG, Schneiderman M, Frei E, Brindley C, Gold G, Schnider B. Appriasal of methods for the study of chemotherapy of cancer in man: Comparative therapeutic trial of nitrogen mustard and triethylene thiophosphoramide. J Chronic Dis. 1960;11:17–33.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49(6):822–30.
Cappelleri JC, Rosen RC, Smith MD, Mishra A, Osterloh IH. Diagnostic evaluation of the erectile function domain of the international index of erectile function. Urology. 1999;54(2):346–51.
Litwin MS, Hays RD, Fink A, Ganz PA, Leake B, Brook RH. The UCLA prostate cancer index: development, reliability, and validity of a health-related quality of life measure. Med Care. 1998;36(7):1002–12.
Ishihara M, Suzuki H, Akakura K, Komiya A, Imamoto T, Tobe T, et al. Baseline health-related quality of life in the management of prostate cancer. Int J Urol. 2006;13(7):920–5.
Pistrang N, Barker C. The partner relationship in psychological response to breast cancer. Soc Sci Med. 1995;40:789–97.
Laurenceau JP, Barrett LF, Rovine M. The interpersonal process model of intimacy in marriage: a daily-diary and multilevel modeling approach. J Fam Psychol. 2005;19(2):314–23.
Christensen A, Sullaway M. Communication patterns questionnaire. Unpublished manuscript. Los Angeles: University of California; 1984.
Christensen A. Dysfunctional interaction patterns in couples. Perspectives on Marital Interaction. 1988;30–52.
Heavey CL, Layne C, Christensen A. Gender and conflict structure in marital interaction: a replication and extension. J Consult Clin Psychol. 1993;61(1):16–27.
Spanier GB, Filsinger EE. The dyadic adjustment scale. Marriage and family assessment: a sourcebood for family therapy. 1st ed. Beverly Hills: Sage; 1983. p. 155–68.
Schaefer MT, Olson DH. Assessing intimacy: the pair inventory. Journal of Marital and Family Therapy. 1981;47–60.
Talmadge L, Dabbs JM. Intimacy, conversational patterns, and concomitant cognitive/emotional processes in couples. J Soc Clin Psychol. 1990;9(4):473–88.
Derogatis L. BSI 18 administration, scoring and procedures manual. Minneapolis: NCS Pearson; 2001.
Kenny D, Kashy DA, Cook D. Dyadic data analysis. New York: Guilford; 2006.
Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Meth. 2002;7(4):422–45.
Srivastava S, McGonigal KM, Richards JM, Butler EA, Gross JJ. Optimism in close relationships: how seeing things in a positive light makes them so. J Pers Soc Psychol. 2006;91(1):143–53.
Kurdek LA. The allocation of household labor by partners in gay and lesbian couples. J Fam Issues. 2007;28(1):132–48.
Baron R, Kenny D. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82.
Kenny DA, Korchmaros JD, Bolger N. Lower level mediation in multilevel models. Psychol Meth. 2003;8(2):115–28.
Manne SL, Ostroff J, Sherman M, Heyman R, Ross S, Fox K. Couples' support-related communication, psychological distress and relationship satisfaction among women with early stage breast cancer. J Consult Clin Psychol. 2004;72(4):660–70.
Berg CA, Wiebe DJ, Butner J, Bloor L, Bradstreet C, Upchurch R, et al. Collaborative coping and daily mood in couples dealing with prostate cancer. Psychol Aging. 2008;23(3):505–16.
Manne SL, Alfieri T, Taylor K, Dougherty J. Preferences for spousal support among individuals with cancer. J Appl Soc Psychol. 1999;29(4):722–49.
Finch J, Zautra A. Testing latent longitudinal models of social ties and depression among the elderly: A comparison of distribution-free and maximum likelihood estimates with nonnormal data. Psychol Aging. 1992;7(1):107–18.
Manne SL, Zautra AJ. Spouse criticism and support: their association with coping and psychological adjustment among women with rheumatoid arthritis. J Pers Soc Psychol. 1989;56:608–17.
Rosenthal R. Advanced social psychology. In: Tesser A, editor. Methodology. Boston: McGraw-Hill; 1995.
Schmitt N. Uses and abuses of coefficient alpha. Psychol Assess. 1996;8(4):350–3.
Northouse LL, Mood DW, Schafenacker A, Montie JE, Sandler HM, Forman JD, et al. Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer. 2007;110(12):2809–18.
Canada AL, Neese LE, Sui D, Schover LR. Pilot intervention to enhance sexual rehabilitation for couples after treatment for localized prostate carcinoma. Cancer. 2005;104(12):2689–700.
Harden J, Northouse L, Cimprich B, Pohl JM, Liang J, Kershaw T. The influence of developmental life stage on quality of life in survivors of prostate cancer and their partners. J Cancer Surviv. 2008;2(2):84–94.
Kim Y, Kashy DA, Wellisch DK, Spillers RL, Kaw CK, Smith TG. Quality of life of couples dealing with cancer: dyadic and individual adjustment among breast and prostate cancer survivors and their spousal caregivers. Ann Behav Med. 2008;35(2):230–8.
Acknowledgements
This work was supported by an Established Investigator in Cancer Prevention and Control Award to Sharon Manne by the NCI (K05 CA109008), a Cancer Prevention and Control Career Development Award by the NCI (K07 CA124668) to Hoda Badr, a Memorial Sloan Kettering Society grant to David Kissane, and by a P30 CA006927 grant to Fox Chase Cancer Center. We would like to acknowledge the assistance of Drs. John Mulhall, Eric Horwitz, Richard Greenberg, David Chen, James Easton, Robert Uzzo, and Alan Pollack for allowing access to their patients for this study. Jennifer Burden, Megan Eisenberg, Kristen Sorice, and Sara Worhach collected study data. Maryann Krayger provided technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Manne, S., Badr, H., Zaider, T. et al. Cancer-related communication, relationship intimacy, and psychological distress among couples coping with localized prostate cancer. J Cancer Surviv 4, 74–85 (2010). https://doi.org/10.1007/s11764-009-0109-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-009-0109-y