Abstract
Background and Purpose
Although evidence suggests that survivors and spousal caregivers tend to experience somewhat similar levels of distress and that the survivor’s distress affects his/her own quality of life, the degree to which each person’s distress has an independent effect on their partner’s quality of life is unknown. Thus, this study aimed to examine the dyadic effects of psychological distress on the quality of life of couples dealing with cancer.
Methods
A total of 168 married survivor–caregiver dyads participating in the American Cancer Society’s Study of Cancer Survivors-I and Quality of Life Survey for Caregivers provided complete data for study variables. Participating survivors were diagnosed with either breast or prostate cancer approximately 2 years prior to participating in the study.
Results
Using the Actor Partner Interdependence Model, results revealed that although each person’s psychological distress is the strongest predictor of their own quality of life, partner’s distress and (dis)similarity in distress of the couple also play significant roles in one’s quality of life. In addition, the adverse effect of having a partner who is less emotionally resourceful was especially pronounced on men’s physical health.
Conclusions
Our systematic investigation provided valuable evidence for identifying the subgroup of cancer survivors and their spouses who are vulnerable to poor quality of life due to their mutual psychological distress. These findings suggest that couples may benefit from interventions that enhance their ability to manage psychological distress, particularly the wife’s, which may improve the mental and physical health of both partners when they are dealing with cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An estimated 1.4 million individuals in the United States were diagnosed with cancer in 2007 [1], with a similar number of family members expected to provide care or support. Cancer imposes challenges not only on the individual diagnosed with cancer, but also on their family members. The challenges associated with providing care to cancer survivors may weigh most heavily on their spouses, as they are typically the primary caregivers to adult patients [2, 3].
Although research findings on the level of psychological distress experienced by spousal caregivers compared with patients have been inconsistent [4, 5], it is the general consensus that cancer diagnosis and treatment are highly distressing events both to patients and their family members. Indeed, approximately 25% of cancer survivors remain highly distressed years after the initial diagnosis [6, 7], and one study found that 13% of caregivers of advanced cancer patients met the criteria for a psychiatric disorder [8].
Two recent reviews examining the relationship between the cancer patient’s psychological distress and their caregiver’s distress suggest that patients’ and their caregivers’ levels of psychological distress are related [5, 9]. In a meta-analysis of 21 studies, Hodges and colleagues [5] found that the overall effect size of correlation between patient distress and caregiver’s was 0.35. Both patients and their husbands facing breast cancer, compared with couples dealing with benign breast disease, reported similar levels of higher emotional distress and more distress within the marriage [10]. The significant similarity in psychological distress between cancer patients and their spouses implies dyadic mutuality, with one partner’s distress spilling over to the other [5, 11].
Although the evidence suggests that survivors and caregivers tend to experience similar levels of distress, the similarity coefficient is only modest in size, implying that there may be considerable divergence in distress scores for some survivors and caregivers. If there is dissimilarity in levels of distress, then, because survivors and caregivers are part of an interdependent system, important questions to be asked are whether a person’s distress and his/her partner’s distress have independent effects on each person’s quality of life, and whether the two partners’ levels of distress have interactive effects on each person’s quality of life.
More specifically, our question concerns the extent to which similarity or dissimilarity in psychological distress impacts the survivor’s and caregiver’s quality of life. This is an important gap in our knowledge of how cancer impacts both survivors and caregivers for at least two reasons. First, individuals diagnosed with cancer often do not adjust to their cancer alone but share the concerns brought up by the cancer with their families. Accumulating evidence has shown that the involvement of a spouse or significant other in the journey of adjusting to cancer has a salutary effect on the survivor’s quality of life [12, 13]. Because the existing studies yield mixed reports, however, it remains unclear whether such effects also hold true for the caregivers [14, 15].
Second, although psychological distress is known to be a significant negative factor in an individual’s quality of life [16], the effects of a partner’s distress on a person’s quality of life, particularly in the context of cancer, is less obvious. Moreover, the substantial difference in roles for the survivors and their caregivers adds to the question’s complexity: Is it better for survivors to have caregivers who are less distressed than they are or is it better for caregivers to have survivors who are less distressed?
These questions require that we examine how psychological adjustment of both cancer survivors and their caregivers relates to each person’s quality of life. Kenny and his colleagues [17] have referred to the effect of a person’s own characteristics (e.g., psychological distress) on that same person’s outcomes (e.g., quality of life) as an actor effect. In contrast, a partner effect occurs when a person’s characteristics affect his or her partner’s outcomes. Beyond these two “main effects,” Kenny et al. suggest that actor and partner effects may interact, and they propose that one way to frame such an interaction is as a similarity (or dissimilarity) variable. Within the type of interdependent relationship that occurs between survivors and caregivers, dissimilarity in psychological distress might play as a moderator of the relation between one’s psychological distress and quality of life outcomes. For example, when one person is highly distressed and the other person is not (i.e., the two are dissimilar), the dissimilarity in distress might provide a buffering effect such that individuals have better quality of life. Furthermore, the degree to which dissimilarity acts as a moderator may depend on which person’s quality of life is at issue: the survivor or the caregiver.
Cancer care involves a variety of tasks to meet the patients’ needs [18]. Managing the emotional stress of the survivor in addition to managing their own distress has been identified by caregivers as the most difficult task [19], which has been true not only around the time of diagnosis and treatment but also across various phases in the illness trajectory [14, 18, 20]. As a primary support resource for the survivor [20–22], the caregiver’s heightened level of psychological distress may lead to the caregiver being less resourceful, which may interfere with carrying out the expected role of providing emotional support to the survivor. Therefore, we hypothesized that spousal caregivers being more distressed than the cancer survivors they care for would have a greater adverse effect not only on their own quality of life, but also the survivors’.
Past research has shown that a number of other factors beyond psychological distress have a significant impact on quality of life within the cancer context. For example, Gilbar [23] and Given et al. [24] have shown that age affects quality of life, and Hagedoorn et al. [25] demonstrated that a person’s role (i.e., patient or caregiver) impacts quality of life, with patients tending to have lower quality of life than do caregivers. Other cancer-specific factors that have been shown to affect quality of life include stage of cancer [26] and type of cancer [27]. Therefore, in our analyses examining the unique effects of distress (dis)similarity on quality of life, these factors are included as covariates.
In sum, this study investigates the effect of (dis)similarity in psychological distress between cancer survivors and their spousal caregivers on each person’s quality of life as measured by mental and physical health. We attempt to fill in gaps and expand the literature by examining the unique effects of dyad-level predictor variables (i.e., cancer type, stage of cancer, and the extent to which levels of psychological distress are dissimilar between cancer survivors and their spouse) and individual-level predictor variables (i.e., the person’s psychological distress and the partner’s psychological distress, patient vs. caregiver role, and age) on mental and physical health outcomes for survivors and their caregivers. Systematic investigation of this question has the potential to provide valuable evidence for identifying the subgroup of cancer survivors and their spouses who are vulnerable to poor quality of life due to their mutual psychological distress. It will further guide the development of tailored interventions to enhance their quality of life.
Method
Participants and Procedure
The American Cancer Society’s Study of Cancer Survivors-I (SCS-I) was developed to assess the quality of life of cancer survivors [28]. Survivors participating in SCS-I were identified by state cancer registries and met the following eligibility criteria: (a) 18 years or older at diagnosis, (b) diagnosed with one of the 10 most highly incident cancers (bladder, breast, colorectal, kidney, lung, non-Hodgkin lymphoma, ovarian, prostate, skin melanoma, or uterine), (c) fluent in either English or Spanish, and (d) a resident of the United States. SCS-I participants nominated individuals in family-like relationships who consistently provided help to them during their cancer experience. These nominated caregivers were invited to participate in the American Cancer Society’s Quality of Life Survey for Caregivers, which was designed to assess the impact of cancer on the quality of life of family members and close friends who care for cancer survivors. Eligibility criteria for the caregiver study were age 18 years and older, able to speak/read English or Spanish, and residing in the United States. Data reported here are from the first cohort of the initial data collection of the Quality of Life Survey for Caregivers and their matched survivors.
A total of 739 caregivers completed the initial caregiver survey (66.7% response rate). The 316 care recipients of those caregivers were diagnosed with either breast or prostate cancer. Two survivors diagnosed with distant cancer were excluded. Of the remaining 314 dyads, 218 were spousal pairs, of which 168 dyads provided complete data for the study variables and were included in the analyses. Participants with incomplete data did not differ in available study variables from those providing complete information (ps > 0.24). Demographic and medical characteristics of participants are reported in Table 1. The cancer had been diagnosed an average of 2.15 years (SD = 0.4 year) before the participants completed the survey.
Measures
Psychological Distress
Psychological distress of each participant was assessed using the 37-item Profile of Mood States-Short Form (POMS-SF; 1 = not at all, 5 = extremely; 29). Each subscale score was calculated by averaging relevant items for each subscale. A psychological distress composite score was then calculated by summing the subscale scores of anger, anxiety, confusion, depression, and fatigue items, and subtracting the vigor subscale score from the sum. Thus, higher scores on this composite reflect a greater level of psychological distress. The psychological distress composite score had good internal consistency (αs = .91 for both survivors and caregivers).
(Dis)similarity in Psychological Distress
The extent to which a survivor and his/her spousal caregiver were (dis)similar in levels of global psychological distress was calculated by subtracting survivor’s psychological composite score measured by the POMS-SF from their caregiver’s psychological composite score, also measured by POMS-SF. To avoid multicollinearity with each person’s psychological distress score, the difference score was then converted to an absolute difference score. Higher scores on the (dis)similarity in psychological distress reflected greater discrepancy in the levels of psychological distress within the couple.
Age
Self-reported age of the participants was used in the analyses.
Cancer Type and Stage
Information about cancer type (breast or prostate) and stage of cancer (localized or regional) was obtained from the state cancer registry, and cancer stage was coded as 0 for localized and 1 for regional.
Quality of Life
Self-reported levels of mental and physical health of participants were measured using the Medical Outcomes Study 36-Item Short Form Health Survey (MOS SF-36; 30). The mental functioning score was a composite of weighted vitality, social functioning, role-emotional, and mental health subscale scores. The physical functioning score was a composite of weighted physical functioning, role-physical, bodily pain, and general health subscale scores. Higher composite scores reflected better mental and physical health.
Analytic Strategies
Mean differences between survivors and caregivers on psychological distress and quality of life (i.e., mental and physical health) were tested using paired t tests, and the degree to which spouses were similar on these factors was estimated and tested using Pearson zero-order correlation coefficients. Each of these analyses was conducted separately for the two types of cancer included in this research (i.e., breast and prostate cancer).
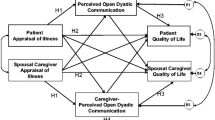
The Actor Partner Interdependence Model (APIM; 17) served as the general data analytic strategy to address the central questions in this study. The model parameters were estimated using structural equation modeling (SEM) with manifest variables (AMOS 6.0; 31). The survivor’s psychological distress score, caregiver’s psychological distress score, and (dis)similarity in psychological distress scores within the couple were exogenous variables, and mental health and physical health scores of survivors and caregivers were endogenous variables. Individual’s age and stage of cancer (localized vs. regional) served as covariates (see Fig. 1). Measurement errors between survivor’s psychological distress score, caregiver’s psychological distress score, and (dis)similarity in psychological distress score; between survivor’s mental health and physical health scores; between caregiver’s mental health and physical health scores; and survivor’s age and caregiver’s age were allowed to be correlated with each other.
Actor and partner effects of psychological distress predicting each individual’s QOL. * p < 0.05; ** p < 0.01; *** p < 0.001. Significant standardized coefficients for breast cancer and for prostate cancer (in parentheses); solid lines are for significant paths of both breast cancer and prostate cancer cases; broken lines are for significant paths of either breast cancer or prostate cancer cases; Stage of cancer: 0 for localized, 1 for regional cancer
We found that the assumption of multivariate normality was violated in the data. Thus, we implemented the Bollen-Stine (BS) bootstrap method [32] for correcting chi-square values. Three model-fit indices are reported: the goodness of fit index (GFI), the confirmatory fit index (CFI), and the root mean squared error of approximation (RMSEA). For the GFI, values of >0.90 [33], for the CFI, values of >0.95, and for the RMSEA measure, values of <0.06 [34] reflect adequate fit of a specified model to the data. The study model was compared for breast cancer and prostate cancer.
Results
As shown in Table 1, the sample consisted of similar numbers of couples in which the survivor had breast or prostate cancer. The participants were predominantly middle-aged, Caucasian, relatively educated, and affluent. Results comparing survivor and caregiver means (shown in Table 2) revealed no significant differences between survivors and caregivers in psychological distress (i.e., total mood disturbance score of POMS-SF) or quality of life indicators (i.e., MOS SF-36 mental health composite score and physical health composite score), with one exception. The exception, which was not expected, was that prostate cancer survivors, on average, reported better physical health than their caregivers.
Table 2 also presents the dyadic correlations for survivors and caregivers. Psychological distress was moderately correlated for both types of cancer dyads. Thus, there was evidence that across the two types of cancer, partners were at least moderately similar in their levels of psychological distress. On the other hand, the dyadic correlations for spouses’ mental health and physical health scores were significantly different from zero only for prostate cancer dyads. Tests of whether these correlations differed across cancer type indicated that the correlations for mental health did not differ significantly, z = 1.57, p = 0.12, but that they were different for physical health, z = 1.94, p = 0.05. This indicates that there was more similarity in physical health for couples in which the husband had prostate cancer than for couples in which the wife had breast cancer.
The SEM model implied by the APIM is one in which each person’s outcomes (i.e., the survivor’s and caregiver’s physical and mental health), are each predicted to be a function of each person’s distress as well as the absolute difference between the two partners’ distress. The model also included the person’s age and the survivor’s cancer stage as covariates. Thus, the actor effect of distress for the survivor was the degree to which the survivor’s distress predicted that survivor’s quality of life (i.e., mental and physical health), and the partner effect for the survivor was the degree to which the caregiver’s distress predicted the survivor’s quality of life. In a parallel fashion, the actor effect for the caregiver was the degree to which the caregiver’s distress predicted his or her quality of life, and the partner effect for the caregiver was the degree to which the survivor’s distress predicted the caregiver’s quality of life. In addition to the actor and partner effects, the model predicting each person’s quality of life included the dissimilarity-in-distress variable, as well as the person’s age and cancer stage.
Table 3 presents the parameter estimates for this model. A multiple-groups test was conducted to determine the degree to which the model was an adequate representation for both breast cancer and prostate cancer dyads. The fit of the unconstrained model was satisfactory: multivariate kurtosis = 23.01, p < 0.001 for breast cancer dyads; multivariate kurtosis = 25.05, p < .001 for prostate cancer dyads, χ 2 (38) = 43.83, BS p = 0.29; GFI = 0.953; CFI = 0.993; and RMSEA = 0.030. The fit of the constrained model between the two types of cancer was worse than that of the unconstrained model, however: χ 2 diff = 65.51 with degree of freedom = 36, p < 0.01. This indicated that the relations among variables were not comparable for the two cancer groups, so the two types of cancer were examined separately.
Psychological Distress and Mental Health
Examination of individual-level effects (each person’s psychological distress and age: Table 3) indicates evidence of actor effects for both patients and caregivers such that the level of a person’s psychological distress was strongly related to his or her own mental health, and these strong actor effects occurred for both breast cancer and prostate cancer couples. There was no evidence of partner effects for either survivors or caregivers, and this was true for both cancer types. In other words, for either breast cancer or prostate cancer couples, a person’s level of psychological distress had no independent effect on his or her partner’s mental health. In addition, the person’s age significantly related to mental functioning score only for prostate cancer survivors: older prostate cancer survivors reported better mental health.
Beyond these individual-level effects, at the dyadic level a greater dissimilarity in psychological distress was only associated with poorer mental health of wife caregivers of prostate cancer survivors. In other words, over and above the effects of each person’s distress, when there was a greater difference in psychological distress between the couple, wife caregivers reported poorer mental health. Stage of cancer was not related to the mental health of either survivors or caregivers.
Psychological Distress and Physical Health
As was the case with mental health, actor effects for both survivors and caregivers emerged such that more psychologically distressed individuals had poorer physical health (see Table 3). In addition, there was evidence of partner effects for both types of cancer. In the breast cancer group, the survivor’s distress predicted the caregiver’s physical health, and in the prostate cancer group, the caregiver’s distress predicted the survivor’s physical health. Although these two partner effects may seem disparate, they are actually very similar in that they both show that the woman’s psychological distress (as either survivors or caregivers) was negatively related to her husband’s physical health. There was also evidence that the person’s age negatively related to his or her physical health, with the exception of breast cancer survivors.
At the dyadic level, for men, a greater dissimilarity in psychological distress was associated with better physical health. That is, over and above the effects of each person’s distress on physical health, when there was a greater difference in psychological distress between the couple, both husband caregivers of breast cancer survivors and husband prostate cancer survivors reported better physical health. Finally, the cancer stage of prostate cancer survivors related to their physical health. Prostate cancer survivors diagnosed with localized cancer reported better physical health than those diagnosed with regional cancer.
Discussion
The goal of this study was to examine the effects of psychological distress on the quality of life of couples dealing with cancer. Our findings demonstrate that although each person’s psychological distress is the strongest predictor of their own quality of life, the partner’s distress, and the (dis)similarity in distress of the couple also play significant roles in one’s quality of life.
The overall levels of psychological distress that we observed in both spousal caregivers and survivors were lower than those found in patients who have undergone bone marrow transplant [35] or in cancer patients with pain complaints [29]. The levels of psychological distress of our sample more closely resemble those of a normative geriatric sample [36]. Similarly, the mental and physical functioning scores of our sample were comparable to the U.S. population norms [30]. Thus, our study participants appear to have passed the initial period of crisis of cancer diagnosis and treatment and now, at 2 years postdiagnosis, display normal levels of psychological well-being and quality of life.
With regard to the effects of psychological distress on the quality of life, three findings deserve further discussion. First, cancer survivors and their spousal caregivers reported similar levels of psychological distress and quality of life. Our findings of the similarity in psychological distress between spouses and the magnitude of the similarity are consistent with those found in a meta-analytic study by Hodges and colleagues [5]. They concluded that psychological distress between survivors and their caregivers appears to be congruent across different time points in the earlier survivorship phase, with the exception of around the time of diagnosis and near the end of treatment. Our finding adds support to the literature that married couples experience similar levels of psychological distress beyond the earlier phase of the illness trajectory, approximately 2 years postdiagnosis.
Second, although the size of the (dis)similarity in psychological distress of couples was moderate, (dis)similarity in psychological distress was a significant predictor of quality of life in a distinctive way. Specifically, dissimilarity in psychological distress had an adverse influence on the mental health of wife caregivers of prostate cancer survivors, whereas it was beneficial for the physical health of husband caregivers of breast cancer survivors. Women may perceive lack of emotional mutuality or reciprocity [37, 38] with an ill spouse as the result of emotional abandonment and their own deficiencies in interpersonal sensitivity, which leads to feelings of isolation and social inadequacy, and thus poorer mental health [39, 40]. This was not the case for male caregivers. One may speculate that male caregivers who are emotionally disconnected from their ill spouses are not only less likely to suffer from the emotional abandonment, but also more likely to have their time and energy freed up, which may result in better physical functioning.
Third, there was evidence of partner effects, at least for women. That is, women’s distress predicted men’s physical health, over and above the men’s distress, couple (dis)similarity in distress, survivor’s age, and cancer stage. This partner effect on men’s physical health occurred regardless of whether the man was the survivor or the caregiver. It is noteworthy that the adverse effect of having a partner who is less emotionally resourceful is limited to men’s physical health, but not vice versa, or when the male partner distanced himself psychologically. Our finding on the unequal influence of gender on the partner’s distress is consistent with findings in some studies [27, 41], although other studies have found no gender differences [42, 43], and the effects of social support on physical health have not been consistent [44, 45].
Together, our findings suggest that when a couple is dealing with a major illness such as cancer, the extent to which women psychologically adjust to the situation plays a key role not only in their own well-being [46, 47] but also their spouse’s. This finding implies that both cancer survivors and their partners should be included in psychosocial programs [13]. It also suggests that helping women adjust better to their own or their husband’s cancer would benefit both partners.
Limitations and Directions for Future Studies
Several limitations of our study should be noted. First, the findings are based on cross-sectional analyses, which clearly preclude definitive causal interpretations. We plan to address these concerns with follow-up data on this sample. Second, all variables included in this study were self-reported and therefore may not reflect objective distress and health status. Future studies should include behavioral and physiological indicators of distress and quality of life as well as survivors’ comorbid conditions. Third, we compared breast cancer survivors and their husband caregivers with prostate cancer survivors and their wife caregivers. Thus, although our findings on the disproportionate effects of women’s psychological distress on men’s quality of life are intriguing, these findings need to be replicated. In particular, it is necessary to replicate the current findings with types of cancer that are not gender-specific, such as colorectal or lung cancer. Finally, generalizability of the findings is limited to caregivers who are Caucasian, relatively educated, and relatively affluent. Future studies are needed with ethnic minorities and individuals of lower socioeconomic status.
Conclusions
Notwithstanding these limitations, the findings add significant information to a growing body of research on the quality of life of cancer survivors and their family caregivers. Our findings support the widely accepted concept that cancer impacts not only the person diagnosed with the disease but also their family. Our investigation of the effects of psychological distress on the quality of life of couples provides valuable evidence for identifying the subgroup of cancer survivors and their spouses who are vulnerable to poor quality of life due to their mutual psychological distress. These findings suggest that couples may benefit from interventions that enhance their ability to manage psychological distress, particularly women’s, which may improve the mental and physical health of both partners when they are dealing with cancer.
References
American Cancer Society. Cancer Facts and Figures, 2006. Atlanta, GA: American Cancer Society; 2007.
Hughes SL, Giobbie-Hurder A, Weaver FM, et al. Relationship between caregiver burden and health-related quality of life. Gerontologist. 1999; 39: 534–545.
Nijboer C, Triemstra M, Tempelaar R, et al. Patterns of caregiver experiences among partners of cancer patients. Gerontologist. 2000; 40: 738–746.
Baider L, Cooper C, De-Nour AK. Cancer and the Family. 2nd ed. New York: Wiley; 2000.
Hodges LJ, Humphris GM, Macfarlane G. A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Soc Sci Med. 2005; 60: 1–12.
Nordin K, Berglund G, Glimelius B, et al. Predicting anxiety and depression among cancer patients: a clinical model. Eur J Cancer. 2001; 37: 376–384.
Roth A, Kornblith AB, Batel-Copel L, et al. Rapid screening for psychologic distress in men with prostate carcinoma: a pilot study. Cancer. 1998; 82: 1904–1908.
Vanderwerker LC, Laff RE, Kadan-Lottick NS, et al. Psychiatric disorders and mental health service use among caregivers of advanced cancer patients. J Clin Oncol. 2005; 23: 6899–6907.
Pitceathly C, Maguire P. The psychological impact of cancer on patients’ partners and other key relatives: a review. Eur J Cancer. 2003; 39: 1517–1524.
Northouse LL, Templin T, Mood D, et al. Couples’ adjustment to breast cancer and benign breast disease: a longitudinal analysis 18. Psycho-Oncol. 1998; 7: 37–48.
Manne SL. Cancer in the marital context: a review of the literature. Cancer Investig. 1998; 16: 188–202.
Manne SL. Coping and social support. In: Nezu AM, Nezu CM, Geller PA, eds. Handbook of Psychology: Health Psychology, vol. 9. Hoboken, NJ: John Wiley & Sons, Inc; 2003: 51–74.
Nezu AM, Nezu CM, Felgoise SH, et al. Project Genesis: assessing the efficacy of problem-solving therapy for distressed adult cancer patients. J Consult Clin Psychol. 2003; 71: 1036–1048.
Nijboer C, Triemstra M, Tempelaar R, et al. Determinants of caregiving experiences and mental health of partners of cancer patients. Cancer. 1999; 86: 577–588.
Kim Y, Schulz R, Carver CS. Benefit-finding in the cancer caregiving experience. Psychosom Med. 2007; 69: 283–291.
Holland JC, Reznick I. Pathways for psychosocial care of cancer survivors. Cancer. 2005; 104: 2624–2637.
Kenny DA, Kashy DA, Cook WL. Dyadic Data Analysis. New York, NY: Guilford Press; 2006.
Given BA, Given CW, Kozachik S. Family support in advanced cancer. Ca. 2001; 51: 213–231.
Kim Y, Schulz R. Family caregivers’ strains: Comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. Journal of Aging and Health. 2007 (in press).
Hagedoorn M, Kuijer RG, Buunk BP, et al. Marital satisfaction in patients with cancer: does support from intimate partners benefit those who need it the most? Health Psychol. 2000; 19: 274–282.
Brown SL, Nesse RM, Vinokur AD, et al. Providing social support may be more beneficial than receiving it: results from a prospective study of mortality. Psychol Sci. 2003; 14: 320–327.
Manne SL, Ostroff J, Sherman M, et al. Buffering effects of family and friend support on associations between partner unsupportive behaviors and coping among women with breast cancer. J Soc Pers Relatsh. 2003; 20: 771–792.
Gilbar O. Gender as a predictor of burden and psychological distress of elderly husbands and wives of cancer patients. Psycho-Oncol. 1999; 8: 287–294.
Given B, Wyatt G, Given C, et al. Burden and depression among caregivers of patients with cancer at the end of life. Oncol Nurs Forum. 2004; 31: 1105–1117.
Hagedoorn M, Buunk BP, Kuijer RG, et al. Couples dealing with cancer: role and gender differences regarding psychological distress and quality of life. Psycho-Oncol. 2000; 9: 232–242.
Foxall MJ, Gaston-Johansson F. Burden and health outcomes of family caregivers of hospitalized bone marrow transplant patients. J Adv Nurs. 1996; 24: 915–923.
Baider L, Ever-Hadani P, Goldzweig G, et al. Is perceived family support a relevant variable in psychological distress? A sample of prostate and breast cancer couples. J Psychosom Res. 2003; 55: 453–460.
Smith T, Stein KD, Mehta CC, et al. The rationale, design, and implementation of the American Cancer Society's studies of cancer survivors. Cancer. 2007; 109: 1–12.
Shacham S. A shortened version of the Profile of Mood States. J Pers Assess. 1983; 47: 305–306.
Ware JE Jr., Kosinski M, Keller S. SF-36 Physical and Mental Health Summary Scales: A User's Manual. 2nd ed. Boston, MA: Health Institute, New England Medical Center; 1994.
Arbuckle JL, Wothke W. Amos Users’ Guide, Version 6.0. Chicago: SmallWaters Corporation; 2005.
Bollen KA, Stine RA. Bootstrapping goodness-of-fit measures in structural equation models. In: Bollen KA, Long JS, eds. Testing Structural Equation Models. Newbury Park, CA: Sage; 1993: 111–135.
Jöreskog KG, Sörbom D. LISREL VI User's Guide. (3rd). Mooresville, IL: Scientific Software; 1984.
Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999; 6: 1–55.
Baker F, Denniston M, Zabora J, et al. A POMS short form for cancer patients: psychometric and structural evaluation. Psycho-Oncol. 2002; 11: 273–281.
McNair DM, Neuchert JWP. Profile of Mood States: Technical Updates. Multi-Health Systems, Inc., 2005.
Coyne JC, Smith DA. Couples coping with a myocardial infarction: a contextual perspective on wives’ distress. J Pers Soc Psychol. 1991; 61: 404–412.
Hooker K, Manoogian-O'Dell M, Monahan DJ, et al. Does type of disease matter? Gender differences among Alzheimer's and Parkinson's disease spouse caregivers. Gerontologist. 2000; 40: 568–573.
Miller B, Cafasso L. Gender differences in caregiving: fact or artifact. Gerontologist. 1992; 32: 498–507.
Yee JL, Schulz R. Gender differences in psychiatric morbidity among family caregivers: a review and analysis. Gerontologist. 2000; 40: 147–164.
Kiecolt-Glaser JK, Newton T, Cacioppo JT, et al. Marital conflict and endocrine function: are men really more physiologically affected than women? J Consult Clin Psychol. 1996; 64: 324–332.
Baider L, Koch U, Esacson R, et al. Prospective study of cancer patients and their spouses: the weakness of marital strength. Psycho-Oncol. 1998; 7: 49–56.
Burman B, Margolin G. Analysis of the association between marital relationships and health problems: an interactional perspective. Psychol Bull. 1992; 112: 39–63.
Kiecolt-Glaser JK, Newton TL. Marriage and health: his and hers. Psychol Bull. 2001; 127: 472–503.
Shumaker SA, Hill DR. Gender differences in social support and physical health. Health Psychol. 1991; 10: 102–111.
Andrykowski MA, Manne SL. Are psychological interventions effective and accepted by cancer patients? I. Standards and levels of evidence. Annals Behav Med. 2006; 32: 93–97.
Antoni MH, Lechner SC, Kazi A, et al. How stress management improves quality of life after treatment for breast cancer. J Consult Clin Psychol. 2006; 74: 1143–1152.
Acknowledgment
This study was funded by the American Cancer Society National Home Office, intramural research. We wish to extend our appreciation to Dr. Charles Carver for thoughtful comments; to Dr. Corinne Crammer for editorial assistance; and to all the families who participated in this investigation. The first author dedicates this research to the memory of Heekyoung Kim.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kim, Y., Kashy, D.A., Wellisch, D.K. et al. Quality of Life of Couples Dealing with Cancer: Dyadic and Individual Adjustment among Breast and Prostate Cancer Survivors and Their Spousal Caregivers. ann. behav. med. 35, 230–238 (2008). https://doi.org/10.1007/s12160-008-9026-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-008-9026-y