Abstract
The combined index of hemoglobin, albumin, lymphocyte, and platelet (HALP) is a novel indicator reflecting systemic inflammation and nutritional status. To explore the relationship between HALP score and ICU mortality risk in patients with acute exacerbations of chronic obstructive pulmonary disease (AECOPD). A total of 1533 AECOPD patients from the eICU Collaborative Research Database (eICU-CRD) between 2014 and 2015 were included in this retrospective cohort study. Univariate and multivariate Cox proportional hazards models were utilized to investigate the association of HALP score, platelet-to-lymphocyte ratio (PLR) score, and lymphocyte-to-monocyte ratio (LMR) score with the ICU mortality risk in patients with AECOPD. Stratified analyses were performed based on patients’ ICU admission type, body mass index (BMI), and Acute Physiology, Age and Chronic Health Evaluation IV (APACHE IV) score. Of these 1533 AECOPD patients, 123 (8.00%) patients died in the ICU. Low HALP score [hazard ratio (HR) = 1.69; 95% confidence interval (CI) 1.14–2.53] and low LMR score (HR = 1.60; 95% CI 1.07–2.39) were associated with an increased ICU mortality risk in patients with AECOPD after adjusting for all confounders. Stratified analyses indicated that low HALP score were still associated with a higher ICU mortality risk in patients admitted to ICU by emergency (HR = 1.81; 95% CI 1.11–2.96), obese patients (HR = 2.81; 95% CI 1.29–6.10), and patients with low APACHE scores (HR = 2.87; 95% CI 1.75–4.69). Low HALP score was associated with an increased risk of ICU mortality in patients with AECOPD, suggesting that the HALP score may be a novel prognostic predictor in patients with AECOPD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is a respiratory disease characterized by persistent respiratory symptoms and airflow limitation, and is closely related to airways, lung tissue, and systemic inflammatory responses [1]. COPD is the third leading cause of death worldwide, with approximately 3 million deaths each year [2]. Acute exacerbations of COPD (AECOPD) are the leading cause of hospitalization and death in COPD patients [3, 4]. Considering the poor prognosis of patients with AECOPD, early and accurate assessment of individual mortality risk during acute exacerbation is critical for clinical management.
AECOPD is associated with increased airway and systemic inflammatory responses [4]. Previous studies have shown that inflammatory markers such as neutrophils and lymphocytes in peripheral blood are associated with the prognosis of COPD patients [5,6,7]. Inflammatory markers based on blood cell levels, such as the neutrophil to lymphocyte ratio (NLR) [8], the platelet to lymphocyte ratio (PLR) [9], and the lymphocyte to monocyte ratio (LMR) [10], have been used to predict the prognosis of patients with COPD. However, nutritional status also plays an important role in the prognosis of COPD patients [11, 12], and the above-mentioned inflammatory indicators cannot reflect the nutritional status of patients. Malnutrition is a common and underestimated problem in COPD patients. As the disease progresses, factors such as tissue hypoxia, metabolic and intake imbalances, systemic inflammatory response, oxidative stress, and drug side effects lead to widespread nutritional problems in COPD patients [13], and the degree of airflow limitation is closely related to malnutrition [14]. A novel index, hemoglobin, albumin, lymphocyte, and platelet (HALP), was proposed to reflect the inflammatory and nutritional status of patients. Several studies have demonstrated that the HALP score was associated with survival in patients with esophageal squamous cell carcinoma [15], prostate cancer [16], acute ischemic stroke [17], and pancreatic cancer [18]. However, studies on the relationship between HALP score and survival in AECOPD patients have not been reported. Thus, we aimed to investigate the prognostic value of HALP score in patients with AECOPD based on a multicenter database.
Methods
Data source and study participants
Data for this retrospective cohort study were extracted from the eICU Collaborative Research Database (eICU-CRD) (https://eicu-crd.mit.edu/gettingstarted/overview/) between 2014 and 2015. The eICU-CRD is a public multicenter intensive care unit (ICU) database. To obtain permission to access the database, the author had taken a series of courses offered by the National Institutes of Health (NIH) and obtained authorization to access the eICU-CRD database after passing the necessary assessments. The eICU-CRD used stratified random sampling to select patients and contained 200,859 patient unit encounters for 139,367 unique patients admitted to 208 hospitals in the United States between 2014 and 2015. Data collected in the database includes vital signs, laboratory measurements, medications, Acute Physiology, Age, and Chronic Health Evaluation IV (APACHE IV) components, care plan information, admission diagnosis, patient history, time-stamped diagnoses from a structured problem list, and similarly chosen treatments [19]. Identification of patients with AECOPD in eICU-CRD was based on the International Classification of Diseases, Ninth and Ten Revision (ICD-9, ICD-10) codes (ICD-9:49,121, ICD-10: J441). The inclusion criteria were as follows: (1) patients aged ≥ 18 years; (2) patients who were diagnosed with AECOPD at ICU admission; (3) patients with ICU stay of at least 24 h. The exclusion criteria were as follows: (1) patients with missing key data, such as hemoglobin, albumin, lymphocytes, platelet, etc.; (2) patients with missing survival information; (3) patients with abnormal data, such as height ≤ 128 cm, lymphocytes ≤ 0, and APACHE score ≤ 0, etc. Protocols of eICU-CRD were approved by the Institutional Review Board (IRB) of the Massachusetts Institute of Technology and informed consent was obtained from patients or their families.
Outcomes
The primary outcome of this study was patient death within the ICU or discharge. The eICU-CRD only records the data of each patient per admission to the ICU, and there is no follow-up interval. For patients with multiple hospital admissions records, data were only collected for their first ICU admission.
Data collection
The demographics, vital signs, patient history, and laboratory measurements data of patients were collected including age, sex (male and female), ethnicity (African-American, Asian, Caucasian, Hispanic, Native American, and others), type of ICU admission (emergency and non-emergency), body mass index (BMI) (underweight, normal, overweight, and obesity), coronary artery disease (yes and no), congestive heart failure (yes and no), atrial fibrillation (yes and no), vasopressor (yes and no), heart rate, respiratory rate, saturation of peripheral oxygen (SPO2), systolic blood pressure (SBP), diastolic blood pressure (DBP), body temperature, partial pressure of oxygen (PO2), pH, eosinophils, coefficient of variation of red cell volume distribution width (RDW-CV), bilirubin, creatinine, blood urea nitrogen (BUN), glucose, bicarbonate, sodium, potassium, chloride, hemoglobin, albumin, lymphocyte, platelet, monocyte, APACHE score, and survival time.
Definition
HALP score was calculated as hemoglobin level (g/L) × albumin level (g/L) × lymphocyte count (/L)/platelet count (/L) [18]. PLR score was determined by platelet count (/L)/lymphocyte count (/L). LMR score was calculated as lymphocyte count (/L)/ monocyte count (/L). The HALP, PLR, and LMR scores were divided into high and low groups according to their cut-off values, respectively. Cut-off values for HALP, PLR, LMR, and APACHE scores were calculated with the surv_cutpoint function, which is one of the functions in the survminer package of the R software. The cut-off value with the smallest P value calculated from the log-rank test for survival was determined as the optimal cut-off value. Cut-off values for HALP, PLR, LMR, and APACHE scores were 9.086, 329.412, 0.75 and 81, respectively (Supplement Fig. 1).
Missing data
Variables with more than 20% missing values were excluded. Variables with less than 20% missing values were imputed using multiple imputation and all missing data were filled with Monte Carlo method. Sensitively analysis was performed between the data before and after imputation, and the results indicated that there was no statistically significant difference before and after data imputation (Supplement Table. 1).
Statistical analysis
Continuous variables with normal distribution were described as mean ± standard deviation (SD), and Student’s t test was used for comparison between groups. Continuous variables with skewed distribution were expressed as median and interquartile ranges [M (Q1, Q3)], and Wilcoxon rank-sum test was utilized for comparison between groups. Categorical variables were described as number and percentages [n (%)], and the comparison between groups using Chi-square test or Fisher’s exact test.
Univariate and multivariate Cox proportional hazards model were utilized to investigate the association of HALP score, PLR score, and LMR score with the ICU mortality risk in patients with AECOPD. Variables with statistically significant differences in univariate analysis were incorporated into multivariate analysis. Stratified analyses were performed based on patients’ ICU admission type, BMI, and APACHE score. Hazard ratio (HR) with 95% confidence interval (CI) and C-index were used for outcome assessment. P value < 0.05 was considered to be significant. Multiple imputation, Kaplan–Meier (K–M) curves and forest plots were completed with R 3.6.3 software (R Foundation for Statistical Computing, Vienna, Austria). Univariate and multivariate Cox proportional hazards models and C index calculation was performed by SAS 9.4 software (SAS Institute Inc., Cary, NC, USA).
Results
Characteristics of patients
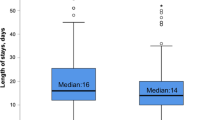
A total of 3962 patients with AECOPD were extracted from the eICU-CRD. After screening, 2429 patients were excluded, including 76 patients under 18 years old, 817 patients with ICU stay less than 24 h, 1509 patients with missing HALP calculation data, 16 patients with abnormal data, and 11 patients with missing survival information. Finally, 1533 patients with AECOPD were included in this study (Fig. 1). Table 1 shows the characteristics of all included AECOPD patients. Among these 1533 patients, the mean age was 67.48 years, 814 (53.10%) were female, and 1206 (78.67%) patients admitted to ICU by emergency. The mean or median hemoglobin, albumin, lymphocyte, platelet, and monocyte levels were 124.06 ± 23.02 g/L, 33.48 ± 5.92 g/L, 1.01 (0.57, 1.70) × 109/L, 221.00 (173.00, 282.00) × 109/L, and 0.71 (0.44, 1.04) × 109/L, respectively. The number of patients with high HALP (≥ 9.086), PLR (≥ 329.412), and LMR (≥ 0.75) scores was 1176 (76.71%), 471 (39.72%), and 1259 (82.13%), respectively. At the end of follow-up, 123 (8.00%) patients died in the ICU and 1410 (92.00%) patients were discharged. The median time to discharge for patients in the survival group and death for those in the death group were 5.85 (3.75, 8.41) and 4.71 (3.07, 8.58) days, respectively.
Significant statistical differences between the survival group and the death group were observed in terms of age, type of ICU admission, BMI, coronary artery disease, atrial fibrillation, vasopressor, SPO2, SBP, DBP, body temperature, eosinophils, bilirubin, creatinine, BUN, hemoglobin, albumin, lymphocyte, PLR score, LMR score, APACHE score, and HALP score (all P < 0.05).
Factors affected ICU mortality risk in patients with AECOPD
Univariate Cox proportional hazards model showed that older age (HR = 1.05; 95% CI 1.03–1.0), Caucasian (HR = 3.28; 95% CI 1.04–10.33), non-emergency ICU admission (HR = 1.51; 95% CI 1.03–2.20), underweight (HR = 1.87; 95% CI 1.08–3.25), coronary artery disease (HR = 2.01; 95% CI 1.13–3.57), atrial fibrillation (HR = 1.76; 95% CI 1.14–2.71), vasopressor (HR = 2.78; 95% CI 1.85–4.18), high bilirubin (HR = 1.29; 95% CI 1.06–1.56), high BUN (HR = 1.01; 95% CI 1.01–1.02), low HALP score (HR = 2.36; 95% CI 1.65–3.38), and low LMR score (HR = 2.41; 95% CI 1.66–3.49) may be associated with an increased ICU mortality risk in patients with AECOPD. Low APACHE score (HR = 0.24; 95% CI 0.17–0.34), high SPO2 (HR = 0.98; 95% CI 0.96–0.99), SBP (HR = 0.99; 95% CI 0.98–0.99), DBP (HR = 0.98; 95% CI 0.97–0.99), body temperature (HR = 0.81; 95% CI 0.67–0.98), eosinophils levels (HR = 0.78; 95% CI 0.65–0.94), and low PLR score (HR = 0.55; 95% CI 0.39–0.79) may be related to a decreased risk of ICU mortality in patients with AECOPD (Table 2).
Low HALP score associated with an increased risk of ICU mortality
Figure 2 presents the association of HALP, PLR, and LMR with ICU mortality risk in AECOPD patients. Univariate Cox proportional hazards model (model 1) indicated that HALP, PLR, and LMR were related to ICU mortality risk in patients with AECOPD (all P < 0.001). After adjusting for age, ICU admission type, BMI, coronary artery disease, atrial fibrillation, vasopressor, APACHE score, SPO2, SBP, DBP, body temperature, eosinophils, bilirubin, and BUN (model 2), low HALP score (HR = 1.69; 95% CI 1.14–2.53) and low LMR score (HR = 1.60; 95% CI 1.07–2.39) were associated with an increased ICU mortality risk in patients with AECOPD, while low PLR score (HR = 0.80; 95% CI 0.55–1.18) may be not related to ICU mortality risk. The K-M curves of HALP score, PLR score, and LMR score with ICU mortality in AECOPD patients were shown in Fig. 3.
Association between HALP score and ICU mortality risk classified by ICU admission type, BMI, and APACHE score
Among patients with emergency ICU admission, low HALP score (HR = 1.81; 95% CI 1.11–2.96) and low LMR score (HR = 1.77; 95% CI 1.07–2.93) were still related to a higher ICU mortality risk, while low PLR score (P = 0.098) may not be associated with ICU mortality risk. Low HALP, LMR and PLR scores may not be related to ICU mortality risk in patients with non-emergency ICU admission (all P > 0.05) (Fig. 4). In patients with different BMIs, low HALP, LMR, and PLR scores may not be associated with ICU mortality risk in both underweight and overweight patients (all P > 0.05) (Fig. 5). And low LMR score (HR = 2.38; 95% CI 1.21–4.69) was associated with a higher ICU mortality risk in normal BMI patients, and low HALP score (HR = 2.81; 95% CI 1.29–6.10) was associated with a higher ICU mortality risk in obese patients. Among patients with different APACHE scores, low HALP, LMR, and PLR scores may not be related to ICU mortality risk in patients with high APSCHE scores (all P > 0.05) (Fig. 6). And low HALP score (HR = 2.87; 95% CI 1.75–4.69) and low LMR score (HR = 2.78; 95% CI 1.69–4.55) were associated with an increased ICU mortality risk in patients with low APACHE scores.
Discussion
This study evaluated the prognostic value of the novel index HALP score in patients with AECOPD. AECOPD represents exacerbation of respiratory symptoms, reflecting worsening of underlying chronic airway inflammation. Our results found that low HALP score was associated with an increased risk of ICU mortality in patients with AECOPD. Subgroup analysis showed that the association between low HALP score and higher risk of ICU mortality may be more significant in patients admitted to ICU by emergency, obese patients, and patients with low APACHE scores.
Previous studies have shown that the HALP score is an important prognostic indicator for many diseases [15,16,17,18, 20]. The study by Cong et al. reported that a high HALP score was associated with longer progression-free survival in patients with esophageal squamous cell carcinoma [15]. Guo et al. demonstrated that the HALP score is an independent prognostic factor for progression-free survival after cytoreductive radical prostatectomy in patients with metastatic prostate cancer [16]. Tian et al. found that increased HALP score was associated with a decreased risk of recurrent stroke and death within 90 days and 1 year after stroke onset in patients with acute ischemic stroke [17]. Our study was the first to explore the association between HALP score and ICU mortality risk in AECOPD patients, and our results found that low HALP score was associated with an increased risk of ICU mortality in patients with AECOPD. Furthermore, the association between low HALP score and higher risk of ICU mortality may be more significant in patients admitted to ICU by emergency, obese patients, and patients with low APACHE scores. The possible explanation for the more significant association between low HALP scores and ICU mortality risk in emergency department AECOPD patients was that emergency department AECOPD patients often present fairly advanced disease [21]. The association between low HALP scores and ICU mortality risk in obese populations may be related to the fact that FEV1 is lower in obese populations [22]. Among patients with different APACHE IV scores, the overall status of patients with low APACHE IV scores was more stable, and the HALP score could well reflect the death risk of patients.
Systemic inflammation and immune response are the main factors influencing the prognosis and survival of patients with AECOPD [23]. Several studies have shown that nutrition and inflammation status parameters, including hemoglobin levels, albumin levels, lymphocyte counts, and platelet counts, are critical for survival in COPD [24,25,26,27]. Low levels of hemoglobin are associated with adverse response to treatment and worsening survival, especially in patients with advanced disease [28]. Serum albumin is routinely used to assess a patient’s nutritional status and visceral protein synthesis [29]. Low levels of serum albumin have also been identified as an independent risk factor for survival in COPD patients [26]. The counts of lymphocytes and platelets reflect the systemic inflammatory response and are novel biomarkers for the progression of COPD to AECOPD [27, 30]. The HALP score combines factors of malnutrition such as hemoglobin and albumin levels, and factors of inflammatory response such as lymphocyte and platelet counts. The HALP score can reflect the inflammation-nutritional status of patients [17, 18]. Our results suggested that the HALP score had a good prognostic value for ICU mortality risk in patients with AECOPD. In addition, indicators of hemoglobin level, albumin level, lymphocyte count, and platelet count were the most commonly used blood tests in clinical practice. The HALP score can be easily and inexpensively applied in clinical practice to monitor the risk of ICU mortality in patients with AECOPD.
In this study we explored the relationship between HALP score and ICU mortality risk in AECOPD patients based on multicenter data from eICU-CRD. Then we further analyzed the association between HALP score and ICU mortality risk in AECOPD patients in different populations according to ICU admission type, BMI, and APACHE score. However, there were some limitations to this study. First, we only obtained laboratory indicators such as hemoglobin level, albumin level, lymphocyte count, and platelet count at admission, but did not explore the impact of dynamic changes in HALP scores at different stages on patient mortality. Second, the retrospective design of this study had certain biases, which may affect the accuracy of the results. Third, the effect of specific medication conditions such as corticosteroid use on patient survival was not considered due to database limitations. Fourth, our study was based on the eICU database, and additional external data are needed to validate the predictive value of HALP scores for ICU mortality risk in patients with AECOPD.
Conclusions
This study investigated the association between HALP score and ICU mortality risk in patients with AECOPD based on the multicenter database. Low HALP score was associated with an increased ICU mortality risk in patients with AECOPD, suggesting that the HALP score may be a novel prognostic predictor in patients with AECOPD. Future studies may focus on the impact of dynamically changing HALP scores or HALP score trajectories on the prognosis of patients with AECOPD.
References
Celli BR, Wedzicha JA (2019) Update on clinical aspects of chronic obstructive pulmonary disease. New Engl J Med 381(13):1257–1266. https://doi.org/10.1056/NEJMra1900500
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N et al (2018) Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global burden of disease study 2017. Lancet (London, England) 392(10159):1736–1788. https://doi.org/10.1016/s0140-6736(18)32203-7
Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Chen R, Decramer M, Fabbri LM, Frith P, Halpin DM, López Varela MV, Nishimura M, Roche N, Rodriguez-Roisin R, Sin DD, Singh D, Stockley R, Vestbo J, Wedzicha JA, Agustí A (2017) Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report GOLD executive summary. Am J Respir Crit Care Med 195(5):557–582. https://doi.org/10.1164/rccm.201701-0218PP
MacLeod M, Papi A, Contoli M, Beghé B, Celli BR, Wedzicha JA, Fabbri LM (2021) Chronic obstructive pulmonary disease exacerbation fundamentals: diagnosis, treatment, prevention and disease impact. Respirology (Carlton, Vic) 26(6):532–551. https://doi.org/10.1111/resp.14041
Paliogiannis P, Fois AG, Sotgia S, Mangoni AA, Zinellu E, Pirina P, Negri S, Carru C, Zinellu A (2018) Neutrophil to lymphocyte ratio and clinical outcomes in COPD: recent evidence and future perspectives. Eur Respir Rev 27(147):170113. https://doi.org/10.1183/16000617.0113-2017
Kandemir Y, Doğan N, Yaka E, Pekdemir M, Yılmaz S (2021) Clinical characteristics of neutrophilic, eosinophilic and mixed-type exacerbation phenotypes of COPD. Am J Emerg Med 45:237–241. https://doi.org/10.1016/j.ajem.2020.08.044
Semenzato U, Biondini D, Bazzan E, Tiné M, Balestro E, Buldini B, Carizzo SJ, Cubero P, Marin-Oto M, Casara A, Baraldo S, Turato G, Gregori D, Marin JM, Cosio MG, Saetta M (2021) Low-blood lymphocyte number and lymphocyte decline as key factors in COPD outcomes: a longitudinal cohort study. Respir Int Rev Thorac Dis 100(7):618–630. https://doi.org/10.1159/000515180
Yao C, Liu X, Tang Z (2017) Prognostic role of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio for hospital mortality in patients with AECOPD. Int J Chron Obstruct Pulmon Dis 12:2285–2290. https://doi.org/10.2147/copd.S141760
Kumar P, Law S, Sriram KB (2017) Evaluation of platelet lymphocyte ratio and 90-day mortality in patients with acute exacerbation of chronic obstructive pulmonary disease. J Thorac Dis 9(6):1509–1516. https://doi.org/10.21037/jtd.2017.05.77
Baldemir R, Cirik M (2022) Practical parameters that can be used for nutritional assessment in patients hospitalized in the intensive care unit with the diagnosis of chronic obstructive pulmonary disease: prognostic nutritional index, neutrophil-to-lymphocyte, platelet-to-lymphocyte, and lymphocyte-to-monocyte ratio. Medicine 101(24):e29433. https://doi.org/10.1097/md.0000000000029433
Raad S, Smith C, Allen K (2019) Nutrition status and chronic obstructive pulmonary disease: can we move beyond the body mass index? Nutr Clin Prac 34(3):330–339. https://doi.org/10.1002/ncp.10306
Girón R, Matesanz C, García-Río F, de Santiago E, Mancha A, Rodríguez-Salvanés F, Ancochea J (2009) Nutritional state during COPD exacerbation: clinical and prognostic implications. Ann Nutr Metab 54(1):52–58. https://doi.org/10.1159/000205960
Yang IA, Brown JL, George J, Jenkins S, McDonald CF, McDonald VM, Phillips K, Smith BJ, Zwar NA, Dabscheck E (2017) COPD-X Australian and New Zealand guidelines for the diagnosis and management of chronic obstructive pulmonary disease: 2017 update. Med J Aust 207(10):436–442. https://doi.org/10.5694/mja17.00686
Mekal D, Czerw A, Deptala A (2021) Dietary behaviour and nutrition in patients with COPD treated with long-term oxygen therapy. Int J Environ Res Public Health 18(23):12739. https://doi.org/10.3390/ijerph182312793
Cong L, Hu L (2017) The value of the combination of hemoglobin, albumin, lymphocyte and platelet in predicting platinum-based chemoradiotherapy response in male patients with esophageal squamous cell carcinoma. Int Immunopharmacol 46:75–79. https://doi.org/10.1016/j.intimp.2017.02.027
Guo Y, Shi D, Zhang J, Mao S, Wang L, Zhang W, Zhang Z, Jin L, Yang B, Ye L, Yao X (2019) The Hemoglobin, albumin, lymphocyte, and platelet (HALP) score is a novel significant prognostic factor for patients with metastatic prostate cancer undergoing cytoreductive radical prostatectomy. J Cancer 10(1):81–91. https://doi.org/10.7150/jca.27210
Tian M, Li Y, Wang X, Tian X, Pei LL, Wang X, Zhang L, Sun W, Wu J, Sun S, Ning M, Buonanno F, Xu Y, Song B (2020) The Hemoglobin, albumin, lymphocyte, and platelet (HALP) score is associated with poor outcome of acute ischemic stroke. Front Neurol 11:610318. https://doi.org/10.3389/fneur.2020.610318
Xu SS, Li S, Xu HX, Li H, Wu CT, Wang WQ, Gao HL, Jiang W, Zhang WH, Li TJ, Ni QX, Liu L, Yu XJ (2020) Haemoglobin, albumin, lymphocyte and platelet predicts postoperative survival in pancreatic cancer. World J Gastroenterol 26(8):828–838. https://doi.org/10.3748/wjg.v26.i8.828
Pollard TJ, Johnson AEW, Raffa JD, Celi LA, Mark RG, Badawi O (2018) The eICU collaborative research database, a freely available multi-center database for critical care research. Sci Data 5:180178. https://doi.org/10.1038/sdata.2018.178
Leetanaporn K, Hanprasertpong J (2022) Predictive value of the hemoglobin-albumin-lymphocyte-platelet (HALP) index on the oncological outcomes of locally advanced cervical cancer patients. Cancer Manag Res 14:1961–1972. https://doi.org/10.2147/cmar.S365612
Rowe BH, Bhutani M, Stickland MK, Cydulka R (2011) Assessment and management of chronic obstructive pulmonary disease in the emergency department and beyond. Expert Rev Respir Med 5(4):549–559. https://doi.org/10.1586/ers.11.43
Spelta F, Fratta Pasini AM, Cazzoletti L, Ferrari M (2018) Body weight and mortality in COPD: focus on the obesity paradox. Eat Weight Disord 23(1):15–22. https://doi.org/10.1007/s40519-017-0456-z
Shi L, Zhu B, Xu M, Wang X (2018) Selection of AECOPD-specific immunomodulatory biomarkers by integrating genomics and proteomics with clinical informatics. Cell Biol Toxicol 34(2):109–123. https://doi.org/10.1007/s10565-017-9405-x
Park SC, Kim YS, Kang YA, Park EC, Shin CS, Kim DW, Rhee CK (2018) Hemoglobin and mortality in patients with COPD: a nationwide population-based cohort study. Int J Chron Obstr Pulm Dis 13:1599–1605. https://doi.org/10.2147/copd.S159249
Toft-Petersen AP, Torp-Pedersen C, Weinreich UM, Rasmussen BS (2016) Association between hemoglobin and prognosis in patients admitted to hospital for COPD. Int J Chron Obstr Pulm Dis 11:2813–2820. https://doi.org/10.2147/copd.S116269
Chen D, Jiang L, Li J, Tan Y, Ma M, Cao C, Zhao J, Wan X (2021) Interaction of acute respiratory failure and acute kidney injury on in-hospital mortality of patients with acute exacerbation COPD. Int J Chron Obstr Pulm Dis 16:3309–3316. https://doi.org/10.2147/copd.S334219
El-Gazzar AG, Kamel MH, Elbahnasy OKM, El-Naggar ME (2020) Prognostic value of platelet and neutrophil to lymphocyte ratio in COPD patients. Expert Rev Respir Med 14(1):111–116. https://doi.org/10.1080/17476348.2019.1675517
Bhindi B, Hermanns T, Wei Y, Yu J, Richard PO, Wettstein MS, Templeton A, Li K, Sridhar SS, Jewett MA, Fleshner NE, Zlotta AR, Kulkarni GS (2016) Identification of the best complete blood count-based predictors for bladder cancer outcomes in patients undergoing radical cystectomy. Br J Cancer 114(2):207–212. https://doi.org/10.1038/bjc.2015.432
Eckart A, Struja T, Kutz A, Baumgartner A, Baumgartner T, Zurfluh S, Neeser O, Huber A, Stanga Z, Mueller B, Schuetz P (2020) Relationship of nutritional status, inflammation, and serum albumin levels during acute illness: a prospective study. Am J Med 133(6):713-722.e717. https://doi.org/10.1016/j.amjmed.2019.10.031
Zinellu A, Paliogiannis P, Sotgiu E, Mellino S, Fois AG, Carru C, Mangoni AA (2021) Platelet count and platelet indices in patients with stable and acute exacerbation of chronic obstructive pulmonary disease: a systematic review and meta-analysis. COPD 18(2):231–245. https://doi.org/10.1080/15412555.2021.1898578
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Protocols of eICU-CRD were approved by the Institutional Review Board (IRB) of the Massachusetts Institute of Technology and informed consent was obtained from patients or their families.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Han, H., Hu, S. & Du, J. Predictive value of the hemoglobin–albumin–lymphocyte–platelet (HALP) index for ICU mortality in patients with acute exacerbations of chronic obstructive pulmonary disease (AECOPD). Intern Emerg Med 18, 85–96 (2023). https://doi.org/10.1007/s11739-022-03132-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-022-03132-4