Abstract
Purpose
The aim of this study is to evaluate the change in rate of increase of bariatric surgery performed compared to the growth of obesity and severe obesity in the United States (US).
Materials and Methods
The number of primary adult bariatric procedures performed in the US between 2015 and 2018 was obtained from the Metabolic and Bariatric Surgery Accreditation Quality and Improvement Project (MBSAQIP) database. The US Census database was used to derive age-adjusted obesity and severe obesity prevalence among adults. Prevalence of bariatric surgery, by year, was estimated as the ratio of the number of patients undergoing surgery and the projected number of eligible individuals for that year.
Results
There were 627,386 bariatric procedures performed for body mass index (BMI) ≥ 30 kg/m2, of which 73.3% (n = 459,800) were performed for BMI ≥ 40 kg/m2. Although the rate of obesity increased by 3.32% per year during this period (RR = 1.0332 per year increase; 95% CI = 1.0313, 1.0352), the rate of surgery per eligible population increased by only 2.47% (RR = 1.0247 per year increase; 95% CI = 1.0065, 1.0432). The prevalence of severe obesity increased from 7.70% (n = 17,494,910) in 2015 to 9.95% (n = 23,135,039) in 2018 while the prevalence of surgery decreased from 0.588 per 100 eligible population in 2015 to 0.566 per 100 eligible population in 2018.
Conclusion
The rate of utilization has not kept up with the rate of increase in this disease, our costliest illness. There is a strong need to educate the public, healthcare professionals, insurance carriers, and legislators.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite its success as the most effective treatment for type 2 diabetes and the other expressions of the metabolic syndrome such as severe obesity, dyslipidemia and non-alcoholic steatotic hepatitis (NASH), and its improved safety profile [1], bariatric surgery remains vastly underutilized; only 1% or less of the eligible population undergoes this treatment [2]. To put it another way, 99% of those Americans who could be freed of our most costly diseases are not getting this therapy.
Obesity is a pandemic. In the United States (US) alone, the prevalence doubled from 1999–2009 and doubled again in the last decade leaving more than a third of the US adult population obese and severely obese [3]. The excess weight affects quality of life, productivity, and longevity. It is associated with our costliest major health comorbidities, including type II diabetes mellitus, hypertension, obstructive sleep apnea, asthma, cardiovascular events, and some cancers. In addition to the direct costs, patients with obesity and with chronic diseases and who undergo surgical procedures have higher rates of complications and longer hospital lengths of stay, adding to an already significant burden to healthcare resources [4, 5]. If trends increase at the current rate, obesity related costs will rise by up to $66 billion a year in the next decade in the US [6]. However, although metabolic surgery has proven to be the most effective treatment to obesity and obesity related co-morbidities [7–9], it remains significantly underutilized. If there were a medication that could produce the same effects, with the same low rate of side effects, would the great majority of our population accept the denial of access?
Although there are studies evaluating the numbers of obesity procedures per year, no studies have evaluated if the rate of increase of procedures is keeping up with the rate of increase of obesity. The purpose of this study is to evaluate the rate of increase of bariatric surgery performed for both obesity and severe obesity using the Metabolic and Bariatric Surgery Accreditation Quality and Improvement Project (MBSAQIP) database and to determine whether the limited increase of these procedures is keeping up with the stepwise progressive increase in the eligible population for bariatric surgery.
Methods
The number of primary bariatric procedures performed in the United States (US) among obese and severe obese adults (ages 20–80) between 2015 and 2018 was obtained from the Metabolic and Bariatric Surgery Accreditation Quality and Improvement Project (MBSAQIP) database. The age group was chosen in order to parallel the population of the US Census. A joint effort by the American College of Surgeons (ACS) and the American Society for Metabolic and Bariatric Surgery (ASMBS), the MBSAQIP database is an administrative database designed to achieve a national accreditation standard for bariatric surgery centers. All accredited centers report their outcomes to the MBSAQIP database. Obesity was defined as body mass index (BMI) ≥ 30 kg/m2 and severe obesity as BMI ≥ 40 kg/m2. BMI cutoffs for obesity and severe obesity are based on Centers for Disease Control and Prevention (CDC) definitions and are typically used to identify eligible patients for surgery in clinical practice. The BMI ≥ 30 kg/m2 was specifically used as a surrogate to describe the prevalence of disease of obesity in the US society. BMI ≥ 35 kg/m2, which is the BMI to qualify for surgery, could not be examined based on the CDC definitions.
The US Census data were used to derive age-adjusted obesity and severe obesity prevalence among adults ages 20–80. Age-adjusted prevalence of obesity and severe obesity were obtained from the CDC brief report [10]. Prevalence of bariatric surgery by year was estimated as the ratio of the number of patients undergoing surgery and the projected number of eligible individuals (obese and severe obese) for that year.
Statistical Analysis
Continuous variables are summarized by presenting the number of non-missing observations, mean, standard deviation (SD), median, 25th, and 75th quartile while categorical variables are summarized by presenting the number of patients and percentage for each category.
The number of eligible individuals and the number of bariatric surgeries were modeled using negative binomial regression with population included as an offset variable. Relative risk (RR) and 95% confidence intervals (CI) are provided as measures of strength of association and precision, respectively.
Ethical Considerations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent does not apply for this study.
Results
Between 2015 and 2018, 627,386 bariatric procedures, performed for BMI ≥ 30 kg/m2, were reported in MBSAQIP. Of these, 73.3% (n = 459,800) of the procedures were performed in patients with BMI ≥ 40 kg/m2. Baseline characteristics are summarized overall and by year of operation in Table 1. Overall, mean age (SD) was 44.8 (11.8) years, 72.7% were White, and 79.6% were female. Nearly half of the patients had pre-operative hypertension requiring medication while 24% had pre-operative hyperlipidemia. Only a small fraction of the patients were on dialysis prior to the procedure.
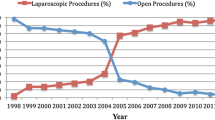
The number of procedures for BMI ≥ 30 kg/m2 increased from 139,083 in 2015 to 168,666 in 2018. Age-adjusted rate of surgery for BMI ≥ 30 kg/m2 relative to the eligible population by year is depicted in Table 2. Although the rate of obesity increased by 3.32% per year from 2015 to 2018 (RR = 1.0332 per year increase; 95% CI = 1.0313, 1.0352), the rate of surgery per eligible population increased by only 2.47% (RR = 1.0247 per year increase; 95% CI = 1.0065, 1.0432) (Fig. 1).
For severe obesity (BMI ≥ 40 kg/m2), 459,800 bariatric procedures were performed between 2015 and 2018, as procedures increased from 102,947 to 122,909 in 2015 and 2018, respectively (Table 2). The prevalence of severe obesity increased from 7.70% (n = 17,494,910.36) in 2015 to 9.95% (n = 23,135,039.32) in 2018 while the prevalence of surgery decreased from 0.588 per 100 eligible population in 2015 to 0.566 per 100 eligible population in 2018 (Fig. 2).
Discussion
Despite the clear benefits of bariatric surgery, it is very underutilized, as overall percent procedures performed was 0.164% for BMI ≥ 30 kg/m2 and 0.566% for BMI ≥ > 40 kg/m2 among the eligible population, based on the procedure numbers being performed at all accredited bariatric centers. This is lower than previously reported utilization of 1% or less 2. Even if the small number of cases performed in non-approved centers of excellence and/or the outpatient setting was included, it is unlikely to change the conclusion that access for optimal care is not occurring at an increasing rate. Alarmingly, while both class I and class III obesity are on the increase, based on the US population census, there is a steady decrease in rates for bariatric procedures ≥ 40 kg/m2 between 2015 and 2018. When comparing the rates of increase in the number of surgeries to the number of those that are eligible, there is a big gap as the number of surgeries is increasing by thousands compared to millions of new obesity patients per year, respectively. However, not all of those who are potential candidates could undergo surgery, as some may be poor candidates due to psychological issues or others factors. However, it is problematic that surgery is lagging so far behind.
As obesity grows, so do the costs associated with the disease. Bariatric surgery, despite being an effective treatment of obesity and obesity related co-morbidities, is additionally less expensive. Obesity is associated with some of the costliest major health co-morbidities, such as type II diabetes mellitus, hypertension, sleep apnea, cardiovascular disease, and certain cancers. As previously mention, both direct and indirect costs significantly contribute to the healthcare burden [4, 5]. In 2017, annual average cost of medical expenditures for a person diagnosed with diabetes was $16,752, while one-time cost of surgery ranges between $14,900 for SG and $23,000 for RYGB [11].
The reasons for underutilization can be multifactorial including bias against the obese, a failure to educate the public, disinformation among health providers, resistance by employers, and carriers as well as inaction by legislators. Access to care is a major barrier and many disparities exist. In a study published in 2010, similar to our findings, the majority (75%) of patients undergoing bariatric surgery were white [12]. In addition, 82% had private insurance and 80% had greater median incomes. However, that does not accurately represent those that are eligible for weight loss surgery, as the majority of eligible candidates are non-white; have lower and have less access to healthcare; with a significant portion either uninsured or underinsured [12, 13].
An informal survey [15] found three major factors that limited access to care: (1) referring physicians had serious doubts about the efficacy and safety of the operations, (2) patients were not informed, and (3) hurdles posed by insurance carriers. Physician bias and perception can play a critical role as recommendation from a primary care physician increases the likelihood of a patient considering bariatric surgery [14]. The physician who is more knowledgeable about bariatric surgery is more likely to consider referral [15]. Because there is a discordance between actual and perceived risks among healthcare providers, teaching and awareness are crucial [16]. Another survey performed by the ASMBS and National Opinion Research Center (NORC) [17] shows that while there is a growing public concern about the dangers of obesity, only one in three of those with obesity reported that they have ever spoken with a doctor about their weight. Furthermore, only 12% of those who describe themselves as having severe obesity reported that a doctor had ever suggested they consider bariatric surgery [17].
Lack of knowledge about insurance coverage can affect referrals as well. In a national survey of primary care physicians, 59% reported that at least one in four of their patients had a BMI of 35 kg/m2. However, cost was a perceived limitation to access to surgery, as more than half believed that their patients could not afford metabolic surgery [14]. Another study of 16 primary care physicians who participated in three focus groups regarding metabolic surgery reported “not knowing if insurance would cover bariatric surgery” as a one of the five factors that made physicians hesitate to recommend and refer patients for metabolic procedures [16]. This is further complicated by insurance companies themselves making it challenging by demanding arbitrary time periods of pre-operative weight loss effort documentation, as the benefits of that requirement has been repeatedly shown to provide no benefit to the patient [18].
Another reason for underutilization of bariatric surgery is the advances in endoscopic procedures in the treatment of obesity as well as newer weight loss medications. Endoscopic bariatric procedures include endoscopic gastroplasty, gastric balloons, and the transpyloric shuttle. Despite these rapid advances, the procedures are typically not be covered by insurance in the US and do not have long-term data. An article published in 2018 reported that these procedures may only account for about 4% of bariatric procedures performed worldwide [19].
There is also widespread public stigma and lack of knowledge towards people with obesity and treatment via metabolic surgery. While the public agrees obesity is a serious disease, the majority believe that patients who undergo bariatric surgery choose “the easy way out” and that bariatric surgery is an elective cosmetic procedure [20, 21]. This perception contradicts the paramount evidence that surgery remains the most effective treatment and that there is no other therapy that provides such a broad and salutary effect on health, function, and quality of life [9, 22–24]. Another misperception is in regard to the safety profile of surgery. Despite often-mentioned concerns about complications and mortality, data across the US for accredited centers prove that weight loss surgery is remarkably safe, particularly in light of the underlying high risk of performing surgery in general in patients with obesity who typically suffer from multiple comorbidities. An analysis of over 400,000 bariatric procedures performed between 2007 and 2012 reported a very low 30-day mortality of 0.1% [25], compared to the mortality of commonly performed procedures like cholecystectomy and other foregut procedures, which are higher (0.27% and 019%, respectively) [26, 27], yet generally believed to be very safe. Perhaps, one explanation is that both physicians and patients rely on bad examples, such as complications they may encounter in the hospital or experiences of friends and media perception. Ongoing education is absolutely vital to ensure that both the public and the medical community have an accurate understanding of the risks and benefits of bariatric surgery.
Educating the public and the medical profession is of outmost importance. Surgeons should work to keep the discussion going with other healthcare providers and patients, providing them with accurate data regarding eligibility and outcomes. Working with insurers is also important in order to ensure that every who is eligible can have access to surgery. In addition, advocacy, both personal and at societal level, is crucial.
The strengths of this study include the use of a large administrative database and the large sample size. Despite these strengths, there are certain limitations that accompany the use of an administrative database, such as the lack of clinically rich data and the possibility of coding errors. We rely on International Classification of Diseases (ICD)-9, ICD-10, and Current Procedural Terminology (CPT) coding which does not describe the full clinical picture. In addition, our numbers are smaller compared to the numbers reported by the ASMBS, as MBSAQIP only collects data from accredited institutions and does not account for those procedures performed at outpatient centers and non-accredited institutions. As the CDC only reports rates of obesity (BMI ≥ 30 kg/m2) and severe obesity (BMI ≥ 40 kg/m2) (Table 3), we could not examine the growth rate of patients with BMI ≥ 35 kg/m2 which is often considered to be a cutoff for bariatric surgery. However, we accounted for that by comparing procedure numbers of BMI ≥ 30 kg/m2 using the MBSAQIP. In addition, we had to exclude patients below age 20, as the US Census database only includes ages 20–80. Despite these limitations, this is the first study to evaluate the rates of utilization compared to the rate of increase in obesity in the USA.
Conclusion
The rate of increase in obesity and utilization of bariatric surgery are not congruous and bariatric surgery is greatly underutilized. The underutilization is multifactorial and largely related to healthcare and public misperception, malalignment of treatment paradigms, and insurance policies. We must continue to educate the public, our medical colleagues, the carriers, and legislators.
References
Aminian A, Andalib A, Khorgami Z, et al. A nationwide safety analysis of bariatric surgery in nonseverely obese patients with type 2 diabetes. Surg Obes Relat Dis. 2016;12(6):1163–70.
English WJ, DeMaria EJ, Hutter MM, et al. American Society for Metabolic and Bariatric Surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis. 2020;16(4):457–63.
Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016 315(21):2284
Sood A, Abdollah F, Sammon JD, et al. The effect of body mass index on perioperative outcomes after major surgery: results from the National Surgical Quality Improvement Program (ACS-NSQIP) 2005–2011. World J Surg. 2015;39(10):2376–85.
Zizza C, Herring AH, Stevens J, et al. Length of hospital stays among obese individuals. Am J Public Health. 2004;94(9):1587–91.
Tremmel M, Gerdtham UG, Nilsson PM, et al. Economic burden of obesity: a systematic literature review. Int J Environ Res Public Health. 2017;14(4):435.
Colquitt JL, Pickett K, Loveman E, et al. Surgery for weight loss in adults. Cochrane Database Syst Rev 2014 8: CD003641.
Inge TH, Courcoulas AP, Jenkins TM, et al. Weight loss and health status 3 years after bariatric surgery in adolescents. N Engl J Med. 2016;374(2):113–23.
Courcoulas AP, King WC, Belle SH, et al. Seven-year weight trajectories and health outcomes in the Longitudinal Assessment of Bariatric Surgery (LABS) study. JAMA Surg. 2018;153(5):427–34.
Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief, no 360. Hyattsville, MD: National Center for Health Statistics 2020.
Association., American Diabetes, Economic costs of diabetes in the U.S. in 2017. Accessed at https://care.diabetesjournals.org/content/41/5/917 on October 22, 2020. , 2018.
Martin M, Beekley A, Kjorstad R, et al. Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. Surg Obes Relat Dis. 2010;6(1):8–15.
Mainous AG, Johnson SP, Saxena SK, et al. Inpatient bariatric surgery among eligible black and white men and women in the United States, 1999–2010. Am J Gastroenterol. 2013;108(8):1218–23.
Tork S, Meister KM, Uebele AL, et al. Factors influencing primary care physicians’ referral for bariatric surgery. JSLS J Soc Laparoendosc Surg, 2015. 19(3): e2015.
Ferrante JM, Piasecki AK, Ohman-Strickland PA, et al. Family physicians’ practices and attitudes regarding care of extremely obese patients. Obesity. 2009;17:1710–6.
Funk LM, Jolles S, Fischer LE, et al. Patient and referring practitioner characteristics associated with the likelihood of undergoing bariatric surgery: a systematic review. JAMA Surg. 2015;150(10):999–1005.
ASMBS/ NORC Brief (2016). Obesity Rises to Top Health Concern for Americans, but Misperceptions Persist. Accessed on Aug 10, 2020 at : https://www.norc.org/PDFs/ASMBS%20Obesity/ASMBS%20NORC%20Obesity%20Poll_Brief%20A%20REV010917.pdf.
ASMBS updated position statement on insurance mandated preoperative weight loss requirements. Surg Obes Relat Dis 2016. 12(5): 955–9.
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, et al. IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018;28:3783–94.
Dolan P, Afaneh C, Symer M, et al. Assessment of Public Attitudes Toward Weight Loss Surgery in the United States. JAMA Surg. 2019;154(3):264–6.
Executive Council of ASMBS. Safer through surgery: American Society for Metabolic and Bariatric Surgery statement regarding metabolic and bariatric surgery during the COVID-19 pandemic. Surg Obes Relat Dis. 2020;16(8):981–2.
Adams TD, Davidson LE, Litwin SE, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377(12):1143–55.
Zhou X, Yu J, Li L, et al. Effects of bariatric surgery on mortality, cardiovascular events, and cancer outcomes in obese patients: systematic review and meta-analysis. Obes Surg. 2016;26(11):2590–601.
Adams TD, Mehta TS, Davidson LE, et al. All-cause and cause-specific mortality associated with bariatric surgery: a review. Curr Atheroscler Rep. 2015;17(12):74.
Sudan R, Nguyen NT, Hutter MM, et al. Morbidity, mortality, and weight loss outcomes after reoperative bariatric surgery in the USA. J Gastrointest Surg. 2015;19:171–9.
Ingraham AM, Cohen ME, Ko CY, et al. A current profile and assessment of North American cholecystectomy: results from the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;211:176–86.
Niebisch S, Fleming FJ, Galey KM, et al. Perioperative risk of laparoscopic fundoplication: safer than previously reported-analysis of the American College of Surgeons National Surgical Quality Improvement Program 2005 to 2009. J Am Coll Surg. 2012;215:61–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• The rate of obesity is increasing in the USA
• The rate of utilization of bariatric surgery has not kept up
• There is a need for education of healthcare professionals and public
Rights and permissions
About this article
Cite this article
Altieri, M.S., Irish, W., Pories, W.J. et al. Examining the Rates of Obesity and Bariatric Surgery in the United States. OBES SURG 31, 4754–4760 (2021). https://doi.org/10.1007/s11695-021-05628-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05628-y