Abstract
The question of whether or not nonsurgical intentional or voluntary weight loss results in reduced mortality has been equivocal, with long-term mortality following weight loss being reported as increased, decreased, and not changed. In part, inconsistent results have been attributed to the uncertainty of whether the intentionality of weight loss is accurately reported in large population studies and also that achieving significant and sustained voluntary weight loss in large intervention trials is extremely difficult. Bariatric surgery has generally been free of these conflicts. Patients voluntarily undergo surgery and the resulting weight is typically significant and sustained. These elements, combined with possible non-weight loss-related mechanisms, have resulted in improved comorbidities, which likely contribute to a reduction in long-term mortality. This paper reviews the association between bariatric surgery and long-term mortality. From these studies, the general consensus is that bariatric surgical patients have: 1) significantly reduced long-term all-cause mortality when compared to severely obese non-bariatric surgical control groups; 2) greater mortality when compared to the general population, with the exception of one study; 3) reduced cardiovascular-, stroke-, and cancer-caused mortality when compared to severely obese non-operated controls; and 4) increased risk for externally caused death such as suicide.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dr. George Bray, pioneer of obesity research, aptly titled his editorial that accompanied two publications associating long-term mortality with bariatric surgery [1, 2], “The Missing Link—Lose Weight, Live Longer” [3]. Indeed, it appears unclear whether significant and sustained intentional weight loss results in improved mortality when equivocal results from observational studies demonstrate an increase [4, 5], decrease [6], or no change [7] in mortality following nonsurgical, voluntary weight loss [8]. While increasing body mass index (BMI) has been plainly associated with increasing disease risk [9–14] and long-term mortality [15], with an even a greater mortality risk when BMI is equal to or greater than 35 kg/m2 compared to class I obesity (BMI equal to 30–34.9 kg/m2) [8, 16–18], most clinical studies (observational in nature) have failed to show decreased mortality for cardiovascular disease subsequent to nonsurgical weight reduction [19] and have, in fact, demonstrated an increased risk following nonsurgical weight loss [19–22]—even if participants were overweight or obese at pre-weight loss intervention [19, 21, 23]. A similar unclear outcome exists for the association of cancer risk and voluntary weight loss. Although multiple studies have demonstrated cancer risk to be positively associated with BMI [24–27], studies linked to voluntary weight loss have reported reduced cancer risk (self-reported, voluntary weight loss) [19, 28, 29] as well as increased cancer risk [4, 19, 30].
Speculation for this apparent paradox (i.e., voluntary, nonsurgical weight loss resulting in equivocal mortality improvement) has centered on a number of methodological issues such as bias and confounding [8, 9, 19, 31]. The task of accurately assigning whether the study participant’s weight loss was voluntary has been problematic, especially in observational studies [8, 19]. The inclusion of subjects with occult disease, tobacco use, or patient’s whose weight loss therapy has been recommended for disease management such as diabetes has also been recognized as possible confounders to truly assessing intentional weight loss outcomes [31]. Perhaps the primary factor that has limited large population intentional weight loss studies (nonsurgical) has been the challenge of participants achieving and sustaining clinically meaningful weight loss over an extended period of time [8, 31–33]. Nonsurgical treatment of obesity, especially for the severely obese (i.e., BMI ≥ 35 kg/m2), has typically been unsuccessful in achieving substantial and sustained weight reduction [9, 34–36], with traditional approaches to weight loss such as behavioral counseling, physical activity, and diet and pharmacological therapy now considered inadequate for treating severe obesity [37–39]. Further, intense medical therapy employed in recent randomized control trials has resulted in only a 5 % weight loss in severely obese participants at 1 to 2 years follow-up [40–42]. Lifestyle-based therapy employed for diabetes prevention has not demonstrated significant prevention of events related to cardiovascular disease over a 10- to 20-year follow-up period [19, 43, 44], and lifestyle therapy plus weight loss medication have not resulted in reduced cardiovascular disease endpoints [19, 45, 46]. In conclusion, quoting Dr. Lars Sjöström, “Taken together, trials of nonsurgical weight loss in obese participants have failed to demonstrate a benefit of reduced mortality or decreased cardiovascular disease event rates” [19].
The only medical intervention (to date) that has demonstrated substantial effects on weight loss in the severely obese population, short- and long-term, is bariatric surgery [1, 47]. Prospectively controlled cohort studies [39, 48], randomized control trials [40, 41], and meta-analysis findings [49] have reported percentages of initial weight loss among severely obese patients undergoing gastric bypass or sleeve gastrectomy procedures to be 25–35 % at 1 to 2 years of follow-up and 25–28 % at 6 to 10 years following surgery. In addition, limited long-term studies have demonstrated clinically relevant improvements in obesity-related conditions such as T2DM remission and improved blood pressure and lipids, with some degree of recurrence of these comorbidities over time [39, 48, 50–53]. Therefore, in contrast to conventional weight loss therapy, bariatric surgery represents a voluntary/intentional intervention resulting in a significant body weight reduction percentage which has been sustained for a meaningful period of time. These factors are likely the primary reasons bariatric surgery has facilitated successful research associating intentional weight loss and long-term mortality, the key that eventually provided the missing link—lose weight and live longer.
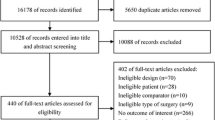
The remainder of this review highlights the number of longer-term mortality post-bariatric surgical studies. Longer-term is defined as at least 2 years of postoperative follow-up after bariatric surgery. Variation in methodological aspects of long-term mortality studies are discussed as well as physiological mechanisms that may explain reduced longer-term mortality following bariatric surgery. Increased risk for externally caused deaths following bariatric surgery such as suicides, accidents and poisonings of undetermined intent, mortality risk prediction, and decision modeling to predict life expectancy (LE) are briefly discussed in this review. Although meaningful effort has been undertaken to perform an exhaustive review of past and current manuscripts relating long-term mortality following bariatric surgery, one or more studies may have been inadvertently omitted. If this is the case, apologies are extended to authors of such scientific reports.
Methodological Characteristics
Since the first published study by MacDonald et al. in 1997 [54] reporting long-term mortality associated with bariatric surgery, there have been at least 28 studies reporting mortality rates at least 2 years after bariatric surgery [1, 2, 54–79]. While the majority of these papers relate to all-cause mortality, deaths caused by cardiovascular disease(s), cancer, and suicide are frequently highlighted. As expected, these studies have included a wide variety of methodological approaches. However, common to all but one of these studies has been the use of a retrospective cohort. Only the Swedish Obesity Subjects study [1] has followed a prospective cohort design. Highlighted in Table 1 is a brief description of these bariatric surgical studies, listed in order by the year in which the research was published.
As detailed in Table 1, bariatric surgical cohorts have ranged in number from 154 [54] to 18,972 patients [58]. Inclusion of control cohorts has been employed by 71 % of the studies (n = 20) with one study comparing the clinical data of patients 2 years prior to bariatric surgery to their post-surgical data [78]. The only study to have actual recruitment of control participants was the SOS study, which included 2037 control patients matched on a number of variables to the 2010 surgical patients [1]. The source of nonsurgical control subjects have included: 1) mortality rates of the general population (state and national) [62, 66–68, 76]; 2) non-bariatric surgical patient data extracted from hospitals, including Veterans Affairs medical centers, health clinics, and bariatric surgical centers; 3) national diabetes registry [79]; and 4) driver license applicants who had not had bariatric surgery [2]. Briefly, other characteristics of interest regarding the selection of control cohorts have included: 1) severely obese subjects without bariatric surgery; 2) control patients with similar cardiovascular events [71] or hospitalizations [73]; 3) severely obese patients seeking bariatric surgery but did not undergo the surgery [54, 60]; severely obese (≥35 kg/m2) male Medicare patients [66]; patients who were diagnosed with T2DM at the time of matching to bairatirc surgical patients [79]; and 5) veterans, representing a generally higher health-risk and predominantly male [65, 69, 77]. Methodological selection of severely obese controls from hospitals, clinics, and medical centers has generally included the use of CPT codes corresponding to obesity or morbid obesity. Mortality rates of the general population have been used in at least six studies [62, 66–68, 76]. In addition to inclusion of the general population mortality rates, two of these studies also involved obese population-based controls [66, 76]. Telem et al. obtained from the Center for Disease Control and Prevention the actuarial mortality rates for the state of New York, and in addition to general mortality rates, they assumed one-third of New York to be obese, estimating the hazard ratio (HR) of the obese population compared to the general population [76, 80]. To obtain both general- and obese-population mortality rates for control comparisons, Marsk et al. accessed data from the Military Service Conscription Registry which included records of height and weight (i.e., BMI) and conscription dates [66]. One motivation for using general population-based control cohorts as opposed to hospital patient-obtained controls is that the hospital patients may naturally have a greater morbidity profile when compared to the general population, possibly introducing a bias (referred to as the Berksonian bias [81]) [62]. Accessing the Swedish National Diabetes Registry, Eliasson et al. matched only bariatric surgical patients who were T2DM prior to gastric bypass surgery with patients who were diagnosed with T2DM at the time of matching [79].
Of the long-term mortality reports, only the study reported by Marsk et al. [66] included only male surgical patients. Two unique study aspects were found in the studies by Johnson et al. [71] and Scott et al. [73]. To explore the safety and long-term survival of bariatric surgical patients who have diagnosed cardiovascular disease prior to their bariatric surgery, Johnson et al. retrospectively compared all-cause mortality of 349 bariatric patients to 903 morbidly obese surgical controls (i.e., non-bariatric surgery), where all patients (bariatric and controls) had a history of a cardiovascular event (myocardial infarction or stroke, which ever occurred first) prior to their bariatric or non-bariatric surgeries [71]. Scott et al. compared long-term cardiovascular events and all-cause mortality of post-bariatric surgical patients to patients who had undergone surgery for either orthopedic- or gastrointestinal-related procedures [73]. As previously indicated, Eliasson et al. matched 6132 RYGB patients with T2DM patients prior to surgery with 6132 control patients diagnosed with T2DM at the time of matching [79]. The first reported long-term mortality following bariatric surgery of MacDonald et al. was limited to type 2 diabetic patients who were seeking bariatric surgery [54]. As highlighted in Table 1, the types of bariatric surgical procedures employed in long-term mortality studies have primarily focused on Roux-en-Y gastric bypass, but have also incorporated gastric banding, biliopancreatic diversion, gastrojejunostomy, and sleeve. Finally, while all but one of the studies have reported on all-cause mortality (study by Tindle et al. [67] reported only on suicide-related mortality), many of the studies have also reported on deaths related to other causes such as cardiovascular disease, cancer, and suicides. Matching-related methods for mortality studies also included a variety of schemes. Due to the prospective nature of the SOS study, Sjöström et al. employed 18 variables to match surgical and nonsurgical participants [1, 82]. The Utah mortality study matched the year of surgery, date-of-birth, gender, BMI, and surgical date of the bariatric surgical patient to driver license applicants using the date of surgery to match with the year that the driver license was obtained [2]. As detailed in Table 1, matching techniques have included group matching with various control group schemes, propensity matching in two of the reported studies [69, 75], and matching by diabetic [54] or prior-to-surgery cardiovascular events [71] in bariatric and non-bariatric participants.
Long-Term Mortality Findings
Of particular interest is the fact that of all studies of long-term mortality following bariatric surgery where bariatric surgical patients have been compared to severely obese control subjects, the bariatric group has a reduced mortality when compared to the non-bariatric control group. The range of reduction in mortality rates of the obese patients in the bariatric surgery groups when compared to the obese control groups not undergoing surgery varied from 24 to 89 %. Obese patients undergoing bariatric surgery reduced their mortality rate or risk of death by approximately 51 %. Although Maciejewski et al. reported a 36 % reduction in mortality among veterans undergoing bariatric surgery compared to non-operated veteran patients (HR: 0.65, 95 % CI, 0.51–0.80), the difference in mortality between bariatric and control groups was no longer significant (HR: 0.83, 95 % CI, 0.64–1.39) when propensity matching was applied (1694 propensity matched patients). Four years after this report study by Maciejewski et al., Arterburn et al. expanded upon this previous research and matched (non-propensity) 2500 post-bariatric surgical veterans with 7462 non-operated veterans and reported a reduced mortality among the bariatric group of 55 % (HR, 0.45 95 % CI, 0.36–0.5) 1 to 5 years post-surgery and 53 % (HR, 0.47, 95 % CI, 0.39–0.58) for 5 to 14 years post-surgery when compared to obese controls [77].
The three studies investigating surgical and control patients with diagnosed pre-surgical diabetes [54; 79] or a major cardiovascular event [71] reported reduced mortality in the pre-surgical diabetic patients when compared to the severely obese diabetic controls (HR, 0.60 (surgical mortality rate 9 % vs. nonsurgical rate 28 %)) [54] (HR, 0.60 (surgical mortality rate 9 % vs. nonsurgical rate 28 %) [54] and HR, 0.42 (95% CI, 0.30-0.57; p<0.0001) [79] and an equally impressive reduction in mortality among the pre-surgical cardiovascular event patients compared to the previous cardiovascular event obese controls (HR, 0.60 (95 % CI, 0.36–0.99) [71]. As previously cited, Scott et al. also focused on disease-related mortality by comparing patients who had undergone orthopedic- or gastrointestinal-related surgeries to postoperative bariatric surgical patients. Following appropriate adjustments, the reported HR was 0.72 (95 % CI, 0.58–0.89) and 0.48 (95 % CI, 0.39–0.61) comparing bariatric to orthopedic and gastrointestinal surgical patients, respectively. With the exception of one study [76], when longer-term mortality of post-bariatric surgical patients has been compared with mortality rates of the general population, there is no significant long-term mortality reduction in the bariatric vs. control subjects. These studies have reported that the bariatric surgery cohort has a greater mortality when compared to the mortality rates of the general population [62, 66–68], with a HR of 1.4 to 1.5 when comparing the bariatric surgical group to obese control groups. The exception is the recently reported study by Telem et al. [76] where long-term observed mortality rate of bariatric surgical patients in New York state were reported to be 1.5 % compared to the predicted general population mortality rate (New York) of 2.1 % (p = 0.005).
Systematic Review and Meta-Analysis
In response to interest in the association of long-term mortality and bariatric surgery, systematic reviews and meta-analysis studies have more recently been reported [83, 84], as well as a review commentary [85] and a systematic review of completed suicide after bariatric surgery [86]. Pontiroli and Morabito, reviewing long-term mortality related to gastric banding and gastric bypass, conducted a meta-analysis of eight mortality studies whose publication year ranged from 1997 to 2007 [1, 2, 54, 55, 57, 59–61]. They reported reduced odds of all-cause mortality (odds ratio [OR], 0.55, 95 % CI, 0.49–0.63), of cardiovascular mortality (OR, 0.58, 95 % CI, 0.46–0.73) and of all-cause mortality (OR: 0.70, 95 % CI, 0.59–0.84) [84]. A systematic review and meta-analysis reported by Kwok et al. [83] included 14 bariatric surgery-related mortality studies [1, 2, 39, 52, 53, 55, 57, 59–61, 69, 70, 73, 87], two of which did not appear to be long-term in nature [53, 87] (assuming long-term to be mortality occurring at least 2 years post-surgery). The reduction in mortality among bariatric surgical patients compared to non-operated controls was OR, 0.48, 95 % CI, 0.35–0.64. In addition, they reported mortality reduction in myocardial infarction (OR, 0.46, 95 % CI, 0.30–0.69) and stroke (OR, 0.49, 95 % CI, 0.32–0.75) bariatric surgical patients compared to nonsurgical controls [83].
Externally Caused Deaths
One of the early reported long-term mortality studies (2007) reported a significant increase in externally caused deaths [2]. Externally caused deaths are defined as deaths such as suicides, accidents, poisonings of undetermined intent, and homicides. Published the same year as the aforementioned Utah study, Omalu et al. reported on death rates and causes of death following bariatric surgery among Pennsylvania residents [62]. Although cardiovascular-related deaths were the primary cause of long-term mortality, the authors noted a meaningful number of suicides and drug overdose-related deaths (45 deaths from 16,683 bariatric operations). Following this study reported by Omalu et al., Tindle et al. published the results of long-term follow-up of bariatric surgery and its association with risk of suicide [67]. Over a 10-year period (1995–2004), Tindle et al. reported “a substantial excess of suicides among all patients who had bariatric surgery in Pennsylvania” [67]. The suicide rate for post-bariatric surgical men was reported to be 13.7/10,000 compared to the Pennsylvania suicide rate of 2.5/10,000 and for post-bariatric surgical women the suicide rate was 5.2/10,000, compared to the Pennsylvania suicide rate of 0.6/10,000 [67]. Peterhänsel et al., further pursuing this topic, published a systematic review of completed suicide following bariatric surgery [86]. From a total of 36 bariatric surgery studies where completed suicide was reported, the authors used data from 28 of these studies to estimate suicide rate of 4.1/10,000 person-years (95 % CI, 3.2–5.1/10,000 person-years) [86], a rate higher than the general population. Although the reason for associated increased suicide and bariatric surgery is not clearly understood, there is an obvious need to better understand this important risk.
Life Expectancy
We identified three papers that estimated life expectancy (LE) gains or losses associated with bariatric surgery [88, 89, 90•]. The overall findings suggest that bariatric surgery is associated with increased life expectancy. Yet, there are several inconsistencies between recently-published and previous findings, suggesting a need to address some of the methodological inconsistencies and limitations that plausibly explain these inconsistencies. Nevertheless, the direct interpretability of gains/losses in life expectancy as an outcome measure, especially when reporting the effectiveness of bariatric surgery, is beneficial in a clinical setting. Many earlier studies of mortality risk associated with bariatric surgery have reported HRs as outcomes instead of using life expectancy. Correct interpretation of HRs is often difficult to communicate outside scientific community.
A recent paper by Schauer et al. (2015) estimated bariatric-associated life expectancies in obese patients with diabetes [90•]. They estimated changes in LE by estimating the LE differences of an obese person with diabetes undergoing surgery vs. a similar person not undergoing surgery. Gains of 6.7 and 6.5 years for a 45-year-old woman and man both with a BMI of 45 and no history of hypertension, coronary artery diseases (CAD), or congestive heart failure (CHF) were estimated, respectively. The absolute gains in LE for a 45-year-old woman and man continued to be as high as 6.7 and 5.4 years even when the patient had a history of hypertension, CAD, and CHF. The LE of a bariatric surgery patient with a history of hypertension, CAD, and CHF, however, remained shorter compared to a bariatric surgery patient with no history of these diseases. For example, the estimated LE of a 45-year-old woman undergoing surgery with no history of hypertension, CAD, or CHF was 38.4 years vs. only 22.3 years when the patient had a history of these diseases. Hence, while the absolute LE gains associated with bariatric surgery were nearly the same for patients with and without history of hypertension, CHF and CAD; the relative LE gains were higher for patients with history of these additional comorbidities. Another interpretation of the shorter LE of an obese diabetic bariatric surgery patient with history of additional comorbidities is that the surgery is unable to eliminate the excess mortality burden of the additional comorbidities when compared to an obese diabetic patient who does not have additional comorbidities.
The authors also reported that the gains in LE decreased as the BMI increased, and after the BMI of 62, a nonsurgical option was expected to achieve greater LE. Some of these findings of Schauer et al. 2015 [90•] seem inconsistent with their own findings published in 2010 [89]. In 2010, Schauer and colleagues had inferred that higher BMIs were associated with greater gains in LE [89]. Further, the magnitude of the LE gains estimated from their previous paper in 2010 was smaller (2.95 years for a 42-year-old woman with BMI of 45 and 2.57 years of gains for a 44-year-old man with BMI of 45). Interestingly, Schauer et al.’s 2010 findings are similar to findings from Pope et al. (2006) [88]. Pope and colleagues estimated bariatric surgery-associated LE gains of 2.6 years and 3.3 for a 40-year-old woman and man, respectively, with a BMI of 40.
Findings from all of these three papers were based on the Markov-based state transition models. In a Markov state transition, modeling framework outcomes or health states for cohorts of patients are simulated over a fixed period of time using at least two more data sources. In all of these papers where the mortality is the final health state, simulation ends when all the patients in the simulation have died. The different pieces of information used to develop these simulations include: 1) efficacy of bariatric surgery; 2) BMI-mortality association; and 3) the short-term 30-day mortality risk associated with bariatric surgery. Some of the inconsistencies in the findings may be attributed to methodological differences. For example, Schauer et al. 2015 [90•] estimated the efficacy of bariatric surgery on obese diabetic patients using data from three HMO research network sites, while in 2010, they estimated the efficacy based on findings of Adams et al. (2007) [2]. This led to at least two analytical differences. First, unlike their 2015 efficacy estimate, the estimated efficacy of bariatric surgery was based on an analysis that did not stratify for diabetic status of the patients. Second, the average length of follow-up while estimating the efficacy for the 2010 paper was 7.1 years while it was only 2 years for the 2015 paper. In addition to pursuing future analyses that may clarify some of these analytical inconsistencies, there may be opportunities to further refine these models and pursue more advanced/direct approaches to estimate LE gains [91, 92].
Conclusion and Research Gaps
Based upon multiple studies associating long-term mortality following bariatric surgery, the following findings have emerged. Bariatric surgical patients have: 1) significantly reduced long-term all-cause mortality when compared to severely obese non-bariatric surgical control groups; 2) greater mortality when compared to the general population, with the exception of one study; 3) reduced cardiovascular-, stroke-, and cancer-caused mortality when compared to severely obese non-operated controls; and 4) increased risk for externally caused death such as suicide.
The exact causal relationship between bariatric surgery and extended mortality when compared to the severely obese, non-bariatric surgery population is not known. However, multiple studies have reported on the long-term benefit/reduction of comorbidities following bariatric surgery [19, 39, 50, 93–99, 100•]. The link between comorbidity reduction in cardiovascular events and long-term mortality, for example, has been hypothesized and possible physiologic mechanisms have been proposed [99]. The degree to which these mechanisms are related to the significant and sustained weight loss achieved through bariatric surgery or to non-weight reduction effects are not clearly understood. Future investigation into the long-term weight loss and clinical outcome durability of bariatric surgery in association with long-term mortality are likely to provide additional understanding of the link between bariatric surgery and reduced long-term mortality. Finally, listed below are a number of gaps related to this topic for which research findings would be beneficial.
-
Is duration of severe obesity prior to surgery more important than age at surgery in relation to post-surgical mortality?
-
Do long-term mortality outcomes vary in relation to bariatric surgical procedures?
-
Does improved mortality equal improved long-term quality of life?
-
Can robust animal models (or well-designed human studies) help disentangle energy-restricted weight loss from physiologic consequences of gastric bypass surgery on reduced mortality?
-
Why do post-surgical bariatric surgery patients have higher mortality from suicide, accidents, and poisonings? (Are current pre-surgical psychological evaluations sufficient to exclude at-risk patients? Are post-surgical counseling strategies needed?)
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61.
Bray GA. The missing link - lose weight, live longer. N Engl J Med. 2007;357(8):818–20.
Yaari S, Goldbourt U. Voluntary and involuntary weight loss: associations with long term mortality in 9,228 middle-aged and elderly men. Am J Epidemiol. 1998;148(6):546–55.
Ostergaard JN, Gronbaek M, Schnohr P, Sorensen TI, Heitmann BL. Combined effects of weight loss and physical activity on all-cause mortality of overweight men and women. Int J Obes (Lond). 2010;34(4):760–9.
Gregg EW, Gerzoff RB, Thompson TJ, Williamson DF. Intentional weight loss and death in overweight and obese U.S. adults 35 years of age and older. Ann Intern Med. 2003;138(5):383–9.
Hu FB, Willett WC, Li T, Stampfer MJ, Colditz GA, Manson JE. Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med. 2004;351(26):2694–703.
Adams TD, Davidson LE, Litwin SE, Hunt SC. Gastrointestinal surgery: cardiovascular risk reduction and improved long-term survival in patients with obesity and diabetes. Curr Atheroscler Rep. 2012;14(6):606–15.
Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ, Colditz GA. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012. JAMA Surg. 2014;149(3):275–87.
Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–9.
National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults--the evidence report. Obes Res. 1998;6 Suppl 2:51S–209S.
Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–45.
Chang SH, Pollack LM, Colditz GA. Life years lost associated with obesity-related diseases for U.S. non-smoking adults. PLoS One. 2013;8(6):e66550.
Willett WC, Dietz WH, Colditz GA. Guidelines for healthy weight. N Engl J Med. 1999;341(6):427–34.
de Berrington Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363(23):2211–9.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82.
Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355(8):763–78.
McTigue K, Larson JC, Valoski A, et al. Mortality and cardiac and vascular outcomes in extremely obese women. JAMA. 2006;296(1):79–86.
Sjostrom L. Review of the key results from the Swedish obese subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219–34.
Nilsson PM, Nilsson JA, Hedblad B, Berglund G, Lindgarde F. The enigma of increased non-cancer mortality after weight loss in healthy men who are overweight or obese. J Intern Med. 2002;252(1):70–8.
Strandberg TE, Strandberg AY, Salomaa VV, et al. Explaining the obesity paradox: cardiovascular risk, weight change, and mortality during long-term follow-up in men. Eur Heart J. 2009;30(14):1720–7.
Doehner W, Erdmann E, Cairns R, et al. Inverse relation of body weight and weight change with mortality and morbidity in patients with type 2 diabetes and cardiovascular co-morbidity: an analysis of the PROactive study population. Int J Cardiol. 2012;162(1):20–6.
Pamuk ER, Williamson DF, Serdula MK, Madans J, Byers TE. Weight loss and subsequent death in a cohort of U.S. adults. Ann Intern Med. 1993;119(7 Pt 2):744–8.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371(9612):569–78.
Reeves GK, Pirie K, Beral V, et al. Cancer incidence and mortality in relation to body mass index in the million women study: cohort study. BMJ. 2007;335(7630):1134.
Samanic C, Chow WH, Gridley G, Jarvholm B, Fraumeni Jr JF. Relation of body mass index to cancer risk in 362,552 Swedish men. Cancer Causes Control. 2006;17(7):901–9.
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17):1625–38.
Williamson DF, Pamuk E, Thun M, Flanders D, Byers T, Heath C. Prospective study of intentional weight loss and mortality in never-smoking overweight US white women aged 40–64 years. Am J Epidemiol. 1995;141(12):1128–41.
Williamson DF, Thompson TJ, Thun M, Flanders D, Pamuk E, Byers T. Intentional weight loss and mortality among overweight individuals with diabetes. Diabetes Care. 2000;23(10):1499–504.
Wannamethee SG, Shaper AG, Whincup PH, Walker M. Characteristics of older men who lose weight intentionally or unintentionally. Am J Epidemiol. 2000;151(7):667–75.
Lewis CE, McTigue KM, Burke LE, et al. Mortality, health outcomes, and body mass index in the overweight range: a science advisory from the American heart association. Circulation. 2009;119(25):3263–71.
Yanovski SZ, Yanovski JA. Obesity. N Engl J Med. 2002;346(8):591–602.
Pamuk ER, Williamson DF, Madans J, Serdula MK, Kleinman JC, Byers T. Weight loss and mortality in a national cohort of adults, 1971–1987. Am J Epidemiol. 1992;136(6):686–97.
McTigue KM, Harris R, Hemphill B, et al. Screening and interventions for obesity in adults: summary of the evidence for the U.S. preventive services task force. Ann Intern Med. 2003;139(11):933–49.
Avenell A, Broom J, Brown TJ, et al. Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement. Health Technol Assess. 2004;8(21):iii–iv. 1–182.
Wadden TA, Volger S, Sarwer DB, et al. A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med. 2011;365(21):1969–79.
Yanovski SZ, Yanovski JA. Long-term drug treatment for obesity: a systematic and clinical review. JAMA. 2014;311(1):74–86.
Li Z, Maglione M, Tu W, et al. Meta-analysis: pharmacologic treatment of obesity. Ann Intern Med. 2005;142(7):532–46.
Adams TD, Davidson LE, Litwin SE, et al. Health benefits of gastric bypass surgery after 6 years. JAMA. 2012;308(11):1122–31.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–76.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366(17):1577–85.
Look ARG, Wing RR, Bolin P, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369(2):145–54.
Uusitupa M, Peltonen M, Lindstrom J, et al. Ten-year mortality and cardiovascular morbidity in the Finnish diabetes prevention study—secondary analysis of the randomized trial. PLoS One. 2009;4(5):e5656.
Li G, Zhang P, Wang J, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing diabetes prevention study: a 20 years follow-up study. Lancet. 2008;371(9626):1783–9.
Nissen SE, Nicholls SJ, Wolski K, et al. Effect of rimonabant on progression of atherosclerosis in patients with abdominal obesity and coronary artery disease: the STRADIVARIUS randomized controlled trial. JAMA. 2008;299(13):1547–60.
James WP, Caterson ID, Coutinho W, et al. Effect of sibutramine on cardiovascular outcomes in overweight and obese subjects. N Engl J Med. 2010;363(10):905–17.
Flum DR, Belle SH, King WC, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361(5):445–54.
Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Attiah MA, Halpern CH, Balmuri U, et al. Durability of Roux-en-Y gastric bypass surgery: a meta-regression study. Ann Surg. 2012;256(2):251–4.
Vest AR, Heneghan HM, Agarwal S, Schauer PR, Young JB. Bariatric surgery and cardiovascular outcomes: a systematic review. Heart. 2012;98(24):1763–77.
Sjostrom L. Bariatric surgery and reduction in morbidity and mortality: experiences from the SOS study. Int J Obes (Lond). 2008;32 Suppl 7:S93–7.
Arterburn D, Bogart A, Coleman KJ, et al. Comparative effectiveness of bariatric surgery vs. nonsurgical treatment of type 2 diabetes among severely obese adults. Obes Res Clin Pract. 2013;7(4):e258–68.
Johnson BL, Blackhurst DW, Latham BB, et al. Bariatric surgery is associated with a reduction in major macrovascular and microvascular complications in moderately to severely obese patients with type 2 diabetes mellitus. J Am Coll Surg. 2013;216(4):545–56. discussion 556–548.
MacDonald Jr KG, Long SD, Swanson MS, et al. The gastric bypass operation reduces the progression and mortality of non-insulin-dependent diabetes mellitus. J Gastrointest Surg. 1997;1(3):213–20. discussion 220.
Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240(3):416–23. discussion 423–414.
White S, Brooks E, Jurikova L, Stubbs RS. Long-term outcomes after gastric bypass. Obes Surg. 2005;15(2):155–63.
Flum DR, Dellinger EP. Impact of gastric bypass operation on survival: a population-based analysis. J Am Coll Surg. 2004;199(4):543–51.
Zhang W, Mason EE, Renquist KE, Zimmerman MB, Contributors I. Factors influencing survival following surgical treatment of obesity. Obes Surg. 2005;15(1):43–50.
Busetto L, Mirabelli D, Petroni ML, et al. Comparative long-term mortality after laparoscopic adjustable gastric banding versus nonsurgical controls. Surg Obes Relat Dis. 2007;3(5):496–502. discussion 502.
Sowemimo OA, Yood SM, Courtney J, et al. Natural history of morbid obesity without surgical intervention. Surg Obes Relat Dis. 2007;3(1):73–7. discussion 77.
Peeters A, O’Brien PE, Laurie C, et al. Substantial intentional weight loss and mortality in the severely obese. Ann Surg. 2007;246(6):1028–33.
Omalu BI, Ives DG, Buhari AM, et al. Death rates and causes of death after bariatric surgery for Pennsylvania residents, 1995 to 2004. Arch Surg. 2007;142(10):923–8. discussion 929.
Marsk R, Freedman J, Tynelius P, Rasmussen F, Naslund E. Antiobesity surgery in Sweden from 1980 to 2005: a population-based study with a focus on mortality. Ann Surg. 2008;248(5):777–81.
Perry CD, Hutter MM, Smith DB, Newhouse JP, McNeil BJ. Survival and changes in comorbidities after bariatric surgery. Ann Surg. 2008;247(1):21–7.
Arterburn D, Livingston EH, Schifftner T, Kahwati LC, Henderson WG, Maciejewski ML. Predictors of long-term mortality after bariatric surgery performed in Veterans affairs medical centers. Arch Surg. 2009;144(10):914–20.
Marsk R, Naslund E, Freedman J, Tynelius P, Rasmussen F. Bariatric surgery reduces mortality in Swedish men. Br J Surg. 2010;97(6):877–83.
Tindle HA, Omalu B, Courcoulas A, Marcus M, Hammers J, Kuller LH. Risk of suicide after long-term follow-up from bariatric surgery. Am J Med. 2010;123(11):1036–42.
Plecka Ostlund M, Marsk R, Rasmussen F, Lagergren J, Naslund E. Morbidity and mortality before and after bariatric surgery for morbid obesity compared with the general population. Br J Surg. 2011;98(6):811–6.
Maciejewski ML, Livingston EH, Smith VA, et al. Survival among high-risk patients after bariatric surgery. JAMA. 2011;305(23):2419–26.
Miranda WR, Goel K, Batsis JA, et al. Long-term mortality in patients undergoing bariatric surgery compared to patients managed non-operatively for morbid obesity. Eur Heart J. 2012;33:494.
Johnson RJ, Johnson BL, Blackhurst DW, et al. Bariatric surgery is associated with a reduced risk of mortality in morbidly obese patients with a history of major cardiovascular events. Am Surg. 2012;78(6):685–92.
Diniz Mde F, Moura LD, Kelles SM, Diniz MT. Long-term mortality of patients submitted to Roux-en-Y gastric bypass in public health system: high prevalence of alcoholic cirrhosis and suicides. Arq Bras Cir Dig. 2013;26 Suppl 1:53–6.
Scott JD, Johnson BL, Blackhurst DW, Bour ES. Does bariatric surgery reduce the risk of major cardiovascular events? A retrospective cohort study of morbidly obese surgical patients. Surg Obes Relat Dis. 2013;9(1):32–9.
Bruschi Kelles SM, Diniz MF, Machado CJ, Barreto SM. Mortality rate after open Roux-in-Y gastric bypass: a 10 years follow-up. Braz J Med Biol Res. 2014;47(7):617–25.
Guidry CA, Davies SW, Sawyer RG, Schirmer BD, Hallowell PT. Gastric bypass improves survival compared with propensity-matched controls: a cohort study with over 10 years follow-up. Am J Surg. 2015;209(3):463–7.
Telem DA, Talamini M, Laurie Shroyer A, et al. Long-term mortality rates (>8 years) improve as compared to the general and obese population following bariatric surgery. Surg Endosc. 2015;29(3):529–36.
Arterburn DE, Olsen MK, Smith VA, et al. Association between bariatric surgery and long-term survival. JAMA. 2015;313(1):62–70.
Morgan DJ, Ho KM, Armstrong J, Litton E. Long-term clinical outcomes and health care utilization after bariatric surgery: a population-based study. Ann Surg. 2015;262(1):86–92.
Eliasson B, Liakopoulos V, Franzén S, Näslund I, Svensson A, Ottosson J, Gudbjörnsdottir S. Cardiovascular disease and mortality in patients with type 2 diabetes after bariatric surgery in Sweden: a nationwide, matched, observational cohort study. Lancet Diabetes Endocrinol. 2015. doi:10.1016/S2213-8587(15)00334-4.
Yan LL, Daviglus ML, Liu K, et al. Midlife body mass index and hospitalization and mortality in older age. JAMA. 2006;295(2):190–8.
Maggard MA, Shugarman LR, Suttorp M, et al. Meta-analysis: surgical treatment of obesity. Ann Intern Med. 2005;142(7):547–59.
Sjostrom L, Larsson B, Backman L, et al. Swedish obese subjects (SOS) - recruitment for an intervention study and a selected description of the obese state. Int J Obes. 1992;16(6):465–79.
Kwok CS, Pradhan A, Khan MA, et al. Bariatric surgery and its impact on cardiovascular disease and mortality: a systematic review and meta-analysis. Int J Cardiol. 2014;173(1):20–8.
Pontiroli AE, Morabito A. Long-term prevention of mortality in morbid obesity through bariatric surgery. A systematic review and meta-analysis of trials performed with gastric banding and gastric bypass. Ann Surg. 2011;253(3):484–7.
Chang J, Wittert G. Effects of bariatric surgery on morbidity and mortality in severe obesity. Int J Evid Based Healthc. 2009;7(1):43–8.
Peterhansel C, Petroff D, Klinitzke G, Kersting A, Wagner B. Risk of completed suicide after bariatric surgery: a systematic review. Obes Rev. 2013;14(5):369–82.
Gentileschi P, D’Eletto M, D’Ugo S, et al. Effect of bariatric surgery on comorbidities vs medical treatment in a cohort of morbidly obese patients: a prospective study. Gastroenterology. 2012;142(5):S1102.
Pope GD, Finlayson SR, Kemp JA, Birkmeyer JD. Life expectancy benefits of gastric bypass surgery. Surg Innov. 2006;13(4):265–73.
Schauer DP, Arterburn DE, Livingston EH, Fischer D, Eckman MH. Decision modeling to estimate the impact of gastric bypass surgery on life expectancy for the treatment of morbid obesity. Arch Surg. 2010;145(1):57–62.
Schauer DP, Arterburn DE, Livingston EH, et al. Impact of bariatric surgery on life expectancy in severely obese patients with diabetes: a decision analysis. Ann Surg. 2015;261(5):914–9. Estimates life expectancy gains associated with bariatric surgery on severely obese patients with diabetes. Estimates are also generated for patients with additional co-morbidities such as hypertension. Estimates are generated from Markov-state transition based simulation model that uses recent primary individual-level data (2000 onwards) from three different data sources.
Robertson HT, de los Campos G, Allison DB. Turning the analysis of obesity-mortality associations upside down: modeling years of life lost through conditional distributions. Obesity (Silver Spring). 2013;21(2):398–404.
Brenner H, Gefeller O, Greenland S. Risk and rate advancement periods as measures of exposure impact on the occurrence of chronic diseases. Epidemiology. 1993;4(3):229–36.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Ricci C, Gaeta M, Rausa E, Macchitella Y, Bonavina L. Early impact of bariatric surgery on type II diabetes, hypertension, and hyperlipidemia: a systematic review, meta-analysis and meta-regression on 6,587 patients. Obes Surg. 2014;24(4):522–8.
Sjostrom L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307(1):56–65.
Poirier P, Cornier MA, Mazzone T, et al. Bariatric surgery and cardiovascular risk factors: a scientific statement from the American heart association. Circulation. 2011;123(15):1683–701.
Athyros VG, Tziomalos K, Karagiannis A, Mikhailidis DP. Cardiovascular benefits of bariatric surgery in morbidly obese patients. Obes Rev. 2011;12(7):515–24.
Tee MC, Cao Y, Warnock GL, Hu FB, Chavarro JE. Effect of bariatric surgery on oncologic outcomes: a systematic review and meta-analysis. Surg Endosc. 2013;27(12):4449–56.
Boido A, Ceriani V, Cetta F, Lombardi F, Pontiroli AE. Bariatric surgery and prevention of cardiovascular events and mortality in morbid obesity: mechanisms of action and choice of surgery. Nutr Metab Cardiovasc Dis. 2015;25(5):437–43.
Arterburn DE, Courcoulas AP. Bariatric surgery for obesity and metabolic conditions in adults. BMJ. 2014;349:g3961. Examines the long-term mortality associated with bariatric surgery as compared to matched controls in the VA population. Unlike their previous findings, which were based on shorter length of follow-up, they estimated significant survival advantage in those undergoing bariatric surgery in this study. Further, they also report that bariatric surgery in the earlier time period had significantly higher postoperative mortality compared to surgery in the more recent period.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ted D. Adams declares grants from NIH-NIDDK; honoraria from Ethicon J&J; and personal fees from NIH and Ethicon J&J for travel.
Tapan S. Mehta declares personal fees for consulting for Gjording Fouser PLLC and PK LifeScience; money paid to an institution for employment with NIH, NIDDR, and CDC; and honoraria for being a reviewer for NSF.
Lance E. Davidson and Steven C. Hunt declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All studies by Ted Adams, Lance Davidson, and Steve Hunt involving human subjects were performed after approval by the appropriate institutional review boards. When required, written informed consent was obtained from all participants.
Additional information
This article is part of the Topical Collection on Lipid and Metabolic Effects of Gastrointestinal Surgery
Rights and permissions
About this article
Cite this article
Adams, T.D., Mehta, T.S., Davidson, L.E. et al. All-Cause and Cause-Specific Mortality Associated with Bariatric Surgery: A Review. Curr Atheroscler Rep 17, 74 (2015). https://doi.org/10.1007/s11883-015-0551-4
Published:
DOI: https://doi.org/10.1007/s11883-015-0551-4