Abstract
Background
Obesity is successfully treated by bariatric operations, but some patients need reoperations. No large national studies are available to evaluate the safety and efficacy after reoperative bariatric surgery.
Methods
Data from June 2007 through March 2012 from the Bariatric Outcomes Longitudinal Database were queried for safety and efficacy of reoperations and compared to those who had initial bariatric operations but did not undergo reoperations. Reoperations were subdivided into corrective operations and conversions.
Results
Out of 449,753 bariatric operations, 28,720 (6.3 %) underwent reoperations of which 19,970 (69.5 %) were corrective and 8,750 (30.5 %) were conversions. The conversion group compared to primary operations was older (47.63 ± 10.8 vs. 45.5 ± 11.8 years), had less males (13.5 vs. 21.3 %), and had more African Americans (14.6 vs. 12 %). Comparing primary operations to corrective and conversions operations, respectively, the following were observed: length of stay (1.78 ± 4.95 vs. 2.04 ± 6.44 and 2.86 ± 4.58 days), severe adverse events at 30 days (1.6 vs. 1.7 and 3.3 %), severe adverse events at 1 year (2.15 vs. 1.9 and 3.61 %), percent excess weight loss at 1 year (43.2 vs. 35.9 ± 92.4 and 39.3 ± 39.9 %), 30-day mortality rate (0.1 vs. 0.12 and 0.21 %), and 1-year mortality rate (0.17 vs. 0.24 and 0.31 %). Comorbidities were resolved after both primary operations and reoperations.
Conclusions
Most bariatric surgery patients do not need reoperations. Among those who do, the complication rate is low and outcomes are clinically comparable to primary procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Obesity is a chronic disease that has been successfully treated by different primary bariatric operations. These operations, in order of increasing complexity, include the laparoscopic adjustable gastric banding (AGB), the sleeve gastrectomy (SG), the Roux-en-Y gastric bypass (RYGB), and the biliopancreatic diversion with or without the duodenal switch (BPD ± DS). In general, higher complexity procedures are associated with greater weight loss and better resolution of certain comorbidities such as diabetes and hypertension.1–3 Patients who are heavier and have more severe comorbidities typically receive the higher complexity procedures.3 However, rates of complications also increase with increasing complexity of the operation3,4, and currently, there is limited data to optimally match patients’ baseline characteristics to a bariatric operation that would be ideal for them. Therefore, patients and surgeons often choose a less severe operation at the outset with the hope of avoiding serious complications. However, the initial operation may not result in adequate weight loss or resolution of comorbid conditions. In some patients, after initial success, weight regain may occur and they may develop new comorbid conditions or have recurrence of the comorbidities that had been previously resolved. In other patients, complications may develop from their original operation necessitating further surgery such as pouch dilation or a gastrogastric fistula.3 Complications have traditionally been covered by payors. However, requests for reoperations due to partial treatment effect for weight loss or resolution of comorbidities are frequently denied. Several factors may contribute toward denial of bariatric reoperations for conversions including higher reported complication rates after such operations.5,6 Uncertain benefits after a conversion operation and a tendency to blame the patient for noncompliance with the prescribed diet and exercise regimens are other potential factors. Most of the data on the outcomes after reoperative bariatric surgery comes from single institution studies, and therefore, the American Society for Metabolic and Bariatric Surgery (ASMBS) convened a task force to address issues related to reoperative bariatric surgery. The task force conducted a systematic review of the literature on reoperative bariatric surgery and identified a paucity of high-quality data. Most studies were single institution and had small numbers of subjects.7 Therefore, the ASMBS decided to examine patterns of reoperations and determine safety and efficacy of reoperations from large databases such as the Bariatric Outcomes Longitudinal Database (BOLD). This is a large multi-institutional bariatric surgery-specific database in which data was submitted from June 2007 through March 2012 by 1,029 surgeons and 709 hospitals participating in the Bariatric Surgery Centers of Excellence (BSCOE) program. The project was funded by an unrestricted grant by Covidien. The funding agency did not have any input in the study design, data extraction, results, or preparation of the manuscripts.
Methods
A task force was convened and comprised of the executive leadership and chairs of several key committees including access to care, clinical issues, quality improvement, research, insurance committee, state chapters, and other at-large members that represented private and academic institutions. The task force obtained data from BOLD®, deidentified it, and obtained a waiver from the Duke University Institutional Review Board (IRB). Patients were included if they were 18 years or older and had either a primary bariatric operation or a reoperation for any reason, including complications or inadequate results.
Baseline variables collected prior to the first operation included patient age at the time of operation, gender, ethnicity, body mass index (BMI), American Society of Anesthesiologists (ASA) class, excess body weight (EBW) and percent excess body weight (% EBW), and comorbid conditions at baseline. Intraoperative data included primary procedure, surgical approach, and adverse events. Postoperative outcomes extracted at 30 days and at 1 year included EBW, percent EBWL, percent weight loss, BMI, resolution of comorbidities, adverse events (AE), and severe adverse events (SAE). Weight loss and resolution of comorbidities were reported only at 1 year (defined as a visit closest to 365 days within a window of ±180 days), whereas SAE and mortality were reported at 30 days and 1 year. Mortality was a SAE but was also reported separately.
Data in BOLD were recorded on 134 different AEs on patients undergoing bariatric operations. A subset of these AEs was designated as SAE. These included cardiac arrest, myocardial infarction, heart failure and pulmonary edema, death, bleeding, liver failure, multisystem organ failure, sepsis, anastomotic leakage, stroke, pneumothorax, pulmonary embolism, respiratory failure, renal failure, evisceration, deep venous thrombosis, etc. Due to the low incidence of individual types of SAE, these were reported as a composite. In BOLD, comorbid conditions were graded on a severity scale. However, for this analysis, the scale was converted to a binary scale and analyzed as either the presence or absence of comorbid conditions based on whether patients were recorded as using medications or a device to treat the comorbid condition.
The ASMBS Task Force also refined definitions for reoperative bariatric surgery. Any operation after the first bariatric operation which qualified toward center of excellence volume requirements was considered a reoperation. Reoperations were further divided into corrective operations or conversions. An operation was considered corrective when complications or incomplete treatment effect of a previous bariatric operation was addressed but the initial operation was not changed. Conversions involved changing an index bariatric operation (first operation) to a different type of bariatric operation, and reversal restored original anatomy.
For the purposes of this manuscript, primary operations were defined as those bariatric operations in which a reoperation was not required. If a reoperation was required, then the first operation was considered the index operation, and the second operation was considered the reoperation (either corrective or conversion).
The following methodology was used to conduct the analysis. First, data were divided into operations that required a reoperation and those that did not. The group that underwent reoperations was then divided into two subgroups: the corrective operations and the conversions. In the corrective subgroup, the index operation and the reoperation were listed by the same name, and in the conversions, the reoperation had a different name from the index operation. The primary operations were then compared to corrective operations and conversions using descriptive statistics and t test for continuous variables and chi-square test for categorical variables.
Results
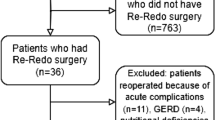
There were a total of 449,473 bariatric operations in the database of which 420,753 (93.6 %) operations had no further reoperations (primary operations) while 28,270 (6.3 %) underwent reoperations. The reoperations were further subdivided into corrective operations (n = 19,970, 69.5 %) and conversions (n = 8,750, 30.5 %) (Fig. 1). When comparing the primary operation group to the conversion group, the mean age of conversion patients was older by 2 years (45 ± 11.8 vs. 47.63 ± 10.8 years), and corrective operation patients were intermediate in age (46.22 ± 11.4). Fewer males (13.5 %) underwent conversion operations compared to either primary operations (21.3 %) or corrective operations (15.7 %). While a greater proportion of African Americans underwent conversions (14.6 %) compared to primary operations (12 %) or corrective operations (13.6 %), fewer Hispanics underwent conversions (6.45 %) compared to primary operations (7.4 %) (Table 1). Most patients in both the primary operation group and the reoperations group were between 31 and 60 years of age (78 %) and the rest were less than 30 (11 %) or greater than 60 years old (11 and 12 %, respectively). The distribution of patients by age for the primary procedures and the reoperations is shown in Fig. 2.
The primary bariatric operations were RYGB (n = 204,705, 49.1 %), AGB (n = 153,142, 36.5 %), SG (n = 42,178, 10 %), and BPD ± DS (n = 4,260, 1 %), and the rest were a miscellaneous category referred to as “other operations.” There were 8,750 conversions. The index operations and the type of operation to which they were converted were as follows: AGB was the index operation in 57.5 % (n = 4,766) of cases, and 63.5 % (n = 3,029) of these were converted to a RYGB. The rest were converted to SG (n = 1,616, 33.9 %) and BPD ± DS (n = 115, 2.4 %). Although vertical banded gastroplasty (VBG) is no longer performed, this category comprised 15.8 % (n = 1,385) of all conversions and most of these were converted to a RYGB (n = 1,194, 86.2 %). The RYGB was the third most often converted operation (13.9 %, n = 1,215) of which 78 % (n = 949) were listed as being converted to AGB. This most likely represented the addition of an AGB to the initial RYGB (band over bypass) as opposed to reversing the RYGB and then performing an AGB (Table 2). Among the 19,970 corrective operations, 10,739 (54 %) were performed within the first postoperative year suggesting that approximately half the complications occurred in the first year and the rest thereafter.
Compared to primary operations, the length of stay (LOS) was longer (p < 0.001) in patients undergoing corrections (1.8 ± 4.9 vs. 2.04 ± 6.44 days) and conversions (2.86 ± 4.58 days). The number of cases with LOS ≤1 day was 12,146 (60 %) for corrections and 2,508 (29 %) for conversions. Weight loss outcomes after primary bariatric operations, conversions, and corrective operations are shown in Table 3. Mean % EBWL at 1 year was 43.5 % after primary operation, 39.3 % after conversions, and 35.9 % after corrective operations. Following conversion to RYGB, AGB, SG, and BPD ± DS, % EWL 1 year was 42.2, 21.6, 33.3, and 43.9 %, respectively. The percent change from baseline in the use of medications or oral appliance for treatment of comorbid conditions after primary operations, conversions, and corrective operations is shown in Table 4. The percentage decline in patients who were taking antihypertensive medications at 1 year was 53.2 % after primary operations, 50.34 % after conversions, and 49.2 % after corrective operations. The percentage decline in patients who were taking medication for diabetes was 72.5 % after primary operations, 68.6 % after conversions, and 64.8 % after corrective operations. For sleep apnea, a 66.6 % decline was seen in the use of oral appliance after primary operation, 59.3 % after conversions, and 60.92 % after reoperation. Similarly, a large percentage of patients were not taking their gastroesophageal reflux disease (GERD) and lipid-lowering medications after primary operations and reoperations (Table 4).
The 30-day mortality rate for corrective operations compared to primary bariatric operations was not significantly higher (0.12 %, n = 23 vs. 0.1 %, n = 408, p < 0.001) but was significantly higher for conversions compared to primary operations (0.21 %, n = 18 vs. 0.1 %, n = 408). The 1-year mortality rate for corrective operations (0.24 %, n = 47) also not statistically significant higher compared to primary operations (0.17 %, n = 704) but, was significant for conversions compared to primary operations (0.31 %, n = 27). Similarly, severe adverse events at 30 days for corrections (1.66 %, n = 332) were not significantly higher compared to those for primary operations (1.61 %, n = 6,774) but were significantly higher for conversions (3.26 %, n = 285). The 1-year rate for severe adverse events showed the same pattern (Table 5).
Discussion
Our data shows that 6.35 % of the operations in BOLD were reoperations and were performed with low morbidity and mortality, with good weight loss and resolution of comorbid conditions. In comparing patients who underwent primary operations to those who underwent reoperations, we found that more females and African Americans underwent conversions. A previous study from BOLD has shown that among all patients obtaining bariatric surgery, the proportion of Caucasians and African Americans was 78 and 10.5 % respectively.8 In our study, the percentage of Caucasians obtaining reoperations was 78.7 %, while the percentage of African Americans obtaining reoperations was 13.9 %. The Longitudinal Assessment of Bariatric Surgery (LABS) study also reported that African Americans underwent more reoperations.9 African Americans have lower weight loss and resolution of comorbidity after RYGB,10 and this may account for a higher reoperation rate in African Americans. On the other hand, the percentage of Hispanics undergoing reoperation was slightly lower. This corroborates with a previous study that shows that Hispanics have higher weight loss and better resolution of comorbid conditions after the initial bariatric operation.10
Also, in this series, there were noticeably fewer males (15 %) who obtained reoperations compared to 21 % males in the primary group. Reports of gender-specific differences after bariatric operations have shown variable results. In some studies, women lost less weight compared to men,11 whereas in others, there was no statistical difference12 or no greater weight loss was observed in women with certain types of operations such as restrictive procedures compared to men.13 Therefore, it is unclear whether men obtained fewer reoperations because of satisfactory results or if they were more reluctant to seek a reoperation compared to women, as may be the case with initial bariatric operations.
In this study, elderly patients (>60 years of age) comprised 11 % of the primary and 12 % of the reoperative group of patients. Elderly patients have previously shown to be at a higher risk of suffering from complications after bariatric surgery.14,15 In a recent study, Gebhart et al. (SOARD, Elsevier, April, 2014, epub ahead of print) evaluated data from the University HealthSystem Consortium (UHC) database and noted that the number of elderly (>60 years of age) obtaining bariatric surgery performed in the USA has risen from 2.7 % of all bariatric operations from 1999 to 2005 to 10 % in the period from 2009 to 2013. In our study, patients who were more than 60 years of age underwent reoperations at a higher rate of 12 %. A slightly higher representation of elderly patients would be expected in this series because centers contributing data to BOLD were approved by Centers for Medicaid and Medicare to perform operations on elderly patients. An increase in initial bariatric operations in the elderly implies that these patients will also need more reoperations. Gebhart et al. found that although mortality of elderly patients was still higher than nonelderly patients in the period from 2009 to 2013 (0.11 vs. 0.05 %), it had declined to levels below the nonelderly seen in 1999–2005. These findings suggest an overall improvement in the rates of morbidity and mortality after bariatric operations over the last few years even for higher risk population. We did not specifically examine complication rates by age but would guess that in experienced centers, such as those meeting criteria for centers of excellence, morbidity and mortality would be equivalent or possibly lower.
When estimating the distribution of reoperations from the time interval between index operations and reoperations, 54 % of the corrections were performed within the first year after the index operation. It is likely that many of these operations were related to complications. However, conversions to other bariatric operations are also possible in the first year such as for band intolerance or a leak or stricture from SG, which are often converted to RYGB. Therefore, reoperations in the first year are most likely due to complications and not necessarily for inadequate weight loss or poor resolution of comorbid conditions. In attributing weight loss or resolution of comorbid conditions to the effectiveness of corrective operations, such factors need to be considered. Weight loss and comorbidity resolution following a bariatric operation is typically rapid in the first year and then stabilizes.3,11 Following this initial period of success, there is a gradual increase in weight and a new balance is achieved at a somewhat higher threshold over the next 2 to 3 years but at a level that still contributes to good resolution of comorbidity and improved quality of life.
However, some patients do not have satisfactory weight loss after the index operation. In others, weight regain continues with return of comorbid conditions after initial success and requires reevaluation for additional surgical intervention, as was found in the LABS study.3 Occasionally, such failure may be the result of a leak in the band, a large stomach pouch, or a gastrogastric fistula that can be corrected with a reoperation. Although noncompliance with diet and exercise regimens does play a role, weight gain and recurrence of comorbid conditions may occur despite patient compliance because of a patient’s inherent biology. In these circumstances, a more aggressive bariatric procedure may be indicated to provide effective therapy. In this study, the overall reoperation rate was 6.35 % and speaks to the success of the initial bariatric operation with a large percentage of patients coming off medications for comorbid conditions. In addition, the percentage of patients using medications or an oral appliance also declined 1 year after the reoperation, and both corrections and conversions were performed with relatively safety compared to the primary operations. The 30-day and 1-year mortality rate for all conversions was 0.21 and 0.31 %, respectively, and although statistically significant, it was not that much higher than a mortality rate of 0.1 and 0.17 % for primary operations from a clinical standpoint. This difference was statistically not significant for primary operations compared to corrective operations. A word of caution is advised when interpreting results from large databases. Statistical significance is often achieved due to a large sample size, but the clinician must also assess if these results are clinically significant. The results of this study provide the clinician with outcomes after reoperative surgery that could be used in counseling patients appropriately and suggest that reoperative surgery is overall safe. This is different from some single institution and pooled series that have reported a high complication rate for revisions despite good weight loss. In a study by Himpens et al., 70 patients underwent a new laparoscopic procedure for poor weight loss or weight regain after a laparoscopic Roux-en-Y gastric bypass. The patients lost very good weight but reported a complication rate of 20.7 %, a reoperation rate of 7.3 %, and an overall leak rate of 12.1 %.5 In a meta-analysis by Buchwald et al., the overall mortality rate of revision operations was as high as 1.65 %.4 This has likely contributed to reluctance on the part of bariatric surgeons to perform reoperations and for insurance carriers to approve them. A higher complication rate may have been historic as surgeons were learning new laparoscopic techniques for these complex operations that have a steep learning curve.16–18 Established surgeons have by now overcome their learning curve, while the new generation of surgeons is learning these operations in fellowship training. It has been shown that fellowship-trained surgeons in their first year after training will have a low morbidity and mortality rate.19 Therefore, with greater familiarity with both primary and revision operations, surgeons with adequate experience in the centers of excellence program were able to perform reoperations with relatively low risk as shown in this study.
We also found that mean % EBWL after conversion to a different bariatric operation was 39.3 % and was 35.9 % after a corrective operation. Although this % EBWL was lower than that after a primary operation (43.5 %), it was still substantial and excellent weight loss. However, not all reoperations will result in further weight loss or resolution of comorbidity. Restorative operations necessitated by intolerable side effects or complications of the index procedure such as removal of the laparoscopic adjustable gastric band for band intolerance or dilated esophagus, or reversing a duodenal switch or a gastric bypass for severe malabsorption, may in fact result in weight gain and return of comorbidities.
When evaluating reoperations by types of index procedures, about 50 % of the reoperations were related to the adjustable gastric band that have been associated with low 30-day and 1-year morbidity and mortality rates. This suggests that both the index and the reoperation for an AGB are safe but could be due to the inclusion of relatively minor reoperations such as repositioning of a malpositioned access port, removing an infected port, or repairing a leak in the band tubing. In this series, reoperations related to AGB formed a large proportion of the total reoperations and may have skewed the total reoperation rate for all bariatric operations as well as contributed to the overall safety of reoperations. In addition, operations with a LOS ≤1 day accounted for 60 % of the corrective operations and 29 % of conversions, suggesting that a large number of reoperations were performed safely and were likely of lesser complexity. With a decline in the frequency with which AGB is being performed, it is possible that the overall rate of reoperations related to bariatric surgery may decline with time. However, as AGB operations are replaced by SG which is more effective but has a higher complication rate than AGB,20 the overall complication rate may increase. In our study, the morbidity and mortality of primary bariatric operations compared to reoperations were acceptable and not as high as previously reported.
The limitations of this study are that outcomes were reported in BOLD by individual practices and it is possible that complications were underreported. There were stringent audit practices at the time of center reaccreditation to ensure completeness of data entry. Although the registry collected information on reoperations and captured the common bariatric operations, the reasons for reoperations or the nomenclature for reoperations was not clearly defined. Therefore, an operation for bowel obstruction or bleeding would also be categorized as an “other” reoperation. This was a free text category and was impossible to extract in this very large database. Despite inclusion of all of these types of reoperations, it is gratifying to note that the reoperations were performed safely and had good resolution of comorbidity.
Conclusions
The rates and outcomes of patients undergoing reoperations were reported by the types of index operations and were compared to primary bariatric operations. The overall rates of reoperations were low, safe, and efficacious. These data should contribute to increasing knowledge regarding reoperations and reassure the medical and insurance communities that proceeding with reoperations not only rectifies complications but also justifies treatment for inadequate weight loss and resolution of comorbid conditions.
References
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA: the Journal of the American Medical Association. 2004 Oct 13;292(14):1724-37.
Prachand VN, Davee RT, Alverdy JC. Duodenal switch provides superior weight loss in the super-obese (BMI > or =50 kg/m2) compared with gastric bypass. Ann Surg. 2006 Oct;244(4):611-9.
Courcoulas AP, Christian NJ, Belle SH, Berk PD, Flum DR, Garcia L, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA: the journal of the American Medical Association. 2013 Dec 11;310(22):2416-25. PubMed PMID: 24189773.
Buchwald H, Estok R, Fahrbach K, Banel D, Sledge I. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery. 2007 Oct;142(4):621-32; discussion 32-5.
Himpens J, Coromina L, Verbrugghe A, Cadiere GB. Outcomes of revisional procedures for insufficient weight loss or weight regain after Roux-en-Y gastric bypass. Obesity surgery. 2012 Nov;22(11):1746-54.
Greenbaum DF, Wasser SH, Riley T, Juengert T, Hubler J, Angel K. Duodenal switch with omentopexy and feeding jejunostomy—a safe and effective revisional operation for failed previous weight loss surgery. Surgery for obesity and related diseases: official Journal of the American Society for Bariatric Surgery. 2011 Mar-Apr;7(2):213-8.
Brethauer SA, Kothari S, Sudan R, Williams B, English WJ, Brengman M, et al. Systematic review on reoperative bariatric surgery: American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg for Obes Relat Dis. 2014 Feb 22. doi: 10.1016/j.soard.2014.02.014.
DeMaria EJ, Pate V, Warthen M, Winegar DA. Baseline data from American Society for Metabolic and Bariatric Surgery-designated Bariatric Surgery Centers of Excellence using the Bariatric Outcomes Longitudinal Database. Surgery for obesity and related diseases: official Journal of the American Society for Bariatric Surgery. 2010 Jul-Aug;6(4):347-55.
Inabnet WB, 3rd, Belle SH, Bessler M, Courcoulas A, Dellinger P, Garcia L, et al. Comparison of 30-day outcomes after non-LapBand primary and revisional bariatric surgical procedures from the Longitudinal Assessment of Bariatric Surgery study. Surgery for obesity and related diseases: official Journal of the American Society for Bariatric Surgery. 2010 Jan-Feb;6(1):22-30.
Sudan R, Winegar D, Thomas S, Morton J. Influence of ethnicity on the efficacy and utilization of bariatric surgery in the USA. Journal of gastrointestinal surgery: official Journal of the Society for Surgery of the Alimentary Tract. 2014 Jan;18(1):130-6.
Mor A, Sharp L, Portenier D, Sudan R, Torquati A. Weight loss at first postoperative visit predicts long-term outcome of Roux-en-Y gastric bypass using Duke weight loss surgery chart. Surgery for obesity and related diseases: official Journal of the American Society for Bariatric Surgery. 2012 Sep-Oct;8(5):556-60.
Stroh C, Weiner R, Wolff S, Knoll C, Manger T, Obesity Surgery Working G, et al. Influences of Gender on Complication Rate and Outcome after Roux-en-Y Gastric Bypass: Data Analysis of More Than 10,000 Operations from the German Bariatric Surgery Registry. Obesity surgery. 2014 Apr 21.
Bekheit M, Katri K, Ashour MH, Sgromo B, Abou-Elnagah G, Abdel-Salam WN, et al. Gender influence on long-term weight loss after three bariatric procedures: gastric banding is less effective in males in a retrospective analysis. Surgical endoscopy. 2014 Mar 20.
Livingston EH, Huerta S, Arthur D, Lee S, De Shields S, Heber D. Male gender is a predictor of morbidity and age a predictor of mortality for patients undergoing gastric bypass surgery. Ann Surg. 2002 Nov;236(5):576-82.
Flum DR, Dellinger EP. Impact of gastric bypass operation on survival: a population-based analysis. Journal of the American College of Surgeons. 2004 Oct;199(4):543-51.
Schauer P, Ikramuddin S, Hamad G, Gourash W. The learning curve for laparoscopic Roux-en-Y gastric bypass is 100 cases. Surgical endoscopy. 2003 Feb;17(2):212-5.
Shikora SA, Kim JJ, Tarnoff ME, Raskin E, Shore R. Laparoscopic Roux-en-Y gastric bypass: results and learning curve of a high-volume academic program. Archives of surgery. 2005 Apr;140(4):362-7.
Sudan R, Bennett KM, Jacobs DO, Sudan DL. Multifactorial analysis of the learning curve for robot-assisted laparoscopic biliopancreatic diversion with duodenal switch. Ann Surg. 2012 May;255(5):940-5.
Ali MR, Tichansky DS, Kothari SN, McBride CL, Fernandez AZ, Jr., Sugerman HJ, et al. Validation that a 1-year fellowship in minimally invasive and bariatric surgery can eliminate the learning curve for laparoscopic gastric bypass. Surgical endoscopy. 2010 Jan;24(1):138-44.
Carlin AM, Zeni TM, English WJ, Hawasli AA, Genaw JA, Krause KR, et al. The comparative effectiveness of sleeve gastrectomy, gastric bypass, and adjustable gastric banding procedures for the treatment of morbid obesity. Ann Surg. 2013 May;257(5):791-7.
Acknowledgments
Funding was provided by an unrestricted grant to the American Society for Metabolic and Bariatric surgery. The funding agency had no input on data collection, analysis, results, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. Alfons Pomp (New York, NY):
I would like to thank the authors for the opportunity to discuss this interesting paper. This is another of an ever expanding group of papers presented at recent national meetings which have mined huge nonadministrative databases with multiple variables and tried to draw meaningful conclusions that are statistically valid. I, and others, remain somewhat dubious that most of these papers will actually allow us to make decisions of clinical significance.
The bariatric surgery databases of outcomes both from BOLD (and ACS) were historically established prior to the CMS decision to link accreditation with surgical outcome follow-up. This paper illustrates how it is actually possible for surgeons in multiple centers to enter data about their patients’ outcomes, use it in a comparative fashion, and then improve quality of care. Incidentally, it also shows just how safe and competent bariatric surgeons are as a group. We operate on these surgically difficult and seriously ill patients, mostly laparoscopically, with fairly amazing results.
My questions are as follows: (1) On what basis did you choose the serious adverse events from the 134 variables in the BOLD database? (2) Do you think the fact that 70 % of your revisions involved band to bypass or bypass to band skewed your results (showing relatively low rates of complications compared to other published series)? And finally (3) there were several statistical differences noted in the reoperation group, other than an increased length of stay (LOS), did you find anything clinically relevant?
Closing Discussant
Dr. Sudan:
Thank you for your comments and questions Dr. Pomp. I agree with you that establishing and participating in the data registry has been a big achievement for bariatric surgeons, and this clinically rich database provides very valuable information that has impacted quality of care. It is also true that bariatric surgeons have established that as a group we are able to perform complex primary bariatric operations very safely. However, the word that we can perform complex reoperative bariatric surgery still needs to get out. Each database has limitations, and therefore, investigators need to be knowledgeable about its nuances and conduct a responsible and careful analysis and we have attempted to do so. In response to your first question, BOLD collected information on 134 adverse events. To define severe adverse events, two experts in bariatric surgery reviewed this list and identified 33 acute adverse events that were potentially life-threatening such as bleeding requiring transfusion, leaks, deep venous thrombosis, sepsis, etc. We hoped that such severe events would be captured more completely in BOLD and, thus, yield valid results. This decision was based on judgment, and it is important to note that this list does not represent the full spectrum of complications that these patients may have suffered. In response to your second question, the vast majority of reoperations were related to an adjustable gastric band, and this may have driven the overall reoperation rate higher but kept the severity of complications low. We did not investigate procedure-specific severe adverse event rates but plan to do so in the future. Finally, when working with large databases, even small differences are statistically significant. Therefore, the results should be placed in a clinical context. In this study, even though length of stay, morbidity, and mortality were statistically higher, but from a clinical perspective, conversions had a length of stay of 3 days. At 1 year, mortality was around 0.3 % and severe adverse events were around 3.5 %. Comorbidities were also resolved. Therefore, the clinicians and patients have to decide if these risks are worth taking not withstanding statistical significance. We certainly believe so and hope that these results will encourage payors, health-care providers, and patients so that more people may benefit from bariatric reoperations.
Rights and permissions
About this article
Cite this article
Sudan, R., Nguyen, N.T., Hutter, M.M. et al. Morbidity, Mortality, and Weight Loss Outcomes After Reoperative Bariatric Surgery in the USA. J Gastrointest Surg 19, 171–179 (2015). https://doi.org/10.1007/s11605-014-2639-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2639-5