Abstract
Purpose
The over-the-scope clip (OTSC) enables non-surgical management of gastrointestinal defects. The aim of this study was to report our experience with OTSC for patients with staple line leaks following laparoscopic sleeve gastrectomy (LSG).
Materials and Methods
A prospectively maintained IRB-approved institutional database was queried for all patients treated with OTSC for staple line leaks following LSG from 2010 to 2018. Primary outcome was complete resolution of leak following OTSC. Secondary outcome was the number of additional procedures needed following OTSC.
Results
Twenty-six patients (13 males, 13 females) were treated with OTSC for staple line leaks following LSG. The median age was 35 years (range 18–62), and mean body mass index was 44 kg/m2. The median time from index operation to leak diagnosis and from leak diagnosis to OTSC was 18 days (range 2–118), and 6 days (range 1–120), respectively. The initial endoscopic treatment was OTSC (n = 19), stent (n = 5), clip (n = 1), and clip and biologic glue (n = 1). OTSC alone led to final resolution of leak in 8 patients (31%) within 43 days of clip deployment (range 5–87). Five leaks resolved after a combination of OTSC and stent (19%) and one leak (4%) resolved after endoscopic suturing following a failed OTSC. Eleven patients (42%) failed endoscopic management and underwent total gastrectomy and esophagojejunostomy. One mortality (4%) was noted. The number of additional endoscopic sessions ranged from 1 to 10 (median 2).
Conclusions
OTSC carries a low success rate for controlling staple line leaks following LSG.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
According to the most recent publication by the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO), laparoscopic sleeve gastrectomy (LSG) is the most commonly performed bariatric operation worldwide [1]. The primary major complication reported after LSG is leak, occurring in 0.5–2% of patients, and its management requires a complex, multidisciplinary approach [2]. It is commonly mentioned that leaks following LSG are more difficult to treat than those following other bariatric procedures such as laparoscopic Roux-en-Y gastric bypass (LRYGB). This difficulty has been proposed to be due to the long staple line and the elevated post-operative intraluminal pressure in the sleeve, which are not present in the gastric pouch following LRYGB [3, 4]. Treatment modalities include various combinations of conservative management, antibiotics, parenteral nutrition, percutaneous or operative drainage, and endoscopic interventions. Endoscopic management of leaks following LSG is being utilized more often [5]. Endoscopic interventions might include fibrin glue, covered stents, plugs, internal drainage septotomy, or clips for full-thickness GI wall closure [6,7,8]. If conservative measures fail to resolve the leak, patients might need operative solutions [2, 3, 9, 10].
The over-the-scope clip (OTSC®, Ovesco Endoscopy AG, Tubingen, Germany) is a novel endoscopic tool that enables the non-surgical management of patients with GI defects. It consists of a Nitinol clip shaped similar to a bear trap, with a wider mouth enabling to grasp a larger amount of tissue with a greater compressive force than the standard clip [11]. Recently published review papers on the clinical utility of the OTSC indicate that since its initial report approximately a decade ago, there have been increasing indications for its use, such as bleeding, perforation, leak, fistula, and closure of gastrostomies and natural orifice transluminal endoscopic surgery (NOTES) access points [12, 13].
Limited data have been published regarding the clinical outcome of the OTSC system for leaks following LSG. A recent review showed an 86.3% (63/73) overall success rate of the OTSC in closing post-LSG leaks. However, the review included 10 studies with a small sample size (the largest study included 26 patients), short-term follow-up, and mixed data of concomitant procedures with OTSC [5].
The aim of this single institute study was to report our experience with OTSC for patients with staple line leaks following laparoscopic sleeve gastrectomy (LSG).
Methods
A prospectively maintained IRB-approved institutional database was queried for all patients treated with OTSC for staple line leaks following LSG from 2010 to 2018. Staple line leak was defined as a defect at the staple line leading to a communication between the intra- and extra-luminal compartments as proven by imaging or endoscopy.
Data collection was separated into 3 categories: pre-procedural, procedural, and post-procedural data. Pre-procedural data included patient demographics, anatomic site of the staple line leak, time from LSG to diagnosis of leak, and time to OTSC deployment. Additional pre-procedural data were prior endoscopic or surgical attempts to manage the defect. Procedural data included the initial endoscopic modality utilized to resolve the leak, as well as technical success, size, location and appearance of the staple line defect, type of OTSC, and procedure-related complications. Post-procedural data included the need for additional interventions, length of follow-up, and status of defect at last follow-up.
Primary outcome was complete resolution of leak following OTSC as a single modality. Leak resolution was defined by return to complete oral nutrition and no evidence of leak on imaging. Secondary outcome was the number of additional endoscopic or surgical procedures needed following OTSC.
Data are presented as the mean ± standard deviation or the median with ranges, as appropriate. Statistical calculations were completed using the statistical software SPSS version 20.0 (IBM, Armonk, NY).
Results
Twenty-six patients (13 males, 13 females) were treated with OTSC for staple line leaks following LSG. The median age was 35 years (range 18–62), and mean body mass index was 44 kg/m2. Nine patients (35%) were referred from an outside hospital. One patient had LSG as revisional surgery after a failed gastric band. Four patients suffered post-operative bleeding after their index LSG, one of whom required diagnostic laparoscopy and the other 3 patients were treated conservatively with blood transfusions. Computed tomography was the imaging modality of choice revealing the staple line leak in all 26 patients. The median time from index operation to leak diagnosis was 18 days (range 2–118) and from leak diagnosis to OTSC, 6 days (range 1–120). All patients had upper staple line leaks near the gastroesophageal junction.
Initial treatment included antibiotics alone (n = 6), computed tomography guided drainage and antibiotics (n = 7), laparoscopic drainage (n = 7), and laparoscopic drainage with suturing of leak site (n = 6). After ensuring adequate drainage, all patients were treated with total parenteral nutrition. Upper endoscopy was performed in all patients revealing an average defect size of 0.9 cm. All the endoscopic procedures were performed by one of two well-experienced interventional endoscopists.
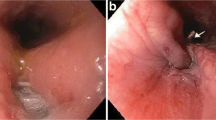
OTSC as a single modality led to final resolution of leak in 8 patients (31%) within 43 days of clip deployment (range 5–87 days). Figure 1 presents a case presentation of a patient treated successfully with OTSC for a staple line leak following LSG. Three leaks (11%) persisted after initial therapy with OTSC and resolved after stent insertion, and two leaks (8%) persisted after initial treatment with a stent and resolved after OTSC deployment, resulting in a total of five leaks (19%) resolved after a combination of OTSC and stent. One leak (4%) resolved after endoscopic suturing following a failed OTSC. Overall combined endoscopic therapy led to resolution of leak in 14 patients (54%) within 42 days of initial endoscopic intervention (range 5–105 days).
A case presentation of a 61-year-old female. Presented with fever and chills on POD#20 after LSG. Her CT showed an abscess near the gastric sleeve (a) and she underwent immediate drainage under CT guidance. Her upper GI endoscopy on POD#21 showed a fistula opening near the GE junction (b). A 12-mm OTSC was placed closing the fistula opening (c and d). Notice the “bear claw” appearance of the OTSC (c). The patient was kept NPO and was treated with IV antibiotics and total parenteral nutrition. Her upper GI swallow study on POD #31 showed normal passage of contrast with no evidence of leak (e). A CT on POD#45 due to abdominal pain showed complete resolution of the abscess and leak (f)
Eleven patients (42%) failed endoscopic management and underwent total gastrectomy and esophagojejunostomy. In these 11 eleven patients, the endoscopic treatment which failed was a combination of both OTSC and stent (n = 4), OTSC alone (n = 4), OTSC and biologic glue (n = 2), and a combination of clip and OTSC (n = 1). One mortality (4%) was noted in a patient who suffered multi-organ failure due to his leak which persisted after OTSC trial. Patient demographics and procedural data are brought in Table 1.
In order to identify factors that might have contributed to endoscopic failure, we compared patients who have had successful endoscopic treatment (n = 14) to those who failed and required surgery (n = 11). Groups were similar for age, gender, BMI, time from LSG to leak, time from leak to OTSC, and defect size (Table 2). Hence, no variable leading to OTSC failure could be identified.
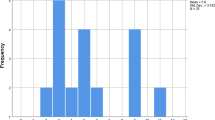
The median number of additional endoscopic sessions was 2 (range, 1–10) and the median number of CT scans performed was 7 (range, 4–14). No procedure-related complications were noted. The average total length of stay was 49 days (range 13–127). Figure 2 illustrates the definitive treatment flow chart.
Discussion
The results of our study show that OTSC as a single endoscopic modality has a 31% (8/26) success rate for resolving a staple line leak after LSG. This low success rate increases to 54% (14/26) when adding patients who were treated with a combination of OTSC and another endoscopic modality such as stent or endoscopic suturing. A recent systematic review by Shoar et al. reported on the efficacy and safety of the OTSC in the management of leak after LSG [5]. The review included 10 retrospective small sample studies and reported that OTSC as a solo procedure was successful in closing the staple line defect in 40% of patients (29/73), while an additional 46% of patients (34/73) required another endoscopic procedure to reach resolution of leak. This resulted in a total of 86% (63/73) success rate for OTSC as a single or combined endoscopic therapy. Similarly, Keren et al. showed that the OTSC as a single modality had a 50% success rate (13/26) for treating staple line leaks after LSG, while an additional 30% of patients (8/26) were treated with at least one other endoscopic modality, resulting in an overall success rate of 80% for OTSC as a single or combined endoscopic therapy [14].
Our success rates for OTSC as a single or combined therapy are lower than the abovementioned reports. Several factors have been attributed to OTSC failure at treating staple line leaks after LSG. Amongst these factors are previous gastric banding, defect size, location of the staple line defect, co-morbidities, and age. Furthermore, time from LSG to leak diagnosis and time from leak diagnosis to OTSC have also been attributed to OTSC failure, due to increased fibrosis with longer time intervals. Unfortunately, previous reports failed to show significant correlation of any of these factors to OTSC failure. Furthermore, these studies reported inconsistently their success rates for single versus combined therapy, time to leak diagnosis and OTSC therapy, defect size, and patient co-morbidities. In our cohort, when comparing patients who have had successful endoscopic treatment (n = 14) to those who failed and required surgery (n = 11), there were no differences in terms of age, gender, BMI, time from LSG to leak, time from leak to OTSC, and defect size (Table 2). Regarding location of the staple line defect, all the patients in our cohort had leaks located at the gastroesophageal junction. In the study by Keren et al., two of the five patients who had failed OTSC had antral leaks believed to be more resistant to endoscopic treatment [14]. One patient in our study had previous gastric banding. This patient underwent stent insertion followed by two OTSC deployments resulting in complete resolution of his staple line leak. Ten out of the 26 patients in the study by Keren et al. had previous bariatric surgery (silastic ring vertical gastroplasty or laparoscopic adjustable gastric banding), but only one patient failed OTSC [14]. Hence, in our opinion, there is no proof that success rates for closing a staple line leak with OTSC are lower if LSG was performed as a revisional procedure.
The success rate of other endoscopic procedures in treating staple line leaks following LSG has been previously published by others. Leeds and Burdick studied the efficacy of the Endo-SPONGE® (E-vac) and showed that all 9 patients in their study had resolution of leaks confirmed by upper gastrointestinal series, after undergoing endo-sponge therapy for an average of 50 days. During treatment, an average of 10.3 procedures per patient was done to place and exchange the Endo-SPONGE® [15]. Guiliani et al. conducted a systematic review on the efficacy of the double pigtail drainage system endoscopically positioned to treat leaks post-sleeve gastrectomy. The review included 385 patients and showed that the pooled proportion of successful leak closures by using double pigtail drainage was 83.41% [16]. Okazaki et al. published a systematic review and meta-analysis on the efficacy and safety of stents in the treatment of fistula after sleeve gastrectomy and gastric bypass. In the sleeve gastrectomy group, 187 patients were included in 24 studies. The overall success rate was 72.8%, mean number of stents per patient was 1.4 ± 0.03, and mean stent dwelling time was 48.77 ± 0.58 days. The stent migration rate was 28.2% considering all studies [17].
Advanced endoscopic interventions, such as stent insertion, OTSC, and endoscopic suturing, require a skilled and experienced endoscopist. Moreover, to maximize success rates of such complex procedures, it is crucial to have a multidisciplinary team comprised of a high-volume bariatric surgeon, a competent interventional radiologist, and a skillful endoscopist. Fortunately, our team consists of the mentioned above and is therefore considered a national referral center. We insist on having the bariatric surgeon present at the endoscopy suite during the procedure in order to reach a joint and suitable decision in a case by case approach. The experienced surgeon should be aware of endoscopic findings such as fibrosis, location, and size of defect in order to acknowledge when it is time for surgery. Perhaps, underestimation of the technical difficulty to fix the device due to the lateral position of the orifice and the inflammation of the tissues have contributed to our high failure rate.
Bariatric surgeons worldwide should be aware of the potential morbidity accompanied with LSG complications, specifically staple line leak. Patients should be educated that even if the endoscopic interventions resolve the leak, they are expected a prolonged length of stay, potential TPN-associated complications, multiple CT scans, and endoscopies. Surgeons should be alerted that if best endoscopic therapy was to fail, they will need to perform complex major abdominal surgery with total gastrectomy and esophagojejunostomy, which has its own inherent complication rate. Therefore, in our opinion, such challenging procedures should be performed by high-volume bariatric surgeons at referral centers.
Obviously, treating a patient with a staple line leak carries a high economic cost influenced by prolonged hospital admissions, intensive care unit stay, total parenteral nutrition feeding, numerous imaging studies, and multiple endoscopic interventions. The cost of the OTSC in out hospital reaches 1000 euros. Clearly, with the low success rate we experienced, we now reconsider more selectively the cases we think may benefit from this approach. Surgeons and health care policy makers should try to calculate a cost-benefit ration when treating a patient with a leak following LSG based both on clinical studies and on their own clinical experience.
This study has several limitations. The retrospective nature of the study has its obvious limitations regarding selection bias. The small sample size limits our ability to draw more definitive conclusions. Finally, OTSC was performed by two different interventional endoscopists with the obvious variability in technical abilities. Despite its limitations, our study supplies valuable clinical data regarding the clinical success rate of OTSC for closing a staple line defect after LSG. Our cohort includes a relatively large number of patients, with only one previous study reporting on the same number of patients.
Our experience shows that OTSC, as either a single or combined endoscopic therapy, carries a low success rate for controlling staple line leaks following LSG. Hence, the OTSC should be kept as an option for patients who failed or could not tolerate other more successful endoscopic therapies such as the double pigtail drainage system, stents, and Endo-SPONGE®. Prospective large cohort studies are needed to further validate this endoscopic tool.
Change history
31 August 2023
A Correction to this paper has been published: https://doi.org/10.1007/s11695-023-06808-8
References
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one year outcomes from the fourth IFSO global registry report 2018. Obes Surg. 2019;29:782–95.
Kim J, Azagury D, Eisenberg D, et al. ASMBS position statement on prevention, detection, and treatment of gastrointestinal leak after gastric bypass and sleeve gastrectomy, including the roles of imaging, surgical exploration, and nonoperative management. Surg Obes Relat Dis. 2015;11(4):739–48.
Nimeri A, Ibrahim M, Maasher A, et al. Management algorithm for leaks following laparoscopic sleeve gastrectomy. Obes Surg. 2016;26(1):21–5.
Yehoshua RT, Eidelman LA, Stein M, et al. Laparoscopic sleeve gastrectomy–volume and pressure assessment. Obes Surg. 2008;18(9):1083–8.
Shoar S, Poliakin L, Khorgami Z, et al. Efficacy and safety of the over-the-scope clip (OTSC) system in the management of leak and fistula after laparoscopic sleeve gastrectomy: a systematic review. Obes Surg. 2017;27(9):2410–8.
Casella G, Soricelli E, Rizzello M, et al. Nonsurgical treatment of staple line leaks after laparoscopic sleeve gastrectomy. Obes Surg. 2009;19(7):821–6.
Moon RC, Shah N, Teixeira AF, et al. Management of staple line leaks following sleeve gastrectomy. Surg Obes Relat Dis. 2015;11(1):54–9.
Sakran N, Goitein D, Raziel A, et al. Gastric leaks after sleeve gastrectomy: a multicenter experience with 2,834 patients. Surg Endosc. 2013;27(1):240–5.
Jacobsen HJ, Nergard BJ, Leifsson BG, et al. Management of suspected anastomotic leak after bariatric laparoscopic Roux-en-Y gastric bypass. Br J Surg. 2014;101(4):417–23.
Abou Rached A, Basile M, El Masri H. Gastric leaks post sleeve gastrectomy: review of its prevention and management. World J Gastroenterol. 2014;20(38):13904–10.
von Renteln D, Vassiliou MC, Rothstein RI. Randomized controlled trial comparing endoscopic clips and over-the-scope clips for closure of natural orifice transluminal endoscopic surgery gastrotomies. Endoscopy. 2009;41(12):1056–61.
Weiland T, Fehlker M, Gottwald T, et al. Performance of the OTSC system in the endoscopic closure of iatrogenic gastrointestinal perforations: a systematic review. Surg Endosc. 2013;27(7):2258–74.
Baron TH, Song LMWK, Ross A, et al. Use of an over-the-scope clipping device: multicenter retrospective results of the first U.S. experience (with videos). Gastrointest Endosc. 2012;76(1):202–8.
Keren D, Eyal O, Sroka G, et al. Over-the-scope clip (OTSC) system for sleeve gastrectomy leaks. Obes Surg. 2015;25(8):1358–63.
Leeds S, Burdick J. Management of gastric leaks after sleeve gastrectomy with endoluminal vacuum (E-Vac) therapy. Surg Obes Relat Dis. 2016 Aug;12(7):1278–85.
Giuliani A, Romano L, Marchese M, et al. Gastric leak after laparoscopic sleeve gastrectomy: management with endoscopic double pigtail drainage. A systematic review. Surg Obes Relat Dis. 2019;15(8):1414–9.
Okazaki O, Bernardo WM, Brunaldi VO, et al. Efficacy and safety of stents in the treatment of fistula after bariatric surgery: a systematic review and meta-analysis. Obes Surg. 2018 Jun;28(6):1788–96.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed Consent does not apply to our study as determined by our institutional review board.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mizrahi, I., Grinbaum, R., Elazary, R. et al. Staple Line Leaks Following Laparoscopic Sleeve Gastrectomy: Low Efficacy of the Over-the-Scope Clip. OBES SURG 31, 813–819 (2021). https://doi.org/10.1007/s11695-020-05036-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-05036-8