Abstract
Background
This prospective study applied magnetic resonance imaging (MRI) to assess the effect of laparoscopic sleeve gastrectomy (LSG) on gastric structure and function. The impact of these changes on patient outcomes was analyzed.
Method
Obese patients without gastrointestinal symptoms referred for bariatric surgery were recruited prospectively. Pre-operative assessment included (i) high-resolution manometry and pH-impedance monitoring and (ii) magnetic resonance imaging (MRI) measurement of gastric capacity, accommodation, and emptying with the 400 ml liquid Nottingham test meal (NTM). Studies were repeated 6–7 months after LSG. Weight loss and changes in the Gastrointestinal Quality of Life Index (GIQLI) assessed patient outcomes.
Results
From 35 patients screened, 23 (66%) completed the study (17 females, age 36 ± 10 years, BMI 42 ± 5 kg/m2). Mean excess weight loss was 59 ± 18% at follow-up. Total gastric volume (capacity) after the meal was 467 mL (455–585 ml) before and 139 mL (121–185 ml) after LSG (normal reference 534 (419–675) mL), representing a mean 70% reduction (p < 0.0001). Similar findings were present for gastric content volume indicating rapid early-phase gastric emptying (GE) post-LSG. Conversely, late-phase GE was slower post-LSG (2.5 ± 1.0 vs. 1.4 ± 0.6 mL/min; p < 0.0001; (reference 1.5(1.4–4.9) mL/min)). Patients with ≥ 80% reduction in gastric capacity had greater weight loss (p = 0.008), but worse gastrointestinal outcomes (p = 0.023).
Conclusions
MRI studies quantified the marked reduction in gastric capacity after LSG. The reduction in capacity was associated with rapid early- but slow late-phase GE after surgery. These changes were associated with weight loss; however, reductions in gastric capacity ≥ 80% were linked to increased acid reflux and impacted on gastrointestinal quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic sleeve gastrectomy (LSG) is the most commonly performed surgical treatment for morbid obesity [1, 2]. Prospective randomized studies show similar outcomes in terms of weight loss after 5 years compared with laparoscopic Roux-en-Y gastric bypass (RYGB), although patients complained of reflux and dyspeptic symptoms more often after LSG than RYGB [3].
The impact of LSG on gastric structure and function and how this relates to food intake, weight loss, and other post-operative outcomes is a subject of debate. The stapling and resection of the gastric body and fundus greatly reduces gastric capacity and limits active relaxation and filling (accommodation) during meal ingestion [4]. This reduction in gastric capacitance leads to high intra-luminal pressures and wall tension in the stomach wall during gastric filling [4]. Changes in gastric structure and function after LSG may also impact on gastric emptying (GE); however, no consistent pattern is reported in the literature. Some studies report increased emptying rate, others no change or delayed emptying [5,6,7,8,9,10]. These effects are clinically relevant because interventions that alter gastric function modulate satiation and satiety. Additionally, impaired gastric accommodation and emptying are important causes of symptoms in patients with functional dyspepsia and gastroparesis [11, 12]. The lack of consensus regarding the effects of bariatric surgery on gastrointestinal physiology and how this relates to patient outcomes is likely related to the lack of standardized surgical technique and also the application of different, and sometimes sub-optimal, investigative methods.
This prospective study acquired comprehensive physiological data before and after surgery to test the hypothesis that changes to gastric structure and function caused by LSG have important effects on weight loss, gastrointestinal symptoms, and quality of life. Validated MRI measurements of gastric capacity, accommodation, and emptying after ingestion of a liquid nutrient test meal. These results were compared with clinical endpoints to better understand the (patho-)physiological mechanisms that determine patient outcome after this form of bariatric surgery.
Materials and Methods
Study Population
This prospective, single-center study was conducted between December 2013 and November 2015 at the Digestive Surgery Department of the Nouvel Hôpital Civil (NHC) in Strasbourg, with the support of the Image-Guided Surgery Institute (Institut de Chirurgie Guidée par l’Image (IHU)). The study was approved by the National Ethics Committee and registered (NCT01980420) and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent to undergo study procedures, including LSG and physiological measurements, was obtained from all patients.
Morbidly obese patients selected to undergo LSG according to international guidelines were recruited [13]. Candidates for a bariatric procedure that did not have reflux symptoms or require acid suppressant medications were eligible for inclusion. Patients with a contraindication for MRI, pregnant or breastfeeding patients, or patients unable to give informed consent were excluded from the study.
Study Design
All patients underwent clinical examination and BMI calculation. Standard pre-operative assessment before LSG in our hospital includes high-resolution esophageal manometry (HRM) and impedance-pH reflux monitoring, an upper gastrointestinal series (UGI), and quality of life (QoL) assessment with the Gastrointestinal Quality of Life Index (GIQLI) and GERD Symptom Assessment Scale (GSAS). Additional measurements included anatomic MRI of the upper gastrointestinal tract before and after ingestion of the 400 ml nutrient liquid Nottingham test meal.
Intra-operative and postoperative complications were recorded, and the patients were followed with regular outpatient visits at 8 days, 1, and 3 months. The final evaluation was scheduled when the patient reached a minimum of 40% reduction in excess weight. At this point, the same anatomical and functional evaluation was repeated. A schematic overview of the study design is available as Supplementary Material.
All operations were performed by one of three senior bariatric surgeons, respecting the same surgical sequences and steps as previously reported [14, 15].
Evaluation of EGJ Structure and Function
All imaging and physiological measurements were performed according to published standards [16,17,18].
High-Resolution Manometry
HRM studies were performed using a solid-state ManoScan™ 360 catheter (Medtronic, Duluth, USA) with 30-s baseline recording and 10 5 mL water swallows in the supine position after an overnight fast. Esophageal motility and EGJ barrier function were evaluated using the ManoView™ ESO analysis program version 3.0 and classified according to Chicago Classification v3.0 [17].
24-h pH-Impedance Measurements
Ambulatory reflux monitoring was performed using a ZepHr@impedence/pH reflux monitoring system (Diversatek Healthcare, Milwaukee, USA) with PPI medication stopped at least 5 days prior to measurement. Patients followed usual activities and diets and recorded timing of meals, symptoms, and position. Data were analyzed by using BioVIEW® analysis software with calculation of total percent of time with pH < 4.0, and/or the total number of reflux episodes (pathological if ≥4% or ≥ 80, respectively) as outlined by the Lyon Classification for GERD diagnosis [19].
Magnetic Resonance Imaging
MRI measurements of gastric morphology were acquired on a MAGNETOM Aera 1.5 T- scanner (Siemens, Münich, Germany) using validated techniques described by Curcic and colleagues [20]. Operating procedures for measurements of GE were based on a protocol for non-invasive assessment of gastric motor and sensory function published by Parker and colleagues (reference intervals in healthy subjects presented in the same publication) [21, 22]. Specifically, after baseline measurements of gastric volume, 400 mL of liquid vanilla nutrition drink (0.75 kcal/mL; Fortimel®, Nutricia) was ingested over 10 min (40 ml cup/min) or until maximum satiation. Image acquisition was performed immediately after ingestion, and subsequently every 10 min for the first 40 min, and at 55, 70, and 90 min after ingestion, for a total of eight acquisitions. If required, image acquisition continued until GE was complete. To acquire volume measurements, a semi-automatic method was used to outline the contents and air on each image slice. This required an intensity-based method to define both high signal intensity gastric content volume (GCV) and low signal intensity air volumes using a custom-written software (IDL version 6.4; Research Systems Inc., Boulder, CO). The total gastric volume (TGV) was calculated from the sum of the air and content regions. The segmented area on each slice was multiplied by the slice thickness and summed over all contoured slices to measure the different stomach volumes (i.e., GCV, TGV) (Fig. 1).
Representative images illustrating change of total gastric volume (TGV) and gastric content volume (GCV) during meal ingestion in a healthy volunteer. The intra-gastric air and liquid contents are colored violet and orange respectively (courtesy of Dr. S. Banerjee, Indian Institute of Technology). Vin, volume of the test meal ingested
TGV0 immediately after meal ingestion (i.e., at time = 0) represents gastric capacitance (a combination of capacity and accommodation). The reduction in TGV after the meal indicates tonic contraction. The change in Gastric Content Volume (GCV) reflects change of meal (including secretion) volume over time. The difference between meal volume and GCV0 provides an assessment of “Early-Phase GE” that commences even before the meal is completed and is determined by physical factors such as gastric capacitance and the volume of the meal [23]. Subsequent “late-phase GE” is determined also by the calorie content and other properties of the meal that regulate GE rate by neurohormonal feedback [23].
Statistical Analysis
The primary outcome measure was GE after ingestion of a 400 ml liquid nutrient Nottingham test meal (NTM). Based on surgical experience we expected at least 50% reduction in total gastric volume (TGV) after LSG. Physical principles dictate that this would also reduce gastric content volume (GCV). Calculations based on published literature indicate that 10 patients would have a > 90% study power to demonstrate a 50% change in TGV0 and GCV0 at a standard level of significance (p > 0.05). We completed measurements in 23 patients undergoing bariatric surgery to ensure that statistical power was adequate not only to demonstrate the effect of surgery on primary outcome measures but to ensure a large enough population was recruited to analyze the association between key measurements and patient outcomes.
Continuous variables were reported as mean ± standard deviation (SD) and categorical variables as numbers and percentages unless otherwise specified. Ordinal qualitative variables and quantitative variables were compared with Wilcoxon rank sum test. Paired comparison of qualitative variables was performed with Fisher’s exact test or chi-square tests. Correlations between MR measurements of gastric physiology and other physiological variables were performed using Pearson correlation coefficient (Pearson’s rho) or Spearman’s correlation coefficient. In case of Pearson’s correlation coefficient < 0.2, a linear regression analysis was performed. The impact of these factors on weight change, patient symptoms, and QoL of patients was also assessed. Results from pre- and post-operative measurements were also compared with reference intervals in age and sex matched healthy subjects on file [21]. All reported p values are two-tailed, and a p value < 0.05 was required to conclude statistical significance. The SPSS software, version 20.0 (IBM-SPSS, Chicago IL), was used for the analysis.
Results
During the study period, a total of 487 patients underwent bariatric surgical procedures, including 406 (83.4%) gastric bypasses and 81(16.6%) LSGs. According to the prospectively defined inclusion criteria, thirty-five patients were enrolled in the study. After the screening visit, 7 patients refused surgery and 5 patients did not undergo the post-operative evaluation. Thus, 23 (66%) of eligible patients completed the study. Patients’ characteristics and clinical evaluation at inclusion visit, admission, and last follow-up are reported in (Table 1).
Patients’ characteristics are reported in Table 1. There was a significant decrease in BMI from the inclusion visit to the follow-up evaluation (p < 0.0001), with a mean excess weight loss of 58.6 ± 17.8% after a mean of 7.09 (±1.7) months.
High-Resolution Manometry and pH-Impedance Monitoring
No patient had a motility disorder, reflux oesophagitis, or hiatal hernia on pre-operative assessment. Esophageal motility was not altered by surgery; however, EGJ intra-abdominal length and pressure were reduced (both p < 0.001). These changes were accompanied by an increase in esophageal acid exposure time and the number and the duration of reflux events (Table 2). Based on Lyon Consensus criteria [18], 8 patients had GERD based on pH-impedance monitoring after LSG (p = 0.001).
MRI Assessment of Gastric Capacity and Emptying
During the pre-operative assessment, all patients ingested the complete 400 mL Nottingham test meal (NTM) without dyspeptic symptoms. After LSG, all patients reported the rapid onset of gastric filling sensations/early satiation and the maximum tolerated volume was a median 200 ml (mean 188 ± 54 ml).
Total gastric volume immediately after ingestion of the test meal (TGV0; an assessment of gastric capacity) was 467 mL (ref 455–585 ml) before and 139 mL (121–185 ml) after LSG (p < 0.0001). Pre-operative values were within the reference range determined in age and sex stratified healthy volunteers (524 mL (415–696) [21]), whereas the post-operative findings were greatly reduced from this level (p < 0.0001). In relative terms, TGV0 was reduced by mean 69% ± 12% of the preoperative value (range 43–93%) with similar findings documented for gastric content volume (GCV), as shown in (Fig. 2).
Even taking into account the reduced volume of the NTM ingested after LSG, compared with baseline measurements, there was a dramatic reduction in GCV0 after surgery indicating very rapid early-phase GE (1.9 vs. 2.69 mL/min; p < 0.0001). Conversely, late-phase GE was significantly slower post-LSG (2.5 vs. 1.4 mL/min; p < 0.0001). There was a highly significant negative correlation between early- and late-phase GE (Pearson r2 = − 0.39; p < 0.001) such that high rates of early GE were associated with slow rates of late gastric emptying. A strong negative correlation was present also between the percentage reduction in the gastric capacity (TGV0) and late-phase GE rate (Pearson: r2 = − 0.52; p < 0.001) (Fig. 3). Expressed in terms of relative TGV reduction, patients with the greatest reduction in gastric capacity (> 80% reduction) had the most rapid early-phase and the slowest late-phase GE rates.
Significant inverse correlation between the reduction in Gastric Capacity (TGV0) and subsequent late-phase gastric emptying rate. Reduction in gastric capacity is directly linked to very rapid early-phase gastric emptying; however, this is followed by relatively slow late-phase gastric emptying likely due to negative neurohormonal feedback
Correlation Between Physiologic Measurement and Patient Outcome
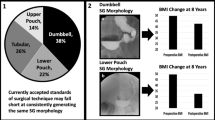
Patients were divided into three groups according to the post-operative reduction in gastric capacity (TGV0): patients with < 60% reduction (n = 6), reduction between 60 and 80% (n = 10), and patients with a > 80% reduction (n = 7).
A correlation was present between the percentage reduction in gastric volume and mean weight loss (Pearson 0.458; p = 0.058). Patients with the largest reduction in gastric capacity had greater weight loss at 6–7 months follow-up after LSG as compared with the other two groups (32.3 ± 3.8 kg vs. 22.3 ± 6.6 kg vs. 21.9 ± 4.5 kg respectively; p = 0.008) (Fig. 4). Similarly, rapid early-phase GE was correlated with higher post-operative weight loss (Spearman 0.458; p = 0.028). No correlation was found between the slow late GE and post-operative weight loss results (Spearman − 0.291; p = 0.201). In a multiple linear regression analysis both reduction in residual TGV0 (β 0.54; I.C. 8.1–1.9; p 0.003) and the rate of early-phase GE (β 0.48; I.C. 0.49–2.6; p 0.007) had statistically significant effects on patient weight loss.
Interaction between reduction in gastric capacity after LSG and clinical outcome after LSG. Quality of life of all subjects improved with weight loss after bariatric surgery. Patients with a large reduction in GVR (> 80%) had greater weight loss; however, 6/7 of this group reported more gastrointestinal symptoms after surgery. The difference between groups evaluated by GIQLI and GIQLI GI domain was not significant
No correlation was observed between esophageal motility and changes in gastric capacity or emptying rate (data not shown); however, as published in a separate report [15], the presence of impaired EGJ function was related to increased risk of gastro-esophageal reflux disease (p = 0.01, Pearson = − 0.54). Additionally, patients with the largest reduction in gastric capacity had more severe reflux in terms of esophageal acid exposure as compared with the other two groups (9.3% ± 7.6 vs. 3.9% ± 3.4 vs. 1.5% ± 1.2; p = 0.002).
Quality of Life
A significant increase in the GIQLI score was documented after LSG compared with baseline representing improved quality of life after surgery (114 ± 10.1 vs. 103 ± 14.5, p = 0.004). Despite the increase in overall score, a worsening in the gastrointestinal subdomain was identified (65.9 ± 6.6 vs. 58.5 ± 5.9, p = 0.001). Overall, 20/23 (87%) patients reported more gastrointestinal symptoms after surgery. In particular, a higher incidence of nausea (p = 0.002) abdominal rumbling (p = 0.01) and constipation (p = 0.002) were present postoperatively. No significant change was noted in the GSAS score documenting reflux symptoms (0.49 ± 0.3 vs. 0.54 ± 0.23), although it was noted that 6 of 7 patients with > 80% of gastric volume reduction after LSG had both increased GSAS and reduced GIQLI.
Discussion
Magnetic resonance (MR) imaging of the stomach provides safe, non-invasive, and quantitative measurements of gastric structure and function before and after LSG [24]. Analysis of the images and comparison with the results of other physiological investigations demonstrates how the important reduction in gastric capacity impacts on food intake and gastric function. The clinical relevance of these results was demonstrated by the association of these findings with patient outcomes including weight loss and gastrointestinal symptoms.
Effects of LSG on Gastric Capacity/Residual Gastric Volume
The change in gastric capacity after LSG was estimated from MR measurements of total gastric volume (TGV) after ingestion of a validated test meal [21, 22]. Subjects ingested a liquid nutrient at 40 ml/min over 10 min until a total of 400 ml had been ingested or until maximum satiation had been reached. Prior to surgery, similar to healthy volunteers, all of the obese patients completed the 400 ml test meal without difficulty and repeated imaging documented that TGV increased by a mean 353 ml. These results were similar to those obtained from healthy controls [21]. By contrast, after LSG, approximately 200 ml was ingested before maximum satiation was reported and TGV increased by only a mean 124 ml (Table 3).Footnote 1
This finding indicates that, not only gastric capacity but also gastric accommodation (i.e., volume increase for a given volume load) is reduced after LSG because the increase in TGV relative to the size of the meal was greater at pre-operative screening than after surgery (353/400 (88%) vs. 124/200 (62%)). Based on absolute measurements of TGV0 immediately after the meal, the average reduction of gastric capacitance (combination of capacity and accommodation) after LSG was 70% (43%–93%). Even this underestimates the real reduction in gastric capacitance after LSG because ingestion was limited to 400 ml liquid nutrient at pre-operative screening, whereas many healthy volunteers can drink > 1000 ml of the liquid nutrient used in this research [22].
To our knowledge, this is the first time that validated MR imaging techniques have been applied to assess gastric structure and function both before and after LSG. Moreover, there is no consensus concerning the optimal diameter or capacity of the residual stomach after LSG. Previous authors reported good outcomes in terms of weight loss in patients with residual gastric volume of 100–150 ml based on conventional barium imaging or 3D CT volumetry [25,26,27]. However, in these studies, the volume of contrast agent ingested was not standardized and similar measurements were not acquired prior to surgery. Notwithstanding these issues, MR measurements indicate that the surgery performed in Strasbourg produced results for residual gastric capacity after LSG that are in the same range as previous reports.
Effects of LSG on Gastric Emptying
As in previous MRI studies in healthy subjects [21, 23], analysis of these images revealed distinct early and late phases of GE. The early-phase of GE is determined mainly by physical factors including gastric capacitance and meal volume, such that the rate of early-phase GE is increased by medications that increase gastric tone and the volume of liquid nutrient ingested [23, 28]. The late-phase of GE is regulated also by neuro-hormonal feedback including the release of incretin peptide hormones (e.g., CCK, GLP-1) that is triggered by absorption of nutrients, such that late-phase GE is reduced by rapid delivery of nutrients into the small bowel [23]. In this study, consistent with prior observations, the reduction of gastric capacitance after LSG was associated with a significant increase in early-phase GE but a decrease in late-phase GE (Fig. 2). Analysis confirmed a significant inverse correlation between the reduction in TGV0 and early-phase GE with late-phase GE (Fig. 3). This dynamic, two-phase pattern is thought to be caused by rapid, early-phase delivery of liquid nutrient into the small bowel leading to activation of the “neurohormonal brake” which leads to subsequent slow, late phase emptying. This “fast then slow” emptying pattern for liquid nutrient test meals has also been observed in studies that have administered medications that increase gastric tone (decrease gastric accommodation) [28], and also in patients with functional dyspepsia with impaired accommodation documented by barostat [29]. Similar observations have been reported also by food engineering studies that manipulate particle size to modulate GE, nutrient absorption, and satiety [30,31,32]. Thus, ingestion of food that has been finely blended or that forms fine protein precipitates or fat emulsions on contact with acid is followed by rapid early-phase GE; however, rapid absorption of nutrients from the small bowel triggers neurohormonal feedback that slows subsequent, late-phase GE and prolongs gastric retention times [30,31,32].
Previous publications have reported the effect of LSG on GE; however, no consistent pattern has been established. Several authors reported increased GE rate; however, others noted no change or delayed emptying [5,6,7,8, 10, 33]. The lack of consensus regarding the effects of bariatric surgery on gastrointestinal physiology is, in part, related to the application of different methods to assess gastric emptying [10]. The dynamic change in GE rate that is documented by MR imaging after ingestion of a liquid nutrient test meal will be either absent or less pronounced after ingestion of a contrast agent with no calories or a solid test meal [22]. Further analysis of MR volume data shows that it is not adequate to describe GE using a single measurement (e.g., GE half-time (T50), retention time at 2 h). Additionally, the lack of standardized surgical technique could influence gastric function after LSG. For example, the distance of the staple line from the pylorus and the consequent effect of antrum preservation has been shown to effect GE rate [9].
Other Effects of LSG on Upper Gastrointestinal Function
In addition to MR imaging of gastric structure and function all patients completed esophageal high-resolution manometry (HRM) and ambulatory reflux monitoring before and after LSG. Consistent with previous reports [34, 35], and as reported previously [15], we documented significant reductions to the basal pressure and length of the esophago-gastric junction (EGJ) after LSG and these changes were associated with increased acid exposure in the distal esophagus. Additionally, patients with > 80% reduction in gastric capacitance had increased reflux events and reflux symptoms compared with the other groups (see “Discussion” in the recent paper [15]). It is known that new-onset reflux and other digestive symptoms can occur after LSG and this is one reason why quality of life (QoL) improves less than expected after bariatric surgery [36]. For example, a prospective randomized trial showed that approximately 1 in 3 patients who underwent LSG reported de novo GERD [3]. As expected, successful weight loss was linked to an increase in the GIQLI score at 6 months after LSG. However, at the same time, gastrointestinal symptoms (e.g., reflux, nausea) were often present and this impacted on the GI subdomain of the score (Fig. 4).
Factors Associated with Weight Loss and Quality of Life After LSG
The limitation of food intake due to gastric volume reduction is thought to be the most important mechanism of weight loss after LSG [37, 38]. This study provides new evidence supporting this hypothesis and also insights into the mechanism by which this is achieved.
A strong trend was present linking the reduction in total gastric volume produced by LSG and weight loss (p = 0.058). In particular, patients with the largest reduction in total gastric volume (> 80%) after ingestion of the test meal had greater weight loss at follow-up compared with other subjects (p = 0.008). Similarly, rapid early-phase GE was correlated with higher post-operative weight loss (p = 0.028). No similar result was found for late-phase GE (p = 0.201). Multiple linear regression analysis confirmed that both the reduction in gastric capacity and the rate of early-phase GE had statistically significant effects on patient weight loss. These findings support the contention that the efficacy of LSG is not only mediated by a physical reduction in gastric capacitance (restriction), but also by effects on gastric function and the neurohormonal regulation of satiation.
Few researchers have attempted to assess gastric capacity both before and after LSG; however, the current findings are consistent with those of previous researchers that reported a small residual gastric volume after LSG was associated with short and medium term weight loss [26, 27]. Using a different approach, Obeidat et al. showed that the volume of the resected stomach during LSG was associated with excess weight loss at 1 year after LSG [39]. More clinical scientists have assessed GE before and/or after LSG to test the hypothesis whether retention of food in the stomach and/or abnormal delivery of nutrients to the small bowel contributes to the reduction in food intake and weight loss after surgery [5,6,7,8,9,10]. No consistent result was obtained because of the use of different methods used to assess GE [22], and the dynamic change in GE rate after ingestion of the meal (discussed above). This study demonstrates that the reduction in gastric capacity after LSG increases the rate of early-phase GE. These effects are likely to be the mechanism by which LSG contributes to early satiation and prolonged satiety. Patients with a small residual stomach often ingested < 200 ml before maximum satiation was reached. Further, rapid delivery of food to the small bowel enhances nutrient absorption and the release of incretin hormones such as CCK and GLP-1 after a meal. Recent papers have shown that such effects appear to help patients lose weight and improve their glucose metabolism after bariatric surgery [33, 40, 41]. It should be noted that rapid delivery of nutrients is present also after laparoscopic Roux-en-Y gastric bypass surgery in which the pouch volume is even smaller (typically 30–50 ml) and emptying even more rapid than that of the stomach after LSG [42]. Future studies will test this mechanism explains improved glycemic control and weight loss after both these surgical procedures or, as is currently thought [41], whether different mechanisms apply.
In conclusion, objective MRI measurements before and after LSG demonstrate that this operation limits gastric capacity to 100–200 ml and also reduces gastric accommodation (i.e., reduced gastric volume increase for a given volume load). These changes have important effects on gastric function with fast early-phase emptying with rapid delivery of nutrients to the small bowel being followed by slow late-phase gastric emptying. Multivariate analysis demonstrated significant effects of LSG on both gastric structure (capacity) and function (early gastric emptying) on patient outcome including weight loss. Specifically, this study provides new evidence that the reduction in gastric capacity is directly related to weight loss; however, if taken too far, this comes at the expense of worse outcomes in terms of high rates of reflux and other gastrointestinal symptoms that impair quality of life.
Important variation in terms of weight loss and gastrointestinal symptoms after LSG were present even in this single-center study in which all operations were performed by the same surgical team using the same surgical technique and bougie of same size. This suggests that the key to optimizing patient outcomes is a better standardization of the procedure, for example, by the use of intra-operative monitoring of EJG function and gastric morphology either by gastric imaging or, potentially, the use of the endoscopic functional luminal imaging probe (Endo-FLIP).
Notes
The increase in TGV after a liquid test meal is often less than the volume ingested because the rate of early-phase GE is greater than the rate of secretion.
References
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the Fourth IFSO Global Registry Report. Obes Surg. 2018:2019.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric Surgery Worldwide. Obes Surg. 2013:2015.
Peterli R, Wölnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity. Jama. 2018;319:255. https://doi.org/10.1001/jama.2017.20897.
Yehoshua RT, Eidelman LA, Stein M, et al. Laparoscopic sleeve gastrectomy - volume and pressure assessment. Obes Surg. 2008;18:1083–8.
Baumann T, Kuesters S, Grueneberger J, et al. Time-resolved MRI after ingestion of liquids reveals motility changes after laparoscopic sleeve gastrectomy-preliminary results. Obes Surg. 2011;21:95–101.
Bernstine H, Tzioni-Yehoshua R, Groshar D, et al. Gastric emptying is not affected by sleeve gastrectomy-scintigraphic evaluation of gastric emptying after sleeve gastrectomy without removal of the gastric antrum. Obes Surg. 2009;19:293–8.
Braghetto I, Davanzo C, Korn O, et al. Scintigraphic evaluation of gastric emptying in obese patients submitted to sleeve gastrectomy compared to normal subjects. Obes Surg. 2009;
Shah S, Shah P, Todkar J, et al. Prospective controlled study of effect of laparoscopic sleeve gastrectomy on small bowel transit time and gastric emptying half-time in morbidly obese patients with type 2 diabetes mellitus. Surg Obes Relat Dis. 2010;
Garay M, Balagué C, Rodríguez-otero C, Gonzalo B, Domenech A, Pernas JC, et al. Influence of antrum size on gastric emptying and weight-loss outcomes after laparoscopic sleeve gastrectomy (preliminary analysis of a randomized trial). Surg Endosc. Springer US; 123AD;0:0. https://doi.org/10.1007/s00464-017-5972-4
Melissas J, Leventi A, Klinaki I, et al. Alterations of global gastrointestinal motility after sleeve gastrectomy: a prospective study. Ann Surg. 2013;258:976–82.
Pilone V, Tramontano S, Di Micco R, et al. Gastric emptying after sleeve gastrectomy: statistical evidence of a controlled prospective study with gastric scintigraphy. Minerva Chir. 2013;
Azpiroz F, Feinle-Bisset C, Grundy D, et al. Gastric sensitivity and reflexes: basic mechanisms underlying clinical problems. J Gastroenterol. 2014;49:206–18.
Grundy SM, Barondess JA, Bellegie NJ, et al. Gastrointestinal surgery for severe obesity. Ann Intern Med. 1991;
Fiorillo C, Quero G, Vix M, et al. 6-Month Gastrointestinal Quality of Life (QoL) Results after endoscopic sleeve gastroplasty and laparoscopic sleeve gastrectomy: a propensity score analysis. Obes Surg. 2020; https://doi.org/10.1007/s11695-020-04419-1.
Quero G, Fiorillo C, Dallemagne B, et al. The causes of gastroesophageal reflux after laparoscopic sleeve gastrectomy: quantitative assessment of the structure and function of the esophagogastric junction by magnetic resonance imaging and high-resolution manometry. Obes Surg. 2020;30:2108–17.
Fuchs KH, Babic B, Breithaupt W, Dallemagne B, Fingerhut A, Furnee E, et al. EAES recommendations for the management of gastroesophageal reflux disease. Surg Endosc. 2014;
Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of Esophageal Motility Disorders v3.0. Neurogastroenterol Motil. 2016;
Gyawali CP, Kahrilas PJ, Savarino E, Zerbib F, Mion F, Smout AJPM, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut [Internet]. 2018;gutjnl-2017-314722. Available from: https://doi.org/10.1136/gutjnl-2017-314722, 2018
Prakash Gyawali C, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;
Curcic J, Fox M, Kaufman E, et al. Gastroesophageal junction: structure and function as assessed by using MR imaging. Radiology. 2010;257:115–24.
Parker H, Hoad CL, Tucker E, et al. Gastric motor and sensory function in health assessed by magnetic resonance imaging: establishment of reference intervals for the Nottingham test meal in healthy subjects. Neurogastroenterol Motil. 2018;30:e13463.
Parker HL, Tucker E, Hoad CL, et al. Development and validation of a large, modular test meal with liquid and solid components for assessment of gastric motor and sensory function by non-invasive imaging. Neurogastroenterol Motil. 2016;
Kwiatek MA, Menne D, Steingoetter A, et al. Effect of meal volume and calorie load on postprandial gastric function and emptying: studies under physiological conditions by combined fiber-optic pressure measurement and MRI. Am J Physiol - Gastrointest Liver Physiol. 2009;297:G894–901.
Schwizer W, Steingoetter A, Fox M. Magnetic resonance imaging for the assessment of gastrointestinal function. Scand J Gastroenterol. 2006;41:1245–60.
Braghetto I, Cortes C, Herquiñigo D, et al. Evaluation of the radiological gastric capacity and evolution of the BMI 2-3 years after sleeve gastrectomy. Obes Surg. 2009;19:1262–9.
Alvarez V, Carrasco F, Cuevas A, et al. Ghiardo D, et al. Nutrition: Mechanisms of long-term weight regain in patients undergoing sleeve gastrectomy; 2016.
Hanssen A, Plotnikov S, Acosta G, et al. 3D Volumetry and its correlation between postoperative gastric volume and excess weight loss after sleeve gastrectomy. Obes Surg. 2018;28:775–80.
Kwiatek MA, Fox MR, Steingoetter A, et al. Effects of clonidine and sumatriptan on postprandial gastric volume response, antral contraction waves and emptying: an MRI study. Neurogastroenterol Motil. 2009;21:928–e71.
Tucker E, Parker H, Hoad C, et al. PWE-048 gastric volume response and emptying after a large liquid nutrient meal in functional dyspepsia and health assessed by non-invasive gastric scintigraphy (GS) and MRI: a pilot study to identify candidate biomarkers. Gut. 2012;61:A316.1–A316.
Fox M, Georgi G, Boehm G, et al. Thumshirn M. Clin Nutr: Dietary protein precipitation properties have effects on gastric emptying in healthy volunteers; 2004.
Marciani L, Hall N, Pritchard SE, et al. Preventing gastric sieving by blending a solid/water meal enhances satiation in healthy humans. J Nutr. 2012;
Steingoetter A, Radovic T, Buetikofer S, et al. Imaging gastric structuring of lipid emulsions and its effect on gastrointestinal function: a randomized trial in healthy subjects. Am J Clin Nutr. 2015;101:714–24.
Mans E, Serra-Prat M, Palomera E, et al. Sleeve gastrectomy effects on hunger, satiation, and gastrointestinal hormone and motility responses after a liquid meal test1. Am J Clin Nutr. 2015;102:540–7.
Braghetto I, Lanzarini E, Korn O, et al. Manometric changes of the lower esophageal sphincter after sleeve gastrectomy in obese patients. Obes Surg. 2010;
Burgerhart JS, Schotborgh CAI, Schoon EJ, et al. Effect of sleeve gastrectomy on gastroesophageal reflux. Obes Surg. 2014;
Strain GW, Saif T, Gagner M, et al. Cross-sectional review of effects of laparoscopic sleeve gastrectomy at 1, 3, and 5 years. Surg Obes Relat Dis. 2011;7:714–9.
Baltasar A, Serra C, Pérez N, et al. Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation. Obes Surg. 2005;15:1124–8.
Melissas J, Koukouraki S, Askoxylakis J, Stathaki M, Daskalakis M, Perisinakis K, et al. Sleeve gastrectomy - a restrictive procedure? Obes Surg. 2007;
Obeidat FW, Shanti HA, Mismar AA, et al. Volume of resected stomach as a predictor of excess weight loss after sleeve gastrectomy. Obes Surg. 2014;
Papamargaritis D, Le Roux CW, Sioka E, Koukoulis G, Tzovaras G, Zacharoulis D. Changes in gut hormone profile and glucose homeostasis after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2013;
Svane MS, Bojsen-Møller KN, Martinussen C, et al. Postprandial nutrient handling and gastrointestinal hormone secretion after Roux-en-Y gastric bypass vs sleeve gastrectomy. Gastroenterology. 2019;
Riccioppo D, Santo MA, Rocha M, et al. Small-volume, fast-emptying gastric pouch leads to better long-term weight loss and food tolerance after Roux-en-Y gastric bypass. Obes Surg. 2018;
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(TIFF 40.4 kb)
Rights and permissions
About this article
Cite this article
Fiorillo, C., Quero, G., Dallemagne, B. et al. Effects of Laparoscopic Sleeve Gastrectomy on Gastric Structure and Function Documented by Magnetic Resonance Imaging Are Strongly Associated with Post-operative Weight Loss and Quality of Life: a Prospective Study. OBES SURG 30, 4741–4750 (2020). https://doi.org/10.1007/s11695-020-04831-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04831-7