Abstract
Background
One-anastomosis gastric bypass (OAGB) has gradually gained in popularity. Evidence of the validity of the technique and the quality of life in the longer term is scarce. The aim of this study was to retrospectively evaluate the longitudinal (≥ 5 years) safety, weight-loss efficacy, comorbid disease improvement, and quality of life of patients following OAGB.
Methods
Data from patients who underwent OAGB from January 2009 to December 2011 were retrospectively reviewed. Preoperative clinical characteristics and data through 8 years were analyzed.
Results
A total of 163 patients completed 5 to 8 years of follow-up with a mean age of 41 ± 11.4 years (22–65). Ninety-four patients (57.6%) had undergone prior bariatric surgery (gastric band). Mean body mass index (BMI, kg/m2) at the time of OAGB was 41.2 ± 6.5 (range 30.1–50.6). Twenty-one patients (13.0%) suffered from type 2 diabetes mellitus (T2DM), 59 (36.2%) hypertension, 31 osteoarthritis (19.0%), and 24 had obstructive sleep apnea (14.7%). At 5, 6, 7, and 8 years of follow-up, respective mean BMI reduction was 12.6 (n = 163), 11.8 (n = 100), 10.7 (n = 82), and 8.8 (n = 40). Respective mean excess weight loss was 81.8 ± 23.6%, 75.9 ± 20.8%, 69.1 ± 20.4%, and 62.3 ± 23.4%. All obesity-related comorbidities decreased significantly at follow-up time points. Five patients (3%) underwent laparoscopic reoperation within 90 days after surgery. Incidence of recurrent reflux was 14.0%. At a mean follow-up of 92 months (76–111), improved or greatly improved quality of life was reported by 86.0% of patients.
Conclusion
OAGB provided very good weight loss, comorbidity improvement, and quality of life at follow-up of ≥ 5 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the initial study by Rutledge (2001) [1], the one-anastomosis gastric bypass (OAGB) has experienced controversy, yet gained steadily in popularity. A 2018 systematic review summarized outcomes in 12,807 OAGB patients [2], suggesting that it is now a widely established procedure. Also, a recent worldwide survey of bariatric procedures reported a continuing upward trend in OAGB use [3], noting that the actual number of procedures performed is likely underestimated, as OAGB data were not provided by the United States and Canada in this global summary.
As evaluated by systematic review [2, 4], multiple studies demonstrate OAGB efficacy and safety despite the continued controversy associated with the procedure. A 2018 position statement from the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) attempted to end the equivocation by officially recognizing the OAGB as effective and safe [5]. Yet, a number of surgeons continue to contest the safety of this procedure [6]. One of the main arguments against the OAGB is its correlation with chronic biliary reflux and the theorized increased risk of esophageal and gastric cancer development over time [7, 8].
There is no ideal bariatric operative technique. Although the trend worldwide is to perform the simplest, easiest, and least-invasive procedure [3], each procedure has unique characteristics that require consideration in relation to the individual patient. In 2013, sleeve gastrectomy (SG) overtook Roux-en-Y gastric bypass (RYGB) as the most frequently performed bariatric procedure in the world [9]. Similarly, the simpler OAGB technique compared to that of RYGB, together with the promising weight-loss outcomes of OAGB, is attractive to many surgeons.
Obesity is a chronic disease, and any weight reduction surgery should be durable. Studies should include assessment of the quality of life (QoL) experienced by patients after OAGB over the long term. To date, few studies have reported mid- or long-term OAGB outcomes. Moreover, to the best of our knowledge, no published QoL study has followed OAGB patients beyond 5 years of surgery. The current study aimed to evaluate the long-term efficacy, safety, and QoL of patients following OAGB.
Methods
Study Design
A retrospective review of patients who underwent OAGB in our center between January 2009 and December 2011 was performed. All patients met the international criteria for bariatric surgery (i.e., European Guidelines [10]; US National Institutes of Health 1991 Guidelines [11]).
Patients
Patients underwent a preoperative work-up, including upper gastrointestinal (GI) endoscopy with Helicobacter pylori screening, and were evaluated by a multidisciplinary team specialized in bariatric and metabolic surgery. The exclusion criteria for OAGB were super obese patients with body mass index (BMI) > 50 kg/m2, and patients younger than 18 years old or older than 65 years old. Patients who had undergone a previous bariatric procedure or who had a hiatal hernia were not excluded. BMI and obesity-related diseases were evaluated in relation to longitudinal weight loss, change in comorbid disease, and early (< 30 days) and late complications.
Outcome Evaluation
Effectiveness end points included BMI, percentage of excess weight loss (%EWL), improvement/resolution of obesity-related comorbidities, and quality of life (QoL). Weight loss was calculated as reduction in BMI and percentage of excess weight loss (%EWL, calculated as [initial weight − follow-up weight] × 100 / [initial weight − ideal weight]; ideal weight was set as that equivalent to a BMI of 25 kg/m2.) Weight regain was defined as a gain of at least 25.0% of the weight from that measured at postoperative weight nadir.
Criteria used for diagnosis or remission of obesity-related metabolic disorders were remission of hypertension (blood pressure < 135/85 mm Hg without medication) and remission of type 2 diabetes mellitus (fasting glucose < 126 mg/dL with HbA1C < 6.5% without medication). Reflux was defined as the presence of symptoms despite the use of medication. Remission of sleep apnea was based on each patient’s statement and their cessation of continuous positive airway pressure machine usage. Improvement of osteoarthritis was evaluated based on symptoms and mobility. Serum level of albumin was used to assess biological malnutrition; severe albumin deficiency was defined as < 3.0 g/dL.
The Moorehead-Ardelt II questionnaire [12] was used to assess patient QoL. Questionnaires were completed by mail or telephone calls. The questionnaire examines 6 keys area: self-esteem, physical wellbeing, social relationships, work, sexuality, and food perception. Two “yes/no” questions were added at the end of the questionnaire: “Would you have OAGB done again?” and “Would you recommend this intervention to friends or family?” All patients were individually interviewed at or beyond 6 years of surgery.
Surgical Technique
For those patients who had conversion surgery from band to OAGB due to inadequate weight loss, the procedure was completed in two stages—first, LAGB removal, later followed by the OAGB procedure. A subgroup comparison of the two procedures was performed.
Patients underwent OAGB according to one standardized procedure. All operations were performed laparoscopically. The operating table was tilted to the reverse Trendelenburg position. Pneumoperitoneum was obtained by a Veress needle inserted in the left hypochondrium. OAGB was performed using 5 trocars (2 × 12 mm, 1 × 11 mm, and 2 × 5 mm). The first step was to ensure the jejunum reached the stomach and the anastomosis could be completed free of tension. The small bowel was measured to 150 cm from the duodenojejunal junction. The biliopancreatic limb length was 150 cm in all procedures regardless of patient BMI. Dissection was begun at the crow’s foot to access the lesser sac. The first staple was applied with a 45-mm cartridge. The size of the gastric tube was calibrated with a 36 Fr orogastric bougie. The gastric transection was performed using sequential applications of a 60-mm linear stapler. The lateral gastrojejunal anastomosis was accomplished by stapled anastomosis after creation of the 150-cm biliopancreatic limb. The enterotomy closure was completed using continuous V-lock sutures. Intraoperative leak test was systematically performed. Petersen’s space was not closed. No drain or nasogastric tube was placed; patients started a liquid diet the day of surgery and were discharged typically 2 days following surgery.
Statistical Analysis
Analyses were performed using the SPSS statistical package (version 20; IBM, Chicago, IL). Continuous data were presented using means, standard deviations, and/or ranges; 95% confidence intervals (CIs) were calculated for weight outcome variables. Categorical data were presented using frequencies and percentages.
Results
Studied Population
During the study period, 295 patients underwent an OAGB procedure. Among them, 132 patients had fewer than 5 years of follow-up and therefore were excluded from the data analysis. A total of 163 patients completed long-term study follow-up of ≥ 5 years. The mean follow-up was 82 months (60–111) with 100% at 5-year follow-up and 48.5% at 7-year follow-up (Table 1).
The mean age of patients at baseline was 41 ± 11.4 years (range 22–65) in a predominantly female cohort (129 females, 34 males) with a preoperative mean BMI of 41.2 ± 6.5 kg/m2 (30.1–50.6). Ninety-four (57.6%) had undergone previous bariatric surgery (laparoscopic adjustable gastric band [LAGB]). Twenty-one patients suffered from T2DM (13.0%), 59 (36.2%) hypertension, 31 osteoarthritis (19.0%), and 24 had obstructive sleep apnea (14.7%).
Weight Loss
At 92 months, mean excess weight loss (EWL) was 68.9 ± 22.8%, (95% CI 64.4, 73.4). Mean BMI was 29.7 ± 12.9 kg/m2, representing an overall BMI reduction of 10.6 kg/m2 (95% CI 7.8, 13.4). At 5, 6, 7, and 8 years of follow-up, respectively, mean EWL was 81.8 ± 23.6%, 75.9 ± 20.8%, 69.1 ± 20.4%, and 62.3 ± 23.4% and mean BMI decreased to 27.7 ± 4.7, 28.5 ± 3.7 kg/m2, 29.6 ± 3.3 kg/m2, and 31.5 ± 4.1 kg/m2.
A comparison between moderately obese (BMI 30–40, n = 72) and severely obese patients (BMI 40–50, n = 91) was performed (Table 2). The average preoperative BMI of these 2 groups was 36.5 ± 2.3 and 43.7 ± 2.9 kg/m2, respectively. The two groups had comparable baseline characteristics, including age (p = 0.36) and gender (p = 0.63). In the severely obese group, %EWL was somewhat higher than in the moderately obese group, though the difference was not significant (p = 0.621). The rate of weight regain did not differ between the studied groups (p = 0.85).
A comparison between conversion OAGB group (due to prior weight-loss failure, n = 94) and primary OAGB group (n = 63) was performed in the 94/163 (57.7%) patients who completed the ≥ 5-year OAGB study. The two groups were comparable in baseline characteristics, including age (p = 0.44) and gender (p = 0.81). Baseline BMI was significantly higher in the primary OAGB group (p = 0.04). The revision group experienced less weight loss than the primary group. There was no significant difference in their rate of GERD (Table 3).
Comorbidities
At long-term follow-up, all obesity-related comorbid diseases had improved significantly or resolved. Patients presenting with T2DM, hypertension, osteoarthritis, and sleep apnea improved/resolved in 82.4%, 81.3%, 80.6%, and 79.2%, respectively (Table 4).
Complications
There was no biological malnutrition, defined as severe albumin deficiency. Hemoglobin levels of < 10 g/dL were seen in 17 patients (10.4%). All patients received routine multivitamin complex supplementation for 6 months after surgery. There were no perioperative complications. There was one early complication (anastomotic leakage). Five patients (3.0%) underwent laparoscopic reoperation at ≤ 90 days after surgery. These GI complications included hematoma, GI, early anastomotic, or staple line bleeding. Six patients (3.7%) underwent reintervention for delayed complications (> 90 days postoperative). These included 1 incisional hernia, 2 perforated ulcers, and 3 patients with recurrent heartburn requiring conversion to RYGB. One of these 3 patients had preoperative reflux symptoms. All of the patients with ulcers were smokers. There were no thromboembolic events (e.g., deep venous thrombosis, pulmonary embolism) observed. There was no mortality.
Gastroesophageal Reflux
Reflux was defined in the study as a typical symptom such as heartburn or regurgitation, present despite the use of a reflux medication (e.g., proton pump inhibitor [PPI]). Proton pump inhibitors were systematicaly prescribed for 1 month after surgery. After this period, the PPI was continued only in case of GERD symptoms. Respective incidence of at least weekly recurrent reflux, and daily reflux was 14.0% and 3.0%. The incidence of new onset gastroesophageal reflux was 11.0%.
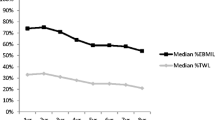
Quality of Life
QoL was assessed using the Moorehead-Ardelt II (MA-II) questionnaire, completed by each patient at a median of 92 months (76–111). This questionnaire examines 6 keys area: self-esteem, physical wellbeing, social relationships, work, sexuality, and food perception. Points are added or subtracted according to a patient’s response. Patients were classified as having “very good,” “good,” “fair,” “poor,” and “very poor” QoL (Fig. 1). Of note, no patients classified themselves as having a score of “very poor,” and only 5 classified themselves as experiencing “poor” QoL using the MA-II scoring system. All of them were refluxers. A majority of patients (79.0%) reported an improved or greatly improved QoL following the surgery.
Two “Yes/No” questions were added by our center at the end of the questionnaire: “Would you have OAGB done again?” and “Would you recommend this intervention to friends or family?” Most patients (86.0%) respond “Yes” to both questions.
Discussion
The current report presents the long-term follow-up of our OAGB cohort. The results suggest that the OAGB procedure, as described, is both safe and effective. There was no mortality, weight loss was excellent, and all comorbidities improved or resolved in the majority of patients.
More than half of our patients had a previous LAGB, which was considered an attractive procedure due to its simplicity and good short-term results. However, this procedure is associated with substantial failure over time. The current study demonstrates that the conversion of LAGB to OAGB for weight-loss failure is safe and feasible and provides good results. Nonetheless, the weight-loss benefit in patients converted from LAGB to OAGB remained lower than after primary OAGB surgery.
The adverse effects of morbid obesity on QoL and physical performance are widely known. Although evaluation of QoL has gained attention and is considered the third element of the “bariatric triple assessment,” along with weight loss and resolution of comorbidities, published QoL evidence is relatively scarce after OAGB. In this study, improved QOL in 79.0% was demonstrated using the translated, validated, and disease-specific MA-II questionnaire. Notably, 86.0% of our patients would again choose to undergo the same procedure.
Three patients in this study had symptomatic biliary reflux requiring revision surgery. OAGB exposes the gastric mucosa to bile. OAGB patients may have a higher gastric bile concentration, similar to that of patients who have undergone the Mason loop gastric bypass. Yet, a major difference between the 2 procedures is the length of the gastric pouch. The Mason loop features a high transverse gastric pouch based on the fundus, and the OAGB features a long narrow gastric pouch based on the lesser curvature. Another major difference is the anastomosis itself, which in OAGB is vertical or slightly oblique in the posterior wall of the pouch, favors gastric emptying, and potentially averts significant reflux. The perceived potential risk of Barrett’s esophagus and esophageal cancer may be due to the biliary reflux into the esophagus, although a long, narrow gastric pouch should make esophageal biliary reflux less likely compared to the shorter loop gastric bypass.
The role of biliary reflux in esophageal cancer remains hotly debated; it is surprising that the role of acid reflux is generally not considered a cancer concern. Recently, Felsenreich et al. published a study of SG in which they found a high incidence of reflux 10 years after surgery [13]. Indeed, more than half of the patients presented with esophageal reflux, and Barrett’s metaplasia was found in 14.0% of their SG patients. Patients with Barrett’s esophagus develop esophageal adenocarcinoma more frequently than the general population. The annual risk of progression to esophageal adenocarcinoma varies from 0.3 to 7.0%, depending on the grade of dysplasia [14]. As SG is the most frequently performed primary bariatric procedure worldwide, the long-term complication of this procedure should be of concern for several hundred thousand patients annually [3, 15].
Malnutrition has been reported with the OAGB procedure and may result in the need for revisional surgery. Rutledge et al. observed malnutrition in 31 of 2401 patients [16]. It is commonly believed that this procedure is more malabsorptive than RYGB, which may account for the superior weight loss. The longer the biliopancreatic limb, the more aggressive metabolic effect and superior EWL are typically; however, the risk of severe complications of liver failure and severe malnutrition is also higher. In the current study of 163 patients, there were no cases of malnutrition. We believe this may due to the length of the biliopancreatic limb used in our center (always < 150 cm). Also, our very close follow-up and cooperation between the patients and the bariatric team may have contributed to the avoidance of this complication. Oral protein supplementation and multivitamins or trace elements were often prescribed to patients. A baseline BMI of 35–50 did not appear to influence weight loss or weight regain. Our study demonstrated that a 150-cm biliopancreatic limb length is adequate for patients with a BMI of 35–50 kg/m2. This length provides good results with very minimal nutritional complications.
We previously performed laparoscopic sleeve gastrectomy (LSG) in super obese patients (BMI ≥ 50 kg/m2) due to excess abdominal and omental fat. No standard technique has been established for the length of the bypassed limb, which may result in the reported variability in OAGB weight loss and malnutrition. As noted in the IFSO Statement, a randomized controlled trial is needed to define an optimized OAGB operative technique [5].
The OAGB is an easier surgical technique than RYGB, resulting in a shorter learning curve and shorter operative time [9]. Lee et al. estimated the learning curve for OAGB to be 30 cases fewer than that for RYGB [17]. Obviating the need for a jejuno-jejunostomy reduces the number of sites for leakage. OAGB may be a simpler and safer alternative to RYGB [18]. A recent review suggested that OAGB is safe and effective in the super obese population and comparable to LSG and RYGB [19]. Further, the RYGB jejuno-jejunal anastomosis may lead to chronic left abdominal pain related to internal herniation and bacterial overgrowth.
OAGB is not associated with internal hernia, which is a distinct advantage relative to the high incidence of internal hernia with RYGB (≤ 14.0%). However, Petersen’s space is enlarged after laparoscopic OAGB, although very few cases of Petersen’s hernia have been reported, likely due to the absence of a mesenteric dissection. In our surgical technique, Petersen’s space was never closed; none of our 163 patients developed an internal hernia during the follow-up of 5–8 years.
Conclusion
To our knowledge, this is the first study to describe long-term safety, efficacy, and QoL following OAGB. At ≥ 5-year follow-up, OAGB was safe and effective for weight loss and reduction of obesity-related diseases, and patients were satisfied with their quality of life.
References
Rutledge R. The mini-gastric bypass: experience with the first 1274 cases. Obes Surg. 2001;11(3):276–80.
Parmar CD, Mahawar KK. One-anastomosis (mini) gastric bypass is now an established bariatric procedure: a systematic review of 12,807 patients. Obes Surg. 2018;28(9):2956–67.
Angrisani L, Santonicola A, Iovino P, et al. IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018;28(12):3783–94.
Georgiadou D, Sergentanis TN, Nixon A, et al. Efficacy and safety of laparoscopic mini gastric bypass: a systematic review. Surg Obes Relat Dis. 2014;10:984–91.
De Luca M, Tie T, Ooi G, et al. Mini gastric bypass–one anastomosis gastric bypass (MGB-OAGB)–IFSO position statement. Obes Surg. 2018;28(5):1188–206.
Mahawar KK, Borg C-M, Kular KS, et al. Understanding objections to one anastomosis (mini) gastric bypass: a survey of 417 surgeons not performing this procedure. Obes Surg. 2017;27(9):2222–8.
Guirat A, Addossari HM. One anastomosis gastric bypass and risk of cancer. Obes Surg. 2018;28(5):1441–4.
Aggarwal S, Bhambri A, Singla V, et al. Adenocarcinoma of oesophagus involving gastro-oesophageal junction following mini-gastric bypass/one anastomosis gastric bypass. J Minim Access Surg. 2019; https://doi.org/10.4103/jmas.JMAS_320_18.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery and endoluminal procedures: IFSO worldwide survey 2014. Obes Surg. 2017;27(9):2279–89.
Fried M, Hainer V, Basdevant A, et al. Inter-disciplinary European guidelines on surgery of severe obesity. Int J Obes. 2007;31(4):569–77.
NIH Consensus Development Conference Statement: gastrointestinal surgery for severe obesity. Obes Surg 1991;1:243-256.
Moorehead MK, Ardelt-Gattinger E, Lechner H, et al. The validation of the Moorehead-Ardelt quality of life questionnaire II. Obes Surg. 2003;13(5):684–92.
Felsenreich DM, Ladinig LM, Beckerhinn P, et al. Update: 10 years of sleeve gastrectomy—the first 103 patients. Obes Surg. 2018;28(11):3586–94.
Singh T, Sanaka MR, Thota PN. Endoscopic therapy for Barrett’s esophagus and early esophageal cancer: where do we go from here? World J Gastrointest Endosc. 2018;10(9):165–74.
Oor JE, Roks DJ, Ünlü C, et al. Laparoscopic sleeve gastrectomy and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Surg. 2016;211(1):250–67.
Rutledge R, Walsh TR. Continued excellent results with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg. 2005;15(9):1304–8.
Lee WJ, Yu PJ, Wang W, et al. Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity: a prospective randomized controlled clinical trial. Ann Surg. 2005;242(1):20–8.
Lee WJ, Lin YH. Single-anastomosis gastric bypass (SAGB): appraisal of clinical evidence. Obes Surg. 2014;10:1749–56.
Parmar CD, Bryant C, Luque-DeLeon E, et al. One anastomosis gastric bypass in morbidly obese patients with BMI ≥ 50 kg/m2: a systematic review comparing it with Roux-en-Y gastric bypass and sleeve gastrectomy. Obes Surg 2019 Sep;29(9):3039-3046.
Acknowledgments
We thank J.N. Buchwald, Medwrite Medical Communications, WI, USA, for substantial assistance with manuscript development.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all participants.
Human and Animal Rights
The study was performed in accord with the ethical standards of the Declaration of Helsinki.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Neuberg, M., Blanchet, MC., Gignoux, B. et al. Long-Term Outcomes After One-Anastomosis Gastric Bypass (OAGB) in Morbidly Obese Patients. OBES SURG 30, 1379–1384 (2020). https://doi.org/10.1007/s11695-019-04287-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04287-4