Abstract
Background
One-anastomosis gastric bypass (OAGB) is gaining more attention in patients with severe obesity and recently is used for patients with body mass index (BMI) < 35 kg/m2. In this 5-year single center experience we aim to report our outcomes of using OAGB for patients with BMI < 35 kg/m2.
Methods
This is a retrospective analysis of prospectively collected data recorded in to our national obesity registry database. Variables including age, sex, weight, BMI, any associated disease, blood levels of metabolic markers, nutrients, and vitamins before and after surgery were extracted and analyzed.
Results
173 patients with mean age and BMI of 41 ± 10 years and 33 ± 1 kg/m2 underwent OAGB and at least one of the obesity-associated medical problems was found in 88 (50.5%) of them preoperatively. The mean duration of surgery and length of hospital stay were 60.7 ± 7.4 min and 1.3 ± 1.4 days. 78% and 70% of patients had available data at 24 and 60 months, respectively. The mean BMI was 23.9 ± 2.2 kg/m2 1 year after surgery and each year after that till 5 years was 24 ± 2, 24.4 ± 2.6, 25.1 ± 2.7, and 25.5 ± 2.7 kg/m2. Significant improvement in levels of fasting blood glucose, lipid profile, and liver enzymes were observed.
Conclusion
OAGB for BMI < 35 kg/m2 has significant effects in weight loss, helps remit diabetes and hypertension in the majority of cases, improves lipid profile, and has no increased burden of postoperative problems or deficiency in nutritional factors rather than what is known and predictable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In the most recent International Federation for Surgery of Obesity (IFSO) and American Society for Metabolic and Bariatric surgery (ASMBS) guidelines, the body mass index (BMI) threshold for metabolic bariatric surgery (MBS) has been lowered and it is recommended in patients with type 2 diabetes mellitus (T2DM) and BMI ≥ 30 kg/m2 or individuals with a BMI of 30–34.9 kg/m2 who do not achieve a considerable weight loss or improvement in a list of comorbidities using nonsurgical methods [1,2,3,4,5,6,7]. Based on the supported data, sleeve gastrectomy (SG) and Roux-en-Y gastric bypass (RYGB) are among the highly recommended procedures [1, 2]. Absolutely evident that these international authorities came to conclusion to recommend MBS to patients with BMI < 35 kg/m2 grounded on the published data by many researchers around the world showing safety, efficacy, and sustainability of surgical weight loss over community weight loss programs before become published in guidelines. However, One Anastomosis Gastric Bypass (OAGB) as one of the popular MBS procedures has been rapidly gaining momentum in recent years [8, 9]; ranking third in the list of most frequently performed primary MBS worldwide and first in some countries [10]. OAGB shows favorable outcomes, including short operative time, low perioperative complication rate, significant weight loss, and good remission of obesity associated medical problems [11,12,13]. Therefore, OAGB has been approved as a standard procedure for the treatment of severe obesity with or without associated medical problems [8, 9, 12,13,14]. However, the safety and efficacy of OAGB for patients with a BMI < 35 kg/m2 are still controversial, as there is limited evidence reporting OAGB for this group of obesity [15]. A large international survey of bariatric surgeons declared reversible procedure is more preferable than irreversible approaches such as SG; however, they have performed more SG and RYGB for adult patients with class I obesity instead of OAGB, which may relate to its unknown outcomes in this group, being approved as one of the MBS procedures by IFSO and ASMBS in recent years, or surgical team’s preference [4]. Furthermore, after many years of investigation and publication, there are still controversial aspects in its surgical steps such as pouch size and biliopancreatic limb (BPL) length [16,17,18]. A systematic review with 376 pooled patients showed that the safety and metabolic efficacy of OAGB for patients with T2DM with BMI < 35kg/m2 is at least as good as, if not superior to, SG and RYGB [15]. As stated by the systematic review, due to the limited number of studies with large samples and long duration, OAGB in class I obesity needs more evaluations [15]. Moreover, we need to know does OAGB work for patients with class I obesity and no obesity-related medical problem who failed to lose weight with nonsurgical methods. Therefore, in this study, we aim to report our 5-year experience of OAGB in patients with BMI < 35 kg/m2 from a high-volume center of excellence for MBS with a high referral rate.
Materials and methods
Design and settings
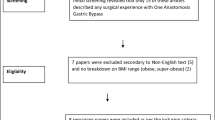
A retrospective study on prospectively collected data was conducted on a sample of 182 patients who underwent OAGB between 2012 and 2023 and had a 30 ≤ BMI < 35 kg/m2. Among them, eight secondary conversional OAGB were excluded. The indication for MBS in our center was based on the available treatment of obesity published by IFSO and ASMBS and their following amendments [2, 6,7,8,9, 14, 19]. The necessary data for the study were obtained from our national registry database of obesity surgery (INOSD) [20]. Choosing BPL (range, 100–200 cm) was based on the our institutional expert panel discussion and final decision by the leading surgeon due to lack of international consensus for this group and an ongoing debate on the proper BPL length for OAGB even for this specific BMI group [4, 16, 17]. All patients provided their consent for the surgery and usage of their information with perseveration of their personal information confidential.
Extracted variables were as follow: age, sex, preoperative weight, height, BMI, obesity-associated medical problems [i.e. T2DM, hypertension (HTN), hyperlipidemia (HLP), obstructive sleep apnea (OSA)] or any other disease found during preoperative evaluations (e.g., hypothyroidism, heartburn, low back pain, knee pain, and polycystic ovary syndrome), available weight and BMI at each post-operative visit, and before and after surgery reports of hematologic and metabolic factors including blood glucose [fasting as FBS and glycosylated hemoglobin; HbA1c), lipid profile (including triglyceride (TG), total cholesterol (TC), high- and low-density lipoprotein (HDL and LDL, respectively)], nutritional status [including albumin (Alb), hemoglobin, and important vitamins and minerals (vitamin B12, folic acid, vitamin D3, ferritin, calcium, and zinc)], liver enzyme [i.e., aspartate and alanine aminotransferases (AST and ALT, respectively) and alkaline phosphatase (ALK)], uric acid, and thyroid stimulating hormone.
Statistical analysis
Quantitative and qualitative variables were expressed as mean ± standard deviation (SD) and number (percentage), respectively. Each variable checked for normal distribution with Q-Q plot and their appropriate tests (Shapiro–Wilk or Kolmogorov–Smirnov). The chi-square test was used for evaluating the association between nominal variables and t test (paired and independent) was used for numerical variables between two groups. A p value less than 0.05 was considered significant. Statistical Package for the Social Sciences (SPSS) Statistics for Windows, version 25.0 (SPSS Inc., Chicago, USA) was used for all analyses.
Results
Preoperative
In total, 173 patients with class I obesity underwent OAGB with 83% female predominance. The mean age and BMI before surgery were 41 ± 10 years (range 15 to 70 years) and 33.4 ± 1.3 kg/m2, respectively. The preoperative characteristics of included patients are shown in Table 1. At least one of the obesity-associated medical problems was found in 88 (50.5%) of the patients before surgery. For weight loss before the surgery, 82 (47.1%), 125 (71.8%), and 11 (6.3%) patients experienced community weight loss programs including exercising, dieting, and taking different medications twice or more, respectively.
Perioperative
The duration of surgery and length of hospital stay were 60.7 ± 7.4 min and 1.3 ± 1.4 days, respectively with no significant difference when separated the groups based on their baseline obesity-associated medical problems. Only two patients had intraoperative complications including small bowel perforation and bleeding from spleen injury (one patient for each complication), which were managed accordingly by in-situ repair. In addition, eight patients required ICU care based on the anesthesiologist’s opinion.
Postoperative problems
During the 30-day post-operative period, no death was recorded; however, four patients (2.3%) experienced bleeding. Two patients had intraluminal bleeding that were managed conservatively, while two patients had extraluminal bleeding (from staple line) and required laparoscopy. One patient was admitted due to diabetic ketoacidosis and one patient had leak that were addressed accordingly through laparoscopy. One patient underwent cholecystectomy due to gallstones and cholecystitis.
Weight loss outcomes
The number of eligible patients for each postoperative follow-up visit and the percentage of them with available data, with mean BMI and weight loss are provided in Table 2. Our follow up rate was 78% and 70% in 24 and 60 months after surgery, respectively. The trends of %TWL and %EWL of patients in 5 years in total population are shown in Figs. 1 and 2. The peak of all weight-change variables is at 12- and 18-month after surgery. %TWL reached the peak of 28% at 12 and 18 months after the operation and %EWL reached near 100% at 6-month and was maintained > 100% between 9 and 48 month after surgery. During the study period, three patients had BMI < 18.5 kg/m2 diagnosed at 12, 18, and 36 months after surgery and had BPL of 200, 140, and 110 cm, respectively. Only the last one required partial reversal (gastrogastrostomy) due to excessive weight loss (BMI = 18.2 kg/m2, %EWL = 218.1, and %TWL = 40.8), resistance to nutritional therapy, and personal preference (fear of more weight loss). The mean BMI between diabetic vs. non-diabetic patients was not significant in any of the postoperative evaluations except at one- and 12-month (p = 0.02 and 0.04, respectively). The BPL was categorized to 100–150 cm (n = 133) and 150–200 cm (n = 30) and no significant difference in %EWL and %TWL was found except at 18-month for both variables and at 36-month for %TWL (Table 3).
Nutritional outcomes
Reports of blood sample results are in Table 4. The mean Alb in patients did not decrease significantly after the operation. However, one patient in 12-month and one patient in 24-month with respective BPL of 130 and 180 cm had Alb < 3.5 g/dL, which were evaluated for liver failure with additional blood tests (INR and bilirubin levels, which were normal) and managed with supplemental protein and total parental nutrition. No further drop was recorded. Among women, 88.7% had hemoglobin more than 12 g/dL before surgery, and the hemoglobin of 27.9%, 24.1%, and 29.4% of them dropped below 12 g/dL at 6, 12, and 24 months after the surgery with no statistical significance. A full work-up panel for anemia was conducted for all and no patients diagnosed having microcytic anemia due to deficiency in iron or megaloblastic anemia due to vitamin B12 or folic acid deficiency. Although we prescribed multi-vitamin and mineral supplement, this decrease in Hb level was remained unknown change after OAGB. The average levels of vitamin B12 and vitamin D3 increased significantly after surgery, which is attributed to the administration of supplements after surgery.
Remission of obesity associated medical problems
Based on the available data in our registry, the mean levels of fasting blood glucose, HbA1c, and lipid profile except HDL reduced up to 2 years after the OAGB (Table 4). The difference in HbA1c level in 2-year and HDL in 6- and 12-month after surgery were not statistically significant with their preoperative values. Regardless of the missed cases in follow-up, a significant improvement was observed at 6 and 12 months after surgery in patients who had pre-existing obesity-associated medical disease (Table 5).
Discussion
The findings of this study as the first large study from a single center indicate that OAGB is an acceptable MBS procedure for patients with class I obesity (BMI < 35 kg/m2) with substantial and sustainable weight loss during 5 years, has a noticeable rate of resolution in associated medical problems such as T2DM, HTN, and HLP, with no increased burden in either postoperative complications or serious change in the blood level of micronutrients, minerals, and vitamins rather than what is expected or know from previous reports. It seems that the outcomes of OAGB in this class are similar to what have been reported for this group with diabetes in the recent systematic review [15] and agreed on in the group with BMI > 35 kg/m2 [8, 9, 11, 14, 17, 21]. Furthermore, although not recommended by the current guidelines, patients without any obesity associated medical problems who failed to lose weight nonsurgically before operation may benefit from OAGB to return to the normal BMI range.
Previous comparisons between OAGB vs. SG or RYGB on BMI ≥ 35 kg/m2 revealed that this procedure brings a significant and long-lasting weight loss, has high rates of remission in obesity associated medical problems, and has an acceptable and predictable profile of postoperative complications similar to RYGB with no increased burden of malnutrition or serious problems [11]. In the next step, as the MBS recommendation moved from class II obesity to class I, more data from different area of the world is needed [1, 4, 15, 22]. As recommended by the latest IFSO and ASMBS guidelines, surgical weight loss is highly recommended in patients with BMI < 35 kg/m2 after a full discussion of all the pros and cons especially when non-surgical managements have failed or one of the obesity-associated medical problems mostly T2DM has occurred [1,2,3]. As reported in these guidelines, there is accumulated evidence regarding the usage of other more well-known MBS procedures rather than OAGB due to being one of the new MBS procedures and lack of sufficient evidence on its long-term safety and efficacy [1]. However, OAGB has been gaining more attention and IFSO and ASMBS have reported their own statement for this type of MBS [8, 9].
Lastly, the systematic review of 9 studies with 376 OAGB candidates with BMI ≤ 35 kg/m2 (ranging from 18 to 35 kg/m2) and T2DM and postoperative follow-up period ranging from 6–84 months revealed that at 12 months, BMI decreased to 23.8 kg/m2, ranging 21.2–25.4 kg/m2 from different studies [15]. However, (1) all of these researches were conducted on the diabetic population and no study evaluated the safety and efficacy of OAGB for class I obesity without associated medical problems who fail to lose weight non-surgically as we did, (2) they were different in their sample size; only two studies had more than 100 patients, (3) most of them are from East Asia where their ethnicity affects the classification of normal BMI range and obesity, (4) definition of T2DM varied between studies, (5) preoperative BMI level had a wide range; patients with BMI < 25 kg/m2 were included in some studies, (6) OAGB’s surgical technique was different and unclear in some reports; BPL was between 100–200 cm, and (7) duration of follow-up was not enough in most studies; only four of them reported to have ≥ 3 years of postoperative visit. In our total population, the mean BMI reached 23.9 kg/m2 at the 12-month follow-up, which is similar to the systematic review and in line with some prior investigations [21,22,23,24,25,26]. The difference with other experiments could be related to the preoperative BMI, gastric pouch volume, and BPL length [27,28,29,30]. The lowest BMI was observed at 12 and 18 months, which also reported by Kular et al. [25]. The association between pre-operative BMI level, BPL length, and weight loss after surgery is a complicated dilemma [16, 17], especially for class I obesity in which there is a fear of excessive weight loss and reaching to BMI < 18.5 kg/m2 [15]. There are reports of insidious malnutrition refractory to medical treatments and acute liver failure in cases with BMI > 35 kg/m2 and BPL of 200 cm and standard gastric pouch, which necessitated reversing the procedure [31]; however, the most routine and safe BPL is around 150 cm in class II obesity [16] but no consensus has been reached for class I obesity [4, 15]. The mean BPL length of the previous studies is around 150 cm (median: 120 cm), which was declared to be safe by the authors too [15]. Except for one study on 11 patients, which used the step-wise increase in BPL from 100 to 150 cm with an increase in BMI [29], two studies with 117 patients performed the OAGB with BPL of 200 cm [23, 24]. An increase in the length of the bypassed intestine from 100 to 200 cm did not help remitting more diabetic patients though increased the number of anemic patients and to compensate for the amount of BPL length, Kim et al. increased the pouch size causing more cases to have marginal ulcer [23, 24]. It has to be mentioned that the %EWL in our study was reached to near 100% at 6 months and maintained > 100% in 9–48 months after surgery. Although three patients had BMI < 18.5 kg/m2, one patient with BPL of 110 cm needed reattaching the remnant stomach and gastric pouch due to %EWL > 200, resistance to nutritional supplements, and her preference. At 12- and 24-month follow-up, only two patients had benign low levels of albumin responsive to medical treatment and unrelated to BPL lengths (i.e., 130 and 180 cm). Three and one patients in Kular et al. study with BPL of 150 cm for all candidates faced low BMI and Alb after surgery, respectively [25]. No other study in this subject reported these events in their patients, which could be underestimated by not following for sufficient amount of time, not including enough sample size, or not testing the blood for this variable. Regardless of the fact that we have not yet reached to a consensus on a safe BPL in OAGB for class I obesity and the patient with BPL = 200 cm reached to the BMI < 18.5 kg/m2 sooner than others, these are indicating that excessive weight loss may not solely relate to BPL and formulas like %EWL as an indicator to track the amount of weight loss after surgery may not work for class I the same it does for class II obesity; we recommend using %TWL instead.
Most patients with obesity associated medical problems experience remission within 6–12 months after surgery. The overall complete and partial remission of T2DM was reported to be 75.5% and 10.3%, respectively from different studies [15]. Based on our available data at 6- and 12-month follow-up, T2DM remission rates were 77.7% and 66.7%, respectively. Similar to our findings, OAGB in patients with T2DM and BMI < 35 kg/m2 improved HTN and all metabolic parameters including lipid profile in previous publications. Except for one patient in Lee et al. study [32], mortality was 0% similar to our population; however, the risk of anemia was 4.7% [15, 23, 26]. Although Hb level was decreased in our patients too and some of them were diagnosed as having anemia based on the reference level of 12 mg/dl, they were successfully managed on conservative management with multi-vitamin plus mineral supplement. Although life-long daily multivitamin consumption is one of our routine postoperative protocols, this decrease in Hb level in some patients had no explanation, which needs more investigation.
OAGB is not without risks and limitations. Although no serious problem was found in our patients during this follow-up, some potential complications of OAGB such as GERD, bile gastritis, anastomotic ulcer, internal hernia, malnutrition, liver failure and mineral-vitamin deficiencies are reported in the literature [4, 11, 15, 21, 23, 24, 26, 32, 33]. Some of these complications may require reoperation, conversion to RYGB, reversing the whole OAGB, or lifelong supplementation. Moreover, OAGB may not be suitable for all BMI < 35 kg/m2 with and without obesity-associated medical disease, as some factors such as life-style, compliance with dietary and exercise recommendations, traits of psychological problems, number and types of previous attempts to lose weight, diabetes duration, insulin use, and glycemic control may affect the outcomes of the surgery. Therefore, OAGB should be carefully considered and individualized for each patient, taking into account the benefits and risks, the patient's preferences and expectations, and the availability and expertise of the surgical team [1, 2, 8, 9, 15, 34, 35].
To state the limitations of this ongoing study which mandate to interpret the results cautiously are related to our sample size, retrospective single center nature, lack of an unanimous length for BPL in this specific BMI group, and lack of data from some patients that have been missed during the follow-up period.
Conclusion
OAGB for BMI < 35 kg/m2 (class I obesity) with or without obesity-associated medical problems has significant and sustainable effects in losing weight with a peak effect at 12 and 18 months, helps to remit T2DM and HTN in a majority of cases, improving lipid profile, and has no increased burden of postoperative problems or deficiency in nutritional factors, minerals, or vitamins rather than what is expected and known from previous investigation except for a risk of excessive weight loss apparently unrelated to BPL length, decrease in Hb and Alb not be reached to a dangerous levels or become symptomatic necessitating to put all patients under surveillance with regular checking of different variables in their blood after surgery at least for 24 months in order not to risk malnutrition or liver failure.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author through email address on reasonable request.
References
Aminian A, Chang J, Brethauer SA, Kim JJ (2018) ASMBS updated position statement on bariatric surgery in class I obesity (BMI 30–35 kg/m2). Surg Obes Relat Dis 14:1071–1087. https://doi.org/10.1016/j.soard.2018.05.025
Busetto L, Dixon J, De Luca M, Shikora S, Pories W, Angrisani L (2014) Bariatric surgery in class i obesity: a position statement from the international federation for the surgery of obesity and metabolic disorders (IFSO). Obes Surg 24:487–519
Vitiello A, Angrisani L, Santonicola A, Iovino P, Pilone V, Forestieri P (2019) Bariatric surgery versus lifestyle intervention in class I obesity: 7–10-year results of a retrospective study. World J Surg 43:758–762. https://doi.org/10.1007/s00268-018-4847-8
Shahmiri SS, Parmar C, Yang W, Lainas P, Pouwels S, DavarpanahJazi AH et al (2023) Bariatric and metabolic surgery in patients with low body mass index: an online survey of 543 bariatric and metabolic surgeons. BMC Surg 23:1–13. https://doi.org/10.1186/s12893-023-02175-4
Sharaiha RZ, Shikora S, White KP, Macedo G, Toouli J, Kow L (2023) Summarizing consensus guidelines on obesity management: a joint, multidisciplinary venture of the International Federation for the Surgery of Obesity & Metabolic Disorders (IFSO) and World Gastroenterology Organisation (WGO). J Clin Gastroenterol 57(10):967–976. https://doi.org/10.1097/MCG.0000000000001916
Salminen P, Kow L, Aminian A, Kaplan LM, Nimeri A, Prager G et al (2024) IFSO consensus on definitions and clinical practice guidelines for obesity management—an international Delphi study. Obes Surg 34:30–42. https://doi.org/10.1007/s11695-023-06913-8
De Luca M, Angrisani L, Himpens J, Busetto L, Scopinaro N, Weiner R et al (2016) Indications for surgery for obesity and weight-related diseases: position statements from the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO). Obes Surg 26:1659–1696. https://doi.org/10.1007/s11695-016-2271-4
Ghiassi S, Nimeri A, Aleassa EM, Grover BT, Eisenberg D, Carter J (2023) American Society for Metabolic and Bariatric Surgery position statement on one-anastomosis gastric bypass. Surg Obes Relat Dis 20(4):319–335. https://doi.org/10.1016/j.soard.2023.11.003
De Luca M, Piatto G, Merola G, Himpens J, Chevallier JM, Carbajo MA et al (2021) IFSO update position statement on One Anastomosis Gastric Bypass (OAGB). Obes Surg 31:3251–3278. https://doi.org/10.1007/s11695-021-05413-x
Brown WA, Shikora SA, Liem R, Holland J, Campbell AB, Sprinkhuizen SM et al (2022) Seventh IFSO global registry report. https://www.ifso.com/pdf/ifso-7th-registry-report-2022.pdf
Li X, Hu X, Fu C, Han L, Xie M, Ouyang S (2023) Efficacy and safety of one anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity: a meta-analysis and systematic review. Obes Surg 33:611–622
Mahawar KK, Himpens J, Shikora SA, Chevallier JM, Lakdawala M, De Luca M et al (2018) The first consensus statement on one anastomosis/mini gastric bypass (OAGB/MGB) using a modified Delphi approach. Obes Surg Obesity Surgery 28:303–312
Parmar CD, Mahawar KK (2018) One anastomosis (mini) gastric bypass is now an established bariatric procedure: a systematic review of 12,807 patients. Obes Surg 28(9):2956–2967. https://doi.org/10.1007/s11695-018-3382-x
Ramos AC, Chevallier J-M, Mahawar K, Brown W, Kow L, White KP et al (2020) IFSO (International Federation for Surgery of Obesity and Metabolic Disorders) consensus conference statement on one-anastomosis gastric bypass (OAGB-MGB): results of a modified Delphi study. Obes Surg 30:1625–1634. https://doi.org/10.1007/s11695-020-04519-y
Parmar CD, Zakeri R, Mahawar K (2020) A systematic review of one anastomosis/mini gastric bypass as a metabolic operation for patients with body mass index ≤ 35 kg/m2. Obes Surg Obesity Surg 30:725–735
Tasdighi E, Barzin M, Mahawar KK, Hosseinpanah F, Ebadinejad A, Taraghikhah N et al (2022) Effect of biliopancreatic limb length on weight loss, postoperative complications, and remission of comorbidities in one anastomosis gastric bypass: a systematic review and meta-analysis. Obes Surg 32:892–903. https://doi.org/10.1007/s11695-021-05848-2
Boyle M, Mahawar K (2020) One anastomosis gastric bypass performed with a 150-cm biliopancreatic limb delivers weight loss outcomes similar to those with a 200-cm biliopancreatic limb at 18–24 months. Obes Surg 30:1258–1264. https://doi.org/10.1007/s11695-019-04359-5
Pizza F, Lucido FS, D’Antonio D, Tolone S, Gambardella C, Dell’Isola C et al (2020) Biliopancreatic limb length in one anastomosis gastric bypass: which is the best? Obes Surg 30:3685–3694
Eisenberg D, Shikora SA, Aarts E, Aminian A, Angrisani L, Cohen RV et al (2023) 2022 American Society of Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) indications for metabolic and bariatric surgery. Obes Surg 33:3–14. https://doi.org/10.1007/s11695-022-06332-1
Kermansaravi M, Shahmiri SS, Khalaj A, Jalali SM, Amini M, Alamdari NM et al (2022) The first web-based Iranian national obesity and metabolic surgery database (INOSD). Obes Surg 32:2083–2086. https://doi.org/10.1007/s11695-022-06014-y
Lee WJ, Wang W, Lee YC, Te HM, Ser KH, Chen JC (2008) Effect of laparoscopic mini-gastric bypass for type 2 diabetes mellitus: comparison of BMI >35 and <35 kg/m2. J Gastrointest Surg 12:945–952
Kermansaravi M, Valizadeh R, Shahsavan M, Adel Maleknia S, Eghbali F, Pazouki A et al (2024) Metabolic and bariatric surgery in patients with class I obesity; a two-year follow-up. BMC Surg 24:1–7
Kim MJ, Hur KY (2014) Short-term outcomes of laparoscopic single anastomosis gastric bypass (LSAGB) for the treatment of type 2 diabetes in lower BMI (<30 kg/m2) patients. Obes Surg 24:1044–1051
Kim Z, Hur KY (2011) Laparoscopic mini-gastric bypass for type 2 diabetes: the preliminary report. World J Surg 35:631–636
Kular KS, Manchanda N, Cheema GK (2016) Seven years of mini-gastric bypass in type II diabetes patients with a body mass index <35 kg/m2. Obes Surg 26:1457–1462
Osman Abouzeid TA, Ain Shoka AA, Abd Elsamee Atia KS (2019) From diabetes remedy to diabetes remission; could single-anastomosis gastric bypass be a safe bridge to reach target in non-obese patients? Asian J Surg 42:307–313. https://doi.org/10.1016/j.asjsur.2018.04.002
Amirbeigi A, Abbaslou F, Talebpour M, Soroush A, Elyasinia F, Zabihi Mahmoudabadi H et al (2022) One anastomosis gastric bypass surgery in Type2 diabetes patients with body mass index < 35 kg/m2: a multi-center retrospective cohort study. Ann Med Surg 79:104102. https://doi.org/10.1016/j.amsu.2022.104102
Navarrete Aulestia S, Leyba JL, Navarrete Llopis S, Pulgar V (2019) One anastomosis gastric bypass/minigastric bypass in patients with BMI < 35 kg/m2 and type 2 diabetes mellitus: preliminary report. Obes Surg 29:3987–3991
García-Caballero M, Valle M, Martínez-Moreno JM, Miralles F, Toval JA, Mata JM et al (2012) Resolution of diabetes mellitus and metabolic syndrome in normal weight 24–29 BMI patients with one anastomosis gastric bypass. Nutr Hosp 27:623–631
Vázquez Pelcastre R, Zenteno Martínez DC, Arana Reyes JC, Méndez Vivas WR, Ríos Ayala EV, Briseño DB (2021) One-anastomosis gastric bypass in patients with BMI < 30 kg/m2 and diabetes mellitus type 2. Nutr Hosp 38:971–977
Keleidari B, Mahmoudieh M, Shahabi S, Sheikhbahaei E, Rezaei M, Sayadi M et al (2020) Reversing one-anastomosis gastric bypass surgery due to severe and refractory hypoalbuminemia. World J Surg 44:1200–1208
Lee WJ, Chong K, Lin YH, Wei JH, Chen SC (2014) Laparoscopic sleeve gastrectomy versus single anastomosis (mini-) gastric bypass for the treatment of type 2 diabetes mellitus: 5-year results of a randomized trial and study of incretin effect. Obes Surg 24:1552–1562
Davarpanah Jazi AH, Shahabi S, Sheikhbahaei E, Tolone S, El SM, Kabir A et al (2023) A systematic review and meta-analysis on GERD after OAGB: rate, treatments, and success. Expert Rev Gastroenterol Hepatol. https://doi.org/10.1080/17474124.2023.2296992
Kermansaravi M, Abbas A, Pishgahroudsari M, Pazouki A (2021) Short-term outcomes of the conversion of one anastomosis gastric bypass to Roux-en-Y gastric bypass in symptomatic reflux patients without revising the size of the gastric pouch. J Minim Access Surg 17:318–321
Kermansaravi M, Parmar C, Chiappetta S, Shahabi S, Abbass A, Abbas SI et al (2022) Patient selection in one anastomosis/mini gastric bypass—an expert modified Delphi consensus. Obes Surg 32:2512–2524
Funding
This experimental study was not funded in any way.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Shahab Shahabi Shahmiri, Shiva Safari, Erfan Sheikhbahaei, Mohammad Fathi, Delaram Moosavi, Seyed Nooredin Daryabari, Abdolreza Pazouki, Chetan D. Parmar, and Mohammad Kermansaravi: have no conflicts of interest or financial ties to disclose.
Ethical approval
N/A (retrospective analysis from a database registry).
Consent for publication
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shahabi Shahmiri, S., Safari, S., Sheikhbahaei, E. et al. Midterm outcomes of one anastomosis gastric bypass for patients with BMI < 35 kg/m2 from a large single center. Surg Endosc 38, 3940–3947 (2024). https://doi.org/10.1007/s00464-024-10928-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-024-10928-2