Abstract
Introduction
The development of achalasia after Roux-en-Y gastric bypass (RYGB) is rare. Heller myotomy (HM) is the gold standard treatment while peroral endoscopic myotomy (POEM) is an emerging technique with promising results. The aim of this narrative review was to summarize the current knowledge on the treatment of esophageal achalasia after RYGB.
Methods
PubMed, EMBASE, and Web of Science databases were consulted. All articles that described the management of achalasia after RYGB were included in this narrative review.
Results
Twelve studies for a total of 28 patients were included. The age of the patient population ranged from 44 to 70 years old and 80% were females. Overall, 61.5% underwent laparoscopic RYGB while 38.5% underwent open RYBG. The elapsed time from the RYGB to myotomy ranged from 14 months to 14 years. Dysphagia (64%) and regurgitation (60.7%) were the most commonly reported symptoms; type I achalasia was diagnosed in 50% of patients. Surgical HM was performed in 17 patients (61%) while POEM was performed in 11 patients (39%). Postoperative morbidity was 3.6% with no differences comparing surgical HM and POEM (6% vs. 0%, p = 0.43). The follow-up time ranged from 1 to 43 months. The overall recurrence rate requiring reoperation was 7% with no differences comparing surgical HM and POEM (12% vs. 0%; p = 0.25).
Conclusion
Both HM and POEM seem feasible, safe, and effective in the management of achalasia after RYGB. The role of POEM in the management algorithm of these patients should be further evaluated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Achalasia is a rare primary esophageal motility disorder characterized by loss of physiological esophageal body peristalsis and lack of relaxation of the lower esophageal sphincter (LES). Dysphagia, regurgitation, chest pain, cough, and weight loss are common symptoms [1]. Heller myotomy (HM) and endoscopic pneumatic dilation (PD) are the gold standard treatments while peroral endoscopic myotomy (POEM) is an emerging technique with promising results.
Morbid obesity is considered a contributing factor in the development of esophageal motility disorders, with a reported prevalence of 20–61% [2, 3]. Transition from nonspecific esophageal motility disorders to achalasia has been documented suggesting a possible pathological continuum [4]. The development of achalasia in patients that previously underwent Roux-en-Y gastric bypass (RYGB) is rare and the prevalence is unknown [5, 6]. The management of such patients is challenging and it is likely that because the increasing number of morbidly in obese patients and concomitant increase in weight-loss procedures (especially RYGB) [7], the number of these patients will grow in the future.
The purpose of this narrative review was to summarize the current knowledge on the treatment of esophageal achalasia after RYGB.
Materials and Methods
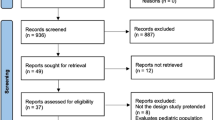
An extensive literature search was conducted by two authors (AA, ST) to identify all English-written published series on esophageal achalasia diagnosed after RYGB. PubMed, EMBASE, and Web of Science databases were consulted matching the terms “achalasia” and “gastric bypass” with “AND” until 30th November 2018. The search was completed by consulting the listed references of each article.
All the articles, case reports, and case series were included in this narrative review. Two authors (AA, ST) independently extracted data from eligible studies. Data extracted included study characteristics (first author name, year, and journal of publication), number of patients included in the series, time frame, clinical and demographic characteristics of patients’ population, type of surgical procedure, and postoperative outcomes. Recurrence was defined as the need for reintervention.
Results
A 51-year-old female complained 10-month history of worsening dysphagia to solids, regurgitation, and weight loss (Eckardt score, 9). She previously underwent laparoscopic RYGB for morbid obesity 9 years before. The patient was diagnosed with type II achalasia. A pneumatic endoscopic dilation was performed with partial symptoms relief and the patient was addressed to laparoscopic Heller myotomy (Fig. 1a–c). The postoperative course was uneventful and at 24-month follow-up, the patient has symptom remission (Eckardt score, 2).
a Dissection of the anterior esophageal wall was performed by freeing the visceral surface from dense abdominal adhesions. b Careful dissection allows precise identification and preservation of the anterior vagus nerve. c The myotomy was performed on the esophagus (6 cm) and extended distally on the gastric pouch (2 cm). An anterior hiatoplasty with interrupted non absorbable suture was performed
Narrative Review
Until 31st December 2018, 11 papers and the present case were included in this narrative review for a total of 28 patients (Table 1). The age of the patient population ranged from 44 to 70 years old and 80% were female. Overall, 61.5% of patients were treated with a laparoscopic RYGB (LRYGB) while 38.5% were operated through an open approach (ORYBG). None of the papers reported patient body mass index (BMI), comorbidities, and ASA score at the bariatric procedure. The elapsed time from the RYGB ranged from 14 months to 14 years. The symptom duration ranged from 1 month to 6 years and the preoperative Eckardt score, reported in 11 patients, ranged from 4 to 9. Dysphagia (64%), regurgitation (60.7%), and chest pain (10.7%) were the most commonly reported symptoms (Table 2). Upper endoscopy, barium swallow study, and esophageal manometry were preoperative evaluations. The manometric pattern was reported in 22 patients: type 1 achalasia was diagnosed in 50% of patients, followed by type 2 (41%), and type III (9%). Overall, 12 patients (43%) underwent a previous non-resolutive treatment. PD was performed in 6 patients (50%), botulin injection followed by PD was performed in 5 patients (42%), and HM was performed in one patient (8%).
Twenty-eight patients underwent definitive treatment. Surgical HM was performed in 17 patients (61%): the surgical approaches were laparoscopy (65%), laparotomy (29%), and robotic (6%). A modified Dor fundoplication using the gastric remnant was fashioned in 2 patients (11.7%). POEM was performed in 11 patients (39%); a selective anterior wall myotomy was performed in 70% of patients while a posterior wall myotomy was performed in 30% of patients. The overall myotomy length ranged from 6 to 12 cm in the surgical HM group and from 10 to 14 cm in the POEM group.
The overall morbidity was 3.6% with no differences comparing surgical HM and POEM (6% vs. 0%; p = 0.43). Iatrogenic full-thickness perforation occurred during LHM and managed with interrupted sutures. There was no mortality. The follow-up time ranged from 1 to 43 months. The recurrence rate was 7% with no differences comparing surgical HM and POEM (12% vs. 0%; p = 0.25). In one patient, recurrence of dysphagia 24 months after surgical HM required reoperation through POEM. The postoperative Eckardt score ranged from 1 to 2 with a significant decrease compared with preoperative data. Pre- and postoperative esophageal manometry and pH testing comparison were reported in one POEM study with a significant decrease in the mean LES resting pressure, integrated relaxation pressure (IRP), and normal pH exposure (DeMeester < 14.72).
Discussion
It has been shown that obesity might be an independent risk factor for the development of esophageal motility disorders, but to date, no clear correlation exists [2,3,4]. There is contradictory evidence on the postoperative impact of bariatric surgery, especially RYGB, on esophageal motility. Some studies showed a minimal effect on physiological esophageal bodily motility and LES pressure [17]. By contrast, some authors hypothesized that the surgical trauma or iatrogenic vagus nerve injury might cause a neuropathic dysfunction with consequent development of new or worsening of previous asymptomatic motility disorders [4, 8]. Schrumpf et al. hypothesized a possible hormonal effect caused by the postprandial gastrin decrease with consequent significant rise in the LES resting pressure [18]. Although the incidence of achalasia in the bariatric population is unknown, transition from nonspecific esophageal motility disorders to achalasia has been documented in the literature and may suggest common pathogenesis [4]. The prevalence of achalasia after RYGB is unknown; however, because the increasing number of morbidly obese patients and weight-loss procedures (especially RYGB), it is likely that the number of these patients will grow in the future.
Achalasia is an uncommon esophageal motility disorder with an annual incidence of 1.5 cases per 100,000 individuals [19]. The disease results from inflammation and consequent degeneration of ganglion cells in the esophageal myenteric plexuses with consequent loss of inhibitory innervation. This results in an increase of the LES basal pressure and aperistalsis of the esophageal body [20]. Usually, males and females are equally affected. Notably, in our study, the majority of patients that developed achalasia after RYGB were females (80%). The development of achalasia after RYGB may be extremely variable in term of timing and symptom presentation. The analysis of the elapsed time from the RYGB to myotomy revealed inconstant data without a specific timing for development. At presentation, dysphagia and regurgitation were commonly reported but atypical symptoms such as chronic cough and aspiration pneumonia may also exist.
Endoscopy and/or barium swallow study is mandatory to exclude any possible dysfunction or strictures of the gastrojejunal anastomosis [21]. Standard or high-resolution esophageal manometry is needed to confirm the diagnosis. Notably, there was no clear correlation between RYGB and achalasic manometric pattern with 50% of the patients having a type I achalasia and 40%, a type II.
Multidisciplinary management involving endoscopists, esophageal surgeons, bariatric surgeons, and anaesthesiologist is mandatory in the management of these patients. HM and endoscopic PD are the standard of care with similar results in the medium and long-term follow-up [22]. Sequential pneumatic dilation has been shown to be effective but, in case of symptom recurrence, surgical myotomy should be considered as definitive treatment [23]. Surgical HM was adopted in 60% of patients with the majority operated via laparoscopy (65%). Because of the presence of intra-abdominal adhesions and anatomical variations, there is a hypothetical increase in mucosal perforation rate and iatrogenic vagus nerve injury. Careful dissection of the distal esophagus, hiatus, and proximal portion of the gastric pouch is mandatory to reduce the risk of such complications [24]. In addition, the use of intraoperative endoscopy to guide dissection, to check for the completeness of the myotomy, and to test for the presence of occult perforations should be considered [25]. Robotic HM has been described in one case with the potential advantage to reduce the risk of mucosal perforation because of the stable working platform and tremor filtering [12]. A modified Dor fundoplication using the gastric remnant was fashioned in two patients. In post-RYGB patients, fundoplication is probably not essential because the exclusion of the acid-production portion of the stomach should theoretically prevent reflux [26].
Different studies have assessed the role of POEM in the treatment of esophageal achalasia with satisfactory short- and medium-term outcomes [27, 28]. Yang et al. first described the use of this technique in post-RYGB achalasic patient [29]. Because the presence of a small gastric pouch, a theoretical high risk of postprocedural regurgitation and gastric perforation has been presumed [16]. In our series, almost 40% of patients underwent POEM with a selective anterior myotomy in the majority of cases. Notably, a trend toward longer overall myotomy length, reduced overall morbidity (6% vs. 0%; p = 0.43), and lower symptoms recurrence rate (12% vs. 0%; p = 0.25) was observed. Even if these results were not statistically significant, with all the limitations related to the small number of patients and study design, a clinical suggestion could be gathered and in selected patients, POEM might be considered as primary treatment in the management algorithm. The possibility to perform a long myotomy, the less invasivity, the operative-naïve field, and the possibility to complete a selective anterior or posterior wall myotomy is unquestionable advantages [16].
Principal limitations of this narrative review are the small number of patients and the possible background selection bias related to the heterogeneity of the included studies and methodological quality. Patients were treated in different centers with diverse expertise and endoscopic/surgical skills. Manometric patterns, pH study data, and Eckardt score evaluation were reported in a limited number of patients and a comprehensive subgroup analysis was not feasible. In addition, the risk of underestimation should be considered because of possible underreporting. On the other hand, because of the rarity of the disease, it is challenging to perform a large prospective study and to date, the comparison between surgical HM and POEM appears feasible only through a review. It is likely that because of the increasing number of morbidly obese patients and concomitant worldwide growth in weight-loss procedures, the number of these patients will increase in the future. Future well-designed studies are warranted to further compare pre- and postoperative manometry patterns, pH study data, quality of life, and Eckardt score in such patients. It is worthwhile that the development of achalasia after RYGB should be deeply investigated in patients with suspicious symptoms and reported in follow-up databases.
Conclusions
The onset of achalasia in obese patients after Roux-en-Y gastric bypass (RYGB) is rare. In tertiary care referral centers, Heller myotomy seems feasible, safe, and effective to relieve gastroesophageal outflow obstruction. The role of POEM in the management algorithm of these patients should be further evaluated. The development of achalasia after RYGB should be reported in follow-up databases. The results of this narrative review should be interpreted with caution and further studies are warranted to endorse the results of this study.
References
Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383(9911):83–93.
Jaffin BW, Knoepflmacher P, Greenstein R. High prevalence of asymptomatic esophageal motility disorders among morbidly obese patients. Obes Surg. 1999;9(4):390–5.
Almogy G, Anthone GJ, Crookes PF. Achalasia in the context of morbid obesity: a rare but important association. Obes Surg. 2003;13(6):896–900.
Shah RN, Izanec JL, Friedel DM, et al. Achalasia presenting after operative and nonoperative trauma. Dig Dis Sci. 2004;49(11–12):1818–21.
Ramos AC, Murakami A, Lanzarini EG, et al. Achalasia and laparoscopic gastric bypass. Surg Obes Relat Dis. 2009;5(1):132–4.
Boules M, Corcelles R, Zelisko A, et al. Achalasia after bariatric surgery. J Laparoendosc Adv Surg Tech A. 2016;26(6):428–32.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25(10):1822–32.
Chapman R, Rotundo A, Carter N, et al. Laparoscopic Heller's myotomy for achalasia after gastric bypass: a case report. Int J Surg Case Rep. 2013;4(4):396–8.
Torghabeh MH, Afaneh C, Saif T, et al. Achalasia 5 years following Roux-en-y gastric bypass. J Minim Access Surg. 2015;11(3):203–4.
Johnson WD, Marshall MB. Surgical management of achalasia in a patient with previous gastric bypass. Innovations (Phila). 2016;11(3):214–6.
Luo RB, Montalvo D, Horgan S. Peroral endoscopic myotomy after gastric bypass: an effective solution for de novo achalasia. Surg Obes Relat Dis. 2017;13(2):e1–3.
Masrur M, Gonzalez-Ciccarelli LF, Giulianotti PC. Robotic Heller myotomy for achalasia after laparoscopic Roux-en-Y gastric bypass: a case report and literature review. Surg Obes Relat Dis. 2016;12(9):1755–7.
Nguyen D, Dip F, Lo Menzo E, et al. Heller oesophagomyotomy as treatment for achalasia after gastric bypass for morbid obesity. Ann R Coll Surg Engl. 2016;98(1):e3–5.
Birriel TJ, Claros L, Chaar ME. Laparoscopic Heller myotomy after previous Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2017;13(11):1927–8.
Abu Ghanimeh M, Qasrawi A, Abughanimeh O, et al. Achalasia after bariatric Roux-en-Y gastric bypass surgery reversal. World J Gastroenterol. 2017;23(37):6902–6.
Sanaei O, Draganov P. Kunda R, et al. Endoscopy: Peroral endoscopic myotomy for the treatment of achalasia patients with Roux-en-Y gastric bypass anatomy; 2018. [Epub ahead of print]
Naik RD, Choksi YA, Vaezi MF, et al. Consequences of bariatric surgery on oesophageal function in health and disease. Nat Rev Gastroenterol Hepatol. 2016 Feb;13(2):111–9.
Schrumpf E, Giercksky KE, Nygaard K, et al. Gastrin secretion before and after gastric bypass surgery for morbid obesity. Scand J Gastroenterol. 1981;16(6):721–5.
Sadowski DC, Ackah F, Jiang B, et al. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol Motil. 2010 Sep;22(9):e256–61.
Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Achalasia Lancet. 2014 Jan 4;383(9911):83–93.
Almby K, Edholm D. Anastomotic strictures after Roux-en-Y gastric bypass: a cohort study from the Scandinavian obesity surgery registry. Obes Surg. 2018;11
Moonen A, Annese V, Belmans A, et al. Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut. 2016;65(5):732–9.
Markar SR, Mackenzie H, Askari A, et al. Population-based cohort study of surgical myotomy and pneumatic dilatation as primary interventions for oesophageal achalasia. Br J Surg. 2018;105(8):1028–35.
Andolfi C, Fisichella PM. Laparoscopic Heller Myotomy and Dor fundoplication for esophageal achalasia: technique and perioperative management. J Laparoendosc Adv Surg Tech A. 2016;26(11):916–20.
Bonavina L. Minimally invasive surgery for esophageal achalasia. World J Gastroenterol. 2006;12(37):5921–5.
El-Hadi M, Birch DW, Gill RS, et al. The effect of bariatric surgery on gastroesophageal reflux disease. Can J Surg. 2014;57(2):139–44.
Swanstrom LL, Kurian A, Dunst CM, et al. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg. 2012;256(4):659–67.
Zaninotto G, Bennett C, Boeckxstaens G, et al. The 2018 ISDE achalasia guidelines. Dis Esophagus. 2018;1:31(9).
Yang D, Draganov PV. Peroral endoscopic myotomy (POEM) for achalasia after Roux-en-Y gastric bypass. Endoscopy. 2014;46 Suppl 1 UCTN:E11–2.
Author information
Authors and Affiliations
Contributions
AA, ST, and ER did the literature search.
AA and DB formed the study design.
Data collection is done by A.A, ST, ER, and D.B.
AA and GB analyzed the data.
AA, GB, and DB interpreted the data.
AA wrote the manuscript.
AA, GM, and DB critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Not applicable.
Research Involving Human Participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aiolfi, A., Tornese, S., Bonitta, G. et al. Management of Esophageal Achalasia after Roux-en-Y Gastric Bypass: Narrative Review of the Literature. OBES SURG 29, 1632–1637 (2019). https://doi.org/10.1007/s11695-019-03774-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03774-y