Abstract
Background
Minimally invasive surgery may introduce new ergonomic challenges for surgeons. Increased patient body mass index (BMI) may further add to this ergonomic stress.
Objectives
The objective of this study was to quantify the ergonomic impact of patient BMI on surgeons during laparoscopic surgery.
Setting
University Hospital, USA.
Methods
This prospective cohort study analyzed five minimally invasive surgeons during 24 laparoscopic procedures. Each subject’s muscle stress was assessed by recording surface electromyography (EMG) data from eight upper body muscle groups during laparoscopic procedures. EMG data was normalized against the maximal voluntary contraction (MVC) of each muscle measured before the start of surgery to create a percentage of the MVC value (%MVC). Subject workload was assessed through the NASA Task Load Index (NTLX). Statistical analysis was used to determine significance between surgeons operating on patients with or without obesity for %MVC and NTLX scores.
Results
There was no significant difference (p > 0.05) in both the average muscle activation of all eight muscle groups and NTLX scores during laparoscopic surgery in surgeons operating on patients with BMI > = 30 compared with patients with a BMI < 30.
Conclusions
We detected no differences in ergonomic stress or workload for surgeons operating on patients with or without obesity. For surgeons, the laparoscopic approach may offer an additional advantage over open surgery in patients with obesity. This advantage may be due to an “equalizing effect” of laparoscopy—that surgical ergonomics are less affected by the BMI of the patient when using laparoscopic tools.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As techniques for laparoscopic procedures have evolved over the past 20 years, minimally invasive surgery has become the mainstay for many surgical procedures. Compared with open surgery, minimally invasive surgery offers significant clinical benefits including lower perioperative morbidity, enhanced postoperative recovery, and improved cosmesis [1]. As a result, laparoscopic surgery has become the standard of care for many common procedures including hernia repairs [2,3,4,5], bariatric surgeries [6], and cholecystectomies [7].
The widespread acceptance of minimally invasive surgery has been accompanied by surgeons experiencing new patterns of discomfort during laparoscopic procedures. The laparoscopic approach has new ergonomic challenges that are not present during open surgery. Previous studies have shown that even experienced laparoscopic surgeons often suffer from significantly increased upper extremity muscle discomfort and physical work. Park et al. reported 87% of surgeons who regularly perform minimally invasive surgery suffer from ergonomic-related occupational injury [1]. Several factors contribute to the surgeon’s musculoskeletal stress, including prolonged static head and trunk posture, a greater amount of shoulder and upper arm movements using laparoscopic instruments, and poor mechanical design of laparoscopic instruments [8]. These factors could prolong surgery duration and increase muscular and mental fatigue that could lead to work-related injuries.
Our group has sought to quantify the effect of various factors on surgical ergonomics. We have previously demonstrated the role of operative approach on ergonomic stress, such as robotic vs. laparoscopic and laparoscopic vs. open approaches [9, 10]. We have also studied the effect of surgical team factors including primary vs. assistant surgeon [11].
The aim of this study is to quantify the impact of patient BMI on surgeon ergonomics during laparoscopic surgery. We hypothesize that operating on patients with obesity will increase the minimally invasive surgeon’s muscular stress in some or all of the upper body muscle groups (including bicep, tricep, deltoid, and trapezius) and lead to greater mental and physical workload.
Materials and Methods
Following approval by the institutional review board, five attending surgeons with expertise in laparoscopic surgery (> 500 laparoscopic procedures performed) were recruited from the Department of Surgery and informed consent was obtained. Data was collected from a total of 24 laparoscopic surgeries across three broad categories—benign foregut, abdominal wall, and general abdominal/solid organ (Table 1). Procedures were grouped into these categories based on similar patterns of trocar placement (e.g., upper abdominal and flank) and complexity. Patient BMI was recorded from the anesthesia pre-surgery evaluation. Obesity was defined as a BMI ≥ 30.
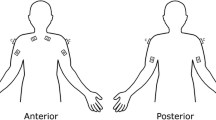
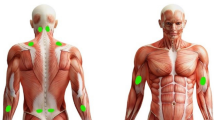
A Trigno Wireless Electromyography (EMG) system was used to quantify the activation of each upper body muscle group. Prior to the beginning of each surgery, surface electrodes were attached to the subject’s left and right biceps, triceps, deltoid, and trapezius muscle groups. These muscle groups were selected to provide continuity and reference points with other surgical ergonomics studies, in which their activation was studied [1, 12]. Static maximum voluntary contraction (MVC) of each muscle group was recorded when the subject was in a sitting position, which was used as a reference value for calculation of relative muscle activation for each group. EMG signals were collected simultaneously from all eight channels at 2000 Hz during the course of surgery from the attending surgeon. Data collection was terminated when the subject finished the laparoscopic procedure. The average muscle activation for each muscle group was calculated using Delsys EMG software and then normalized as a percentage of the MVC value (%MVC). This method of obtaining MVC values has been used in previous studies of surgical ergonomics [11,12,13,14].
The surgeon’s physical and mental workload was assessed following each case using the National Aeronautics and Space Administration Task Load Index (NTLX) survey, a tool that allows subjects to self-assess their performances on six subscales including mental demand, physical demand, temporal demand, performance, effort, and frustration.
Two-sided unpaired Student’s t test were performed to compare the normally distributed mean NTLX scores. Two-sided unpaired Mann–Whitney U test was performed to compare the non-normally distributed mean muscle activation data. A power analysis using the Gpower computer program indicated that a total sample of 8 eight would be needed to detect large effects (d = 5) in the mean muscle activation data with 80% power and alpha at 0.05. Standard error bars were used in the figures for both the mean muscle activation and NTLX scores. A p value of < 0.05 was considered the threshold for statistical significance.
Results
Roughly equal group sizes were chosen for the study—13 patients with obesity and 11 patients without obesity. Similarly, categories and complexities of surgical procedures were comparable across groups (Table 1). There was no statistically significant difference in %MVC calculated for any muscle group between patients with vs. without obesity during laparoscopic procedures: left bicep (4.7 ± 1.4 vs. 2.9 ± 0.8, p = 0.08), left tricep (3.2 ± 1.0 vs. 3.5 ± 1.0, p = 0.73), left deltoid (4.8 ± 1.5 vs. 3.7 ± 1.0, p = 0.33), left trapezius (11.1 ± 3.4 vs. 9.8 ± 2.7, p = 0.73), right bicep (4.0 ± 0.9 vs. 4.4 ± 1.2, p = 0.60), right tricep (2.9 ± 0.9 vs. 4.3 ± 1.2, p = 0.42), right deltoid (5.2 ± 1.6 vs. 5.4 ± 1.5, p = 0.41), right trapezius (10.1 ± 3.0 vs. 12.6 ± 3.5, p = 0.13) (Fig. 1). Similarly, there was no statistically significant difference in subjective workload in any of the six scales of the NTLX between laparoscopic procedures on patients with vs. without obesity: mental demand (46.1 ± 8.3 vs. 48.2 ± 6.2, p = 0.84), physical demand (48.0 ± 7.9 vs. 52.2 ± 5.6, p = 0.15), hurried or rushed (27.5 ± 5.8 vs. 37.7± 3.5, p = 0.37), degree of failure (15.3 ± 4.0 vs. 20.8 ± 4.6, p = 0.37), effort required (51.2 ± 8.9 vs. 52.3 ± 6.2, p = 0.88), and insecure or discouraged (26.6 ± 6.9 vs. 25.9 ± 5.2, p = 0.26) (Fig. 2).
Discussion
As laparoscopic procedures become more prevalent, it has become of increasing importance to address the ergonomically associated pain and discomfort that affects surgeons utilizing laparoscopic techniques. Surgical ergonomics has been pioneered by a series of methodologic and dry-laboratory studies [12, 14, 15] and subsequently used to analyze multiple aspects of surgery, including personnel, operative approach, and training methods [10, 11, 16]. This work is broadly applicable as it utilized routine operative cases and a normal patient population to identify differences related to the BMI of patients as the USA continues to see increasing rates of obesity. This study adds to the growing surgical ergonomics literature by examining one patient characteristic as a contributor to surgical stress.
In addition to patient BMI, there are other factors to consider related to the patient, operative approach, and surgical team, that may contribute to differences in ergonomic stress. For example, patient body mass index (BMI) has subjectively been described as adding to the difficulty of a procedure. Patients with obesity are encountered with increasing frequency in clinical practice with a concomitant increase in the number of surgical procedures on patients with obesity [17]. Multiple studies have shown a marked clinical benefit of the laparoscopic approach compared to the open approach for patients with obesity [18,19,20]. However, there has been little consideration on the effects of laparoscopic procedures for patients with obesity on surgeons. Potentially, minimally invasive surgeons must exert greater torque and alter their positioning when operating on patients with obesity. To date, there has been no published ergonomic literature that describes the association between operating on patients with obesity and the laparoscopic surgeon’s muscle stress.
Interestingly, contrary to our hypothesis, our study does not reveal any significant difference in ergonomic stress or physical and mental workload for surgeons operating on patients with vs. without obesity. There are several possible explanations for this finding. Laparoscopic surgery may reduce the potential difficulties of operating on patients with obesity through less of a need for gross manipulation of tissue. The fulcrum effect in laparoscopy created by the relatively fixed pivot location of the trocar insertion sites may be less affected by obesity than retraction of incisions in patients with obesity. Furthermore, the posture and distance of the surgeon from the operating table may be similar for patients with vs. without obesity in laparoscopy more than it would be for a similar comparison in an open procedure. In effect, laparoscopic surgery could have an “equalizing effect” on surgical procedures in patients with obesity—the surgical ergonomics of laparoscopy are less impacted by the BMI of the patient than they might be in a comparable open procedure. This difference could indicate a further benefit of laparoscopic surgery compared to open surgery in patients with obesity, not just to patients but to surgeons as well. To further explore this aspect, we plan future studies examining the ergonomic stress of surgeons when performing equivalent procedures utilizing the open vs. laparoscopic approach in patients with obesity.
A potential limitation of our study was that surgeon ergonomics was measured clinically for a variety of types of laparoscopic procedures. These procedures involved varying surgical maneuvers and have different durations. Furthermore, other potential patient characteristics (e.g., degree of adhesions and revisional surgery) were not corrected for. In addition, our study focused on collecting data from the primary operating surgeons and did not study the surgical assistant. The role of the attending surgeon versus the surgical assistant could act as a potential confounding factor. Potential future study would be to compare ergonomic stress in both surgeons and surgical assistant during open and laparoscopic procedures in patients with obesity.
Conclusions
This study adds to the growing literature on surgical ergonomics in different operative settings, types of technology, and now, for different types of patients. Our study indicated no difference in ergonomic stress or mental and physical workload for surgeons performing laparoscopic procedures on patients with vs. without obesity. A potential equalizing effect is seen in laparoscopy where the BMI of the patient does not impact surgical ergonomics. We believe this is an advantage of laparoscopic surgery compared to open surgery.
References
Park A, Lee G, Seagull FJ, et al. Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg. 2010;210:306–13.
Lee J, Mabardy A, Kermani R, et al. Laparoscopic vs open ventral hernia repair in the era of obesity. JAMA Surg. 2013;148:723–6.
Lomanto D, Iyer SG, Shabbir A, et al. Laparoscopic versus open ventral hernia mesh repair: a prospective study. Surg Endosc. 2006;20:1030–5.
Schauer PR, Ikramuddin S, McLaughlin RH, et al. Comparison of laparoscopic versus open repair of paraesophageal hernia. Am J Surg. 1998;176:659–65.
Tanphiphat C, Tanprayoon T, Sangsubhan C, et al. Laparoscopic vs open inguinal hernia repair. A randomized, controlled trial. Surg Endosc. 1998;12:846–51.
Schauer PR, Ikramuddin S. Laparoscopic surgery for morbid obesity. Surg Clin North Am. 2001;81:1145–79.
NIH Consensus conference. Gallstones and laparoscopic cholecystectomy. JAMA. 1993;269:1018–24.
Berguer R, Chen J, Smith WD. A comparison of the physical effort required for laparoscopic and open surgical techniques. Arch Surg. 2003;138:967–70.
Zihni AM, Ohu I, Cavallo JA, et al. Ergonomic analysis of robot-assisted and traditional laparoscopic procedures. Surg Endosc. 2014;28:3379–84.
Wang R, Liang Z, Zihni AM, et al. Which causes more ergonomic stress: laparoscopic or open surgery? Surg Endosc. 2017;8:3286–90.
Zihni AM, Cavallo JA, Ray S, et al. Ergonomic analysis of primary and assistant surgical roles. J Surg Res. 2016;203:301–5.
Lee GI, Lee MR, Clanton T, et al. Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc. 2014;28:456–65.
Zihni AM, Ohu I, Cavallo JA, et al. FLS tasks can be used as an ergonomic discriminator between laparoscopic and robotic surgery. Surg Endosc. 2014;28:2459–65.
Lee G, Lee T, Dexter D, et al. Methodological infrastructure in surgical ergonomics: a review of tasks, models, and measurement systems. Surg Innov. 2007;14:153–67.
Lee G, Lee T, Dexter D, et al. Ergonomic risk associated with assisting in minimally invasive surgery. Surg Endosc. 2009;23:182–8.
Zihni A, Ge T, Ray S, et al. Transfer and priming of surgical skills across minimally invasive surgical platforms. J Surg Res. 2016;206:48–52.
Sundbom M. Laparoscopic revolution in bariatric surgery. World J Gastroenterol. 2014;20:15135–43.
Pasam RT, Esemuede IO, Lee-Kong SA, et al. The minimally invasive approach is associated with reduced surgical site infections in obese patients undergoing proctectomy. Tech Coloproctol. 2015;19:733–43.
Hardiman K, Chang ET, Diggs BS, et al. Laparoscopic colectomy reduces morbidity and mortality in obese patients. Surg Endosc. 2013;27:2907–10.
Scheib SA, Tanner E, Green IC, et al. Laparoscopy in the morbidly obese: physiologic considerations and surgical techniques to optimize success. J Minim Invasive Gynecol. 2014;21:182–95.
Acknowledgements
This work was supported by the Society of Gastrointestinal and Endoscopic Surgeons (SAGES) [2012] and Intuitive, Surgical Inc. [2013].
Funding
This work was supported by the Society of Gastrointestinal and Endoscopic Surgeons (SAGES) [2012] and Intuitive, Surgical Inc. [2013].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liang, Z., Gerull, W.D., Wang, R. et al. Effect of Patient Body Mass Index on Laparoscopic Surgical Ergonomics. OBES SURG 29, 1709–1713 (2019). https://doi.org/10.1007/s11695-019-03748-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03748-0