Abstract
Introduction
Many laparoscopic surgeons report musculoskeletal symptoms that are thought to be related to the ergonomic stress of performing laparoscopy. Robotic surgical systems may address many of these limitations. To date, however, there have been no studies exploring the quantitative ergonomics of robotic surgery. In this study, we sought to compare the activation of bilateral biceps, triceps, deltoid, and trapezius muscle groups during traditional laparoscopic surgery (TLS) and robot-assisted laparoscopic surgery (RALS) procedures, as quantified by surface electromyography (sEMG).
Methods
One surgeon with expertise in TLS and RALS performed 18 operative procedures (13 TLS, 5 RALS) while sEMG measurements were obtained from bilateral biceps, triceps, deltoid, and trapezius muscles. sEMG measurements were normalized to the maximum voluntary contraction of each muscle (%MVC). We compared mean %MVC values for each muscle group during TLS and RALS with unpaired t-tests and considered differences with a p value <0.05 to be statistically significant.
Results
Muscle activation was higher during TLS compared to RALS in bilateral biceps (L Biceps RALS:1.01 %MVC, L Biceps TLS:3.14, p = 0.01; R Biceps RALS:1.81 %MVC, R Biceps TLS:4.53, p = 0.0002). Muscle activation was higher during TLS compared to RALS in bilateral triceps (L Triceps RALS:1.73 %MVC, L Triceps TLS:3.58, p = 0.04; R Triceps RALS:1.59 %MVC, R Triceps TLS:5.11, p = 0.02). Muscle activation was higher during TLS compared to RALS in bilateral deltoids (L Deltoid RALS:1.50 %MVC, L Deltoid TLS:3.68, p = 0.03; R Deltoid RALS:1.19 %MVC, R Deltoid TLS:2.57, p = 0.01). Significant differences were not detected in the bilateral trapezius muscles (L Trapezius RALS:1.50 %MVC, L Trapezius TLS:3.68, p = 0.03; R Trapezius RALS:1.19 %MVC, R Trapezius TLS:2.57, p = 0.01).
Discussion
We have quantitatively examined the ergonomics of TLS and RALS and shown that in a single surgeon, TLS procedures are associated with significantly elevated biceps, triceps, and deltoid activation bilaterally when compared to RALS procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The widespread adoption of laparoscopic surgery has been very beneficial for patients with improvements reported in length of hospitalization [1], post-operative pain [2], and post-operative complication rates [3]. For operating surgeons, however, these procedures have been associated with a variety of musculoskeletal symptoms that are thought to be due to the ergonomic stress of performing laparoscopy [4]. A recent study revealed that 73 % of laparoscopic surgeons reported neck, back, shoulder, or hand pain during or after laparoscopy [4]. Another recent report of subjective symptoms showed that 87 % of laparoscopic surgeons regularly experienced musculoskeletal pain or discomfort, and that these symptoms correlated most closely with laparoscopic case volume [5]. The laparoscopic OR environment has many ergonomic challenges that surgeons must contend with, including suboptimal operating table and monitor positioning, non-ergonomic instrument handles, and maintenance of awkward body positioning for extended periods of time [6–9]. Robotic surgical systems seek to address many of these limitations [10–12]. While using a robotic surgical platform, the operating surgeon is in a seated position, viewing the procedure through a viewfinder on the console and manipulating instruments using lightweight masters. These features may provide ergonomic benefits to operating surgeons, and indeed several reports describe subjective improvements in ergonomic stress associated with robotic surgery [13–15]. To date, however, the potential ergonomic benefit of robotic surgery in the operating room has never been objectively analyzed.
Our group is performing a line of research to quantitatively describe the ergonomics of surgical platforms using surface electromyography (sEMG). This technology provides a non-invasive method to capture voltages from working muscles and has been widely used in a variety of industrial fields to help quantify workload [16]. Application of sEMG to study surgical ergonomics has been described in a few recent reports [17]. Lee et al. [18] used sEMG to evaluate ergonomic differences between task performance in a dry lab model using traditional laparoscopic instruments and endoscopic instruments, showing considerable ergonomic challenges associated with endoscopic task performance compared to laparoscopy. Berguer et al. [19] compared laparoscopic task performance to task performance using an early-generation robotic surgical system (ZEUS, Computer Motion, Inc., Goleta, CA) in a dry lab experimental model, identifying significantly lower dominant-arm thenar activation, but no significant differences in deltoid or forearm flexor activation during robotic task performance. Our group recently reported preliminary results from an analysis of fundamentals of laparoscopic surgery (FLS) tasks as an experimental model for comparing traditional laparoscopic surgery (TLS) and robot assisted laparoscopic surgery (RALS) using the da Vinci Surgical System® (dVSS) (Intuitive Surgical, Incorporated; Sunnyvale, CA) [20]. We showed that FLS tasks can be used to identify statistically significant differences in muscle activation as quantified by sEMG, setting the stage for further studies of ergonomics using these tasks. In this study, we sought to compare the activation of bilateral biceps, triceps, deltoid, and trapezius muscle groups during TLS and RALS procedures performed by a single surgeon, as quantified by sEMG data. We hypothesize that muscle activation in all muscle groups tested will be significantly higher during TLS when compared to RALS.
Methods
Subject recruitment
Under an IRB-approved protocol, one general surgeon with fellowship training in minimally invasive surgery and expertise in both TLS (1,250+ cases) and RALS (250+ cases) was recruited to participate in this study.
Operative procedures
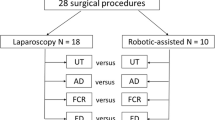
Data were collected during eighteen operative procedures performed at Barnes-Jewish Hospital. Thirteen TLS and five RALS procedures were used. The choice of platform used in this series reflected the practice of the participating surgeon who uses RALS primarily for complex foregut procedures and TLS for abdominal wall hernia and solid organ procedures. All RALS procedures were performed using a da Vinci Si® surgical system (Intuitive Surgical, Incorporated; Sunnyvale, CA),. All procedures were scheduled and identified for use in this study after being added to the operating room schedule as TLS or RALS procedures. There were no procedures that were converted from RALS to TLS, from TLS to RALS, or from either TLS or RALS to open surgery during the course of this study. All procedures were performed with the assistance of a surgical resident or fellow. Data on intra-operative task performance were collected as well. During TLS, only portions of each case in which the surgeon was operating primarily or assisting during laparoscopic surgical task performance were analyzed. Abdominal access and closure were excluded from analysis. During RALS, only portions of each case in which the surgeon was operating using the surgeon’s console were included in the analysis. Abdominal access, closure, and portions of the case in which the surgeon assisted at the bedside were not included in the analysis.
Surface EMG
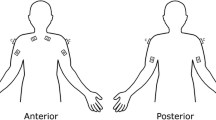
sEMG data were collected with an 8-channel Bioradio® 150 data acquisition system (Great Lakes Neurotechnologies, Incorporated®; Cleveland, OH). Skin surfaces overlying target muscle groups were wiped with rubbing alcohol and allowed to dry, then two 1″ × 1″ MVAP-II® electrodes (MVAP Medical Supplies, Incorporated®; Newbury Park, CA) were placed over the bellies of each muscle group and attached to the positive and negative input poles for each data acquisition channel. Bilateral biceps, triceps, deltoid, and trapezius muscles were tested. The bicep and tricep muscles are very active muscles of arm flexion and extension, two of the most common actions during laparoscopic and robotic surgery, and were therefore selected as indicators of overall muscle activation during task performance. In addition, these muscle groups were selected to provide continuity and reference points with other surgical ergonomics studies, in which their activation was studied [21]. Trapezius and deltoid muscles were also selected because the shoulder and neck are among the most common sites of musculoskeletal symptoms reported by laparoscopic surgeons [22]. An electrode attached to the right elbow served as the ground input to complete the input circuit.
The Biocapture® software package (Great Lakes Neurotechnologies, Incorporated®; Cleveland, OH) was used to filter and record sEMG data. A sampling frequency of 256 Hz was used to capture sEMG data from each channel. Low (<10 Hz) and high frequency (>127 Hz) signals were excluded at the time of data capture using digital signal processing filters.
Before and after each surgical case, EMG data were collected individually from each muscle group while the maximal voluntary contraction (MVC) of that muscle was elicited by an assistant providing resistance. The same assistant was used in every case. The MVC of the biceps was obtained by flexion of each arm against resistance, MVC of the triceps was obtained by extension of the arm against resistance, deltoid MVC data were obtained by abduction of a flexed arm against resistance, and MVC data from trapezius muscles were collected through a shoulder shrug against resistance.
The subject then performed each surgical procedure while continuous sEMG data were collected from each muscle group.
%MVC
The primary outcome variable in this study was the %MVC, calculated by a standard method [17], as defined in the following formula:
Where %MVC is the percentage of maximal voluntary contraction; iEMG is the rectified, processed, and integrated sEMG data for a particular muscle group during a segment of operative task performance; and MVC is the voltage generated by that muscle group during a maximal contraction. In this study, the mean of two MVC repetitions (pre- and post-operative) was used. The %MVC value represents the percentage of maximal muscle effort that is generated by task performance. We analyzed raw sEMG data with the MATLAB® numerical computing environment (MathWorks, Incorporated®; Natick, MA).
Data analysis
Continuous sEMG data were collected from each operative case and divided into 1-minute data segments using MATLAB®. For each data segment, %MVC was calculated for each muscle group tested. This set of %MVC values was used to calculate a mean %MVC value for each muscle group tested during each operative case analyzed. An overall mean %MVC for all TLS cases and a mean %MVC for all RALS cases were calculated for each muscle group. These values were compared using two-sided unpaired student’s t-tests. A p value of <0.05 was considered the threshold of statistical significance for differences seen in this study.
Results
Thirteen TLS and five RALS procedures were used in this study (Table 1). Muscle activation was significantly higher during TLS compared to RALS (Fig. 1) in bilateral biceps (L Biceps RALS: 1.01 ± 0.16 %MVC, L Biceps TLS: 3.14 ± 0.47, p = 0.01; R Biceps RALS: 1.81 ± 0.22 %MVC, R Biceps TLS: 4.53 ± 0.34, p = 0.0002). Muscle activation was significantly higher during TLS compared to RALS in bilateral triceps (L Triceps RALS: 1.73 ± 0.52 %MVC, L Triceps TLS: 3.58 ± 0.47, p = 0.04; R Triceps RALS: 1.59 ± 0.49 %MVC, R Triceps TLS: 5.11 ± 0.83, p = 0.02). Muscle activation was significantly higher during TLS compared to RALS in bilateral deltoids (L Deltoid RALS: 1.50 ± 0.53 %MVC, L Deltoid TLS: 3.68 ± 0.52, p = 0.03; R Deltoid RALS: 1.19 ± 0.49 %MVC, R Deltoid TLS: 2.57 ± 0.28, p = 0.01). Statistically significant differences were not detected in the bilateral trapezius muscle groups (L Trapezius RALS: 1.50 ± 0.53 %MVC, L Trapezius TLS: 3.68 ± 0.52, p = 0.03; R Trapezius RALS: 1.19 ± 0.49 %MVC, R Trapezius TLS: 2.57 ± 0.28, p = 0.01).
The trapezius muscle groups were the only muscles in which similar levels of muscle activation were seen during laparoscopic and robotic procedures, suggesting a specific activation of trapezius muscles during robotic surgery. We performed pairwise comparisons of the trapezius muscle group and other muscle groups during robotic surgery. On the left, the trapezius muscle group showed a significantly greater level of activation during robotic surgery than the biceps (p < 0.0001). No other significant differences were noted on that side. On the right, the trapezius muscle group showed significantly greater activation than the biceps, triceps, and deltoid muscle groups during robotic surgery (p = 0.002, p = 0.003, p = 0.0006, respectively).
Discussion
Laparoscopic surgeons face significant ergonomic challenges. Robotic assistance may provide ergonomic benefit to this critical workforce. In this study, we performed the first quantitative comparison of ergonomic stress associated with TLS and RALS procedures.
An analysis of a single expert robotic and laparoscopic surgeon shows that TLS is associated with significantly higher levels of muscle activation in all muscle groups tested except for the bilateral trapezius muscles. Several-fold differences in %MVC were noted in affected muscles. Absolute differences in mean muscle activation of 2–3 % MVC per minute lead to cumulative effects of increased muscle work over time, particularly in long operative cases, and differences in cumulative muscle activation have been shown to be associated with increased subjective workload in a dry lab model [21]. Our findings suggest that TLS is more ergonomically challenging than RALS for the upper extremity and shoulder. Bilateral trapezius activation was similar on both platforms, potentially reflecting the ergonomic strain on this muscle group associated with operating using the dVSS in a “head down” posture typically employed by operating surgeons using the console. Indeed, we have shown that trapezius muscle groups are activated at a higher level than other ipsilateral muscles during robotic surgery, particularly on the dominant side.
Evaluating a single surgeon’s ergonomic experience during TLS and RALS procedures eliminates many of the possible confounders in an experimental system as complex as surgical task performance, as the subject acts as their own control. While a single-surgeon experience serves as a useful pilot for the study of quantitative ergonomics in the operating room, it will be interesting to assess whether these results are generalizable to additional surgeons. Follow-up studies will be needed to evaluate larger data sets obtained from many laparoscopic and robotic surgeons. Additionally, while it would be ideal to compare the ergonomics of the same procedures on both TLS and RALS platforms, in practice most surgeons at our institution use one platform or the other based on the type of procedure and case complexity. The cases used in this series reflected the practice of the participating surgeon who uses RALS primarily for complex foregut procedures and TLS for abdominal wall hernia and solid organ procedures. As a result, TLS procedures included in this study tended to be shorter and of a lower complexity, potentially introducing the possibility that they may have also been less ergonomically challenging than the RALS cases analyzed due to selection bias. Interestingly, despite these differences the TLS procedures remained more ergonomically challenging than the RALS cases, suggesting that a study of comparably long and complex laparoscopic foregut procedures on both platforms may have yielded even larger differences than those noted in this series. Future multi-surgeon ergonomic evaluations may focus on specific cases that are commonly performed on both platforms. Finally, examining a single mean %MVC value for each muscle group across an entire case creates a broad overview of the ergonomics of a procedure, but compresses hundreds of data points that may contain interesting findings. Future studies will examine muscle activation over the course of individual cases and will identify differences between specific tasks within individual cases, such as assisting and acting as the primary surgeon.
In conclusion, we have quantitatively examined the ergonomics of TLS and RALS procedures for the first time and shown that TLS procedures are associated with significantly elevated biceps, triceps, and deltoid activation bilaterally when compared to RALS procedures. We anticipate these results will be of value in counseling surgeons dealing with significant ergonomic stress when choosing an operative platform. This information may also help to guide the design of future operative robotic systems to further minimize operative stress.
References
Bhogal RH, Athwal R, Durkin D, Deakin M, Cheruvu CN (2008) Comparison between open and laparoscopic repair of perforated peptic ulcer disease. World J Surg 32:2371–2374
Wilson CH, Sanni A, Rix DA, Soomro NA (2011) Laparoscopic versus open nephrectomy for live kidney donors. Cochrane Database Syst Rev 9(11):CD006124
Li MZ, Lian L, Xiao LB, Wu WH, He YL, Song XM (2012) Laparoscopic versus open adhesiolysis in patients with adhesive small bowel obstruction: a systematic review and meta-analysis. Am J Surg 204:779–786
Sari V, Nieboer TE, Vierhout ME, Stegeman DF, Kluivers KB (2010) The operation room as a hostile environment for surgeons: physical complaints during and after laparoscopy. Minim Invasive Ther Allied Technol 19:105–109
Park A, Lee G, Seagull FJ, Meenaghan N, Dexter D (2010) Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg 210:306–313
Berguer R, Chen J, Smith WD (2003) A comparison of the physical effort required for laparoscopic and open surgical techniques. Arch Surg 138:967–970
Berguer R, Smith WD, Chung YH (2001) Performing laparoscopic surgery is significantly more stressful for the surgeon than open surgery. Surg Endosc 15:1204–1207
Lee G, Lee T, Dexter D, Godinez C, Meenaghan N, Catania R, Park A (2009) Ergonomic risk associated with assisting in minimally invasive surgery. Surg Endosc 23:182–188
Berguer R (1998) Surgical technology and the ergonomics of laparoscopic instruments. Surg Endosc 12:458–462
O’Sullivan OE, O’Reilly BA (2012) Robot-assisted surgery: impact on gynaecological and pelvic floor reconstructive surgery. Int Urogynecol J 23:1163–1173
Kumar P, Kommu SS, Challacombe BJ, Dasgup-Ta P (2010) Laparoendoscopic single-site surgery (LESS) prostatectomy–robotic and conventional approach. Minerva Urol Nefrol 62:425–430
Lunca S, Bouras G, Stanescu AC (2005) Gastrointestinal robot-assisted surgery. A current perspective. Rom J Gastroenterol 14:385–391
Wright AS, Gould JC, Melvin WS (2004) Computer-assisted robotic antireflux surgery. Minerva Gastroenterol Dietol 50:253–260
Frick AC, Falcone T (2009) Robotics in gynecologic surgery. Minerva Ginecol 61:187–199
Xia T, Baird C, Jallo G, Hayes K, Nakajima N, Hata N, Kazanzides P (2008) An integrated system for planning, navigation and robotic assistance for skull base surgery. Int J Med Robot 4:321–330
Anton D, Gerr F, Meyers A, Cook TM, Rosecrance JC, Reynolds J (2007) Effect of aviation snip design and task height on upper extremity muscular activity and wrist posture. J Occup Environ Hyg 4:99–113
Lee G, Lee T, Dexter D, Klein R, Park A (2007) Methodological infrastructure in surgical ergonomics: a review of tasks, models, and measurement systems. Surg Innov 14:153–167
Lee G, Sutton E, Clanton T, Park A (2010) Higher physical workload risks with NOTES versus laparoscopy: a quantitative ergonomic assessment. Surg Endosc 25:1585–1593
Berguer R, Smith W (2006) An ergonomic comparison of robotic and laparoscopic technique: the influence of surgeon experience and task complexity. J Surg Res 134:87–92
Zihni AM, Ohu I, Cavallo JA, Ousley J, Cho S, Awad MM (2014) FLS tasks can be used as an ergonomic discriminator between laparoscopic and robotic surgery. Surg Endosc. (Epub ahead of print)
Lee GI, Lee MR, Clanton T, Sutton E, Park AE, Marohn MR (2014) Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc 28(2):456–465
Park A, Lee G, Seagull FJ, Meenaghan N, Dexter D (2010) Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg 210:306–313
Acknowledgments
The authors thank Gyusung Lee, PhD of the Department of Surgery at Johns Hopkins University (Baltimore, MD) for his valuable advice. This study was supported by research grants from the Society of Gastrointestinal and Endoscopic Surgeons (SAGES) and Intuitive Surgical, Inc (Sunnyvale, CA).
Disclosures
This study was supported by a research grant from the Society of Gastrointestinal and Endoscopic Surgeons (SAGES). This study was supported by a research grant from Intuitive Surgical, Inc. (Sunnyvale, CA). Dr. Zihni received research grant funding for unrelated studies from the National Institutes of Health. Dr. Cavallo has received research grant funding for unrelated studies from the National Institutes of Health, the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), and the American Hernia Society in collaboration with Davol® Incorporated; and has served as a one-time consultant for Guidepoint Global® Incorporated. Dr Cho has received research grant funding from the Society of Gastrointestinal and Endoscopic Surgeons (SAGES) and Intuitive, Surgical Inc. (Sunnyvale, CA). Dr Awad has received research grant funding from the Society of Gastrointestinal and Endoscopic Surgeons (SAGES) and Intuitive, Surgical Inc. (Sunnyvale, CA). Mr. Ohu has no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zihni, A.M., Ohu, I., Cavallo, J.A. et al. Ergonomic analysis of robot-assisted and traditional laparoscopic procedures. Surg Endosc 28, 3379–3384 (2014). https://doi.org/10.1007/s00464-014-3604-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3604-9