Abstract
Background
While laparoscopic colorectal resection may be underused in technically challenging circumstances, the minimally invasive approach may in fact maximally benefit patients at the greatest risk of complications. Obesity and proctectomy pose particular technical challenges during laparoscopic resection and are also associated with the greatest risks of complications, especially surgical site infections (SSIs). We evaluated the role of laparoscopy in minimizing SSI in such patients.
Methods
From the American College of Surgeons-National Surgical Quality Improvement Program database, outcomes for obese [body mass index (BMI) ≥ 30 kg/m2] and non-obese (BMI < 30 kg/m2) patients undergoing colectomy or proctectomy between 2006 and 2011 by the laparoscopic (laparoscopic colectomy, laparoscopic proctectomy) or open (open colectomy, open proctectomy) approaches were compared. A univariate analysis was used to determine the influence of laparoscopic surgery within each group on SSI, and a multivariate analysis evaluated the influence of laparoscopy on SSI for obese patients undergoing proctectomy.
Results
OC patients were more likely than OP, LC, and LP, respectively, to undergo emergency operation and have an American Society of Anesthesiologists (ASA) score of 3–5. Overall SSI rates after OC, OP, LC, and LP were 15.2, 17.6, 8.6, and 10.1 %, respectively (p < 0.001), and for obese patients, the rates were 18.7, 22.3, 10.7, and 13.3 % (p < 0.001). On univariate analysis, open surgery, obesity, proctectomy, younger age, race, steroid use, diabetes, chronic obstructive pulmonary disease, prior wound infection, transfusion history, previous operation within 30 days, coronary artery or vascular disease, ASA class 3–5, tobacco use, resident involvement, male gender, albumin <3.5 g/dL, and emergent operation were associated with a higher risk of SSI. Laparoscopy reduced the risk of SSI by at least 35 % across all BMI classes and procedures, an effect that persisted on multivariate analysis even in obese patients undergoing proctectomy.
Conclusions
In colorectal surgery, an already high-risk outlier for SSI, obesity and proctectomy are associated with the highest risk of SSI. Despite the particular technical challenges of laparoscopy in these circumstances, the minimally invasive approach attenuates the risk of SSI in these high-risk patients and thus should be strongly considered during treatment planning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In colorectal surgery, a minimally invasive approach has been shown to be safe and associated with reduced surgical site infection (SSI), length of hospital stay, urinary tract infections (UTI), and ileus [1, 2]. However, the benefits of laparoscopy in obese patients are not as clear [1]. In the past, obesity was even considered a relative contraindication to laparoscopic surgery [3]. Obese patients carry a higher risk of wound and cardiopulmonary complications and are hence predisposed to adverse outcomes after surgical procedures [1, 4]. Although conversion rates and operative times have consistently been shown to be increased in obese patients when compared to the non-obese, several studies show that there can still be a decrease in SSIs, length of stay, and ileus in the obese undergoing laparoscopy when compared to open colorectal surgery [1, 5, 6].
In colorectal surgery which is traditionally associated with a higher SSI risk than other operations, procedures that specifically include rectal resection are associated with an even greater risk of SSI [7, 8]. Thus, it is conceivable that the minimally invasive approach may be maximally beneficial in reducing SSI in obese patients undergoing proctectomy, patients expected to be at the greatest risk of SSI. The beneficial influence of laparoscopic surgery in reducing morbidity after proctectomy in obese patients has, however, not been specifically examined. The aim of this study is to evaluate whether even in obese patients undergoing proctectomy the laparoscopic approach is associated with a reduced SSI and the effect of this approach on other postoperative outcomes.
Materials and methods
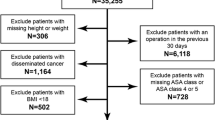
Patients who underwent colon or rectal operations from 2006 to 2011 were identified from the American College of Surgeons-National Surgical Quality Improvement Program (ACS-NSQIP) database after approval by the Institutional Review Board at Columbia University Medical Center. Characteristics of the database have been previously described [6]. Patients were stratified into four groups based on Current Procedural Terminology (CPT) codes: open colectomy, open proctectomy, laparoscopic colectomy, and laparoscopic proctectomy. Calculated body mass index (BMI), with a cutoff of 30 kg/m2, was used to classify patients as non-obese or obese. Patients who had no information about either height or weight were excluded from the analysis. Characteristics and outcomes were evaluated for patients undergoing colectomy or proctectomy by the laparoscopic or open approaches. Data for the subgroup of patients who were obese undergoing surgery were also evaluated and compared. Outcomes evaluated included SSI and other complications including perioperative bleeding, wound dehiscence, pneumonia, and UTI. A multivariable analysis of factors associated with SSI for obese patients undergoing proctectomy was performed to assess the influence of laparoscopy on outcomes for these patients.
Statistical analysis
Descriptive statistics such as frequencies were computed for all categorical variables. Differences in groups were assessed using the Chi-squared or Fisher’s exact tests. A univariate analysis of the influence of a minimally invasive approach on SSI for obese patients undergoing colectomy and proctectomy was performed. Factors that were significantly associated with the outcome were included in the multivariate analysis. A nominal significance level of 0.05 was used for all hypothesis testing. The software utilized was SAS 9.4.
Results
From the NSQIP database, a total of 170,529 patients were identified; 166,704 patients had complete information related to BMI. Patient characteristics are delineated in Table 1. In all, 103,864 (62.3 %) patients underwent open surgery, while 62,840 (37.7 %) underwent laparoscopic surgery. For patients who underwent colectomy, LC was performed in 41,728 (36.4 %) and OC in 72,957 (63.6 %). In those undergoing proctectomy, 21,112 (40.6 %) patients underwent LP and 30,907 (59.4 %) OP. Colorectal cancer (26.4 %) and diverticular disease (20 %) were the most common diagnoses. When comparing the four groups, OC patients were oldest, while LP patients were the youngest and had the lowest mean BMI. Patients with comorbidities most commonly underwent open surgery. Emergency surgery was highest among OC patients (29.5 %) compared to OP (5.0 %), LC (3.8 %), and LP (1.6 %), as was prior wound infection (4.7 %), transfusion (3.8 %), and prior operation in the last 30 days (3.5 %), while LP patients had the lowest rates. Proctectomy cases more commonly had surgical resident involvement than colectomy cases, and operative time was longest in LP patients followed by OP, LC, and lastly OC patients. Mean length of stay was longer (11.3 vs. 6.3 days, respectively), for patients undergoing open surgery than laparoscopic surgery (p < 0.001).
Surgical site infections
Proctectomy was associated with a higher overall SSI rate than colectomy [14.6 vs. 12.8 %, respectively; odds ratio (OR) 1.16, 95 % confidence interval (CI) 1.13–1.20] (p < 0.001). SSIs (superficial, deep, and organ space) were also more common in obese (16.7 %) than in non-obese (11.8 %) patients (p < 0.001). Overall SSI rates were highest for OP (17.6 %) and lowest for LC (8.6 %), while rates in OC and LP patients were 15.2 and 10.1 %, respectively.
Deep SSI occurred at a higher rate after open surgery and proctectomy (p < 0.001 for both comparisons). OP and OC patients most commonly (when compared to LP and LC) had organ space SSI (p < 0.001). Superficial SSI was also highest in OP patients (10.7 %), followed by OC patients (8.6 %). The open procedures had significantly higher superficial SSI than the laparoscopic procedures (p < 0.001). Table 1 also compares other complications between the groups.
Factors associated with the presence of SSI are listed in Table 2. On univariate analysis, factors associated with an increased risk of SSI were BMI ≥ 30 kg/m2, proctectomy, younger age, race, steroid use, diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), prior wound infection, transfusion history, operation in the last 30 days, previous percutaneous coronary intervention, peripheral vascular disease, American Society of Anesthesiologists (ASA) class tobacco use, resident involvement, and emergent operation (Table 2). Laparoscopy, female gender, and albumin ≥3.5 g/dL were conversely associated with a reduced risk.
Obese patients
Table 3 shows the proportion of obese patients undergoing OC, OP, LC, and LP and their characteristics. Overall SSI rates for obese patients were 18.7, 22.3, 10.7, and 13.3 % after OC, OP, LC, and LP, respectively (p < 0.001), highest for OP and lowest for LC. Proctectomy was associated with a higher overall SSI rate (18.9 vs. 15.7 %, respectively) than colectomy (p < 0.001). Deep SSI occurred more commonly after OC (2.9 %) and OP (3.0 %) than LP (1.6 %) and LC (1.0 %) (p < 0.001 for both comparisons). For the obese patients, superficial SSI was highest after OP (14.8 %), followed by OC (10.9 %), and the open procedures had significantly higher superficial SSI than the laparoscopic procedures (p < 0.001). The odds for the development of SSI for obese patients undergoing laparoscopic proctectomy were similar to those after laparoscopic colectomy.
The univariate analysis for factors associated with SSI among obese proctectomy patients is shown in Table 4. The multivariate analysis for the same group of patients is shown in Table 5. Multivariate analysis of factors associated with SSI for obese patients undergoing proctectomy revealed that laparoscopy significantly decreased the odds of SSI when compared to the open approach [OR 0.59 (0.52–0.66); p value <0.0001] when adjusted for age, smoking status, DM, ASA class, prior wound infection, and resident involvement (Table 5).
Other complications
For the obese patients in the NSQIP database who underwent colectomy and proctectomy (both open and laparoscopic), perioperative bleeding, wound dehiscence, pneumonia, and UTI occurred in 8.3, 2.3, 3.3, and 4.0 % of the patients, respectively (Table 3). Bleeding occurred most commonly after OC and less after LC. LP patients likewise had a lower rate of bleeding than OP patients. Wound dehiscence was highest for OC, followed by OP. Laparoscopy decreased this rate, with LC and LP patients experiencing this complication at less than half the rate of their open counterparts (p < 0.001). Obesity was associated with an increased risk of dehiscence, with it occurring in 3.2, 2.7, 0.9, and 1.3 % of OC, OP, LC, and LP patients, respectively (p < 0.001). Pneumonia was less common in LP and LC than in OP and OC (p < 0.001), while UTI was most common in OP patients (5.5 %) and least common in LC patients (2.2 %).
Discussion
Laparoscopy has been very effective in reducing many previously common surgical complications, in particular SSI. SSIs can be problematic and pose great medical, financial, and recovery challenges in the obese [9, 10]. The cost of an SSI is believed to be significant as patients with SSIs frequently have longer hospital stays and require outpatient wound care supplies and home nursing assistance [11, 12]. Laparoscopic surgery may reduce SSI after colorectal surgery, but obesity and pelvic dissection during proctectomy pose particular technical challenges [1]. The potential role of laparoscopy in improving outcomes in obese colorectal surgery patients is important because obesity generally increases technical demand, decreases good exposure, and results in difficulty in maneuvering instruments intra-abdominally [5, 13, 14]. This leads to increased operative time and conversion to open surgery in this patient population [15–17]. Despite this, the procedure has been proven to be safe and can be advantageous in terms of short-term outcomes for obese patients. Our data show that laparoscopy significantly reduces the incidence of complications including SSI after proctectomy, even in obese patients.
Patients undergoing open surgery generally had more preoperative comorbidities than patients undergoing laparoscopy. This is not surprising since, considering the longer operative time with laparoscopy, it is likely that patients with greater medical problems would have been selected for open surgery by surgeons, thus being particularly the case earlier in the learning curve associated with laparoscopic surgery. However, with growing experience with the procedure and recognition of the benefits of the procedure in most patients, the procedure has been increasingly employed even in the most challenging of patients and procedures. Proctectomy increased the risk of SSI for both BMI classes, with an OR of 1.16 overall. Obese patients undergoing OP had by far the highest rate of SSI, but this was reduced by more than 1/3 by laparoscopy. Even though 29.5 % of OC patients underwent emergent operation and 4.7 % had prior wound infection while 5.0 and 2.4 % of OP patients, respectively, did, OP patients still had a higher incidence of SSI than OC patients (p < 0.001). While this may be related to the increased bacterial content in the large bowel when progressing from the cecum to the rectum [8], the technical challenges involved in proctectomy (i.e., pelvic exposure) make for an increased risk of spillage and other complications [6].
Technical and microbial issues with proctectomy are all compounded by obesity. It is postulated that decreased wound oxygen tension, impaired tissue antibiotic penetration, and altered immune function contribute to the increased risk of SSI in these patients [18]. In the entire cohort, LC patients had the lowest overall rate of SSI, at 8.6 %. LP patients had an SSI rate of 10.1 % which was less than the OP rate (17.6 %). Thus, laparoscopy may counteract some of the potential biologic and technical variables that increase the risk of SSI in OP; this reduces the risk of SSI to almost that of patients undergoing colectomy. This holds true even for patients who were obese. In our multivariate analysis, laparoscopy was associated with a reduction in the odds of an SSI for obese patients undergoing proctectomy by 41 % (0.59, 95 % CI 0.52–0.66).
Other complications were increased in the obese and those undergoing open surgery. Wound dehiscence and bleeding were greater after open surgery. Obesity further increased the rate of dehiscence, even in laparoscopy patients. In LC patients, dehiscence increased from 0.7 to 0.9 % when only obese patients were considered. This trend continued for patients who underwent proctectomy when comparing the obese and non-obese. The increased risk in obese patients may be due to the increased abdominal girth, larger incision, and trauma from tissue handling. Such factors are also expected to contribute to the increased bleeding seen in open surgery, which is compounded by obesity. Previous data suggest that hemorrhage is the most common complication in obese patients undergoing colorectal surgery requiring reoperation [19]. Laparoscopy also reduced this rate of bleeding in obese patients by more than half. Pneumonia, UTI, and length of stay were also lower after laparoscopic surgery. Previous studies have similarly shown that laparoscopy reduces the rate of pneumonia in colorectal surgery, even in obese patients [2, 6]. UTI may have been higher because of the increased length of stay of OC and OP patients [20].
Numerous additional factors, besides proctectomy and open surgery, were found to be associated with an increased risk of SSI on univariate analysis. Ricciardi et al. [21] found that obesity and tobacco use were independent risk factors for SSI in colorectal surgery, findings that were similar to ours. Patients who have more comorbidities preoperatively are prone to surgical complications and extended hospital stays, both of which can independently increase the risk of nosocomial infections. DM and steroid use are also well known to be associated with SSI, especially in patients undergoing proctectomy [22, 23]. Other notable risk factors were resident involvement, emergent operation, gender, and COPD. Kiran et al. [24] found that resident involvement increased superficial SSI rates, but 30-day mortality was unchanged. Resident involvement likely indicates surgical complexity, but the presence of the trainee may contribute to minor complications. Emergency procedures are also shown to be associated with increased SSI because of the usually unstable nature of the patients and lack of colon preparation, as seen in cases of colon perforation [25]. Male gender has been shown to increase the incidence of wound complications, possibly due to a narrow pelvis and an increased incidence of metabolic syndrome [26]. Finally, COPD was associated with an increased risk of SSI as has been demonstrated previously [27]. This can be explained by its potential association with hypoxia, and tobacco use.
The findings of the current study suggest that the use of laparoscopy for colorectal surgery in general should be primarily advocated over open surgery because of the reductions in length of stay and perioperative complications, particularly SSI. Our results are supported by some randomized control trials (RCTs). Braga et al. [28] conducted an RCT to assess the cost-benefit analysis of laparoscopy in colorectal surgery and concluded that laparoscopy reduced SSI, one of the most expensive postoperative complications. The COLOR II study showed that laparoscopic proctectomy was associated with a significantly shorter hospital stay than open proctectomy [29]. Although the study found that there was no difference between the two groups in terms of wound infection, the other short-term outcomes like length of hospital stay, intraoperative bleeding, and time to return of bowel function were significantly lower in the laparoscopy group compared to open group [29]. Our findings that laparoscopy, despite its technical complexity, reduced complications even for proctectomy are particularly important. In obese patients and those undergoing proctectomy, where the complications are highest after colorectal surgery, these benefits of laparoscopy support its use despite the anticipated difficulties of performing surgery by the minimally invasive approach in these circumstances. The use of the NSQIP database, which has standard definitions for each of the complications included, assured consistency among the huge amount of patient data that were analyzed. Further, in order to increase the applicability of the study, we chose to divide the patients into those who had colectomy and proctectomy given the differences in the outcomes of those two procedures. Another major strength of this study is that the results are generalizable to the obese patients undergoing proctectomy throughout the USA as the NSQIP database has data from the hospitals all over the USA. Despite these strengths of this study, the limitations are the unselected population and inherent bias of retrospective data. Thus, the patients expectedly had more comorbidities and more frequently underwent emergency surgery than laparoscopy patients. Further, such factors as diversion, preoperative radiation, type of incision and bowel preparation, which are known to be associated with SSI, could not be assessed due to the limitation of the NSQIP data. Another limitation of the study is that there is no information regarding the conversion of laparoscopic procedures to open. This makes it unclear whether the patients who had conversion were included in the laparoscopic group or the open group or were not included at all. If the status of the conversion were available, our plan would have been to not include them in the laparoscopy group and consider them separately.
This study quantifies the differential effects of laparoscopy in patients undergoing colectomy and proctectomy and subdivides them by obesity status. Such a detailed analysis of surgical subgroups is also important in this era of increased government scrutiny of health care cost and utilization.
Conclusions
The findings of the study indicate that laparoscopic colectomy and proctectomy have significantly lower SSI rates than their open counterparts. Laparoscopic surgery was associated with a reduced incidence of SSI in obese patients and should be considered the preferred approach in this patient population.
References
Geiger TM, Muldoon R (2011) Complications following colon rectal surgery in the obese patient. Clin Colon Rectal Surg 24:274–282
Hardiman K, Chang ET, Diggs BS, Lu KC (2013) Laparoscopic colectomy reduces morbidity and mortality in obese patients. Surg Endosc 27:2907–2910
Loffer FD, Pent D (1976) Laparoscopy in the obese patient. Am J Obstet Gynecol 125:104–107
Senagore AJ, Delaney CP, Madboulay K, Brady KM, Fazio VW (2003) Laparoscopic colectomy in obese and nonobese patients. J Gastrointest Surg 7:558–561
Park JW, Lim SW, Choi HS, Jeong SY, Oh JH, Lim SB (2010) The impact of obesity on outcomes of laparoscopic surgery for colorectal cancer in Asians. Surg Endosc 24:1679–1685
Greenblatt DY, Rajamanickam V, Pugely AJ, Heise CP, Foley EF, Kennedy GD (2011) Short-term outcomes after laparoscopic-assisted proctectomy for rectal cancer: results from the ACS NSQIP. J Am Coll Surg 212:844–854
Kiran RP, El-Gazzaz GH, Vogel JD, Remzi FH (2010) Laparoscopic approach significantly reduces surgical site infections after colorectal surgery: data from national surgical quality improvement program. J Am Coll Surg 211:232–238
Degrate L, Garancini M, Misani M et al (2011) Right colon, left colon, and rectal surgeries are not similar for surgical site infection development. Analysis of 277 elective and urgent colorectal resections. Int J Colorectal Dis 26:61–69
Smith RL, Bohl JK, McElearney ST et al (2004) Wound infection after elective colorectal resection. Ann Surg 239:599–605 discussion 605–607
Wick EC, Hirose K, Shore AD et al (2011) Surgical site infections and cost in obese patients undergoing colorectal surgery. Arch Surg 146:1068–1072
Mahmoud NN, Turpin RS, Yang G, Saunders WB (2009) Impact of surgical site infections on length of stay and costs in selected colorectal procedures. Surg Infect (Larchmt) 10:539–544
Fukuda H, Morikane K, Kuroki M et al (2012) Impact of surgical site infections after open and laparoscopic colon and rectal surgeries on postoperative resource consumption. Infection 40:649–659
Bège T, Lelong B, Francon D, Turrini O, Guiramand J, Delpero JR (2009) Impact of obesity on short-term results of laparoscopic rectal cancer resection. Surg Endosc 23:1460–1464
Lascano CA, Kaidar-Person O, Szomstein S, Rosenthal R, Wexner SD (2006) Challenges of laparoscopic colectomy in the obese patient: a review. Am J Surg 192:357–365
Pikarsky AJ, Saida Y, Yamaguchi T et al (2002) Is obesity a high-risk factor for laparoscopic colorectal surgery? Surg Endosc 16:855–858
Schlachta CM, Mamazza J, Grégoire R, Burpee SE, Pace KT, Poulin EC (2003) Predicting conversion in laparoscopic colorectal surgery: fellowship training may be an advantage. Surg Endosc 17:1288–1291
Scheidbach H, Benedix F, Hügel O, Kose D, Köckerling F, Lippert H (2008) Laparoscopic approach to colorectal procedures in the obese patient: risk factor or benefit? Obes Surg 18:66–70
Hourigan JS (2011) Impact of obesity on surgical site infection in colon and rectal surgery patients. Clin Colon Rectal Surg 24:283–290
Schwandner O, Farke S, Schiedeck TH, Bruch HP (2004) Laparoscopic colorectal surgery in obese and nonobese patients: do differences in body mass indices lead to different outcomes? Surg Endosc 18:1452–1456
Kang CY, Chaudhry OO, Halabi WJ et al (2012) Risk factors for postoperative urinary tract infection and urinary retention in patients undergoing surgery for colorectal cancer. Am Surg 78:1100–1104
Ricciardi R, Roberts PL, Hall JF et al (2014) What is the effect of stoma construction on surgical site infection after colorectal surgery? J Gastrointest Surg 18:789–795
Konishi T, Watanabe T, Kishimoto J, Nagawa H (2006) Elective colon and rectal surgery differ in risk factors for wound infection: results of prospective surveillance. Ann Surg 244:758
Ata A, Valerian BT, Lee EC, Bestle SL, Elmendorf SL, Stain SC (2010) The effect of diabetes mellitus on surgical site infections after colorectal and noncolorectal general surgical operations. Am Surg 76:697–702
Kiran RP, Ahmed Ali U, Coffey JC, Vogel JD, Pokala N, Fazio VW (2012) Impact of resident participation in surgical operations on postoperative outcomes: National Surgical Quality Improvement Program. Ann Surg 256:469–475
Watanabe M, Suzuki H, Nomura S et al (2014) Risk factors for surgical site infection in emergency colorectal surgery: a retrospective analysis. Surg Infect (Larchmt) 15:256–261
Kurmann A, Vorburger SA, Candinas D, Beldi G (2011) Operation time and body mass index are significant risk factors for surgical site infection in laparoscopic sigmoid resection: a multicenter study. Surg Endosc 25:3531–3534
Haridas M, Malangoni MA (2008) Predictive factors for surgical site infection in general surgery. Surgery 144:496–501 discussion 501–503
Braga M, Vignali A, Zuliani W, Frasson M, Di Serio C, Di Carlo V (2005) Laparoscopic versus open colorectal surgery: cost-benefit analysis in a single-center randomized trial. Ann Surg 242:890–895 discussion 895–896
van der Pas MH, Haglind E, Cuesta MA et al (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All the procedures performed in this study were in accordance with the ethical standards of Institutional Review Board at Columbia University and with 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal informed consent is not required.
Rights and permissions
About this article
Cite this article
Pasam, R.T., Esemuede, I.O., Lee-Kong, S.A. et al. The minimally invasive approach is associated with reduced surgical site infections in obese patients undergoing proctectomy. Tech Coloproctol 19, 733–743 (2015). https://doi.org/10.1007/s10151-015-1356-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-015-1356-8