Abstract
Background
Endoscopic approaches exist for targeting weight regain after Roux-en-Y gastric bypass (RYGB), including endoscopic suturing, clipping, and sclerotherapy. Argon plasma coagulation (APC) is a noncontact electrocoagulation method, and when used in RYGB patients, it has shown reduction in the diameter of the gastrojejunal anastomosis.
Objectives
To study the effectiveness of APC for weight regain in terms of weight loss for RYGB patients, from eight bariatric centers.
Methods
A retrospective chart review was performed for 558 patients at eight bariatric centers in the USA (1) and Brazil (7) who underwent APC procedure between 31st July 2009 and 29th March 2017. APC was performed on patients who regained weight after RYGB procedure.
Results
Upon exploratory analysis of the individual BMI data, the mean BMI decreased slightly during the first 24 months and increased slightly afterwards following the APC intervention. The mean weight was 94.5 ± 18.6 kg and the mean BMI was 34.0 kg/m2 at APC. Where data were available, the mean of lowest weight was 67.0 ± 23.0 kg and the mean of lowest BMI was 24.1 kg/m2 following gastric bypass. The mean weight loss was 6.5, 7.7, and 8.3 kg at 6, 12, and 24 months, respectively, and the changes in weight over time was statistically significant (p < 0.0001). Multi-level for change model showed the low body mass index (BMI) group (BMI < 30 kg/m2) to have greater TWL than the high BMI (BMI ≥ 30 kg/m2) group at 6, 12, and 24 months. In the low BMI group, the mean TWL was 4.7, 6.1, 6.9, and 2.4%, at 6, 12, and 24 months, respectively. In the high BMI group, the mean TWL was 7.5, 10.4, 13.4, and 3.7%, at 6, 12, 24, and 36 months, respectively. Of the 333 patients in four centers who provided complication information, complications after APC included stenosis (n = 9), GJ ulcer (n = 3), vomiting (n = 3), GJ leakage (n = 2), and melena (n = 1).
Conclusion
APC can be useful in reducing the regained weight after RYGB, and patients showed 6–10% total weight loss at 12 months. Randomized trials would be needed to validate the findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Roux-en-Y gastric bypass (RYGB) provides great advantage in sustainable weight loss than sleeve gastrectomy and adjustable gastric banding [1]. Adams et al. [2] reported that their RYGB patients maintained a mean of 27% percentage of total weight loss (TWL) at 12 years. However, several studies suggested that up to 35% of patients regained some weight after RYGB. The definition of weight loss failure or when the weight regain becomes significant is highly variable, and there are no accepted criteria [3]. Nevertheless, super-obese population is more vulnerable to weight regain than patients with body mass index (BMI) less than 50 kg/m2 [4,5,6]. A combination of genetic, anatomic, behavioral, and psychological components is thought to contribute to weight regain in these patients [7, 8]. Among these, anatomic aspect of the component features enlarged gastric pouch, dilated gastrojejunostomy, or both, which in turn results in lack of restriction [5]. Along with several revision options, endoscopic approaches exist for targeting this anatomic factor, including endoscopic suturing, clipping, and sclerotherapy [7, 9].
Argon plasma coagulation (APC) is a noncontact electrocoagulation method, and radiofrequency energy in forms of ionized gas is applied to the tissue. This results in superficial thermal coagulation and the procedure is very effective for hemostasis [10]. Due to this characteristic, it is used widely from treating endobronchial tuberculosis to gastrointestinal bleeding [10,11,12]. When used in RYGB patients, it has shown reduction in the diameter of the gastrojejunal anastomosis short term [13].
In this study, we aim to study the effectiveness of APC for weight regain in terms of weight loss for RYGB patients, from eight bariatric centers.
Methods and Materials
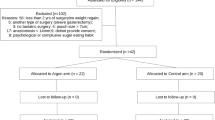
After institutional review board (IRB) approval at each of the eight bariatric centers (Sander Medical Center (Sander), Endodiagnostic (Ramos and Matz), Hospital Vita Batel e pos Graduacao da Universidade Positivo (Baretta), Kaiser Day Hospital (Quadros and Grecco), ABC Medical School (Barrichello), Clinica Concon e Hospital e Maternidade Galileo (Filho), Usuy Clinic (Usuy Jr), Hospital 9 July (Amorim and Neto), and Orlando Regional Medical Center (Teixeira)) in the USA and Brazil, and following the Health Insurance Portability and Accountability Act guidelines, the authors performed a retrospective chart review of 558 patients who underwent APC procedure between 31st July 2009 and 29th March 2017. APC was performed on patients who regained weight after RYGB procedure. For patients who underwent primary RYGB at the same institutions, approximate size of the pouch was 3–6 cm, and the efferent limb length was between 75 and 150 cm, depending on the preoperative BMI. Patients with less than 6 months of follow-up after APC intervention were excluded from the study.
Patients were eligible for APC procedure when longer than 18 months has passed since their primary RYGB procedure, when they gained greater than 10% of their nadir weight, when they complained of lack of satiety, and when the size of GJ anastomosis was greater than 15 mm. The excess BMI loss was calculated as 25 kg/m2 being the ideal BMI. The total weight loss was calculated as the difference between initial weight and follow-up weight, divided by the initial weight. Multi-disciplinary team evaluation was performed prior to the APC procedure. Contraindications for the procedure included coagulation disease, ring displacement, severe gastroesophageal reflux disease, marginal ulcerations, and a pouch that is smaller than 3 cm.
APC Technique
In the endoscopy suite, the patient was placed on left side down, and a monitored anesthesia care (MAC) was given. Sedation was given using propofol under an anesthesiologist, and patients were not intubated. Using a diagnostic Olympus gastroscope 180 access was gained to the gastric pouch and the gastrojejunostomy. The ERBE USA argon plasma coagulator (APC™) Circumferential Probe (O.D. 2.3 mm/6.9 Fr., length 220 cm), that is connected to the ERBE or WEN APC generator with the setting pulsating 2 l and 70 W was passed. After that, the argonium was passed circumferentially at the gastrojejunostomy. Once that was performed, the catheter and scope are retrieved and the patient was taken to the recovery unit. The duration of the procedure was approximately 5–10 min, and the duration of hospital stay was approximately 30–60 min.
The size of the gastrojejunostomy (GJ) was measured using either articulated device for anastomosis scouting or an experimental guidewire with a hydrophilic flexible tip as previously described [14].
Patients were placed on liquid diet for 10–15 days and were allowed to progress on their diet afterwards. Patients were followed up at each office clinic monthly for 6 months after the procedure and every 3–6 months afterwards. Follow-up visits included weight measurement, clinical history, and examination.
Statistical analysis was performed using SAS software version 9.4. All data for age and BMI are demonstrated as mean ± standard deviation, unless otherwise noted. Types of analysis include descriptive analysis, paired Student’s t test, one-way ANOVA, logistic regression, and multi-level model for change with p < 0.05 regarded as statistically significant.
Results
Demographics of patients from each center are shown in Table 1. All centers had a similar distribution in gender (p = 0.70). While most centers were similar in baseline age and BMI, three centers showed older mean age than other centers, one center showed higher mean BMI, and another showed lower mean BMI compared with other centers. The differences are shown in box plots (Fig. 1). Overall, 81.5% were female with a mean age of 40.9 years, and their mean BMI at the time of APC was 34.0 kg/m2.
Details of initial RYGB was not available in all patients, and many patients reported the year of their RYGB procedure. Therefore, mid-point of the year (1st July) was used to calculate the period between RYGB and APC intervention in these patients. The median number of years between RYGB and APC was 7.5 years (Table 2). Many patients underwent APC several times, and the median number of intervention in these patients was two times. However, the trend of weight loss was recorded as using the first APC intervention as baseline.
Mean size of the gastrojejunostomy before APC intervention was 24.4 mm, and this decreased to a mean size of 14.0 mm after the intervention. The difference was statistically significant (p < 0.0001). The mean size of gastrojejunostomy at the time of APC intervention was not correlated to baseline BMI (p = 0.67).
Weight Loss
Upon exploratory analysis of the individual BMI data, the mean BMI decreased slightly during the first 24 months and increased slightly afterwards following the APC intervention (Fig. 2). Due to this trend, a linear regression was not imposed to the model. Rather, we treated time as categorical and allowed the change to differ at different follow-up points. A multi-level for change model was used to show changes in TWL at each center (Fig. 3). The extent of weight loss differed greatly among centers. Overall, the TWL increased rapidly during the first 6 months and showed a decline in some centers and an increase in others until 12 months. Most centers showed a plateau of TWL between 12 and 24 months. After 24 months, all centers with available data showed decrease in TWL. Where data were available, the mean of lowest weight was 67.0 ± 23.0 kg and the mean of lowest BMI was 24.1 kg/m2 following gastric bypass. The mean weight loss was 6.5, 7.7, and 8.3 kg at 6, 12, and 24 months, respectively, and the changes in weight over time was statistically significant (p < 0.0001) (Table 3).
Because our patients included many with BMI of less than 30 kg/m2 and this could skew the result of EBMIL, we divided the patients into two groups, one with pre-APC BMI less than 30 kg/m2, and another with pre-APC BMI greater than or equal to BMI at 30 kg/m2. Multi-level for change model showed the high BMI group to have greater TWL than the low BMI group at 6, 12, and 24 months (Fig. 4). Using Tukey’s adjustment and Toeplitz error covariance structure, at 6, 12, and 24 months, the differences in TWL were significant between the two groups, 2.7% (p < 0.001), 4.4% (p < 0.0001), and 6.3% (p < 0.0001), respectively. However, at 36 months, the differences in TWL between the two groups were not significant (p = 0.45). Mean BMI and EBMIL, as well as TWL in these two groups are shown in Table 4.
While the number of APC procedure performed was correlated to the total weight loss at 12 months (p = 0.02), this correlation was not significant at 24 months (p = 0.76) and at 36 months (p = 0.98).
Complications
Only four centers provided data for complications. Of these 333 patients, a total of 18 (5.4%) patients experienced complication after APC, including stenosis (n = 9), GJ ulcer (n = 3), vomiting (n = 3), GJ leakage (n = 2), and melena (n = 1). These complications were treated conservatively or via endoscopy. GJ leakages were isolated events that occurred at two different centers (one at each center). One patient was 26th patient, and the other was 28th patient.
Discussion
When it comes to managing patients with weight regain, many options exist for bariatric surgeons including revision of gastrojejunostomy and/or trimming of the pouch [15,16,17], banding the bypass [18], converting to a distal RYGB [6, 19, 20], and converting RYGB to biliopancreatic duodenal switch [21, 22]. However, these surgical revisions or conversions come with increased postoperative complication rates, and the effect of conversion on weight loss can sometimes be limited. Nguyen et al. [15] reported that 5 (10.6%) out of 47 patients undergoing revision of the RYGB were converted from laparoscopic to open. Keshishian et al. [22] and Parikh et al. [21] reported their peri-operative complication after conversion to duodenal switch to be 8–12%. Conversion to duodenal switch is also technically challenging and poses malnutrition risk [23]. Weight loss after salvage banding varies greatly among centers, ranging from 28.0 to 64.9% in EBMIL [18]. To minimize complication rate, endoscopic approaches have also been suggested including endoscopic suturing [24].
In this study, endoscopic APC was utilized in the attempt to decrease the diameter of dilated gastrojejunostomy and therefore reinitiate weight loss in RYGB patients. The theory behind this procedure is similar to that of gastrojejunostomy revision in patients with weight regain as well as endoscopic suturing, which focus on the anatomical aspect of causes in weight regain. Endoscopic approaches are less invasive than laparoscopic approaches and minimize exposure of patients to peri-operative complications. As we can see from the results, the diameter of gastrojejunostomy decreased significantly from a mean value of 25.5 to 14.8 mm after the intervention. In comparison, Patel et al. [24] showed gastrojejunostomy diameter to decrease from a mean value of 30.2 to 4.8 mm after endoscopic suturing. Before we dive into details of weight loss, we want to note that 25.1% of our patients had a BMI less than 30 kg/m2 at the time of APC. Because we set the ideal BMI at 25 kg/m2, merely losing 2 BMI point in a patient with pre-APC BMI of 26 kg/m2 can result in 200% of EBMIL, and thereby skew the overall result in EBMIL. Hence, we separated the patients into two groups, one with pre-APC BMI less than 30 kg/m2, and another with pre-APC BMI greater than or equal to 30 kg/m2. The higher BMI group still had a mean BMI of 36.1 ± 4.9 kg/m2, and this is lower than average BMI of patients undergoing a revision.
In the low pre-APC BMI group, we observed a great mean EBMIL of 79.3% at 6 months. However, due to the reason mentioned above, mean TWL was 4.7% in this group. In the high pre-APC BMI group, the mean EBMIL was 26.7% at 6 months, and the mean TWL was 7.5%. As we have predicted, the difference in the mean TWL was significant between the two groups at 6 months. This difference was still observed at 12 and 24 months and was no longer apparent at 36 months. We should note the large standard deviation, and that the result varied greatly from a patient to another. We should also note that the follow-up rate was poor at both 24 and 36 months, and this could have biased the results. Nevertheless, follow-up rate was similar in both groups, 14.6% in the low pre-APC BMI group and 13.0% in the high pre-APC BMI group at 24 months, and 4.3 and 3.6% at 36 months, respectively. In a study by Nguyen et al. [15], percentage of excess weight loss (EWL) of 35, 46, 39, 35, and 34% at 6, 12, 24, 36, and 48 months after revision of the gastrojejunostomy with or without trimming of the pouch. Mean baseline BMI of their patients was 41.6 kg/m2. Considering that the expected EBMIL is less in patients with higher baseline BMI [25,26,27], EBMIL in our patients was comparable with their EWL until 24 months after the intervention. However, difference was observed in the two studies at longer follow-up, and more studies are warranted in the validity of sustainable weight loss for APC patients.
Patel et al. [24] reported EWL of 13.0% at 6 months and 10.0% at 12 months after endoscopic suturing. Baseline mean BMI was higher in their study compared with ours, at 41.7 kg/m2.
It is interesting to note that the pattern of weight loss differed across centers as seen in Fig. 3. This could have been due to differences in APC protocol as well as in baseline patient characteristics. Complication rate in our patients was 3.2% (n = 18), including three patients with vomiting and one with melena. Patel et al. [24] reported that 15 (30.0%) out of 50 patients reported nausea, emesis, and abdominal pain after endoscopic suturing and 3 (6.0%) required a revision. We believe bariatric surgeons and endoscopists with proper training and certification would be able to perform the APC procedure.
Although the cost of APC differs from center to center, the overall cost of the procedure may be comparable with or even less than using weight loss medication. Because the insurance does not cover the weight loss medication, some medications can cost up to $200/month. Adding copayment for clinic visits, medication use can easily add up to $1000–$1500/year.
Several limitations of this study include selection bias due to loss of follow-up. We were not able to demonstrate a significant result for long-term follow-up and a longer prospective study may be needed to validate our result. Because this was a multi-center study, difference in baseline patient characteristics could have skewed the result. Accuracy of the data from each center was not checked, and intervention protocol could have differed from center to center. Also, patient population in general had lower BMI than patients undergoing revisions, and this warrants an inference issue. In addition, performing APC for patients with BMI less than 30 kg/m2 is controversial because the definition of significant weight gain does not apply and the risk of death from obesity is low at this BMI category. We did not have data on total protein, albumin, vitamins, and mineral levels, which could possibly occur when stricture is present after the APC procedure. We also did not have data on how taking or stopping proton pump inhibitors affected symptoms of reflux after the APC procedure, as well as resolution of other comorbid status. Because this is a retrospective study, a randomized, prospective format may be needed to validate the results. However, this is one of the largest reports on utilizing APC for weight regain in RYGB patients, and we believe it provides information on a valid option for addressing weight regain.
Conclusion
APC can be useful in reducing the regained weight after RYGB, and patients showed 6–10% total weight loss at 12 months. Randomized trials would be needed to validate the findings.
References
Maciejewski ML, Arterburn DE, van Scoyoc L, et al. Bariatric surgery and long-term durability of weight loss. JAMA Surg. 2016;151(11):1046–55.
Adams TD, Davidson LE, Litwin SE, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377(12):1143–55.
Hawkins RB, Mehaffey JH, McMurry TL, et al. Clinical significance of failure to lose weight 10 years after roux-en-y gastric bypass. Surg Obes Relat Dis. 2017;13(10):1710–6.
Magro DO, Geloneze B, Delfini R, et al. Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg. 2008;18(6):648–51.
Moon RC, Teixeira AF, Jawad MA. Treatment of weight regain following roux-en-Y gastric bypass: revision of pouch, creation of new gastrojejunostomy and placement of proximal pericardial patch ring. Obes Surg. 2014;24(6):829–34.
Christou NV, Look D, Maclean LD. Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg. 2006;244(5):734–40.
Dakin GF, Eid G, Mikami D, et al. Endoluminal revision of gastric bypass for weight regain--a systematic review. Surg Obes Relat Dis. 2013;9(3):335–42.
Yimcharoen P, Heneghan HM, Singh M, et al. Endoscopic findings and outcomes of revisional procedures for patients with weight recidivism after gastric bypass. Surg Endosc. 2011;25(10):3345–52.
Spaulding L, Osler T, Patlak J. Long-term results of sclerotherapy for dilated gastrojejunostomy after gastric bypass. Surg Obes Relat Dis. 2007;3(6):623–6.
Jin F, Mu D, Xie Y, et al. Application of bronchoscopic argon plasma coagulation in the treatment of tumorous endobronchial tuberculosis: historical controlled trial. J Thorac Cardiovasc Surg. 2013;145(6):1650–3.
Lee YA, Chun P, Hwang EH, et al. Gastric hemangioma treated with argon plasma coagulation in a newborn infant. Pediatr Gastroenterol Hepatol Nutr. 2017;20(2):134–7.
Kapadia S, Nagula S, Kumta NA. Argon plasma coagulation for successful fragmentation and removal of an over-the-scope clip (OTSC). Dig Endosc. 2017;29:820–1.
Baretta GA et al. Argon plasma coagulation of gastrojejunal anastomosis for weight regain after gastric bypass. Obes Surg. 2015;25(1):72–9.
de Quadros LG, Galvão Neto MP, Campos JM, et al. Validation of a new method for the endoscopic measurement of post-bariatric gastric outlet using a standard guidewire: an observer agreement study. BMC Res Notes. 2017;10(1):13.
Nguyen D, Dip F, Huaco JA, et al. Outcomes of revisional treatment modalities in non-complicated roux-en-Y gastric bypass patients with weight regain. Obes Surg. 2015;25(5):928–34.
Patel S, Szomstein S, Rosenthal RJ. Reasons and outcomes of reoperative bariatric surgery for failed and complicated procedures (excluding adjustable gastric banding). Obes Surg. 2011;21(8):1209–19.
Muller MK et al. Laparoscopic pouch resizing and redo of gastro-jejunal anastomosis for pouch dilatation following gastric bypass. Obes Surg. 2005;15(8):1089–95.
Vijgen GH et al. Salvage banding for failed Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2012;8(6):803–8.
Dapri G, Cadiere GB, Himpens J. Laparoscopic conversion of Roux-en-Y gastric bypass to distal gastric bypass for weight regain. J Laparoendosc Adv Surg Tech A. 2011;21(1):19–23.
Rawlins ML, Teel II D, Hedgcorth K, et al. Revision of Roux-en-Y gastric bypass to distal bypass for failed weight loss. Surg Obes Relat Dis. 2011;7(1):45–9.
Parikh M, Pomp A, Gagner M. Laparoscopic conversion of failed gastric bypass to duodenal switch: technical considerations and preliminary outcomes. Surg Obes Relat Dis. 2007;3(6):611–8.
Keshishian A, Zahriya K, Hartoonian T, et al. Duodenal switch is a safe operation for patients who have failed other bariatric operations. Obes Surg. 2004;14(9):1187–92.
Maleckas A, Gudaitytė R, Petereit R, et al. Weight regain after gastric bypass: etiology and treatment options. Gland Surg. 2016;5(6):617–24.
Patel LY, Lapin B, Brown CS, et al. Outcomes following 50 consecutive endoscopic gastrojejunal revisions for weight gain following roux-en-Y gastric bypass: a comparison of endoscopic suturing techniques for stoma reduction. Surg Endosc. 2017;31(6):2667–77.
Moon RC, Nelson L, Teixeira AF, et al. Outcomes of Roux-en-Y gastric bypass in the super obese: comparison of body mass index 50–60 kg/m(2) and>/=60 kg/m(2) with the morbidly obese. Surg Obes Relat Dis. 2016;12(2):292–6.
Taylor JD, Leitman IM, Hon P, et al. Outcome and complications of gastric bypass in super-super obesity versus morbid obesity. Obes Surg. 2006;16(1):16–8.
Thereaux J, Czernichow S, Corigliano N, et al. Five-year outcomes of gastric bypass for super-super-obesity (BMI>/=60 kg/m(2)): a case matched study. Surg Obes Relat Dis. 2015;11(1):32–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
For this type of study, formal consent is not required.
Informed Consent
Does not apply.
Additional information
The abstract of this article has been selected to present at International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) 2017 Annual Meeting (Aug 29th–Sep 2nd, 2017, London, UK)
Rights and permissions
About this article
Cite this article
Moon, R.C., Teixeira, A.F., Neto, M.G. et al. Efficacy of Utilizing Argon Plasma Coagulation for Weight Regain in Roux-en-Y Gastric Bypass Patients: a Multi-center Study. OBES SURG 28, 2737–2744 (2018). https://doi.org/10.1007/s11695-018-3229-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3229-5