Abstract
Background
The failure of approximately 20 % of obese patients who undergo Roux-en-Y gastric bypass (RYGB) to maintain weight loss over the following 18–24 months is related to the surgical procedure, to the patient, or both. Although the underlying mechanisms are uncertain, one factor that has been postulated is the dilation of the gastrojejunal anastomosis. The objective was to evaluate the safety and efficacy of the serial use of argon plasma coagulation (APC) in reducing the diameter of the dilated gastrojejunal anastomosis and post-RYGB weight regain.
Methods
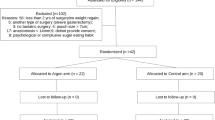
We carried out a prospective, nonrandomized study of 30 patients, with no control or sham group, monitoring RYGB weight regain associated with dilation of the gastrojejunal anastomosis over a postoperative period of 18 months. Each patient underwent three sessions of APC in the anastomosis separated by 8 weeks, with a final endoscopic examination 8 weeks after the last session.
Results
There was a loss of 15.48 kg (range = 8.0–16.0 kg) of the 19.6 kg (range = 7.0–39.0 kg) of regained weight after RYGB and a reduction of 66.89 % in the final anastomotic diameter, with statistically significant reductions between each APC session. Previous body mass index significantly decreased up to the final examination, and the final weight was close to but not at the same level as the nadir.
Conclusions
Our study indicates that the use of APC to treat weight regain after RYGB is a safe and effective procedure and promotes a reduction in gastrojejunal anastomosis, final weight, and BMI, with a low rate of complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Roux-en-Y gastric bypass (RYGB) is the most common bariatric surgery performed all around the world, and weight loss resulting from this procedure leads to the improvement of obesity-related diseases [1]. In general however, approximately 20 % of patients who undergo RYGB will experience weight regain over the 24 months after surgery. A variety of factors have been invoked to explain this phenomenon, including overeating, inappropriate diet, sedentarism and lack of regular exercise, metabolic factors, hormonal changes, inappropriate choice of surgical technique, gastrogastric fistulas, loss of function of the restrictive band when present, dilation of the gastric pouch, and dilation of the gastrojejunal anastomosis [2].
The first and most important step in the treatment of this condition is the reintroduction of the patient to a multidisciplinary clinical team, which entails dietary counseling and behavioral changes. In addition, a variety of endoscopic and surgical procedures methods have been proposed for reducing weight in patients with post-RYGB weight regain. Although revisional surgery can be performed to address anatomical issues associated with weight regain [3], it has been associated with high morbidity [4, 5].
A variety of endoscopic procedures have been designed to reduce the diameter of the gastric pouch and/or gastrojejunal anastomosis to promote weight loss. These include endoluminal injection of sodium morrhuate into the anastomosis [6, 7], the Bard Endocinch® [8], the Stomaphyx® from Endogastric Solutions [9], the ROSE® procedure [10], the Apollo Endosurgery Overstitch® [11], the OTSC® clip [12], and the coagulation of gastrojejunal anastomosis with argon as described by Aly in 2009 [13].
Argon plasma coagulation (APC) is a noncontact eletrocoagulation method in which radiofrequency energy is applied to the tissue by means of ionized gas, and has various applications in the field of bariatric endoscopy. It has been shown to effect a progressive reduction in the diameter of the gastrojejunal anastomosis, with a consequent delay in gastric emptying, resulting early satiety and a reduction in body weight. At the end of 2009, we began performing APC of the dilated gastrojejunal anastomosis in patients with weight regain following RYGB. Here, we evaluated the first 30 cases to assess the safety and efficacy of the use of serial APC to decrease the diameter of the gastrojejunal anastomosis and reduce post-RYGB weight gain.
Materials and Methods
Patients
All 30 patients (Table 1) included in the study exhibited the required weight regain after a minimal period of 18 months post-RYGB in accordance with the criteria for inclusion in the study.
Inclusion Criteria
-
Age between 18 and 65 years;
-
Minimal postoperative period of 18 months;
-
Regain of at least 10 % of lowest weight attained post-RYGB;
-
Anastomotic diameter of at least 15 mm;
-
Able to understand the procedures of the study;
-
Voluntary agreement to participate in the study; signing an informed consent form.
Exclusion Criteria
-
Impossibility of endoscopic handling of the gastrojejunal anastomosis;
-
Stenosis of anastomosis blocking the progression of the apparatus before the end of the third endoscopic session of APC;
-
History of hepatic disease with cirrhosis or active chronic hepatitis
-
Undergoing anticoagulant therapy, with the exception of platelet antiaggregants;
-
Pregnancy or intending to become pregnant in the 12 months after APC;
-
Participating in other ongoing clinical investigation;
-
Anemia or severe nutritional deficiencies, alcoholism and drug addiction, recent neoplasia (less than 5 years), and HIV seropositivity;
-
Allergy to mixtures of the anesthetic propofol;
-
Unable to return for scheduled clinic visits and sessions of APC, and unable to follow nutritional guidelines and to understand the procedures of the study;
-
Dropping out of the study after three endoscopic sessions.
Pre-procedure Preparation
After the endoscopy, a clinic visit recorded the following information in the specific protocol:
-
(a)
Data of prior bariatric operation;
-
(b)
Type of surgical access: conventional or laparoscopic;
-
(c)
Initial weight and BMI (immediately before bariatric operation);
-
(d)
Lowest weight and BMI attained after the bariatric operation;
-
(e)
Weight immediately after the first session of APC;
-
(f)
Percentage of weight regained;
The patients fasted completely for a period of 12 h and underwent upper digestive endoscopy to check the diameter of the gastrojejunal anastomosis.
Endoscopic Technique
-
(a)
Positioning: Patient was positioned in left lateral decubitus with peripheral venous access in the arm, oximeter, and nasal catheter of oxygen at 2 L/min.
-
(b)
Anesthesia: Effected by administration of endovenous propofol and fentanyl under the supervision of the anesthesiologist.
-
(c)
Measurement of Anastomotic Diameter: Upper digestive endoscopy with a Fujinon® series 200 apparatus and measurement of the diameter of the gastrojejunal anastomosis with Olympus® forceps (Centre Valley, PA, USA) with a 20-mm opening and determination of the presence or not of a restrictive band.
-
(d)
Coagulation of Anastomosis: With the use of SS-200E® argon, Argon 2® argon plasma coagulator and WEM® electrocautery device, the coagulation was performed with a disposable endoscopic catheter, with a potency of 90 W and at 2 L/min over the entire circumference of the gastrojejunal anastomosis from the anastomotic portion in the gastric pouch up to the jejunal side with a distance from the point of the catheter up to the mucosa of 3–5 mm (Fig. 1).
-
(e)
The morning before eating, a proton pump inhibitor, pantoprazol (40 mg) was prescribed for up to 30 days after the last endoscopic session, along with paracetamol drops as needed and liquid sucralfate every 6 h for 3 days after each coagulation session.
-
(f)
Patient was placed on a diet that was gradual and progressive in its consistency and volume, 1 week per step for a total of 4 weeks, to avoid bleeding in the coagulated area, as well as an abrupt distension of the gastric pouch and consequent dilation of the gastrojejunal anastomosis.
-
(g)
Two additional sessions were carried out at intervals of 8 weeks (Figs. 2 and 3), followed by a final endoscopic evaluation 8 weeks after the third session (Fig. 4).
Post-procedure Follow-Up
At each endoscopic session (three sessions in total), all patients were evaluated with regard to the following:
-
(a)
Body weight at each endoscopic session and 8 weeks after the session;
-
(b)
Anastomotic diameter at each endoscopic session and 8 weeks after the last session.
There was no specific protocol for physical activity or psychological/psychiatric and nutritional follow-up, with the exception of a stepwise diet of 4 weeks after each session for the purpose of not forcibly dilating the anastomosis. Patients were encouraged to maintain contact with the authors by telephone or e-mail to report any symptoms or clinical signs.
This study was conducted in the Digestive Endoscopy Service of Hospital Vita Batel – Endobatel, which was previously approved by the local Committee of Ethics and Research on Humans under No. 43/2012 and CAAE 08531913.4.0000.5529.
Results
The majority of the study sample were women (86.66 %), and the mean age of the study sample was 42.83 years (range = 22–59 years). Immediately after the surgical treatment of morbid obesity, mean body weight was 121.77 ± 22.50 kg, (range = 95–200 kg) and mean BMI was 45.63 ± 7.63 kg/m2 (range = 33.44–66.22 kg/m2).
RYGB resulted in significant weight loss (p < 0.0001), with a lowest postsurgical mean weight of 74.77 ± 16.51 kg (mean range = 49–127 kg). Compared with the lowest mean weight in the RYGB postoperative period, there was a mean postoperative weight gain of 19.6 kg (27.5 %) (mean range = 7.0–39.0 kg (10.3–65 %) (p < 0.0001). The mean regained weight loss (MRWL) after the three sessions of APC at the gastrojejunal anastomosis was 15.48 kg (8.0 ± 16.0 kg). Statistically significant weight reduction was observed when comparing body weight immediately after the first session of APC with the mean body weight measured after the third session of endoscopic treatment (p < 0.0001), 8 weeks after the third session (p < 0.0001) and between these two events (p < 0.0001) (Fig. 5). Similarly, there was a significant (p < 0.0001) reduction in BMI between the values measured at the beginning of the coagulation sessions, after the third session and 8 weeks after the end of the last session (Table 2). Moreover, there was a progressive statistically significant reduction in the diameter of gastrojejunal anastomosis during all APC sessions, as well as 8 weeks after the end of sessions (p < 0.0001) (Table 3). In addition, compared with the diameter prior to the first session of APC, the diameter of the anastomosis decreased by an average of 17 mm (66.89 %) on final examination after the three endoscopic sessions. All patients in the sample reached a diameter of 12 mm or less, such that 10 % of patients had a final diameter of 10–12 mm, 53.33 % had a final diameter of 8–10 mm, and 36.66 % had a final diameter of 6–7 mm. When %MRWL was compared with the percentage reduction of anastomotic diameter after each session of APC, weight loss increased with decreasing diameter (Fig. 6).
When final anastomotic diameters were divided into two groups (6–9 mm and 10–12 mm), there was a statistically insignificant trend towards higher %MRWL in the larger anastomotic diameter group, demonstrating that a final diameter between 10 and 12 mm is sufficient for adequate weight loss (Table 4). Note that it was not possible to compare individuals under and over 20 mm measured prior to the first APC since only two patients had an anastomosis diameter under 20 mm.
The only complications observed were severe stenosis (anastomotic diameter less than 3 mm) in two patients after the first session of APC; these patients were removed soon after onset of the study. The diameter of the anastomosis prior to the first session of APC was 20 mm in both patients. The incidence of anastomotic ulcers in the second session was 10 % (n = 3), 10 % in the third session (n = 3, where one patient had persistent ulcerated lesion), and only 3 % in the final endoscopic evaluation.
Eating habits and vomiting frequency after each session of endoscopic APC were not evaluated.
Discussion
Weight regain after RYGB, defined as a gain of at least 10 % of the lowest weight achieved after bariatric surgery [14], has been estimated to occur in around 10–20 % of patients over the 5−10 years after the procedure [15]. Although a variety of criteria have been used, such as the loss of more than 50 % of excess weight and BMI <35 kg/m2, there is no well-defined consensus in relation to the failure in the loss and maintenance of weight after bariatric surgery. Accordingly, it may be argued that preferable indications of success might encompass postsurgical improvement in associated and existing comorbidities or even improvement in the quality of life.
APC is a noncontact electrocoagulation method in which radiofrequency energy is applied to the tissue by means of ionized argon gas, and was used initially for open and laparoscopic procedures, prior to its use for digestive endoscopy in a variety of gastrointestinal conditions. The principal indications are gastrointestinal bleeding from diverse etiologies, tissue growth after implantation of stents, opening the lumen of hollow organs obstructed by tumor growth, sectioning of parenchyma of solid organs such as the liver and spleen, and more recently, bariatric endoscopy [16, 17].
The limited depth of tissue penetration of 2–3 mm, associated with excellent coagulation, allows the application of APC in critical areas such as the duodenum and colon. The higher the power input in watts, the greater the depth of penetration, which can affect even the muscular layer of mucosa [18]. It has been well demonstrated that there is greater incidence of dysphagia and stenosis on performing coagulation of the circumferential areas of the esophageal mucosa, mainly associated with the application of a high quantity of energy [19, 20]. A decrease in BMI from 32.8 (±1.9) to 29.7 kg/m2 (±1.8) in 3 months has been reported with the OTSC Clip® (Over the Scope Clip) in patients with weight regain after gastric bypass associated with dilation of the gastrojejunal anastomosis [12]. In addition, a 40.5- to 37.7-kg/m2 decrease in BMI has been reported with the use of the EndoCinch® (Bard), with a loss of 23.4 % of excess weight regained after RYGB [8].
The Randomized Evaluation of Endoscopic Suturing Transorally For Anastomotic Outlet Reduction (RESTORe) clinical study was a sham-controlled trial undertaken to evaluate the safety and effectiveness of an endoluminal approach namely, transoral suturing using the Bard EndoCinch Suturing System, to treat weight regain/inadequate weight loss after RYGB. This trial provided a level I evidence establishing the safety and a 6-month effectiveness of the transoral outlet reduction procedure for treatment of inadequate weight loss and/or weight regain after RYGB [21].
An evaluation of %MRWL after RYGB in 231 patients with one to three sessions of sclerotherapy of the dilated gastrojejunal anastomosis with sodium morrhuate demonstrated a loss of 18 % of weight regained after 6 months. In the 32 % of individuals who underwent two or three sessions of sclerotherapy, the percentage loss of weight regained was as much as 61 % [22]. In 116 patients with weight regain after gastric bypass who underwent the ROSE® (Restorative Obesity Surgery, Endoluminal - USGI) endoscopic procedure, a reduction of 32 % of regained weight was observed 6 months after the procedure [23]. The same procedure was performed in patients with weight regain 24 months after gastric bypass and dilation of the anastomosis and/or gastric pouch. A total of 116 patients were evaluated with 12 months of follow-up after the endoscopic procedure. Mean body weights were 145.3 ± 27.1 kg after gastroplasty, 85.4 ± 17.1 kg the lowest attained and 110.5 ± 20.5 kg after the endoscopic procedure. The corresponding BMIs were 52.4 ± 9.1, 30.8 ± 5.4, and 39.9 ± 6.7 kg/m2, respectively. Loss to follow-up in 12 months was 34.8 %, and weight loss was 5.9 ± 1.1 kg (14.5 ± 3.1 %) [10].
Endoscopic treatment with Stomaphyx® (Endogastric Solutions, Redmond, Washington, USA) was applied in 39 patients with weight regain after RYGB to promote weight loss. The mean weight loss in 1 year was 10.0 kg and the incidence of complications was minimal [9]. In a recent publication, Himpens et al. reported the results of revisional surgery in 58 patients with weight regain or insufficient loss of weight more than 2 years after RYGB. Although BMI decreased from 39.1 ± 11.3 to 29.6 ± 12.4 kg/m2 in 4 years, which is higher than that observed with any endoscopic technique, the rate of general complications was 20.7 %, consisting of reoperations in 7.3 % of patients, and fistula in 12.1 % [5].
Most studies have reported a reduction in BMI and mean body weight and loss of excess weight. Here, we report what we refer to as mean percentage loss of weight regained. %MRWL after RYGB varied from 35.9 to 188.9 % with a mean of 89.10 %, that is, the sample of 30 patients who underwent endoscopic APC lost about 90 % of the weight regained. It should be noted that the %MRWL value was measured only 8 weeks after the third session of APC and likely will not be maintained over time, and additional studies with large sample sizes, control groups, and future examinations will be required to investigate this point.
Some patients reached a weight below the lowest weight achieved after RYGB. The mean weight after APC was 94.35 kg (±18.04), and at the final evaluation 8 weeks after the last session, it was 78.87 kg (±17.11) (p < 0.0001). Although the final body weight (78.87 ± 17.1 kg, range = 48–135 kg), measured 8 weeks after the last session of endoscopic treatment did not return to the lowest point (74.77 ± 16.5 kg, range = 49–127 kg) measured after the gastroplasty, it was nevertheless statistically lower (p = 0.008).
In relation to mean BMI, the initial value in the bariatric surgery period, that after APC and final the 8 weeks after the third endoscopic session were respectively 45.63 ± 7.63, 35.35 ± 6.53, and 31.14 ± 5.81 kg/m2, all of which were statistically significant (p < 0.0001). With regard to mean body weight, the value in the initial phases (after bariatric surgery), the minimal value reached after the surgery, that after APC, that in the third argon session and that on final evaluation 8 weeks after the last session were respectively 121.77 ± 22.50, 74.77 ± 16.51, 94.35 ± 18.04, 83.29 ± 17.10, and 78.87 ± 17.11 kg. This indicates significant weight loss after RYGB (p < 0.0001), significant weight regain after 24 months (p < 0.0001) and significant weight loss after three sessions of APC (p < 0.0001). Compared with other studies, this represents the greatest mean percentage reduction in weight regained after RYGB, although, as noted above, these are short-term results that likely will not maintained over time.
Although most studies use a diameter of >20 mm to define dilation of the anastomosis [24], some use a diameter of 12 mm, similar to that created manually in the gastrojejunal anastomosis using a 36 FR Fouchet bougie [17]. In our study, the minimal cross-section diameter was 15 mm and the maximum measured in the first session was 45 mm, with a minimum of 18 mm; two patients had diameters under 20 mm. This anastomotic diameter was measured using an Olympus® forceps (Centre Valley) with an opening of 20 mm rather than the pivoted instrument from the same company used by Yimcharoen et al. [25], because it is registered by ANVISA in Brazil.
Heylen et al. reported a reduction in mean anastomotic diameter from 35 mm (range = 21–48 mm) to 8 mm (range = 3–21 mm), with a final reduction in diameter of 80 % [12]. Reductions of 68 and 50 % in mean anastomotic diameter have been reported using the Bard EndoCinch® [8] and the ROSE® procedure [10], respectively, the latter study finding a statistically significant greater loss of weight in patients with a diameter of less than 10 mm [10].
In relation to sclerosis of the gastrojejunal anastomosis with sodium morrhuate, Spaulding in 2003 carried out a mean of 1.3 endoscopic sessions in 20 patients aiming (100 %) a final anastomotic diameter of 9–10 mm [6].
We observed a progressive and statistically significant reduction in the diameter of the gastrojejunal anastomosis during all endoscopic sessions, as well as on final evaluation 8 weeks after the end of three sessions (p < 0.0001). While these data do not compare favorably with those obtained using the OTSC® clip (80 % reduction), they are similar to those obtained using EndoCinch® and outperform other procedures with respect to this variable. It should be noted that to restrict the analysis to a single variable, we used only the parameter anastomotic diameter and did not evaluate the length and diameter of the pouch. A final diameter between 10 and 12 mm was found in 33.33 % of patients while 66.66 % had a final diameter between 6 and 9 mm. There was no statistically significant difference between these two groups with respect to final anastomotic diameter, and no difference was observed in relation to percentage loss of weight regained.
Since we found that the diameter could be progressively reduced with increasing number of endoscopic sessions, we performed at least three sessions of APC at the gastrojejunal anastomosis. APC could also be used in a preventative manner to prevent weight gain. For example, since it is known that a dilated gastrojejunal anastomosis is a risk factor for weight regain [26], coagulation could be performed in upper digestive endoscopy at 24 months postoperative, in cases where the anastomosis is dilated (more than 15 mm), to reduce the chance of future weight regain.
The reintroduction of the patient to a multidisciplinary team is mandatory in cases of weight regain and loss to postoperative follow-up. A psychological and/or psychiatric evaluation is obligatory, as well as nutritional therapy and stimulation of physical activity. The monitoring of food intake and body weight, closer follow-up of the operated patients, appropriate choice of technique in accordance with the patient and with the experience of the surgeon, and a good learning curve are factors that can decrease the failure rate of bariatric surgery.
To cause greater tissue retraction and later reduction in anastomotic diameter owing to the greater depth of coagulation in the mucosa, we used a higher voltage (90 W) than that reported by Aly et al. [13] (70 W). Similarly, given the high incidence of anastomotic ulcers observed at the beginning of this study, we used a longer between session interval (8 vs 6 weeks [13]). The incidence of anastomotic ulcers was 10 % (three patients) observed in the second session, 10 % in third session (three patients, one of which had a persistent ulcer) and only 3 % (one patient, with ulcer in the third session but not the second) on final endoscopic evaluation. In total, there were seven anastomotic ulcerated lesions in five patients.
The long-term results of our study are undefined, particularly with respect to the possibility of de novo weight regain or dilation of the anastomosis. As already described, coagulation of the anastomosis using endoscopic APC can be performed in a serial manner and as many times as necessary. Unlike the majority of endoscopic apparatuses for suturing an anastomosis, argon is approved by ANVISA. Moreover, this procedure is low cost, easy to use, is not dependent on further training of endoscopists, and is safe, rapid, and associated with minimal side effects and complications. Compared with other endoscopic methods argon plasma coagulation also exhibits a greater percentage of loss of weight regained and greatly reduces the necessity for revisional surgery in patients with weight regain after RYGB.
Conclusions
Serial APC of the gastrojejunal anastomosis leads to weight regain loss and reduction in the diameter of the anastomosis and BMI in patients with post RYGB weight regain. The reintroduction of the patient to the multidisciplinary team and focused follow-up are mandatory to obtain satisfactory future results.
References
Buchwald H et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Barhouch AS et al. Excess weight loss variation in late postoperative period of gastric bypass. Obes Surg. 2010;20(11):1479–83.
Morales MP et al. Laparoscopic revisional surgery after Roux-en-Y gastric bypass and sleeve gastrectomy. Surg Obes Relat Dis. 2010;6(5):485–90.
McKenna D. et al. Revisional bariatric surgery is more effective for improving obesity-related co-morbidities than it is for reinducing major weight loss. Surg Obes Relat Dis 2013.
Himpens J et al. Outcomes of revisional procedures for insufficient weight loss or weight regain after Roux-en-Y gastric bypass. Obes Surg. 2012;22(11):1746–54.
Spaulding L. Treatment of dilated gastrojejunostomy with sclerotherapy. Obes Surg. 2003;13(2):254–7.
Spaulding L, Osler T, Patlak J. Long-term results of sclerotherapy for dilated gastrojejunostomy after gastric bypass. Surg Obes Relat Dis. 2007;3(6):623–6.
Thompson CC et al. Peroral endoscopic reduction of dilated gastrojejunal anastomosis after Roux-en-Y gastric bypass: a possible new option for patients with weight regain. Surg Endosc. 2006;20(11):1744–8.
Mikami D et al. Natural orifice surgery: initial US experience utilizing the StomaphyX device to reduce gastric pouches after Roux-en-Y gastric bypass. Surg Endosc. 2010;24(1):223–8.
Thompson CC et al. Stoma size critical to 12-month outcomes in endoscopic suturing for gastric bypass repair. Surg Obes Relat Dis. 2012;8(3):282–7.
Galvão Neto M’, Rodriguez L’, Zundel N. Endoscopic revision of Roux-en-Y gastric bypass stomal dilation with a suturing device: preliminary results of a first out-of-United States series. Bariatric Times. 2011;8:1–34.
Heylen AM et al. The OTSC(R)-clip in revisional endoscopy against weight gain after bariatric gastric bypass surgery. Obes Surg. 2011;21(10):1629–33.
Aly A. Argon plasma coagulation and gastric bypass–a novel solution to stomal dilation. Obes Surg. 2009;19(6):788–90.
Brethauer SA et al. Endoscopy and upper gastrointestinal contrast studies are complementary in evaluation of weight regain after bariatric surgery. Surg Obes Relat Dis. 2006;2(6):643–8. discussion 649–50.
Christou NV, Look D, Maclean LD. Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg. 2006;244(5):734–40.
Malick KJ. Clinical applications of argon plasma coagulation in endoscopy. Gastroenterol Nurs. 2006;29(5):386–91. quiz 392–3.
Storek D et al. Endoscopic argon gas coagulation—initial clinical experiences. Z Gastroenterol. 1993;31(11):675–9.
Garrido T. Análise histopatológica do efeito da eletrocoagulação bipolar e da aplicação de plasma de argônio em espécimes cirúrgicos do trato digestório. ABCD Arq Bras Cir Dig. 2002;15(2):116–20.
Pinotti AC et al. Endoscopic ablation of Barrett's esophagus using argon plasma coagulation: a prospective study after fundoplication. Dis Esophagus. 2004;17(3):243–6.
Dotti VP et al. Endoscopic argon plasma thermo-coagulation of Barrett's esophagus using different powers: histopathological and post procedure symptons analysis. Rev Col Bras Cir. 2009;36(2):110–7.
Thompson CC et al. Endoscopic suturing for transoral outlet reduction increases weight loss after Roux-en-Y gastric bypass surgery. Gastroenterology. 2013;145(1):129–37.
Abu Dayyeh BK et al. Endoscopic sclerotherapy for the treatment of weight regain after Roux-en-Y gastric bypass: outcomes, complications, and predictors of response in 575 procedures. Gastrointest Endosc. 2012;76(2):275–82.
Horgan S et al. Incisionless revision of post-Roux-en-Y bypass stomal and pouch dilation: multicenter registry results. Surg Obes Relat Dis. 2010;6(3):290–5.
Herron DM et al. Gastric bypass pouch and stoma reduction using a transoral endoscopic anchor placement system: a feasibility study. Surg Endosc. 2008;22(4):1093–9.
Yimcharoen P et al. Endoscopic findings and outcomes of revisional procedures for patients with weight recidivism after gastric bypass. Surg Endosc. 2011;25(10):3345–52.
Abu Dayyeh BK, Lautz DB, Thompson CC. Gastrojejunal stoma diameter predicts weight regain after Roux-en-Y gastric bypass. Clin Gastroenterol Hepatol. 2011;9(3):228–33.
Conflict of Interest
All authors declare no disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baretta, G.A.P., Alhinho, H.C.A.W., Matias, J.E.F. et al. Argon Plasma Coagulation of Gastrojejunal Anastomosis for Weight Regain After Gastric Bypass. OBES SURG 25, 72–79 (2015). https://doi.org/10.1007/s11695-014-1363-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1363-2